Abstract
Over the past century, the world has seen unprecedented declines in mortality rates, leading to an accelerated increase in the world population. This century will realise falling fertility rates alongside ageing populations. The 20th century was the century of population growth; the 21st century will be remembered as the century of ageing. Increase in life expectancy is one of the highest achievements of humankind; however, ageing and age-related disease is a mounting challenge for individuals, families, and for social, economic, and healthcare systems. Since healthy life expectancy has lagged behind the increase in life expectancy, the rise in morbidity will increase the burden on healthcare systems. Implementation of preventive health strategies to decrease, delay or prevent frailty, lung, breast and colon cancer, cardiovascular disease, metabolic syndrome, osteoporosis and osteopaenia, may increase health expectancy, and permit women to age gracefully and maintain independent living, without disability, for as long as possible.
Keywords: ageing, life expectancy, health expectancy, preventive strategies, fertility rate
Introduction
A growing world
Human populations grew at about 0.05% annually for 10,000 years such that, by the year 1500, the global population was around 400 million people. A significant increase in population growth occurred in the 17th and 18th centuries, with the growth rate increasing to about 0.5% annually and reaching 1 billion at the start of the 19th century. The population growth rate continued to increase to 0.7% after 1900, and to 2% in the 1960s, with 1.6 billion worldwide in the beginning of the 20th century.1 By the year 2000, 6.1 billion people inhabited our planet. The United Nations projects that, by 2100, the world population will reach 11.5 billion people,2 an increase of almost 5 billion3 people between 2000 and 2100.
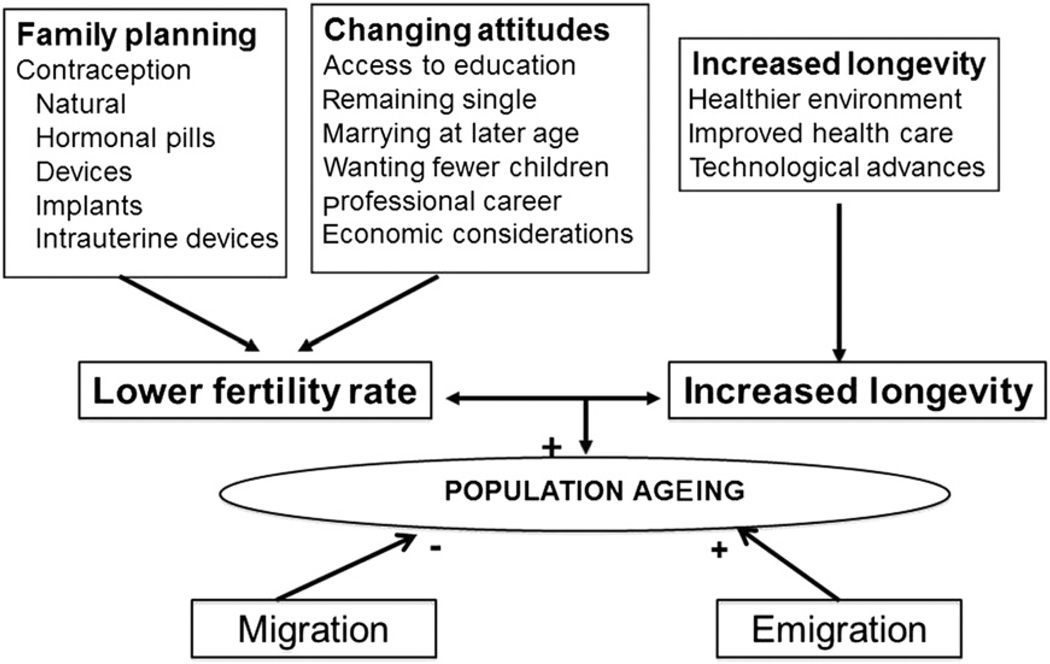
The four most important elements in determining population growth and ageing in any country or region are fertility rate, life expectancy, migration, and emigration.4
Women’s role in society has changed. They have more access to education and greater choice in careers; childcare outside of the home is associated with a decrease in fertility rate. Improvements in healthcare are one of the important factors increasing life expectancy. Population ageing is a direct result of the decrease in the fertility rate and the increase in life expectancy. Migration within and emigration from a country or region are the most important factors affecting demographic change; however, as mostly younger people migrate or emigrate, this will influence the ageing pattern of these countries (Fig. 1).
Fig. 1.
Factors contributing to population ageing.
Immigration has increasingly become perceived as a potential means of preventing population decline, maintaining a sufficient labour force and support ratio, and thus slowing down structural population ageing. In particular, immigration has a potentially strong and long-lasting affect on population growth and composition through the interaction among the number of migrants, their relatively younger age, and their higher fertility, according to Harper.4 Uncontrolled immigration could, however, result in demographic changes that may influence social, cultural, and economic stability, and may lead, in extreme conditions, to discontent.
The increase in world population from 1.6 billion in 1900 to 6.1 billion in 2000 arose primarily from population growth in less developed countries that experienced a significant increase in life expectancy. While rising life expectancy occurred over centuries in Europe, many less developed countries accomplished it in decades. As growth rates in less developed countries rose to levels never experienced in more developed countries, many countries implemented policies to lower the birth rate to adjust for rapidly declining death rates, especially related to lower rates of perinatal and infant mortality. Although some less developed countries had dramatic declines in birth rates, others had a somewhat more gradual decline, and some experienced almost no decline at all.
Overall, the total fertility rate in less developed countries declined from about 6.0 in the early 1950s to about 2.5 today, a much more rapid decrease than that of Europe from 2.5 in 1960 to 1.55 in 2011, and North America from 3.7 in 1960 to 2.16 in 2011. Thus, although less developed countries continue to have population growth, the EU27 countries, in particular, will see population shrinkage of around 0.2% per year between 2020 and 2045. Italy and Germany will be particularly affected, with projected falls from 60 million to 57 million in Italy between 2010 and 2050, and 82 million to 79 million for Germany.3 Italy will need to raise its retirement age to 77 or admit 2.2 million young immigrants annually to maintain its worker to retiree ratio, at the expense of a significant change in its demography.
The past century has witnessed a transition from a high mortality and high fertility pattern to one of historically unprecedented declines in mortality rates followed by equally unprecedented declines in fertility rates. This change has resulted in a rapidly ageing world population. The 20th century was the century of population growth; the 21st century will be remembered as the century of ageing.
In 2010, the world population has reached a transition point. The rapid growth of the second half of the 20th century has slowed, but factors such as continuously increasing longevity and slower-than-expected declines in birth rates, guarantee continued growth for decades.
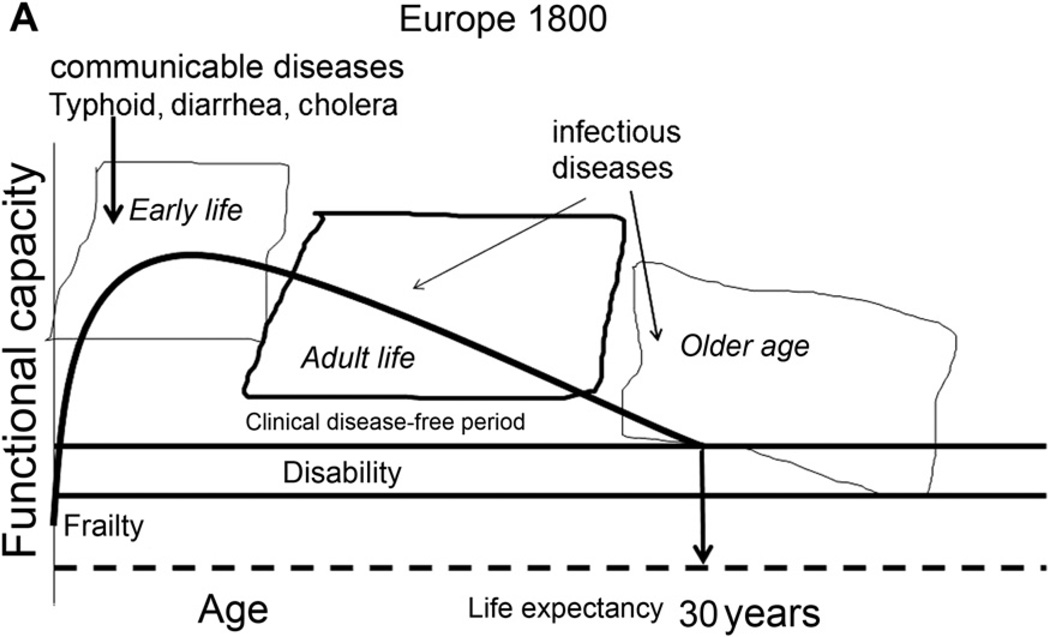
Life expectancy
Humans had a life expectancy of about 30 years for about 99.9% of the time we inhabited this planet (Fig. 2). Today, in developed countries, more than 75% die after the age of 75 years. In the record-holding country, Japan, female life expectancy was 86 years in 2007,7 surpassing the 85-year limit to human life expectancy proposed by Fries et al.8
Fig. 2.
