Abstract
Aims
To compile and analyze critically the literature published on street children and substance use in resource-constrained settings.
Methods
We searched the literature systematically and used meta-analytical procedures to synthesize literature that met the review’s inclusion criteria. Pooled-prevalence estimates and 95% confidence intervals (CI) were calculated using the random-effects model for life-time substance use by geographical region as well as by type of substance used.
Results
Fifty studies from 22 countries were included into the review. Meta-analysis of combined life-time substance use from 27 studies yielded an overall drug use pooled-prevalence estimate of 60% (95% CI = 51–69%). Studies from 14 countries contributed to an overall pooled prevalence for street children’s reported inhalant use of 47% (95% CI = 36–58%). This review reveals significant gaps in the literature, including a dearth of data on physical and mental health outcomes, HIV and mortality in association with street children’s substance use.
Conclusions
Street children from resource-constrained settings reported high life-time substance use. Inhalants are the predominant substances used, followed by tobacco, alcohol and marijuana.
Keywords: Homeless youth, resource-constrained settings, street children, substance use, systematic review, volatile solvent use
INTRODUCTION
Streets throughout the world are home to millions of children [1] who endure hardships and injustices while struggling to survive. The United Nations Children’s Fund (UNICEF) defines children living and working on the street in three categories: ‘children of the street’, ‘children on the street’ and ‘children from street families’ [2]. Children on the street spend a proportion of their time on the street, working to provide an economic contribution to their family, but often return home at night, maintaining familial ties. Children of the street both work and sleep on the streets and have an absence of regular contact with family members. Children from street families live with their families in the street [2].
Although street-involved children and youth (SICY) are a world-wide phenomenon, the dynamics that drive children to the streets are quite diverse and vary between high-income and low- to middle-income countries [3]. While youth in developed countries usually become street-involved due to familial conflict and child abuse [4], children in resource-constrained settings (RCS) succumb to street life due to abject poverty, child abuse, neglect, familial dysfunction, death of one or both parents, war and socio-cultural and religious beliefs [5–9]. Additionally, the substance use habits adopted by SICY in RCS are often divergent from those of their counterparts in high-income countries [10]. Youth in street circumstances in high-income settings engage in using injection drugs and other substances that are not used commonly among children and youth on the streets in RCS [10–12].
Research on street children and their substance use habits in RCS has been limited largely to describing the prevalence and types of substances used. The prevalence estimates within the literature are inconsistent and often very divergent within countries and geographical regions. Despite studies reporting prevalence within specific locations, there are no pooled data available on the prevalence and types of substances used by geographical region, the characteristics associated with street children’s substance use and reasons for use. However, substance use and misuse poses a serious threat to the short- and long-term health and wellbeing of millions of children around the world and greatly affects their potential for re-integration into communities and society. There is an urgent need to compile objective information about the epidemiology of substance use among street children in RCS and to understand the magnitude of the problem. This will inform rehabilitation and other programs designed for reintegrating children into communities. This systematic review and meta-analysis seeks to compile and analyze critically the literature published on SICY and substance use in RCS. It aims to describe the epidemiology of substance use using meta-analytical techniques, while identifying gaps in knowledge, evaluating the strength of existing evidence and identifying research needs.
METHODS
Search strategy
We searched electronic databases systematically, including SCOPUS, MEDLINE, EMBASE, Social Sciences Abstract and PsycINFO for English-language published literature and abstracts from inception to August 2011. We searched Google Scholar to identify any additional relevant documents and papers. We used the following search strategy: (‘street children’ OR ‘street youth’ OR ‘homeless youth’ OR ‘homeless children’ OR ‘runaway children’ OR ‘runaway youth’) AND (‘substance use’ OR ‘substance misuse’ OR ‘substance abuse’ OR ‘drug use’ OR ‘drug misuse’ OR ‘drug abuse’ OR ‘inhalants’ OR ‘solvents’). We hand-searched the bibliographies of full texts assessed for eligibility to identify additional relevant papers. We included our own data that were unpublished at the time of the search [13]. When more than one study reported on the same sample of SICY, the source containing the most detailed data about the prevalence of drug use was selected for the review. One author (L.E.) reviewed all the titles returned and identified eligible studies based on the review’s inclusion and exclusion criteria. We were unable to locate the full text of two papers identified through hand-searching bibliographies [14,15], and were unable to assess their eligibility for inclusion in the review.
