Summary
Objective
African potato (Hypoxis obtusa) is commonly used in Sub-Saharan Africa as a complementary herbal remedy for HIV-infected patients. It is unknown whether or not co-administration of African potato alters the pharmacokinetics of protease inhibitor antiretrovirals. The objective of this study was to investigate the impact of the African potato on the steady-state pharmacokinetics of ritonavir-boosted lopinavir (LPV/r).
Methods
Sixteen adult volunteers were administered LPV/r 400/100 mg twice a day for 14 days, followed by concomitant administration with African potato given once daily for 7 days. Lopinavir plasma exposure as estimated by the area under the concentration–time curve over the 12-h dosing interval (AUC0–12h, AUCτ) was determined on day 14 and again on day 21. Lopinavir in plasma was analyzed using a validated liquid chromatography with tandem mass spectrometry (LC-MS/MS) method. Steady-state AUCτ and the maximum concentration following dose administration (Cmax) were determined using non-compartmental methods using WinNonlin Professional version 5.2.1. Statistical analyses were performed using Stata version 12.1.
Results
Co-administration of African potato was not associated with any change in lopinavir AUCτ, Cmax, or Ctrough.
Conclusions
African potato when taken concomitantly with LPV/r is well-tolerated and not associated with clinically significant changes in lopinavir pharmacokinetics.
Keywords: Herb–drug interactions, Hypoxis obtusa, Pharmacokinetic interactions, Herbal medicines
Introduction
The concomitant use of complementary and alternative medicines in both developing and developed nations is commonplace. More than 30% of HIV-infected patients in Uganda use complementary medicines concomitantly with antiretroviral medicines.1,2 More than 70% of patients with HIV infection in South Africa3 and US African-Americans use these medicines together.4 Similarly, the use of herbal medicines in Zimbabwe is estimated to be over 68% in HIV patients.5,6 This widespread use of herbal medicines in combination with conventional treatments for HIV may result in unanticipated herb–antiretroviral interactions.
Lopinavir/ritonavir (LPV/r) is a potent HIV protease inhibitor combination used with other anti-HIV medicines for the treatment of HIV infection.7–9 Lopinavir (LPV), metabolized primarily by hepatic and gastrointestinal cytochrome p450 3A (CYP3A), is pharmacokinetically ‘boosted’ by ritonavir (RTV) through inhibition of CYP3A.7,10,11 Since LPV and RTV are both substrates for and inhibitors of CYP3A4, caution is warranted in the case of co-administration of LPV/r with medicinal products that are CYP3A4 substrates and/or may alter CYP3A4 activity. St John’s wort (Hypericum perforatum), a known potent inducer of CYP3A4, increases clearance of indinavir, another protease inhibitor that is a substrate of CYP3A4.12 Consequently, St John’s wort is contraindicated while taking LPV/r due to the risk of decreased plasma concentrations and the potential for decreased efficacy.7
The genus Hypoxis, which is also commonly known as African potato, is a genus of plants belonging to the Hypoxidaceae family. Hypoxoside, the main constituent of the Hypoxis genus, is hydrolyzed to its aglycone form, rooperol, which is a bioactive dicatechol agent shown to have anti-cancer,13 antibacterial, and anti-inflammatory properties in vitro.14 In Sub-Saharan Africa, Hypoxis is widely distributed, with over 40 species, including Hypoxis obtusa and Hypoxis hemerocallidea. Hypoxis hemerocallidea is a popular species in South Africa for its use in African traditional remedies and is commonly used for its immune-boosting properties in HIV patients, despite the lack of scientific evidence of clinical efficacy.15 Hypoxis obtusa is found in Zimbabwe, Mozambique, and Kenya.16
In vitro studies with human liver microsomes indicate that extracts of Hypoxis obtusa and Hypoxis hemerocallidea have a significant inhibitory effect on CYP3A4, the primary isozyme responsible for the metabolism of LPV/r.17,18 Multi-drug therapy has been found to be more effective for HIV/AIDS therapy, and less likely to be associated with the development of resistance. It is important to know whether or not the Hypoxis obtusa causes a reduction in exposure that might result in reduced efficacy. Also, an increase in exposure could be associated with an increased lipid/diabetes risk [Au?1]. While in vitro data suggest a significant interaction between Hypoxis and LPV/r, the impact of co-administration of Hypoxis obtusa and LPV/r has not been evaluated in vivo. The objective of this study was to investigate the in vivo effects of Hypoxis obtusa on the clinical pharmacokinetics (PK) of LPV/r.