Life expectancy in Europe 1800.
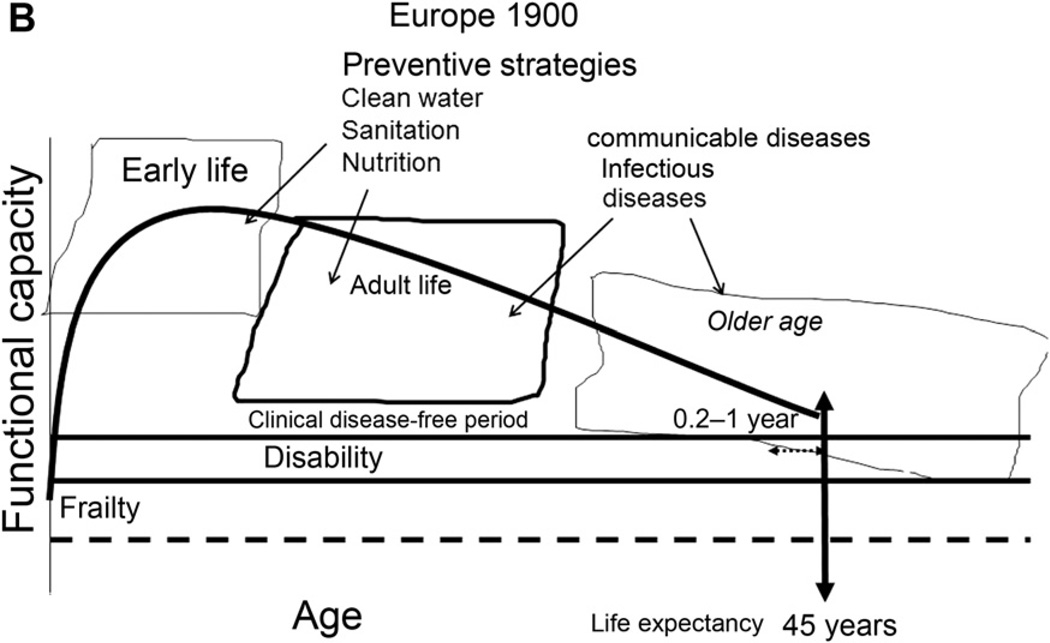
In 1900 in Europe, life expectancy was around 45 years,9 and health expectancy, the ability to live independently, was similar between men and women since one died within days, weeks or months from infectious diseases. Life expectancy estimates reflect how many years a person might be expected to live. Healthy life expectancy is an estimate of how many years they might live in ‘good health and without disability’. Most babies born after 2000 in countries with long-lived residents will celebrate their 100th birthdays if the present yearly increase in life expectancy continues through the 21st century.10
Death rates fell substantially, well before any effective treatment or immunisation was developed. Probably, life-style changes owing to improved sanitation, hygiene and better nutrition contributed to longer life. Advances in the understanding of contagion and infection contributed toward eradication of typhoid and cholera. Hence, public health projects such as sewage and water systems, and better housing and working conditions, helped stop typhoid and diarrhoea and prolong life generally (Fig. 3).
Fig. 3.
Life expectancy in Europe 1900.
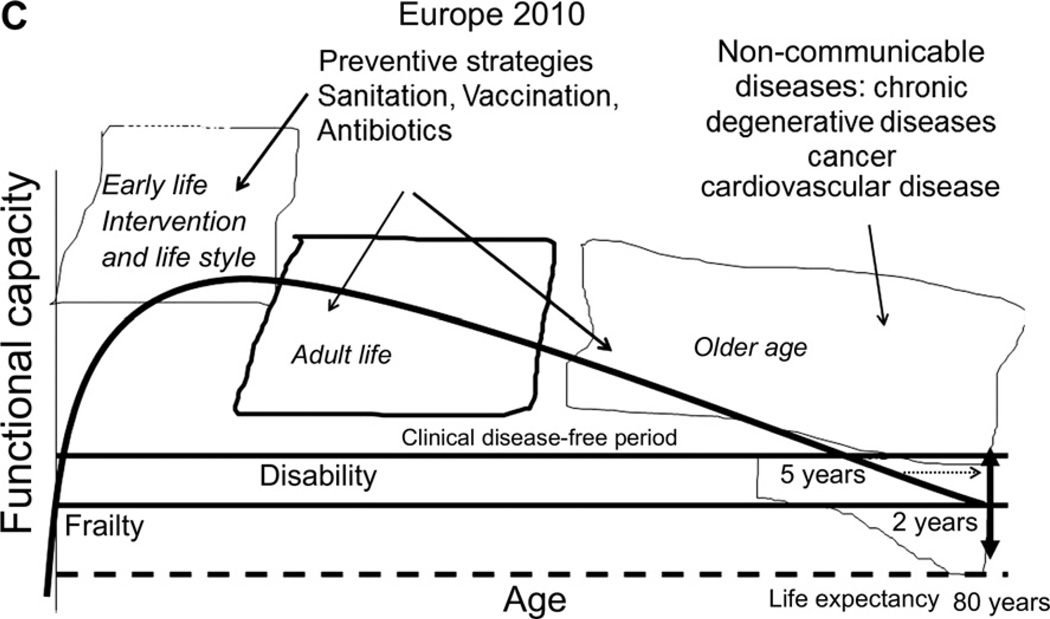
Between the years 1900 to 2000, these public health preventive strategies as well as vaccination and medical advances, such as antibiotics, increased life expectancy; and non-communicable diseases became the main cause of mortality. Even today, more than 2.6 billion people (about 39% of the world’s population) still do not have access to improved sanitation facilities. Sexually transmitted infections (STI), such as chlamydia, contribute to infertility, and human immunodeficiency virus leads to a significant reduction in quality of life, with individual suffering and an extreme cost to society. These diseases could be prevented to a large extent by proper sex education and use of condoms.
In all countries worldwide, poverty is the single greatest obstacle to a secure old age. In less developed countries, the problems associated with old age are poor diet, ill-health and inadequate housing, which are all exacerbated by poverty. Furthermore, because of changes in lifestyles in the developing world, chronic illness is becoming endemic among many older people, because technical advances in medicine have far outrun social and economic development that allows for relatively disease-free living.
Populations in developed countries, by and large, have passed from infectious and parasitic diseases to chronic degenerative diseases. Death from metabolic and degenerative disease increased the gap between male and female mortality by 5–7 years, and between health expectancy and life expectancy in men by 5–7 years, and in women by 7–9 years in most developed countries (Fig. 4). Although women experience greater burdens of morbidity and disability, men die earlier, yet the reasons for such premature mortality are not fully understood (Table 1).11 Health and life expectancy estimates are based on country life tables, analyses of 135 causes of disability for 17 regions of the world and 69 health surveys in 60 countries.12 The estimates of health expectancy are more uncertain than those for life expectancy, because it is difficult to ensure comparable measurements of disability across countries. Because health is a multidimensional notion, several indicators are needed to capture trends. According to Verbrugge and Jette,13 health deterioration can be described by risk factors that lead to diseases and conditions that can cause loss of function and, depending on the environmental context, can result in transition from good health to disability, frailty, and mortality.
Fig. 4.
Life expectancy in Europe 2010.
Table 1.
Life and health expectancy by gender.a
| Country | Life expectancy male versus female years (years beyond males) |
Health expectancy male versus female years (years lost to debility) |
||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| Japan | 79 | 86 (7) | 73 (6) | 78 (8) |
| Monaco | 78 | 85 (7) | 71 (6) | 76 (8) |
| France | 77 | 85 (7) | 71 (6) | 76 (9) |
| Austria | 77 | 83 (6) | 70 (7) | 74 (9) |
| Germany | 77 | 82 (5) | 71 (6) | 75 (7) |
| USA | 76 | 81 (5) | 73 (6) | 78 (8) |
| China | 72 | 75 (3) | 75 (6) | 78 (8) |
| Russian Federation | 60 | 73 (7) | 55 (5) | 65 (7) |
| South Africa | 52 | 55 (3) | 47 (5) | 48 (7) |
On the left side of the table, the age of male life expectancy is listed in years by country. In the next column, the female life expectancy is listed with the number of years women live beyond males in parentheses. On the right side of the table, the expected age of healthy life expectancy for both males and females is listed with the number of years of frailty and disability in parentheses.Adapted from World Health Organization statistics 2008 and 2009.