Definitions
For the purposes of this review, ‘street-involved children and youth’ refers to any child (aged 0–18 years) or youth (aged 15–24 years) who spends a portion or majority of their time on the streets. These children and youth may have been defined in the literature as ‘children on the street’, ‘children of the street’, street children, working children, parking boys or market children. We utilized the Human Development Index (HDI) for restricting our review to resource-constrained countries. The HDI uses a combination of indicators to measure development and categorizes countries into very high, high, medium and low groups [16]. We defined RCS as all those in the high, medium and low rankings on the 2010 HDI [17], excluding all those in the very high category. Developed countries are those in the top quartile and classified as very high; all others are considered developing [17]. We defined life-time drug use as having ever used a substance (even once) and current drug use as drug use within the past 30 days. When a study reported any overall prevalence without defining life-time or current use, for the purposes of the meta-analysis we categorized it as lifetime use.
Inclusion and exclusion criteria
Studies were included if they met the following inclusion criteria: (i) they contained prevalence data on SICY’s substance use in RCS. Studies were required to have data pertaining to prevalence of one or more of the following: life-time drug use, current drug use, inhalants, alcohol, tobacco, marijuana, cocaine or other psychoactive substances; (ii) participants were aged 0–24 years and met our definition of SICY; (iii) the study occurred in an RCS meeting our definition; and (iv) the study was published in English. We included the following study designs: cross-sectional, cohort, case–control, mixed-methods and interventions with baseline data. We excluded studies that did not have prevalence data and dissertations.
Data extraction
A review protocol was drafted, edited and agreed upon by the authors of this review before commencement. Data were extracted from full texts by one author (L.E.) and included details about study design, sample size, study location, sampling location, population demographics and results for all substance use variables of interest. When it was not possible to extract data, we contacted the authors for clarification or to provide data. Of note, for four studies we were unable to extract data for pooled-prevalence estimates [6,18–20].
Data analysis
There lacks a gold standard tool for assessing the quality of observational studies [21]. We sought to assess how studies defined substance use, street children, their sampling and analysis methods and use of validated tools. The assessment was used to establish the quality of studies in this research domain and to identify gaps in the literature; it did not factor into whether or not studies were included in the review or in the meta-analyses.
We performed a meta-analysis to estimate the pooled-prevalence estimates of life-time drug use by geographical region as well as drug use by type of substance. Life-time or current drug use prevalence for specific substances (inhalants, alcohol, tobacco, marijuana and cocaine) was used to perform the meta-analysis by type of drug. When a study reported both life-time and current prevalence for the substance of interest, the life-time use estimate was selected for inclusion in the meta-analysis.
We calculated the pooled-prevalence estimates using a robust random-effects model (i.e. the DerSimonian–Laird method) [22]. In contrast to the more restrictive fixed-effect model (i.e. the Mantel–Haenszel method) [23], this model allows for samples to have been drawn from populations that might differ systematically from one another (heterogeneity). It therefore allows for the prevalence estimates resulting from included studies to differ not only because of the random error within studies (as in the fixed-effects model), but also because of true variation from one study to the next.
The quantity I2, which describes the percentage of variation attributable to heterogeneity, was also calculated. We performed subgroup analyses by geographical region and type of substance. In all the analyses, two-tailed tests were used and a probability level less than 0.05 was considered significant. A sensitivity analysis was performed on the geographical data to test whether one country had an undue influence on the meta-analysis in each of the geographical categories. Analysis was performed using STATA version 10 (Stata Corporation, College Station, TX, USA) software.
RESULTS
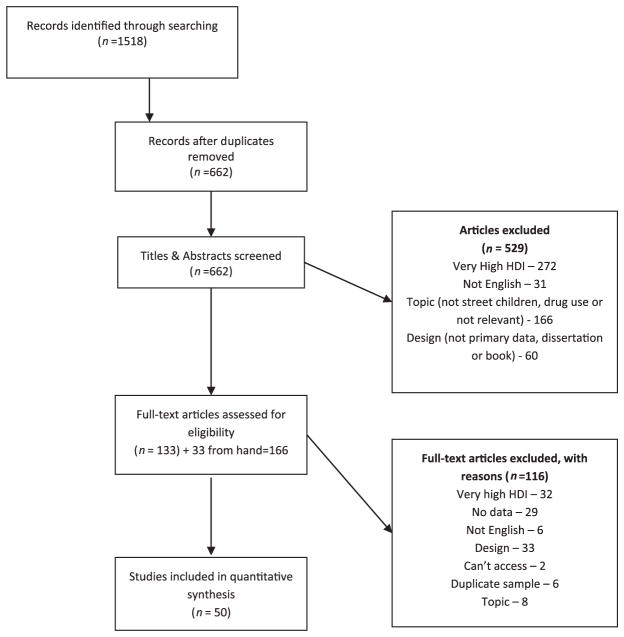
Our search identified 1518 publications (Fig. 1). After removal of duplicates and application of exclusion criteria 133 papers remained for full review, with an additional 33 papers identified through hand-searching bibliographies. There were therefore 166 full texts reviewed, with 50 included in the final review. Characteristics of the studies identified are presented in Table 1, which also contains a study number (used to refer to individual studies in the Tables) and reference number (used to refer to individual studies in the text). The 50 studies included for review consisted of 16 987 participants in total, of whom 75% were males, 21% were females and the gender of the remaining 4% was unknown due to non-reporting.