Methods
Study population
Healthy HIV-seronegative adult volunteers between the ages of 18 and 60 years, weighing at least 50 kg, and within 20% of their ideal body weight, were eligible for enrollment. Female subjects were required to have a negative pregnancy test at screening, to practice adequate birth control, and to be non-lactating at the time of enrollment. Subjects were required to abstain from consuming grapefruit and the use of alcohol and tobacco for at least 48 h before entry and throughout the study period until the last blood samples had been obtained.
Participants with a recent history of illicit drug use or alcohol use, who were using over-the-counter or prescribed medicines known to inhibit/induce CYP450 isozymes or that are substrates of CYP3A4, CYP2D6, CYP2C8 enzymes including oral contraceptives, those with evidence of an acute illness, family history of congenital prolongation of the QTc interval or with any conditions known to prolong the QTc interval, such as cardiac arrhythmias, bradycardia or severe heart disease, and those with a history of hypokalemia, hypomagnesemia, or hypercholesteremia were excluded from participating in this study. Subjects were restricted from taking any medications other than the study medications without the prior approval of the study physicians.
Study setting and ethical conduct of the study
All subjects were admitted to the University of California San Francisco (UCSF) Clinical Research Center at San Francisco General Hospital on the evening of study days 13 and 20. The study was reviewed and approved by the UCSF Committee on Human Research before initiation of study activities. The study was conducted in accordance with the protocol, pertinent requirements of the Committee on Human Research ethics guidelines, and the Declaration of Helsinki. Informed consent was obtained from the volunteers before performing any study-related activities.
Study design and treatment
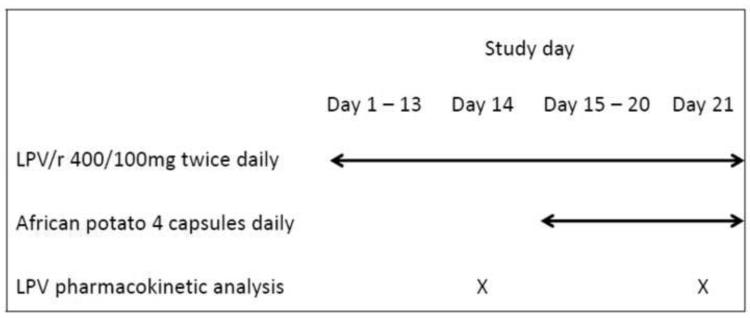
This study was an open-label two-period fixed sequence cross-over PK drug interaction study to investigate the effect of African potato on the steady-state PK of LPV/r (Figure 1). Each subject received LPV/r alone for 14 days, followed by LPV/r plus African potato until day 21. LPV/r was administered at the recommended daily dose of 400 mg/100 mg twice daily. The recommended dosing of African potato is 15 mg/kg/daily of hypoxoside; four capsules of African potato (containing 320 mg hypoxoside) as a single dose once a day in the morning were administered to each subject for 7 days. Subjects were required to fast at least 10 h before until 4 h post administration of the study medicines on days 14 and 21, respectively. The dosing on these study days was observed by Clinical Research Center staff following the overnight fast. Self-reporting and a pill count took place to ensure that participants adhered to the study protocol.
Figure 1.
Schematic of the dosing regimen and pharmacokinetic sample collection.