Ageing successfully would show minimal declines in physiologic function, whereas those ageing ‘poorly’ would show disease-related decrements and loss of reserve capacity, commonly interpreted as the effects of age. The increased gap between health expectancy and life expectancy, however, may be partly due to improved medical knowledge and health-service use in elderly people, without changes in underlying conditions. For instance, initially silent diseases, such as type 2 diabetes, hypertension, and some cancers, now are diagnosed and receive better treatment earlier than previously. This progress leads to a longer period of morbidity, but an improved functional status.14 A rise in prevalence of chronic diseases, including heart disease, arthritis, and diabetes, was recorded in elderly people between the 1980s and 1990s in the USA15 and in 12 Organization for Economic Co-operation and Development countries.16 This increased prevalence may reflect an increase in life expectancy with an increase in the ageing population.
An ageing world
Improved health care, increased access to education, and economic growth, has led to longer life expectancy in every region and across most socioeconomic groups. The proportion of elderly population has been rising and will continue to grow from 8% (551 million people over 65 years) in 2010 to 21% (1964 million people over 65 years) by 2050. The projected two billion elderly people of the year 2050 are already around us as teenagers and young people.
Seventy per cent of all older people now live in low or middle-income countries. Population ageing is also occurring much faster in these countries. These countries have a much briefer opportunity to build the infrastructure necessary to address this demographic trend. The amount of growth and ageing these developing countries experience, however, depends upon the degree to which mother and child health services are able to decrease maternal, neonatal and child mortality. Couples who have access to family planning and health services might choose to reduce family size, raising fewer, but healthy children.
Although this shift to increased life expectancy and decreased fertility rates represents a major global success story, ageing populations also present challenges to families, communities, and countries. This demographic shift is unprecedented in world history, and is most likely irreversible. Not only is the world’s population becoming older, the older are living longer. Those aged 80 years and older are the most rapidly growing age group worldwide. The population of centenarians in 2050 will be 16 times larger than in 2000 (2.2 million compared with 135,000) with the male-to-female ratio of centenarians falling to about 1:4.To maintain current standards of living in more developed countries, and to improve prospects for those in less developed countries, countries must include and involve older populations as productive and active contributors to society. A larger, dependent and elderly population will place greater financial demands on the working population and governmental budgets.17
The trend towards breakdown of extended families, changing lifestyles, and emigration from rural to urban areas has forced elderly people to live alone. The family network was often the only form of welfare and support for elderly people. Now, old people are often considered a family burden. The processes of social change, such as industrialisation, urbanisation, and migration often have a negative effect on care for elderly people, particularly in rural areas.
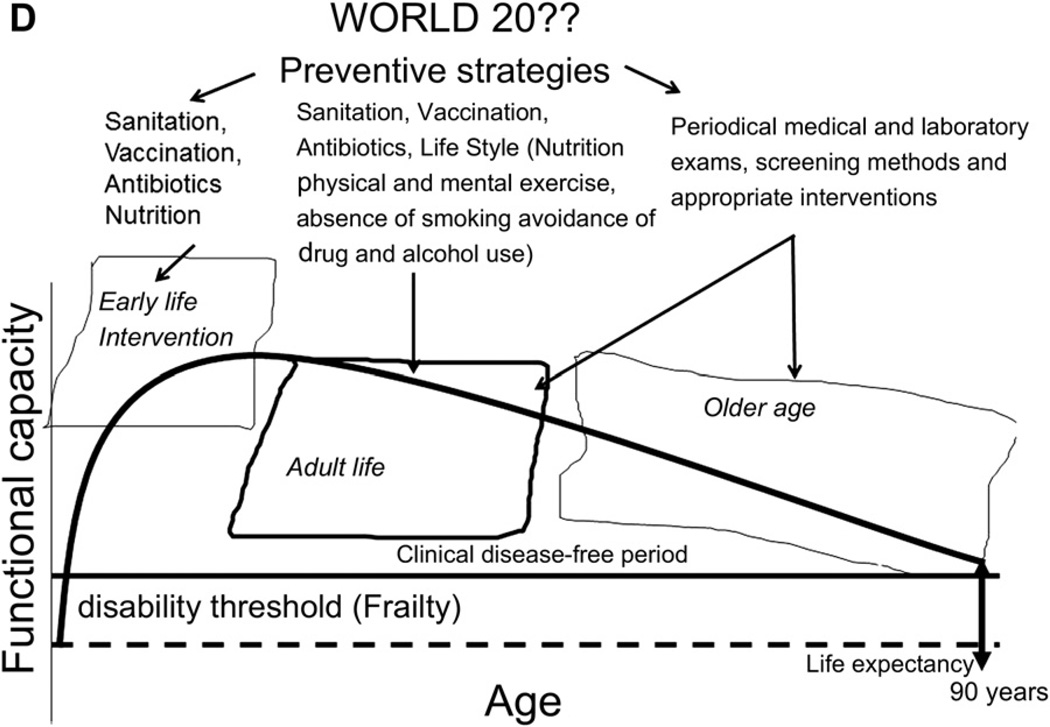
Life course perspective
The life course perspective considers the gap between onset of debilitating illness and death, and illustrates that women die after the age of 80 years in many regions in the world mostly from non-communicable diseases (Fig. 4). This life course perspective leads to important policy and strategy decisions. Cross-sectional studies show differences in mortality and morbidity as a function of socioeconomic status, across various disease categories throughout the life span. Ageing successfully would show minimal declines in physiological function, whereas those ageing ‘poorly’ would show disease-related decrements and loss of reserve capacity, commonly interpreted as the effects of age. We propose six components of successful ageing, namely: (1) avoidance of risk factors for disease (hygiene, absence of smoking and limiting excessive use of alcohol); (2) active engagement (social and emotional health); (3) optimal nutrition; (4) physical activity; (5) retaining a high level of cognitive function (by engaging in cultural and intellectual activity) and (6) periodic medical and laboratory exams and screening methods to early detect and treat any pathological processes (Fig. 5).
Fig. 5.
Potential worldwide life expectancy.
Poverty significantly affects life and health expectancy. It should be measured in terms of property, employment, wages and income, and also in terms of basic education, healthcare, nutrition, water and sanitation. Educational level and marital status have also been shown in several longitudinal studies to be powerful predictors of morbidity, health expectancy, and mortality.18
The economic consequences of retirement place many older citizens in positions of financial vulnerability. As populations age in the developing and the developed worlds, the issue becomes how to keep older persons economically viable within their respective societies. No community is exempt from the financial hardships experienced by ageing populations.
It is clearly possible (and indeed desirable) to improve the health status of women and men when they are old. Yet, a complementary approach to improving the health of older people would focus on appropriate interventions from a much earlier age in order to prevent frailty, which is now seen as a multi-system disorder and one of the central geriatric syndromes. Frailty can be triggered by multiple pathophysiological processes such as malnutrition, hormonal imbalances, chronic inflammation, and multimorbidity. Frailty often leads to deterioration of health status, immobilisation, disability and death, and is particularly characterised by a reduced functional reserve and increased vulnerability to internal and external stressors. Frailty imposes, therefore, an increased risk on older people to recover inadequately from even minor events such as gastroenteritis or change of residence.
The increasing number of frail older people will seriously challenge the healthcare system because primary care for these patients is currently fragmented, time consuming and reactive.1,19 To preserve functional performance and maintain independent living in this vulnerable population, a transition is needed towards more proactive, integrated, and structured health care for older people.
Life-history studies of childhood and adolescence demonstrate clearly that social factors probably operate in a cumulative fashion.20 Significant social class differences exist in attaining height and other aspects of physical development, as well as in incidence of infectious and other diseases, and risk of injury. In early life and childhood, primary prevention strategies include a healthy lifestyle and proper nutrition to build functional capacity to a maximum and adhering to vaccination schedules.
During adult life, and at older age, the goal is to maintain the highest possible level of functioning through continuing a healthy life-style with proper nutrition, physical and mental exercise, and preventive strategies to detect and treat any pathological processes early. With a better understanding of the biology of the ‘front end’ of chronic disease, the emphasis has shifted from the preventive care of women in their middle years21 to include that of younger women.22 Over time, ageing in health and with dignity through the practice of preventive ambulatory care will begin in infancy and, in the future, may start before conception.
Thus, the goal of preventive medicine is to keep the ageing population productive and as healthy as possible, hopefully reducing the length of time in which their health and functionality are compromised before death. The ultimate goal being ‘ageing in health and with dignity.’