Figure 1.
Flow diagram of study selection
Table 1.
Characteristics of the 50 studies identified for review.
| Study no. | First author [reference no.] | Year | Country | Study design | N | Male n (%) | Female n (%) | OF the streetd n (%) | ON the street n (%) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Abdulmalik [24] | 2009 | Nigeria | Cross-sectional | 340 | 340 (100) | 0 (0) | .(.) | .(.) |
| 2 | Abou-Hatab [25] | 2010 | Egypt | Conference abstracts | 100 | . (.) | . (.) | .(.) | . (.) |
| 3 | Adebiyi [26] | 2008 | Nigeria | Cross-sectional | 360 | 210 (58) | 150 (42) | 51 (14)A,C | 309 (86) |
| 4 | Aidan [27] | 1997 | Zambia | Cross-sectional | 100 | 70 (70) | 30 (30) | 26 (26)C | 74 (74) |
| 5 | Ayayab [6] | 2001 | Kenya | Cross-sectional | 141a | . (.) | . (.) | 47 (33)A | 38 (27) |
| 6 | Elkoussi [28] | 2011 | Egypt | Cross-sectional | 120 | 117 (98) | 3 (3) | .(.) | .(.) |
| 7 | Embleton [13] | 2012 | Kenya | Cross-sectional | 146 | 114 (78) | 32 (22) | 98 (67)A,B | 48 (33) |
| 8 | Kayembe [29] | 2008 | DRC* | Cross-sectional | 880 | 692 (79) | 188 (21) | 880 (100)C | 0 (0) |
| 9 | Kudrati [30] | 2008 | Sudan | Mixed-methods | 432 | 397 (92) | 35 (8) | 330 (76)C | 102 (24) |
| 10 | Morakinyo [8] | 2003 | Nigeria | Cross-sectional | 180 | 174 (97) | 6 (3) | .(.) | .(.) |
| 11 | Nada [31] | 2010 | Egypt | Cross-sectional | 857 | 727 (85) | 130 (15) | .(.) | .(.) |
| 12 | Nzimakwe [32] | 1994 | South Africa | Cross-sectional | 50 | 40 (80) | 10 (20) | .(.) | .(.) |
| 13 | Okwaraji [33] | 1996 | Nigeria | Cross-sectional | 100 | 60 (60) | 40 (40) | .(.) | .(.) |
| 14 | Olley [5] | 2006 | Nigeria | Cross-sectional | 169 | 151 (89) | 18 (11) | .(.) | .(.) |
| 15 | Othieno [34] | 2000 | Kenya | Cross-sectional | 50 | 36 (72) | 14 (28) | .(.) | .(.) |
| 16 | Project Concern [35] | 2002 | Zambia | Cross-sectional | 1232 | 1010 (82) | 222 (18) | 309 (25)C | 761 (62) |
| 17 | Salem [36] | 2002 | Egypt | Cross-sectional | 100 | 100 (100) | 0 (0) | 94 (94)A | 6 (6) |
| South and Central America | |||||||||
| 18 | Bezerra [37] | 2011 | Brazil | Cross-sectional | 651 | 465 (71) | 186 (29) | .(.) | .(.) |
| 19 | Campos [38] | 1994 | Brazil | Mixed-methods | 376 | 289 (77) | 87 (23) | 200 (53)B | 176 (47) |
| 20 | Carlini-Cotrim [39] | 1988 | Brazil | Cross-sectional | 120 | 90 (75) | 30 (25) | .(.) | .(.) |
| 21 | de Carvalho [10] | 2006 | Brazil | Cross-sectional | 161 | 128 (80) | 33 (20) | .(.) | .(.) |
| 22 | Forster [40] | 1996 | Brazil | Cross-sectional | 79a | 67 (85) | 12 (15) | 31 (39)B | 48 (61) |
| 23 | Huang [41] | 2004 | Bolivia | Cross-sectional | 124 | 85 (69) | 39 (31) | 124 (100)A | 0 |
| 24 | Noto [42] | 1997 | Brazil | Cross-sectional | 565 | 410 (73) | 154 (27) | 414 (73)C | 148 (27) |
| 25 | Obandob [18] | 2004 | Costa Rica | Cross-sectional | 83 | 59 (71) | 24 (29) | .(.) | .(.) |