Pharmacokinetic sampling and drug concentration assays
Subjects were confined to the San Francisco General Hospital Clinical Research Center from at least 10 h before to 12 h following administration of the study dose on days 14 and 21. A total of nine blood samples (5 ml each) were collected pre-dose (within 1 h before dosing) and at 1, 2, 4, 6, 8, and 12 h post-dose for each study period. A physical examination and vital examination was done during screening, at the time of admission to and discharge from the Clinical Research Center, and at the time of the post-study follow-up visit.
LPV/r (Kaletra; manufactured by Abbott Laboratories, USA) and the African potato (manufactured by Herbal Solutions, Harare, Zimbabwe) were used in the study. The liquid chromatography with tandem mass spectrometry (LC-MS/MS) system consisted of twin PE 200 micro LC pumps, a PE 200 autosampler (Perkin-Elmer, Norwalk, CT, USA), and the API 2000 triple quadrupole mass spectrometer (AB Sciex, Concord, Ontario, Canada). Chromatographic separation was achieved on a Zorbax C 8 column (50 × 2.1 mm, 5 μm; Agilent Technologies Inc., Santa Clara, CA, USA). All chemicals were of HPLC grade.
Samples for PK analysis were analyzed within the Drug Research Unit of the Department of Clinical Pharmacy. Plasma samples were stored at −70 °C until analysis. Lopinavir was quantitated using a validated liquid chromatography tandem mass spectrometry method (LC tandem MS). Briefly, 50 μl of plasma sample was mixed with 150 μl ammonium formate (10 mM, pH 4.0) and 50 μl internal standard (methyl indinavir) (0.8 μg/ml), and then 400 μl acetonitrile was added and vortex-mixed for 15 s. After centrifugation at 20 000 g for 10 min, the sample was transferred to an autosampler vial. The injection volume was 10 μl. Electron spray ionization in positive mode (ESI+) was used for ion source, and multiple-reaction monitoring (MRM) mode was chosen for quantification. The precursor-product ion pairs for quantification were m/z 630→429 for LPV and m/z 629→421 for the IS [Au?2]. Samples from treatments A and B for each subject were analyzed in a single run. The linearity range of 0.050 μg/ml to 8.0 μg/ml for LPV was used to quantify concentration in subject plasma samples. The calibration curves consisted of eight non-zero calibrators for LPV.
Efficacy and safety measurements
Safety was evaluated by monitoring adverse events, vital signs, and laboratory results during the study period and through self-reporting by subjects. Clinical laboratory tests monitored during the study included the complete blood count (CBC) with differential, liver function tests (LFTs), and lipid profile. These tests were conducted before enrollment (during screening), on days 14, 18, and 21, and at 2 weeks, on completing the study (follow-up visit).
Pharmacokinetic analysis
The following LPV PK parameters were determined on day 14 after LPV/r alone and day 21 after LPV/r plus African potato: area under the concentration–time curve over the 12-h dosing interval (AUC0–12h, AUCτ), maximum concentration following dose administration (Cmax), concentration at the end of the dosing interval (Ctrough), time to maximum concentration following dose administration (Tmax), and apparent clearance (CLF). The primary PK parameters AUC0–12 h (AUCτ) and Cmax, and the secondary PK parameters Ctrough, Tmax, T1/2 [Au?3], and Kel [Au?3], were derived from plasma concentrations of LPV for each individual by non-compartmental methods using WinNonlin Professional version 5.2.1 (Pharsight Corp., USA). The maximum concentration following dose administration and Tmax were taken directly from the plasma concentration–time profiles of individual subjects. The AUCτ in ng*h/ml was calculated by linear trapezoidal rule from the measured data points from time of administration until 12 h post-dose. The Kel was calculated as the negative slope of the log-linear terminal portion of the plasma concentration versus time curve using linear regression with 1/x2 weighting. A minimum of three concentrations were considered. The T1/2 was estimated from the elimination rate constant using T1/2 = 0.693/Kel.