Clinical consequences of an ageing world
Since now increased disability and sickness often accompany the last years of life, the demands for social and health services will increase immensely. The high cost of these services will strain the health, social and even political infrastructures of developing, and most developed and industrialised nations. Less developed countriesd—which have much lower levels of economic development and access to adequate health care than more developed countriesd—will be hard-pressed to meet the challenges of greater numbers of elderly people, especially as traditional family support systems for the elderly are deteriorating. Policymakers in the developing world need to invest soon in formal systems for old-age support to meet these challenges in the coming decades.
To the prudent healthcare administrators, establishing preventive measures rather than concentrating only on treatments is an important strategy in overall management of the ageing population. Frailty, disability and dependency will increase vastly the demand for social and health services. Crucial factors to significant reductions in health-service costs include maintaining health, permitting women and men to age gracefully, live independently, free of disability, for as long as possible. To achieve these objectives, a holistic approach to the management of ageing has to be taken.
The promotion of healthy ageing and prevention, or drastic reduction of morbidity and disability of elderly people must become central to the formulation of health and social policies. An all-encompassing lifelong approach to the ageing process beginning with pre-conceptual events and appropriate interventions at all stages of life should be emphasised.
The transformations in this century have led to increased medical needs of older people, who often have multiple chronic conditions, decrements in functional ability and age-related disease, but also to the increase of social expenditures, such as pension funds and health insurance to support them. The life course perspective enables the envisioning of important policy and strategy decisions.20
As morbidity and mortality in women (and men) often result from lifelong processes, a life-course perspective is a necessary framework when discussing the prevention and control of health problems of an ageing population. Primary prevention strategies promoting healthy lifestyles will be most effective if they are started early in life. Coronary heart disease, cerebrovascular disease, and lung cancer are good examples of common diseases in elderly people, for which primary prevention strategies are available, although not universally applied for a variety of reasons, including cost effectiveness and lack of perceived risk.
A complementary approach to improving the health of older men and women should focus on appropriate interventions at all stages of their lives. The determinants of ‘ageing’ and of ‘life expectancy’ extend from genetic and molecular determinants to the increasingly powerful forces of environmental, economical, technological and cultural globalisation. Specific measures for promoting healthy ageing should therefore include: (1) the promotion of a safe environment; (2) healthy lifestyle, including proper nutrition and avoidance of drug and alcohol abuses; (3) preventive strategies for cancers (e.g. lung cancer and chronic respiratory diseases, colorectal cancer, cervical cancer, breast cancer, endometrial cancer, and ovarian cancer); (4) preventive medical strategies to maintain quality of life and delay, decrease or prevent frailty and disabilities. These strategies include health care, improving social interactions to maintain good health, and preventing, identifying and managing chronic illnesses such as: cardiovascular diseases; subclinical hyperthyroidism; frailty; urinary tract infection and incontinence; and osteoporosis.
The promotion of a safe environment
A basic requirement of a supportive physical environment is the provision of a safe and accessible living environment. Falls are the most common, and preventable, threat to senior independence and also account for significant morbidity, including fracture, impaired mobility, depression, admission to long-term care facilities, decreased quality of life due to fear of falling, and death.23
As a person ages, they are more likely to have risk factors that contribute to falling, such as loss of vision, reduced fitness and muscle strength, osteoporosis, dementia, chronic health problems such as arthritis, as well as infections and other illnesses. Women are three times more likely to suffer from osteoporosis than men (17.6% v 5.2%). Osteoporosis significantly affects the pain and discomfort dimension of quality of life in women.24,25 As many as one in two postmenopausal women and one in five older men are at risk for an osteoporosis-related fracture. The 10-year fracture risk in a 65-year-old white woman without additional risk factors is 9.3%.26
Prescription drugs and too much alcohol are major risk factors for falling if they cause dizziness or affect alertness. Other contributing features include environmental factors like the presence of stairs or frailty due to factors like poor nutrition.
Healthy lifestyle, including proper nutrition and avoidance of drug and alcohol abuses
Two-third of adults27 and nearly one-third of children21 are overweight or obese in the USA, resulting in concurrent epidemics of diabetes and its complications, and other serious health conditions such as hypertension, hypercholesterolaemia, coronary heart disease, stroke, gallbladder disease, osteoarthritis, sleep apnoea, and respiratory problems, as well as contributing to the risk of endometrial, breast, and colon cancers.
A healthy lifestyle includes regular physical activity, balancing the number of calories one consumes with the number of calories one’s body uses through healthy eating, and avoiding drug and alcohol abuses. A healthy lifestyle is the best strategy to prevent obesity and its consequences. A recent critical review on the associations between the intake of vegetables and fruit, and the risk of several chronic diseases, shows that a high daily intake of these foods promotes health. Therefore, national campaigns to increase vegetable and fruit consumption are desirable strategies, which may decrease the burden of several chronic diseases in Western societies.28–30 Multi-component exercise programmes (usually focused on resistance, balance, aerobic, and flexibility training) have been shown to improve mobility,31 balance confidence,32 and lower blood lipid profiles.33 They also reduce fall risk and fall rate,34 improve quality of life,35 and can strengthen the cardio-vascular system as well muscles around joints. Improved fitness can help prevent injury and reduce the risk of falls, reduce wear and tear on joints, and help increase bone density.
Preventive strategies for cancers
Key cancer preventive strategies are to (1) reduce exposure to tobacco to the lung, oral cavity and pharynx to decrease respiratory cancers; (2) reduce salt intake and identify and treat Helicobacter pylori infections to decrease gastrointestinal cancers and heart disease36; (3) reduce food intake, improve diet and increase exercise to decrease colon-rectum, kidney, breast, ovary and endometrial cancer; (4) increase water intake, particularly to decrease urinary bladder cancer.37
Primary and secondary prevention
Primary prevention is aimed at reducing carcinogen activation, which leads to focal lesions and includes education about risk factors. Secondary prevention covers screening and early detection, along with education to help ensure that patients comply with screening guidelines and present for treatment as soon as symptoms develop. Screening for colorectal, breast, and cervical cancers, like that recommended by the US Preventive Services Task Force (USPSTF), can reduce morbidity and death through early detection and treatment of cancers and pre-cancers.38 Yet, many adults are not receiving regular, recommended, potentially life-saving screenings. Each year, about 350,000 people are diagnosed with, and nearly 100,000 die from, breast, cervical, or colorectal cancer in the USA.38
Lung cancer and chronic respiratory diseases
Cigarette smoking is the most common preventable cause of lung cancer, the leading cause of cancer death in both men and women in our society. Clinicians are uniquely positioned to affect smoking rates. In all countries, implementation of comprehensive tobacco control policies, including prohibition of cigarette advertising, tax increases and health promotion strategies, have the potential to reduce lung-cancer mortality. Anti-smoking policies may contribute to other health gains, including the prevention of chronic respiratory and cardiovascular disease.
Colorectal cancer
Primary prevention of colorectal cancer is accomplished by life-style factors, such as limiting obesity and excessive alcohol consumption. Dietary principles that decrease colorectal cancer risk entail increasing vegetables and fruit while reducing meat and refined carbohydrate consumption. An added benefit arises from ingesting olive oil and other unsaturated fats, common to the Mediterranean diet rather than using animal and saturated fats.39 Tobacco and dietary carcinogens may be secondary risk factors. Importantly, female hormone use decreases the relative risk to 0.82 (95% confidence interval 0.72 to 0.93) as shown by 11 case–control studies reporting information on oral contraceptives use and colorectal cancer risk.40
Colorectal cancer screening includes digital rectal examination, testing for occult blood, and colonoscopy, and is cost-effective compared with no screening. Digital rectal examination can detect up to one-third of cases, but fails to detect cancers above the palpated area. Testing stools for occult blood (iFOBT) detects about 17% of cases but is associated with false-positive results, thereby subjecting healthy individuals to additional diagnostic evaluation.41 Colonoscopy every 10 years offers better prevention against colorectal cancer than other screening methods. Screening people aged 50–60 years by iFOBT and people aged 60–72 years old with colonoscopies every 10 years is the most cost-effective strategy.42
Cervical cancer
Cervical cancer screening has begun to include human papillomavirus testing as a complement to cytology testing, as this testing has identified women at risk of developing cervical cancer.43 In recognition of new technologies and research on cervical cancer screening, the US Guidelines for the Prevention and Early Detection of Cervical Cancer now recommend that women aged 30–65 years may be screened every 5 years by co-testing with cervical cytology and high-risk human papillomavirus testing, and women aged 21–29 years may be screened with cervical cytology alone every 3 years.44 Vaccination against human papillomavirus in combination with triennial screening would be cost-effective, especially if vaccine cost is reduced.45
Breast cancer
Nulliparity, younger age of menarche, older age at menopause and late age at first birth and infertility are known potential risk factors for breast cancer.46 Pregnancy and breast feeding, combined with regular exercise, maintaining a healthy weight, and avoiding alcohol can help lower the risk.