| 26 | Opaleyeb [19] | 2009 | Brazil | Cross-sectional | 2807 | 2120 (76) | 687 (24) | .(.) | .(.) |
| 27 | Pinto [43] | 1994 | Brazil | Cross-sectional | 394 | . (.) | . (.) | 195 (49)B | 199 (51) |
| 28 | Portob [20] | 1994 | Brazil | Cross-sectional | 496 | 463 (93) | 33 (7) | 395 (80)A,B | 101 (20) |
| 29 | Souza [44] | 2010 | Honduras | Cohort | 236 | . (.) | . (.) | .(.) | .(.) |
| 30 | Tyler [45] | 1991 | Columbia | Cross-sectional | 94 | 94 (100) | 0 (0) | .(.) | .(.) |
| 31 | Wittig [46] | 1997 | Honduras | Cross-sectional | 1244 | 722 (58) | 522 (42) | 160 (13)A,B | 1084 (87) |
| Asia | |||||||||
| 32 | Bal [47] | 2010 | India | Cross-sectional | 554 | 362 (65) | 192 (35) | .(.) | .(.) |
| 33 | Benegal [48] | 1998 | India | Mixed-methods | 281 | 230 (82) | 50 (18) | 150 (53)C | 131 (47) |
| 34 | Gaidhane [49] | 2008 | India | Cross-sectional | 163 | 163 (100) | 0 (0) | 83 (51)B | 80 (49) |
| 35 | Khurana [50] | 2004 | India | Cross-sectional | 150 | 150 (100) | 0 (0) | .(.) | .(.) |
| 36 | Lamsal [51] | 2009 | India | Conference abstracts | 100 | . (.) | . (.) | .(.) | .(.) |
| 37 | Njord [52] | 2008 | Philippines | Cross-sectional | 179 | 107 (60) | 72 (40) | 179 (100)C | 0 (0) |
| 38 | Njord [9] | 2010 | Philippines | Cross-sectional | 311a | 182 (59) | 129 (41) | 141 (45)A,B | 171 (55) |
| 39 | Pagare [53] | 2004 | India | Cross-sectional | 115 | 115 (100) | 0 (0) | .(.) | .(.) |
| 40 | Rai [54] | 2002 | Nepal | Cross-sectional | 118 | 118 (100) | 0 (0) | .(.) | .(.) |
| 41 | Tamesis Jr [55] | 2003 | Philippines | Cross-sectional | 22 | 18 (82) | 4 (18) | .(.) | .(.) |
| 42 | Techakasem [56] | 2006 | Thailand | Case–control | 21a | 7 (33) | 14 (67) | .(.) | .(.) |
| 43 | Tiwari [57] | 2007 | India | Cross-sectional | 400 | 400 (100) | 0 (0) | .(.) | .(.) |
| Europe/Eurasia | |||||||||
| 44 | Alexandrescu [60] | 1996 | Romania | Cross-sectional | 245 | . (.) | . (.) | .(.) | .(.) |
| 45 | Kissin [61] | 2007 | Russia | Cross-sectional | 313 | 198 (63) | 115 (37) | .(.) | .(.) |
| 46 | Olgar [62] | 2008 | Turkey | Case–control | 53a | 53 (100) | 0 (0) | .(.) | .(.) |
| 47 | Robbins [63] | 2010 | Ukraine | Cross-sectional | 929 | 706 (76) | 223 (24) | .(.) | .(.) |
| 48 | Turkmen [64] | 2004 | Turkey | Cross-sectional | 52 | 50 (96) | 2 (4) | 1 (2)C | 46 (88) |
| Middle East | |||||||||
| 49 | Ataei [59] | 2010 | Iran | Conference abstracts | 399 | 271 (68) | 128 (32) | .(.) | .(.) |
| 50 | Sherman [58] | 2005 | Pakistan | Cross-sectional | 347 | 333 (96) | 14 (4) | 261 (75)C | 41 (12) |
| TOTAL | 16 987 | 12 693 (75) | 3604 (21) | 4169 (25) | 3563 (21) | ||||
Excludes non-street children from sample.
Drug use data not used in meta-prevalence analysis. Data not reported.
Democratic Republic of the Congo.