Statistical analysis
Statistical analyses were performed using Stata version 12.1 (StataCorp, TX, USA). Based on the intra-subject coefficient of variation of 15% for PK parameters for LPV,19 a 5% consumer risk with 80% power, and assuming no difference between treatments, 16 subjects were necessary to demonstrate equivalence within the conventional acceptance range of 0.80–1.25 applied for bioequivalence studies.20
Arithmetic means and standard deviations were calculated on the individual concentrations. Ratios of the means were calculated using the geometric mean (GM) of log-transformed Cmax, Ctrough, and AUCτ. Ratios of means are expressed as a percentage of the GM of the LPV/r alone. The test of bioequivalence between LPV/r alone and in combination with African potato was assessed using the 90% confidence interval for the GM ratios for the PK parameters. To conclude a lack of interaction/effect, the 90% confidence intervals within 80–125% for the AUCτ and Cmax was used.20 The Wilcoxon signed-ranks test was used to test for statistical significance in the median Tmax. Descriptive statistics were used to evaluate adverse events (AEs) occurring during the study.
Results
Demographics and baseline characteristics
Sixteen subjects (12 males, four females) were enrolled and completed the study. The median (range) age of subjects was 28 years (19–53 years). The median (range) weight was 78.4 kg (53.3–96.0 kg) and body mass index was 25.2 kg/m2 (19.0–31.9 kg/m2). Four subjects whose weight was outside the inclusion criterion of ±20% of ideal body weight were enrolled in the study. This protocol deviation is not expected to impact significantly on study results since each subject acted as their own control. All 16 subjects who completed the study were included in the PK and statistical analysis.
Effect of African potato on LPV steady-state pharmacokinetics
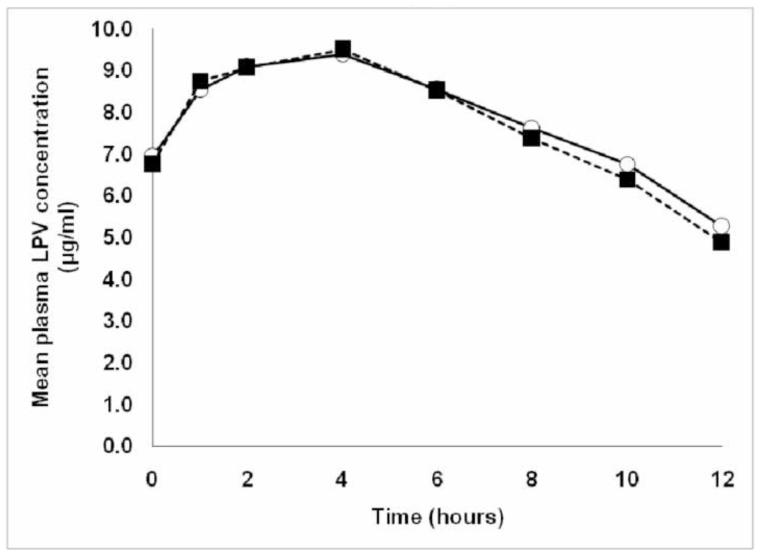
Steady-state plasma concentration–time profiles of LPV with and without African potato were similar (Figure 2). Relative to repeated administration of LPV/r alone, the steady-state PK parameters Cmax and AUCτ of LPV remained unchanged following concomitant administration of multiple-dose African potato (Table 1). The corresponding 90% confidence intervals were within the 80–125% limit, indicating a lack of clinically significant interaction. There was no statistically significant difference (p = 0.5488) in Tmax between the two treatments based on the Wilcoxon signed-ranks test. The data on Ctrough were inconclusive (Table 1) since the upper confidence limit was marginally outside the acceptance limit and the confidence interval included PE [Au?4] = 100.
Figure 2.
Mean steady-state plasma lopinavir concentration–time profiles with and without African potato (n = 16): ○, LPV in 400/100 mg LPV/r doses twice daily (n = 16); ■, LPV in 400/100 mg LPV/r doses twice daily plus African potato four capsules once daily (n = 16).
Table 1.