The US Preventive Services Task Force recommends that women aged between 50 and 74 years be screened for breast cancer by mammography every 2 years. The adjunctive use of ultrasound may be useful in carefully, selected cases. Breast self-examination may be the most effective approach if only to improve awareness and early presentation at hospital when symptoms are detected. As our knowledge of genetic susceptibility improves, guidelines related to screening some subgroups of women such as those with BRCA1 or BRCA2, or those with ataxia-telangiectasis mutated gene have been developed.
Endometrial cancer
Early menarche, late menopause, nulliparity, obesity, increased body mass index, and unopposed oestrogen in anovulatory women (e.g. polycystic ovary syndrome) are all associated with developing endometrial cancer.47,48 Compared with the general population, the risk of endometrial cancer is increased nine-fold in infertile women with chronic anovulatory disorders.49,50 Long-term use of combined oral contraceptive use decreases the risk of endometrial cancer as does the use of oral progestins and progestin-releasing intrauterine devices.46 Progestins induce glandular epithelial secretory activity and decidual transformation of stromal fibroblasts in women with oestrogen-induced hyperplasia. Progestin-treated endometriums are terminally differentiated cells that can no longer proliferate and are shed in withdrawal bleeding. Thus, for women with endometrial cancer precursors, systemic or local progestin therapy is a commonly used alternative to hysterectomy, albeit unproven, which may be appropriate for women who want to retain fertility or are poor surgical candidates.51
Ovarian cancer
Nulliparity, and, for some women, genetic defects such as BRCA, are risk factors for epithelial ovarian cancer. ‘Incessant ovulation’ and associated alteration in endogenous hormones during reproductive years have been theorised as increasing ovarian cancer risk.52,53 Use of combined oral contraceptives has a significant protective effect on the ovarian cancer risk,54,55 by preventing ovulation and also in preventing retrograde menstruation.51 The protection increases with duration of use (relative risk decreased by 20% for each 5 years of use) and has been confirmed for BRCA1 and BRCA2 mutation carriers.56 The decreased risk is an important non-contraceptive benefit of oral contraception. Tubal ligation also decreases the risk of ovarian cancer.
Preventive medical strategies to maintain quality of life, and delay, decrease or prevent frailty and disabilities
Longevity has increased so rapidly during the last century that menopause is now a mid-life, rather than end-of-life event. Menopausal symptoms of hot flushes, night sweating, insomnia, panic attacks, depressive moods, and loss of libido significantly affect quality of life. Genitourinary symptoms developing early in the menopause transition add to a woman’s distress. An appropriately adjusted oestrogen regimen treats most menopausal symptoms, protects against osteoporosis and, when used in women younger than 60 years, may half the risk of both cardiovascular disease57,58 and cognitive impairment.59 In women with intact uteri, endometrial protection with progestogens is required. Women with oestrogen-sensitive cancers like endometrial or breast carcinoma or thromboembolic disorders may have significant increased health risk in the use of hormone replacement therapy.
The lowest effective oestrogen dose should be used to treat symptoms. Transdermal, ultralow dose administration may be considered if risk factors for venous thromboembolism exist. Additionally, different progestogens likely differ in their cardiovascular effects. Observational studies suggest that micronised progesterone or dydrogesterone may have a better risk profile than other progestogens for thrombotic risk.60
Medical health care, including the control of chronic illnesses and cardiovascular disease
A healthy life style, including limiting salt from processed foods, may be a cost-effective preventive measure to reduce cardiovascular disease, and thus will lead to improvements in population health,61 especially if begun early in life. Similarly, reducing high cholesterol levels to the normal range even in people who do not yet have cardiovascular disease has contributed most to the decline in coronary heart disease mortality in some European countries62 and in the USA. Consequently, reducing low-density lipoprotein cholesterol to reduce residual cardiovascular disease risk is the principal therapeutic target in lipid management.27 A recent practice guideline63 suggests the use of alternative biomarkers, such as non-high-density lipoprotein cholesterol (HDL) (total cholesterol minus HDL cholesterol) or Apo lipoprotein-B (apo B) to monitor the effects of lipid-lowering treatment. The additional monitoring of these biomarkers may be especially helpful in people who have low or moderate levels of low-density lipoprotein (LDL) cholesterol but also have other cardio-metabolic risk factors, particularly elevated triglycerides. Unlike LDL, measurement of non-HDL cholesterol and apo B does not require fasting overnight. In addition, both biomarkers are better predictors of cardiovascular disease risk than LDL cholesterol, especially in people treated with statins. Although hormone-replacement therapy has shown no protective effects in the presence of established atherosclerotic disease, it may have beneficial or neutral effects on healthy vasculature or early atherosclerosis. The cardiovascular effects of oestrogens in women who have not undergone a hysterectomy are influenced by the type, dosage, and route of administration of the concurrently administered progestin,64 and the time since menopause. Therefore, women receiving hormone replacement therapy early after menopause have a significantly reduced risk of mortality, heart failure, or myocardial infarction, without any apparent increase in risk of cancer, venous thromboembolism, or stroke after 10 years of treatment.58,65
Subclinical hyperthyroidism
Several changes in thyroid hormone secretion, metabolism, and action occur with increasing age. Ageing is associated with a decrease in serum thyroid stimulating hormone and T3 levels, whereas serum free T4 levels sometimes remain unchanged.66 The prevalence of thyroid dysfunction is higher in elderly people compared with younger people. It is thus warranted to check thyroid-stimulating hormone, T3 and T4 periodically. In elderly individuals, non-specific clinical manifestations of thyroid hormone excess or deprivation can confound clinical presentations67,68 Thyroid dysfunction is often asymptomatic, but carries a risk of long-term complications. For example, subclinical hyperthyroidism is associated with atrial fibrillation in people older than 60 years, in particular. The frequency in which subclinical hyperthyroidism progresses to overt thyrotoxicosis is uncertain, but it has been reported to range from 2–45% per year.69 The adverse effects of hyperthyroidism on the skeleton were first reported in 1891 when von Recklinghausen described the ‘worm eaten’ appearance of the long bones of a young woman who died from hyperthyroidism.67 Recent studies have suggested that subclinical hyperthyroidism and long-term suppressive doses of thyroxine (T4) used in treating hypothyroidism may result in decreased bone mineral density and an increased risk of fragility fracture, particularly in postmenopausal women.70
Frailty
Fried et al.71 described frailty as a state of global deficiency of physiological reserves and functional dysregulation involving multiple organ systems, resulting in poor homeostasis and increased vulnerability when faced with stressors. The frailty phenotype is a clinical syndrome characterised by shrinking (unintentional weight loss and sarcopaenia and muscle wasting), weakness, and exhaustion. Frailty and sarcopaenia are associated, but distinct, correlates of musculoskeletal ageing that have many causes, including age-related changes in body composition and inflammation.72 With advancing age, the risk of frailty increases, but not all elderly people become frail.73 In frail individuals, even minor negative events are likely to result in adverse outcomes such as falls, hospitalisation, disability and death.74
Several factors earlier in life may predict frailty and other co-morbidities. In a large prospective study, circulating levels of IL-6 greater than 2.5 pg/mL predicted future mobility disability (walking 1/2 mile or climbing stairs) in older adults who had no disability at baseline.75 As individuals age, continuing to exercise as well as engaging in social and cultural activity, may slow the development of frailty.
Urinary tract infection and incontinence
Urinary tract conditions can profoundly affect the quality of life of post-menopausal women. Urinary tract infection is the most common bacterial infection in women in general and in postmenopausal women in particular. Fifteen to 20% of women aged 65–70 years and 20–50% of women older than 80 years old have bacteriuria.76 Oestrogen deficiency may contribute to bacteriuria in postmenopausal women. Oestrogen stimulates the proliferation of lactobacillus on the vaginal epithelium, reduces pH, and limits vaginal colonisation with Enterobacteriaceae, which are the main pathogens of the urinary tract. Randomised-controlled trials confirm that oestrogen use in post-menopausal women decreases the rate recurrent urinary tract infections and urinary incontinence.77
Other effects of the decrease in oestrogen after the menopause include decreased vaginal muscle volume and slackness of the pelvic floor ligaments, resulting in genital and bladder prolapse. Pelvic floor muscle training and topical vaginal oestrogen preparations may reverse urogenital atrophic changes, relieving associated urinary symptoms while avoiding systemic oestrogenic and progestogenic effects.