Categories of street children according to A, B or C:
utilized the UNICEF ON/OF classifications for street children’s inclusion;
reported UNICEF ON/OF classifications in results;
review derived ON/OF classifications based on study results indicating sleeping at ‘home’ or in streets/public places.
Table 2 presents the methodological and geographical characteristics of the 50 studies. There were studies from 22 countries, the majority (62%) being from Africa [5,6,8,13,24–36] and South and Central America [10,18–20,37–46], with the remainder located in Asia [9,47–57], the Middle East [58,59] and Europe [60–64]. Almost all studies (41 of 50) were cross-sectional. Only eight studies utilized the UNICEF definition of street children for their inclusion criteria and only 15 studies defined drug use clearly in their methods.
Table 2.
Methodological characteristics and geographical location of 50 studies included for review.
| Variable | No. of studies (%) |
|---|---|
| Geographical location | |
| Africa | 17 (34) |
| Middle East | 2 (4) |
| Asia | 12 (24) |
| South and Central America | 14 (28) |
| Europe | 5 (10) |
| UNICEF definitions of street children for inclusion criteria | 8 (16) |
| Defined drug use | 15 (30) |
| Defined life-time drug usea | 5 (19) |
| Defined current drug useb | 8 (89) |
| Used a validated questionnaire | 8 (16) |
| Ethics approval reported | 23 (46) |
| Sampling origin | |
| Temporary home/institution | 9 (18) |
| Drop-in centres | 10 (20) |
| Streets | 26 (52) |
| Mixed (streets, institutions) | 2 (4) |
| Unknown | 1 (2) |
| Otherc | 2 (4) |
| Sampling methodology | |
| Non-probability | 34 (68) |
| Probability | 12 (24) |
| Unknown | 4 (8) |
| Analysis | |
| Descriptive only | 26 (52) |
| Bivariate only | 14 (28) |
| Multivariate only | 2 (4) |
| Bivariate and multivariate | 8 (16) |
| Study design | |
| Cross-sectional | 41 (82) |
| Case–control | 2 (4) |
| Cohort | 1 (2) |
| Mixed methods | 3 (6) |
| Conference abstracts | 3 (6) |
Of those who reported life-time use (n = 27).
Of those who reported current use (n = 9).
Aljamiri schools, hospital records.
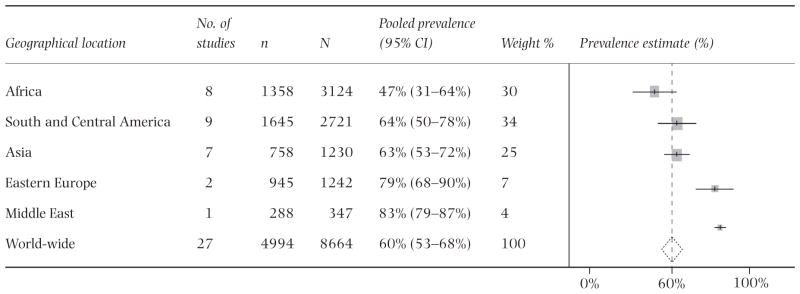
The life-time drug use prevalence varied substantially world-wide, from 14% in Nigeria [5] to 92% in Honduras [44] and Brazil [39]. Additionally, life-time substance use varied substantially intracontinentally. In Africa, the lifetime drug use prevalence ranged from 14% in Nigeria [5] to 74% in Kenya [13]. Similarly, in South and Central America (40% Brazil [10]—92% Honduras [44] and Brazil [39]) and Asia (48% Thailand [56]—81% India [49]) a wide range of life-time drug use was reported. Figure 2a demonstrates the geographical distribution of life-time substance use among SICY from 27 studies in 13 countries. Meta-analysis of life-time substance use from these studies yielded an overall life-time drug use pooled-prevalence estimate of 60% [95% confidence interval (CI) = 51–69%]. The I2 statistic demonstrated significant heterogeneity between studies, I2 = 97.2%, P = 0.000 (Table 3a). Subgroup analyses demonstrated differences in life-time drug use prevalence by geographical region. Sensitivity analysis to assess whether one country had an undue influence on the meta-analysis in the geographical subcategories revealed that the combined effects did not differ significantly when omitting any given country.
Figure 2.