Summary of steady-state plasma LPV pharmacokinetic parameters following repeated dose administration (n = 16)
| Arithmetic mean (SD) | Geometric means | PE | 90% CI | CV (%) | |||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| LPV/r | LPV/r plus AP | LPV/r | LPV/r plus | ||||
| AP | |||||||
| AUCτ (μg*h/ml) | 94.40 (25.11) | 93.18 (26.76) | 90.78 | 89.66 | 98.77 | 91.81–106.25 | 15.10 |
| Cmax (μg/ml) | 10.06 (1.99) | 10.18 (2.25) | 9.86 | 9.95 | 100.90 | 94.48–107.76 | 16.78 |
| Ctrough (μg/ml) | 4.85 (2.18) | 4.90 (2.61) | 4.13 | 4.38 | 105.98 | 86.81–129.38 | 48.00 |
| Tmax (h)a | 4 (1, 8) | 4 (1, 10) | - | - | - | - | - |
| CLF (l/h) | 4.61 (1.56) | 4.64 (1.32) | - | - | - | - | - |
AUCτ, area under the concentration–time curve within a dosing interval; Cmax, maximum concentration following dose administration; Ctrough, plasma concentration at the end of the dosing interval; 90% CI, 90% confidence interval of the geometric mean ratio; CLF, apparent clearance; CV (%), coefficient of variation; LPV/r, lopinavir/ritonavir 400/100 mg (alone) twice daily for 14 days; LPV/r plus African potato, lopinavir/ritonavir 400/100 mg twice daily plus African potato (four capsules) once daily for 7 days; PE is the point estimate of the ratio of geometric means of LPV/r plus African potato and LPV/r; SD, standard deviation from the mean; Tmax, time to reach Cmax.
Median (minimum, maximum).
Safety and tolerability
The study medications were generally well tolerated throughout the study. There were no serious adverse events observed in the study. As expected, there were a few cases of mild diarrhea and headache on LPV/r initiation. These were considered mild and resolved after a few days on the LPV/r medication. Total cholesterol and triglycerides were elevated but within limits during LPV/r treatment, except in one subject with grade 1 elevation (<400 mg/dl) in triglyceride concentrations. There were no clinically significant changes in vital signs or laboratory results in both treatments during the study.
Discussion
To our knowledge, our study is the first in vivo trial to evaluate the impact of co-administration of any African herbal remedy and antiretroviral protease inhibitors. We specifically elected to study the African potato due to its documented wide usage in Sub-Saharan Africa. LPV/r was the selected antiretroviral due to its primary role in the treatment of HIV, as well as its known risk for multiple drug interactions. Our study demonstrated that the African potato had no significant effect on the steady-state pharmacokinetics of LPV boosted with RTV. While previous in vitro studies have noted a significant Hypoxis effect on CYP3A4,17,21 this interaction was not observed in vivo. Our confirmation of a lack of clinically significant interaction is consistent with that observed with the co-administration of Hypoxis hemerocallidea and efavirenz. 22 Of note, while AUCτ and Cmax were highly consistent among subjects, LPV trough concentrations were found to be highly variable. The reasons for this finding are unknown.
Hypoxoside is rapidly converted to its aglycone, rooperol, in the gastrointestinal tract by beta-glucosidase enzymes.23 Consequently, it is possible that the plasma concentrations of hypoxoside achieved in plasma following oral administration were low compared to the concentrations used in previous in vitro experiments.
Ritonavir, a potent inhibitor of CYP3A4 is included in the LPV formulation to boost the plasma levels of LPV.10,11 Consequently, it is conceivable that the lack of effect with African potato on LPV pharmacokinetics may have been confounded by the presence of RTV. However, considering that the standard of care is RTV-boosting of LPV or other protease inhibitors, results suggest a lack of clinically important pharmacokinetic drug interactions with African potato and RTV-boosted protease inhibitor regimens.