Urinary incontinence has a negative effect on a woman’s sexual function. Among sexually active older women with urinary incontinence, 22% report being moderately or extremely worried that sexual activity would cause urine loss.76 Treatment of urinary incontinence can improve sexual function in older women. Among sexually active women (n = 53) who underwent mid-urethral slings procedures for the correction of urinary incontinence, increased coital frequency, decrease fear of incontinence with coitus, and decreased embarrassment due to incontinence was reported 6 months after surgery.78
Social interactions to maintain good mental health
Mental health plays a major role in women of any age. Depression is the most common mental health problem among older people, critically affecting their sense of well-being and quality of life. A critical aspect of care of any age, especially in elderly people, is distinguishing which women will benefit from behavioural and lifestyle changes from those who will benefit from pharmacological intervention.
Research has shown that both general practitioners and specialists lack training in mental and sexual assessments. For example, despite the known prevalence of sexual dysfunction among older women,79 few intervention studies have focused on this population. Often, medical professionals falsely assume that discussion of sexuality in older women with gynaecological pathology is unimportant or irrelevant.
Behavioural health specialists, such as psychologists, can play an integral role in facilitating open and genuine communication between the patient and the provider. Learning to ask open ended questions will help providers in these important assessments. Improved communication for patients includes helping them to discuss symptoms like sexuality about which they may be very anxious.
Osteoporosis
The World Health Organization identifies osteoporosis as one of the leading health problems in the Western world. Osteoporosis is common among all racial groups, is most common in white people and increases with age. Despite the availability of effective preventive treatments, osteoporosis is frequently underdiagnosed and undertreated, particularly among elderly people who are also at greatest risk. In addition, the presence of co-morbid medical conditions may be a barrier to osteoporosis care and a risk factor for falls; thus, individuals with multiple co-morbid conditions may be a particularly high-risk group.
The most serious consequence of this disorder is fractures, which have a serious negative effect on quality of life and are often the trigger for accelerated deterioration, ultimately ending in death. As many as one in two postmenopausal women and one in five older men are at risk for an osteoporosis-related fracture. An increased risk of fragility-related fracture is observed in more socially disadvantaged individuals in most western countries. Despite recent advances in osteoporosis care, additional action is urgently needed to improve the quality of life of people with osteoporosis in general and of elderly people, in particular, as fracture outcomes are typically poorer in older than in younger people.80
Dual-energy X-ray absorptiometry is currently the procedure of choice to diagnose osteoporosis and assess fracture risk.81 Recent evidence suggests that optimal intervals for rescreening to detect osteoporosis in older, postmenopausal women with normal bone density or mild osteopaenia is 15 years, 5 years for those with moderate osteopaenia, and 1 year for women with advanced osteopaenia.82
The management of osteoporosis involves improving bone health via adequate nutrition, weight-bearing exercise, calcium and vitamin D supplements, and fall prevention strategies. Data from large cohort studies clearly indicate that serum 25-(OH)D concentrations around 50 nmol/l are sufficient to minimise the risk of osteoporotic fractures, colorectal and breast cancer, and cardiovascular mortality. The fact that the risk-reducing potential of vitamin D depends on adequate calcium intake and absorption is widely ignored.83
Although these measures are important in the management of all patients, most elderly people are likely to need additional pharmacological treatment to adequately reduce their fracture risk. Several pharmacological treatments have been shown to reduce the risk of fracture significantly, including bisphosphonates (e.g. alendronate, risedronate, ibandronate, zoledronic acid), denosumab, raloxifene, calcitonin and teriparatide. Hormone replacement therapy still constitutes a first-line choice for prevention of bone loss and fracture in the early postmenopausal period for up to 5 years. The fear of long-term side effects of hormone-replacement therapy, such as breast cancer, coronary heart disease and thromboembolic events has increased the demand to evaluate the role of alternative osteoporosis and fracture-prevention medications in ageing women.
In some women with low risk of breast cancer and cardiovascular disease, hormone-replacemenet therapy can be continued. Some propose that limiting systemic progestin while protecting the endometrium, such as using a progestogen intrauterine device in combination with transdermal oestrogen, may be the best alternative for long-term treatment.84 This combination minimises cardiovascular risk by avoiding the first-pass metabolism in the liver from oral compounds and minimises exposure to progestogens. Since the publication of the Women’s Health Initiative in 2002, the rapid worldwide decrease of use may result in an increased incidence of fractures. Women who discontinue hormone-replacement therapy should be advised about rapid bone loss after hormone replacement therapy, and given other potential treatment options.85
Selective oestrogen receptor modulators are valuable alternatives, particularly in women with osteopaenia (t-score −1.0 to −2.5) at increased risk of breast cancer, but their general lack of anti-fracture efficacy towards non-vertebral fractures limits their use in women at high risk of osteoporotic fracture.77
Conclusion
A better understanding of molecular mechanisms of ageing, embedded in a translational matrix of gerontology and geriatric medicine, will enable the development of new clinical strategies to prevent and manage age-associated dysfunctions and diseases. Moreover, placing greater emphasis and increasing research on public health issues, including health-promotion strategies, prevention of disease, disability and frailty, and improving quality of life, quality of care, healthcare organisation and health economy aspects, will allow better translation of basic and clinical research findings into everyday practice. A new focus on ageing will necessitate a quantum leap in multi-disciplinary and internationally co-ordinated research efforts, supported by a new partnership between industry and governments, philanthropic and international organisations. It is essential to prepare healthcare providers and societies to meet the needs of older populations. This includes training for health professionals on old-age care, preventing and managing age-associated chronic diseases, designing sustainable policies on long-term and palliative care, and developing age-friendly services and settings. Effective implementation of primary and secondary prevention measures will increase length of productive life of ageing populations, decrease dependency, and ultimately decrease health costs. With an enriched understanding of health and ageing, we can improve the quality of life, prevent the preventable, and postpone and decrease the pain and suffering of the inevitable.
Practice points.
An all-encompassing lifelong pursuit of preventive measures and interventions improves healthy ageing compared with concentrating only on treatments.
Effective implementation of primary and secondary prevention measures will increase length of productive life of ageing populations, decrease dependency, and ultimately decrease health costs.
A healthy life-style with proper nutrition, physical, and mental exercise is the key primary preventive measure to healthy ageing.
Research agenda.
Delineate molecular mechanisms of ageing to develop new clinical strategies to prevent and manage age-associated dysfunctions and diseases.
Effect of health-promotion strategies in preventing disease, disability and frailty of ageing.
Effect of cost-effective laboratory exams and screening methods on early detection and treatment of common aspects of ageing.
Acknowledgement
This work was supported in part by the Intramural Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the NIH Clinical Center. We thank Nancy Terry, MLS, informationist at the NIH Clinical Center for her assistance in formatting the references for publication.
References
- 1.Lunenfeld B. Hormone replacement therapy in the aging male: editorial. Aging Male. 1999;2:1–5. [Google Scholar]
- 2.United Nations Department of Economic and Social Affairs Population Division. World population prospects: the 2004 revision. New York: United Nations; 2005. [accessed 10.02.13]. http://www.un.org/esa/population/publications/WPP2004/2004Highlights_finalrevised.pdf. [Google Scholar]
- 3.Population Reference Bureau. Population reference bureau. Washington, DC: Population Reference Bureau; 2012. [accessed 10.02.13]. http://www.prb.org/ [Google Scholar]
- 4.Harper S. Environment, migration and the European demographic deficit. Environ Res Lett. 2012;7:015605. [Google Scholar]
- 5.Hoorens S, Clift J, Staetsky L, et al. Low fertility in Europe: is there still reason to worry? Cambridge: Rand Europe; 2011. [accessed 10.02.13]. http://www.rand.org/content/dam/rand/pubs/monographs/2011/RAND_MG1080.pdf. [Google Scholar]
- 6.World Bank. [accessed 10.02.2013];World development indicators. 2012 http://data.worldbank.org/data-catalog/world-development-indicators.