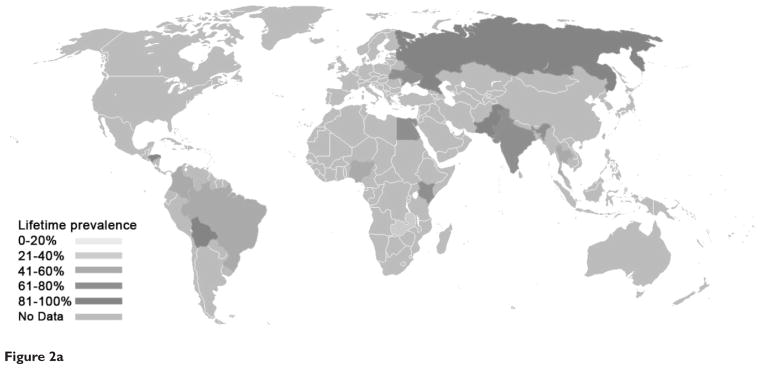

Figure 2a Life-time substance use among street-involved children and youth from 27 studies in 13 countries
Figure 2b Inhalant use by street-involved children and youth from 27 studies representing 14 resource-constrained countries
Table 3a.
Forest plot and pooled prevalence of life-time drug use by geographical region in resource-constrained settings among street-involved children and youth.
|
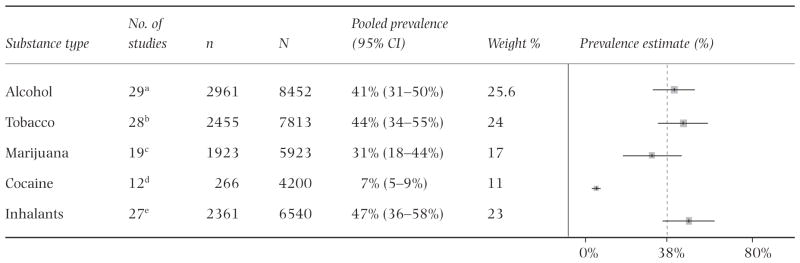
Similar types of substance use were reported consistently by studies world-wide. Meta-analysis revealed that SICY reported most commonly using inhalants, followed by tobacco, alcohol and marijuana (Table 3b). Tests for homogeneity revealed that studies were heterogeneous for each substance category. The reported use of inhalants varied widely throughout geographical regions and countries. Figure 2b demonstrates the geographical distribution of inhalant use by SICY from 27 studies representing 14 resource-constrained countries. The meta-analysis revealed an overall pooled-prevalence estimate of 47% (95% CI = 36–58%) for street children’s reported inhalant use. Additionally, tobacco use measured in 28 studies from 14 countries yielded a pooled-prevalence estimate of 44% (95% CI = 34–55%); alcohol use measured in 29 studies representing 15 countries yielded a pooled prevalence of 41% (95% CI = 31–50%); and marijuana use measured in 19 studies representing 10 countries yielded a pooled prevalence of 31% (95% CI = 18%–44%). Fewer studies [12], representing six countries, measured cocaine use. The combined cocaine data revealed a pooled-prevalence estimate of 7% (95% CI = 5–9%). The majority of cocaine use was concentrated in five studies originating from Brazil (16% crude unweighted mean), with the remaining studies from Africa [6] and Eurasia [1] with a low prevalence (2% crude unweighted mean). The use of other psychoactive substances, including pharmaceuticals (six studies) [13,19,28,34,40,61] and injection drugs (seven studies), were reported much less frequently. Injection drug use occurred primarily in two Eastern European studies [61,63] (43% crude unweighted mean); the remaining studies reporting injection drug use were from South and Central America [10,38], Asia [51,57] and the Middle East [58], all with a low prevalence (3% crude unweighted mean).
Table 3b.
Forest plot and pooled prevalence of drug use by substance type in resource-constrained settings among street-involved children and youth.
|
Table 4 presents the characteristics analyzed by studies utilizing bivariate and multivariate analyses to test associations between selected variables and substance use. There was a total of 41 socio-demographic, psychosocial, health and emotional characteristics tested for their association with SICY’s substance use. In those with significant findings, using substances was associated with participants who were older, male, classified as children of the street, those who had been street-involved for a greater duration, those without family contact, and those sleeping in public or communal places at night. In multivariate analysis, no consistent associations appeared, with the exception of age.
Table 4.