In conclusion, the concomitant administration of usual doses of African potato with RTV-boosted LPV is not associated with clinically significant pharmacokinetic changes in LPV/r. We conclude that African potato can be safely administered concomitantly with LPV/r.
Acknowledgements
The authors would like to thank Tina Lee and Kira Freeman for the assistance in the recruitment of study subjects and co-ordination of the study. The authors would also like to thank the study subjects and the assistance and support provided by Sarah Lange and the staff at the UCSF Clinical Research Center at San Francisco General Hospital during the clinical phase of the study.
Funding: This work was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), through UCSF-CTSI (grant number UL1 RR024131) and in part by the NIH sponsored UCSF Center for AIDS Research (grant number P30A1022763). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. LG was the recipient of a Fogarty International Fellowship award for research training at the University of California San Francisco in the United States and the International Pharmaceutical Federation (FIP) Foundation for Education and Research’s Young Pharmacist/Pharmaceutical Scientist Grant for Professional Innovation, which supported the preliminary research work.
Ethical approval: The study was reviewed and approved by the University of California San Francisco Committee on Human Research before initiation of study activities. The study was conducted in accordance with the protocol, pertinent requirements of the Committee on Human Research ethics guidelines, and the Declaration of Helsinki. Informed consent was obtained from the volunteers before performing any study-related activities.
Footnotes
Conflict of interest: The authors have no personal or financial relationships with people or other organizations that might inappropriately influence this work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Langlois-Klassen D, Kipp W, Jhangri GS, Rubaale T. Use of traditional herbal medicine by AIDS patients in Kabarole District, western Uganda. Am J Trop Med Hyg. 2007;77:757–63. [PubMed] [Google Scholar]
- 2.Namuddu B, Kalyango JN, Karamagi C, et al. Prevalence and factors associated with traditional herbal medicine use among patients on highly active antiretroviral therapy in Uganda. BMC Public Health. 2011;11:855. doi: 10.1186/1471-2458-11-855. [Au?5] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Babb DA, Pemba L, Seatlanyane P, Charalambous S, Churchyard GJ, Grant AD. Use of traditional medicine by HIV-infected individuals in South Africa in the era of antiretroviral therapy. Psychol Health Med. 2007;12:314–20. doi: 10.1080/13548500600621511. [DOI] [PubMed] [Google Scholar]
- 4.Owen-Smith A, McCarty F, Hankerson-Dyson D, Diclemente R. Prevalence and predictors of complementary and alternative medicine use in African-Americans with acquired immune deficiency syndrome. Focus Altern Complement Ther. 2012;17:33–42. doi: 10.1111/j.2042-7166.2011.01140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sebit MB, Chandiwana SK, Latif AS, et al. Quality of life evaluation in patients with HIV-I infection: the impact of traditional medicine in Zimbabwe. Cent Afr J Med. 2000;46:208–13. [Au?5] [PubMed] [Google Scholar]
- 6.Sebit MB, Chandiwana SK, Latif AS, et al. Neuropsychiatric aspects of HIV disease progression: impact of traditional herbs on adult patients in Zimbabwe. Prog Neuropsychopharmacol Biol Psychiatry. 2002;26:451–6. doi: 10.1016/s0278-5846(01)00285-8. [Au?5] [DOI] [PubMed] [Google Scholar]
- 7.Product monograph: Kaletra (lopinavir/ritonavir) tablets and oral solution. Abbott Laboratories; North Chicago, IL, USA: May, 2012. [Google Scholar]