- 7.Japanese Government Ministry of Health Labour and Welfare Minister’s Secretariat Statistics and Information Department. Abridged life tables for Japan 2009. Tokyo: Japanese Government Statistics and Information Department; 2009. [accessed 10.02.13]. http://www.mhlw.go.jp/english/database/db-hw/lifetb09/dl/contents.pdf. [Google Scholar]
- 8.Fries JF, Nesse RM, Schneider EL, et al. Aging, natural death, and the compression of morbidity. N Engl J Med. 1984;310:659–660. [PubMed] [Google Scholar]
- 9.Myers G, Manton K. The rate of population aging: new views of epidemiologic transitions. In: Maddox G, Busse E, editors. Aging the universal human experience. New York: Springer; 1987. pp. 263–283. [Google Scholar]
- 10.Christensen K, Doblhammer G, Rau R, et al. Ageing populations: the challenges ahead. Lancet. 2009;374:1196–1208. doi: 10.1016/S0140-6736(09)61460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organisation. World Health Statistics 2012. Geneva: WHO Press; 2012. [Google Scholar]
- 12.United Nations Department of Economic and Social Affairs Population Division. World population prospects: the 2008 revision highlights. New York: United Nations; 2009. [accessed 10.02.13]. http://www.un.org/esa/population/publications/wpp2008/wpp2008_highlights.pdf. [Google Scholar]
- 13.Verbrugge LM, Jette AM. The disablement process. Soc Sci Med. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- 14.Jeune B, Brønnum-Hansen H. Trends in health expectancy at age 65 for various health indicators, 1987–2005, Denmark. Eur J Ageing. 2008;5:279–285. doi: 10.1007/s10433-008-0100-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Freedman VA, Martin LG. Contribution of chronic conditions to aggregate changes in old-age functioning. Am J Public Health. 2000;90:1755–1760. doi: 10.2105/ajph.90.11.1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lafortune G, Balestat G. Trends in severe disability among elderly people: assessing the evidence in 12 OECD countries and future implications. Paris: Organization for Economic Co-operation and Development; 2007. [accessed 10.02.13]. http://www.oecd.org/social/socialpoliciesanddata/38343783.pdf. [Google Scholar]
- 17.Diczfalusy E. An aging humankind: is our future behind us? Aging Male. 1998;1:8–19. [Google Scholar]
- 18.Wilkins R, Adams OB. Health expectancy in Canada, late 1970s: demographic, regional, and social dimensions. Am J Public Health. 1983;73:1073–1080. doi: 10.2105/ajph.73.9.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bodenheimer T, Starfield B, Treadway K, et al. The future of primary care: the community responds. N Engl J Med. 2008;359:2636–2639. doi: 10.1056/NEJMp0809792. [DOI] [PubMed] [Google Scholar]
- 20.Kalache A, Lunenfeld B. Health and the ageing male. Aging Male. 2000;3:1–2. [Google Scholar]
- 21.Noteloviz M. The adult women’s plan. In: Schneider HPG, editor. Menopause: the state of the art in research and management. Boca Raton, London and Washington DC: Parthenon Publishing Group; 2003. pp. 502–507. [Google Scholar]
- 22.Notelovitz M. Optimizing women’s health: adult women’s health and medicine. Climacteric. 2005;8:205–209. doi: 10.1080/13697130500190893. [DOI] [PubMed] [Google Scholar]
- 23.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337:1279–1284. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 24.Bianchi ML, Orsini MR, Saraifoger S, et al. Quality of life in post-menopausal osteoporosis. Health Qual Life Outcomes. 2005;3:78. doi: 10.1186/1477-7525-3-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cockerill W, Lunt M, Silman AJ, et al. Health-related quality of life and radiographic vertebral fracture. Osteoporos Int. 2004;15:113–119. doi: 10.1007/s00198-003-1547-4. [DOI] [PubMed] [Google Scholar]
- 26.Kanis JA, Johnell O, Oden A, et al. FRAX™ and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19:385–397. doi: 10.1007/s00198-007-0543-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Panel AP. Reducing residual cardiovascular risk: the relevance of raising high-density lipoprotein cholesterol in patients on cholesterol-lowering treatment. Diab Vasc Dis Res. 2006;3:S1–S12. doi: 10.3132/dvdr.2006.011. [DOI] [PubMed] [Google Scholar]
- 28.Boeing H, Bechthold A, Bub A, et al. Critical review: vegetables and fruit in the prevention of chronic diseases. Eur J Nutr. 2012;51:637–663. doi: 10.1007/s00394-012-0380-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Strandberg TE, Sirola J, Pitkälä KH, et al. Association of midlife obesity and cardiovascular risk with old age frailty: a 26-year follow-up of initially healthy men. Int J Obes. 2012;36:1153–1157. doi: 10.1038/ijo.2012.83. [DOI] [PubMed] [Google Scholar]
- 30.Steib S, Schoene D, Pfeifer K. Dose-response relationship of resistance training in older adults: a meta-analysis. Med Sci Sports Exerc. 2010;42:902–914. doi: 10.1249/MSS.0b013e3181c34465. [DOI] [PubMed] [Google Scholar]
- 31.Pahor M, Blair SN, Espeland M, et al. Effects of a physical activity intervention on measures of physical performance: results of the lifestyle interventions and independence for elders pilot (LIFE-P) study. J Gerontol A Biol Sci Med Sci. 2006;61:1157–1165. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- 32.Büla CJ, Monod S, Hoskovec C, et al. Interventions aiming at balance confidence improvement in older adults: an updated review. Gerontology. 2011;57:276–286. doi: 10.1159/000322241. [DOI] [PubMed] [Google Scholar]
- 33.Carvalho J, Marques E, Ascensão A, et al. Multicomponent exercise program improves blood lipid profile and antioxidant capacity in older women. Arch Gerontol Geriatr. 2010;51:1–5. doi: 10.1016/j.archger.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 34.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2009;2:CD007146. doi: 10.1002/14651858.CD007146.pub2. [DOI] [PubMed] [Google Scholar]
- 35.Justine M, Hamid TA, Kamalden TFT, et al. A multicomponent exercise program’s effects on health-related quality of life of institutionalized elderly. Topic Geriatr Rehab. 2010;26:70–79. [Google Scholar]
- 36.Fock KM, Talley N, Moayyedi P, et al. Asia-Pacific consensus guidelines on gastric cancer prevention. J Gastroenterol Hepatol. 2008;23:351–365. doi: 10.1111/j.1440-1746.2008.05314.x. [DOI] [PubMed] [Google Scholar]
- 37.Moore MA, Sobue T. Strategies for cancer control on an organ-site basis. Asian Pac J Cancer Prev APJCP. 2010;11(Suppl. 2):149–164. [PubMed] [Google Scholar]
- 38.Klabunde CN, Brown M, Ballard-Barbash R, et al. Cancer screening - United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:41–45. [PubMed] [Google Scholar]
- 39.Gallus S, Bosetti C, La Vecchia C. Mediterranean diet and cancer risk. Eur J Cancer Prev. 2004;13:447–452. doi: 10.1097/00008469-200410000-00013. [DOI] [PubMed] [Google Scholar]
- 40.Bosetti C, Bravi F, Negri E, et al. Oral contraceptives and colorectal cancer risk: a systematic review and meta-analysis. Hum Reprod Update. 2009;15:489–498. doi: 10.1093/humupd/dmp017. [DOI] [PubMed] [Google Scholar]
- 41.Shike M, Winawer SJ, Greenwald PH, et al. Primary prevention of colorectal cancer. Bull World Health Org. 1990;68:377–385. [PMC free article] [PubMed] [Google Scholar]
- 42.Dan YY, Chuah BYS, Koh DCS, et al. Screening based on risk for colorectal cancer is the most cost-effective approach. Clin Gastroenterol Hepatol. 2012;10:266–271. doi: 10.1016/j.cgh.2011.11.011. [DOI] [PubMed] [Google Scholar]
- 43.Sankaranarayanan R, Nene BM, Shastri SS, et al. HPV screening for cervical cancer in rural India. N Engl J Med. 2009;360:1385–1394. doi: 10.1056/NEJMoa0808516. [DOI] [PubMed] [Google Scholar]
- 44.Chelmow D, Waxman A, Cain JM, et al. The evolution of cervical screening and the specialty of obstetrics and gynecology. Obstet Gynecol. 2012;119:695–699. doi: 10.1097/AOG.0b013e31824b2ed8. [DOI] [PubMed] [Google Scholar]
- 45.Chen MK, Hung HF, Duffy S, et al. Cost-effectiveness analysis for Pap smear screening and human papillomavirus DNA testing and vaccination. J Eval Clin Pract. 2011;17:1050–1058. doi: 10.1111/j.1365-2753.2010.01453.x. [DOI] [PubMed] [Google Scholar]
- 46.Lee E, Ma H, McKean-Cowdin R, et al. Effect of reproductive factors and oral contraceptives on breast cancer risk in BRCA1/ 2 mutation carriers and noncarriers: results from a population-based study. Cancer Epidemiol Biomarkers Prev. 2008;17:3170–3178. doi: 10.1158/1055-9965.EPI-08-0396. [DOI] [PubMed] [Google Scholar]