The proportion of studies that found a significant association (P < 0.05) in bivariate or multivariate analyses among those that measured the selected characteristics.
| Variable | Proportion of studies with significant findings
|
|||
|---|---|---|---|---|
| Bivariate
|
Multivariate
|
|||
| Proportiona | Study no. | Proportiona | Study no. | |
| Age | 7/9 | 1*, 7*, 10, 14, 21*, 26*, 32*, 47*, 50* | 6/7 | 1*, 7*, 21*, 31*, 32, 34*, 50* |
| Male sex | 5/8 | 7, 15*, 32*, 21*, 23, 26, 37*, 50* | 1/4 | 7, 21, 31, 32* |
| UNICEF ON/OF the street classification | 5/6 | 7*, 19*, 22*, 27*, 28, 38* | 1/1 | 34* |
| Duration street involved | 5/5 | 7*, 21*, 24*, 26*, 50* | 2/5 | 7*, 10* |
| Family contact | 5/5 | 3*, 7*, 21*, 32*, 33* | 1/3 | 3, 21*, 32 |
| Where staying at night | 4/4 | 3*, 7*, 32*, 50* | 3/6 | 3, 7*, 10, 31*, 32*, 50, |
| Sexual activity data | 3/4 | 7, 21*, 33*, 50* | 2/2 | 8*, 50* |
| Familial substance use | 2/4 | 7*, 39, 43, 50* | 1/1 | 7* |
| Daily earnings | 2/4 | 7, 10, 33*, 50* | 1/3 | 10, 31, 50* |
| Parental marital status | 2/4 | 1*, 3, 10, 39* | 1/3 | 1*, 10, 31 |
| Parental vital status | 2/4 | 3*, 10, 32*, 39 | 0/1 | 32 |
| Frequency on streets (hours/day) | 3/3 | 7*, 21*, 26* | 2/2 | 21*, 31* |
| HIV data | 2/2 | 21*, 45*, 47* | 1/1 | 21* |
| Connectedness with parent(s)/family relations | 2/2 | 3*, 26* | 2/2 | 3*, 31* |
| Current school attendance | 2/2 | 21*, 26* | – | – |
| Education level achieved/literacy | 1/2 | 7, 10* | 0/2 | 10, 31 |
| Work | 1/2 | 39*, 50 | 0/2 | 10, 31 |
| Ever arrested/crime involvement | 1/1 | 50* | 2/2 | 31*, 50* |
| Accessing services for street children | 1/1 | 7* | 0/2 | 7, 31 |
| Polygamous homes | 1/1 | 1* | 1/1 | 1* |
| Feelings of loneliness | 1/1 | 1* | 1/1 | 1* |
| Connectedness with friends | 1/1 | 3* | 1/1 | 3* |
| Inflicting self-harm | 1/1 | 50* | 1/1 | 50* |
| Feeling public hatred | 1/1 | 50* | 1/1 | 50* |
| Maltreatment at home | 1/1 | 39* | 1/1 | 39* |
| Parental work-place | 1/1 | 3* | 0/1 | 3 |
| Desire to return home | 1/1 | 50* | 0/1 | 50 |
| Health problems | 1/1 | 33* | 0/1 | 31 |
| Parental education | 1/1 | 1* | – | – |
| Domestic violence | 1/1 | 39* | – | – |
| Depressive symptoms | 1/1 | 1* | – | – |
| Maladaptive/antisocial coping strategies | 1/1 | 33* | – | – |
| Runaway | 1/1 | 39* | – | – |
| Religion | 0/1 | 10 | 0/2 | 10, 31 |
| Drug use knowledge | 1/1 | 7* | 0/1 | 7 |
| Drug use attitudes | 0/1 | 7 | – | – |
| Satisfaction with street life | 0/1 | 10 | – | – |
| Peer substance use | – | – | 1/1 | 34* |
| Worry | – | – | 1/1 | 1* |
| Family pathology | – | – | 1/1 | 34* |
| Hunger | – | – | 0/1 | 1 |
Top number is number of studies that found a significant association; bottom number is the number that measured the association.
P < 0.05. Study no. represents the study no. presented in Table 1 (not the reference).
Our review demonstrates that only five studies [10,13,29,48,58] measured the association between SICY’s substance use and sexual activity outcomes and three studies [10,61,63] in relation to HIV. However, qualitative and quantitative evidence suggests that SICY are engaging in risky sexual behavior in association with their substance use. In Sudan, qualitative inquiry found that street children admitted to exchanging sex in order to receive glue [30]. In Pakistan, 30% of male street children reported exchanging sex for drugs, with 71% of them doing so with strangers [65]; drug users were 3.4 times more likely have ever exchanged sex for food, shelter, drugs or money [58]. Additionally, in Brazil 34% of participants in street circumstances sampled had engaged in any unprotected sex under the influence of drugs or alcohol in their life-time and the odds of unsafe sex in those using inhalants in the past year were increased [10]. In India, almost half of all children who indicated being sexually active had been forced into, paid for or were offered drugs in exchange for sex; being sexually active was associated with inhalant use [48]. Of the three studies that investigated the relationship between substance use and HIV, two studies from Eastern Europe found that being HIV-positive was associated with life-time substance use, injection drug use, the use of inhalants and other psychoactive drugs [61,63]. In Brazil, those who had used illicit substances were 11.4 times more likely to have ever been tested for HIV and 7.8 times more likely to have friends with HIV [10].