- 8.Panel on Antiretroviral Guidelines for Adults and Adolescents . Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. US Department of Health and Human Services; 2012. pp. F–3. [Google Scholar]
- 9.Antiretroviral therapy for HIV infection in adults and adolescents: recommendations for public health approach. World Health Organization; Geneva: 2012. [PubMed] [Google Scholar]
- 10.Kumar GN, Dykstra J, Roberts EM, et al. Potent inhibition of the cytochrome P-450 3A-mediated human liver microsomal metabolism of a novel HIV protease inhibitor by ritonavir: a positive drug–drug interaction. Drug Metab Dispos. 1999;27:902–8. [Au?5] [PubMed] [Google Scholar]
- 11.Sham HL, Kempf DJ, Molla A, et al. ABT-378, a highly potent inhibitor of the human immunodeficiency virus protease. Antimicrob Agents Chemother. 1998;42:3218–24. doi: 10.1128/aac.42.12.3218. [Au?5] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Piscitelli SC, Burstein AH, Chaitt D, Alfaro RM, Falloon J. Indinavir concentrations and St John’s wort. Lancet. 2000;355:547–8. doi: 10.1016/S0140-6736(99)05712-8. [DOI] [PubMed] [Google Scholar]
- 13.Albrecht CP, Theron EJ, Kruger PB. Morphological characterisation of the cellgrowth inhibitory activity of rooperol. S Afr Med J. 1995:853–60. Au?5. [PubMed] [Google Scholar]
- 14.Laporta O, Funes L, Garzon MT, Villalain J, Micol V. Role of membranes on the antibacterial and anti-inflammatory activities of the bioactive compounds from Hypoxis rooperi corm extract. Arch Biochem Biophys. 2007;467:119–31. doi: 10.1016/j.abb.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 15.Mills E, Cooper C, Seely D, Kanfer I. African herbal medicines in the treatment of HIV: Hypoxis and Sutherlandia. An overview of evidence and pharmacology. Nutr J. 2005;4:19. doi: 10.1186/1475-2891-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nordal I, Lane MM, Holt E, Staubo I. Taxonomic studies of the genus Hypoxis in East Africa. Nordic J Bot. 1985;5:15–30. [Google Scholar]
- 17.Gwaza L, Wolfe AR, Benet LZ, et al. In vitro inhibitory effects of Hypoxis obtusa and Dicoma anomala on cyp450 enzymes and p-glycoprotein. African Journal of Pharmacy and Pharmacology. 2009;3:539–46. [Au?5] [Google Scholar]
- 18.Nair VD, Foster BC, Thor Arnason J, Mills EJ, Kanfer I. In vitro evaluation of human cytochrome P450 and P-glycoprotein-mediated metabolism of some phytochemicals in extracts and formulations of African potato. Phytomedicine. 2007;14:498–507. doi: 10.1016/j.phymed.2006.12.004. [Au?6] [DOI] [PubMed] [Google Scholar]
- 19.Wire MB, McLean HB, Pendry C, Theodore D, Park JW, Peng B. Assessment of the pharmacokinetic interaction between eltrombopag and lopinavir–ritonavir in healthy adult subjects. Antimicrob Agents Chemother. 2012;56:2846–51. doi: 10.1128/AAC.05214-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.US FDA guidance for industry: statistical approaches to establishing bioequivalence. US Department of Health and Human Services; 2001. [Google Scholar]
- 21.Vipin DP, Nair BC, Foster J, Arnason T, Mills EJ, Kanfer I. In vitro evaluation of human cytochrome P450 and P-glycoprotein-mediated metabolism of some phytochemicals in extracts and formulations of African potato. Phytomedicine. 2007:498–507. doi: 10.1016/j.phymed.2006.12.004. [Au?7] [Au?6] [DOI] [PubMed] [Google Scholar]
- 22.Mogatle S, Skinner M, Mills E, Kanfer I. Effect of African potato (Hypoxis hemerocallidea) on the pharmacokinetics of efavirenz. S Afr Med J. 2008;98:945–9. [PubMed] [Google Scholar]
- 23.Kruger PB, Albrecht CF, Liebenberg RW, van Jaarsveld PP. Studies on hypoxoside and rooperol analogues from Hypoxis rooperi and Hypoxis latifolia and their biotransformation in man by using high-performance liquid chromatography with in-line sorption enrichment and diode-array detection. J Chromatogr B Biomed Appl. 1994;662:71–8. doi: 10.1016/0378-4347(94)00392-0. [DOI] [PubMed] [Google Scholar]