- 47.Cetin I, Cozzi V, Antonazzo P. Infertility as a cancer risk factor: a review. Placenta. 2008;29:169–177. doi: 10.1016/j.placenta.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 48.Cramer DW. The epidemiology of endometrial and ovarian cancer. Hematol Oncol Clin North Am. 2012;26:1–12. doi: 10.1016/j.hoc.2011.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ron E, Lunenfeld B, Menczer J. Cancer incidence in a cohort of infertile women. Am J Epidemiol. 1987;125:780–790. doi: 10.1093/oxfordjournals.aje.a114595. [DOI] [PubMed] [Google Scholar]
- 50.Modan B, Ron E, Lerner-Geva L, et al. Cancer incidence in a cohort of infertile women. Am J Epidemiol. 1998;147:1038–1042. doi: 10.1093/oxfordjournals.aje.a009397. [DOI] [PubMed] [Google Scholar]
- 51.Trimble CL, Method M, Leitao M, et al. Management of endometrial precancers. Obstet Gynecol. 1971;120:1160–1175. doi: 10.1097/aog.0b013e31826bb121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fathalla MF, et al. Incessant ovulation: a factor in ovarian neoplasia? Lancet. 1971;2:163. doi: 10.1016/s0140-6736(71)92335-x. [DOI] [PubMed] [Google Scholar]
- 53.Cramer DW, Hutchison GB, Welch WR. Determinants of ovarian cancer risk. I. reproductive experiences and family history. J Natl Cancer Inst. 1983;71:711–716. [PubMed] [Google Scholar]
- 54.Winer E, Gralow J, Diller L, et al. Clinical cancer advances 2008: major research advances in cancer treatment, prevention, and screening: a report from the American Society of Clinical Oncology. J Clin Oncol. 2009;27:812–826. doi: 10.1200/JCO.2008.21.2134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Beral V, Doll R, Hermon C, et al. Ovarian cancer and oral contraceptives: collaborative reanalysis of data from 45 epide-miological studies including 23,257 women with ovarian cancer and 87,303 controls. Lancet. 2008;371:303–314. doi: 10.1016/S0140-6736(08)60167-1. [DOI] [PubMed] [Google Scholar]
- 56.Cibula D, Gompel A, Mueck AO, et al. Hormonal contraception and risk of cancer. Hum Reprod Update. 2010;16:631–650. doi: 10.1093/humupd/dmq022. [DOI] [PubMed] [Google Scholar]
- 57.Hsia J, Langer RD, Manson JE, et al. Conjugated equine estrogens and coronary heart disease: the women’s health initiative. Arch Intern Med. 2006;166:357–365. doi: 10.1001/archinte.166.3.357. [DOI] [PubMed] [Google Scholar]
- 58.Schierbeck LL, Rejnmark L, Tofteng CL, et al. Effect of hormone replacement therapy on cardiovascular events in recently postmenopausal women: randomised trial. BMJ. 2012;345:e6409. doi: 10.1136/bmj.e6409. http://dx.doi.org/10.1136/bmj.e6409. [DOI] [PubMed] [Google Scholar]
- 59.Zandi PP, Carlson MC, Plassman BL, et al. Hormone replacement therapy and incidence of Alzheimer disease in older women: the Cache County Study. JAMA. 2002;288:2123–2129. doi: 10.1001/jama.288.17.2123. [DOI] [PubMed] [Google Scholar]
- 60.Schenck-Gustafsson K, Brincat M, Erel CT, et al. EMAS position statement: managing the menopause in the context of coronary heart disease. Maturitas. 2011;68:94–97. doi: 10.1016/j.maturitas.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 61.Cobiac LJ, Magnus A, Lim S, et al. Which interventions offer best value for money in primary prevention of cardiovascular disease? PLoS One. 2012;7:e41842. doi: 10.1371/journal.pone.0041842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Palmieri L, Bennett K, Giampaoll S, et al. Explaining the decrease in coronary heart disease mortality in Italy between 1980 and 2000. Am J Public Health. 2010;100:684–692. doi: 10.2105/AJPH.2008.147173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Smith SC, Jr, Benjamin EJ, Bonow RO, Jr, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update. J Am Coll Cardiol. 2011;58:2432–2446. doi: 10.1016/j.jacc.2011.10.824. [DOI] [PubMed] [Google Scholar]
- 64.Rosano G, Vitale C, Spoletini I, et al. Cardiovascular health in the menopausal woman: impact of the timing of hormone replacement therapy. Climacteric. 2012;15:299–305. doi: 10.3109/13697137.2012.658899. [DOI] [PubMed] [Google Scholar]
- 65.Salpeter SR, Cheng J, Thabane L, et al. Bayesian meta-analysis of hormone therapy and mortality in younger post-menopausal women. Am J Med. 2009;122:1016–1022. doi: 10.1016/j.amjmed.2009.05.021. e1. [DOI] [PubMed] [Google Scholar]
- 66.Mariotti S, Barbesino G, Caturegli P, et al. Complex alteration of thyroid function in healthy centenarians. J Clin Endocrinol Metab. 1993;77:1130–1134. doi: 10.1210/jcem.77.5.8077303. [DOI] [PubMed] [Google Scholar]
- 67.Mitrou P, Raptis SA, Dimitriadis G. Thyroid disease in older people. Maturitas. 2011;70:5–9. doi: 10.1016/j.maturitas.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 68.Nanchen D, Gussekloo J, Westendorp RGJ, et al. Subclinical thyroid dysfunction and the risk of heart failure in older persons at high cardiovascular risk. J Clin Endocrinol Metab. 2012;97:852–861. doi: 10.1210/jc.2011-1978. [DOI] [PubMed] [Google Scholar]
- 69.Tenerz A, Forberg R, Jansson R. Is a more active attitude warranted in patients with subclinical thyrotoxicosis? J Intern Med. 1990;228:229–233. doi: 10.1111/j.1365-2796.1990.tb00223.x. [DOI] [PubMed] [Google Scholar]
- 70.Nicholls JJ, Brassill MJ, Williams GR, et al. The skeletal consequences of thyrotoxicosis. J Endocrinol. 2012;213:209–221. doi: 10.1530/JOE-12-0059. [DOI] [PubMed] [Google Scholar]
- 71.Fried LP, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59:255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 72.Lowry KA, Vallejo AN, Studenski SA. Successful aging as a continuum of functional independence: lessons from physical disability models of aging. Aging Dis. 2012;3:5–15. [PMC free article] [PubMed] [Google Scholar]
- 73.Ahmed N, Mandel R, Fain MJ. Frailty: an emerging geriatric syndrome. Am J Med. 2007;120:748–753. doi: 10.1016/j.amjmed.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 74.Rockwood K, Hogan DB, MacKnight C. Conceptualisation and measurement of frailty in elderly people. Drugs Aging. 2000;17:295–302. doi: 10.2165/00002512-200017040-00005. [DOI] [PubMed] [Google Scholar]
- 75.Ferrucci L, Harris TB, Guralnik JM, et al. Serum IL-6 level and the development of disability in older persons. J Am Geriatr Soc. 1999;47:639–646. doi: 10.1111/j.1532-5415.1999.tb01583.x. [DOI] [PubMed] [Google Scholar]
- 76.Raz R. Urinary tract infection in postmenopausal women. Korean J Urol. 2011;52:801–808. doi: 10.4111/kju.2011.52.12.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Koski ME, Chermansky CJ. Does estrogen have any real effect on voiding dysfunction in women? Curr Urol Rep. 2011;12:345–350. doi: 10.1007/s11934-011-0208-y. [DOI] [PubMed] [Google Scholar]
- 78.Ratner ES, Erekson EA, Minkin MJ, et al. Sexual satisfaction in the elderly female population: a special focus on women with gynecologic pathology. Maturitas. 2011;70:210–215. doi: 10.1016/j.maturitas.2011.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Figueroa JR, Jara AD, Fuenzalida PA, et al. Prevalence of sexual dysfunction among climacteric women. Rev Med Chil. 2009;137:345–350. [in Spanish] [PubMed] [Google Scholar]
- 80.Curtis JR, Safford MM. Management of osteoporosis among the elderly with other chronic medical conditions. Drugs Aging. 2012;29:549–564. doi: 10.2165/11599620-000000000-00000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Brennan SL, Wluka AE, Gould H, et al. Social determinants of bone densitometry uptake for osteoporosis risk in patients aged 50 years and older: a systematic review. J Clin Densitom. 2012;15:165–175. doi: 10.1016/j.jocd.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 82.Gourlay ML, Fine JP, Preisser JS, et al. Bone-density testing interval and transition to osteoporosis in older women. N Engl J Med. 2012;366:225–233. doi: 10.1056/NEJMoa1107142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Peterlik M. Vitamin D insufficiency and chronic diseases: hype and reality. Food Funct. 2012;3:784–794. doi: 10.1039/c2fo10262e. [DOI] [PubMed] [Google Scholar]
- 84.Eriksen EF. Hormone replacement therapy or SERMS in the long term treatment of osteoporosis. Minerva Ginecol. 2012;64:207–221. [PubMed] [Google Scholar]
- 85.Tuppurainen M. HT and SERMs in the long-term management of osteoporosis. Minerva Ginecol. 2012;64:195–205. [PubMed] [Google Scholar]