In relation to physical and mental health measures, we identified two studies investigating the relationship between substance use and physical health outcomes [46,48] and one study to a mental health outcome [24]. One study found a significant association between the use of inhalants and physical symptoms of tingling and numbness, burning sensations while urinating, genital sores, headaches and stomach problems [48]. Depressive symptoms characterized as feeling sad for 2 or more weeks and feelings of loneliness were identified as being associated with the use of inhalants, alcohol, tobacco and other psychoactive substances by street children in Nigeria [24].
We identified a total of 12 studies [8,9,13,28,30, 33,34,38,39,42,49,54] from eight countries, measured using qualitative and quantitative methods, that explored the reasons why street children engage in drug use or their reason for first use. A wide variety of responses was reported, with the five most commonly reported reasons for engaging in substance use being: peers and peer pressure (seven studies), to forget their problems and to escape reality (five studies), to feel good or pleasurable (five studies), to experiment (four studies) and to gain courage and strength on the streets (three studies).
DISCUSSION
Main findings
This systematic review and meta-analysis indicate a high prevalence of substance use of SICY in RCS with significant variation by geographical region and study methodology. Specifically, our results confirm that the majority of SICY around the world, in a variety of cultures and contexts, are using volatile solvents. Although injection drug use garners significant attention in the literature due to the risk of contracting HIV and other blood-borne infections, our review demonstrates that non-injection drug use is more common among SICY in RCS. The nature of the substances they use could have a major impact on morbidity and mortality [66], as well as impacting upon their potential for social reintegration. Further, these pooled-prevalence estimates are several times higher than those published by the World Health Organization of the life-time psychoactive substance use (including alcohol) of non-street youth globally [67].
Our findings provide insight into the factors associated with substance use. In particular, the duration of time a child has been street-involved, where the child was staying at night and having family contact were associated consistently with substance use in all studies that measured these characteristics; moreover, older age, male sex, sexual activity and whether being on or of the street are all related to substance use. Our review further identifies that peers and peer pressure are the most commonly reported reasons why SICY engage in substance use.
Gaps in the literature and research priorities
This review has determined that the majority of the substance use literature encompassing SICY in RCS is cross-sectional and descriptive in nature, focused on determining the type and prevalence of drug use with limited statistical analysis. Expanding research initiatives and conducting longitudinal studies is necessary to understand the risk and protective factors associated with substance use in this vulnerable population. We have minimal knowledge about what predicts street children’s initiation, ongoing use and cessation of substances. We also found a poor representation of females in these studies; nine did not include any girls in their sample. Street-involved girls and young women might be both more marginalized and more vulnerable while also being less accessible for research. This lack of equity is likely to result in an important gender-based selection bias in this field of inquiry.
Another major concern is the paucity of information available on the physical and mental health outcomes that street children and youth could develop due to their misuse of multiple substances. In other populations, inhalants have been linked to cognitive and neurological impairment, sudden sniffing death syndrome due to cardiac arrhythmia, renal, pulmonary and teratogenic effects [58,66,68]. Additionally, evidence exists of psychological and physical dependence among volatile solvent users [30,69]. However, little is known about street children’s addiction to inhalants, and the psychological and cognitive impacts sustained by this population. Although the use of substances is linked to detrimental health outcomes, our review revealed that only two studies investigated the relationship between substance use and physical health outcomes [46,48] and one study to a mental health outcome [24].
The use of drugs often leads to risky sexual behavior, including commercial sex work, exchanging sex for drugs and forced sex. These high-risk behaviors, in association with drug use, could expose individuals to HIV, other sexually transmitted infections and violence, yet little to no information about these behaviors and health outcomes in this population is available. Although it has been identified that some SICY are exchanging sex for receiving substances or while under the influence, little else is known. Due to the relationship that is known to exist [70] between drug and alcohol use and engaging in unsafe sex, exchanging or selling sex and rape, it is crucial to understand these dynamics more clearly in the context of solvent use and understand their impact upon HIV and mortality risks. The dearth of data on these issues represents several critical gaps in the literature.
Limitations
There are limitations to our findings. First, this review included only studies published in English. Secondly, the quality of the studies did not factor into whether or not they were included in the review or meta-analyses. Thirdly, we were unable to perform meta-analytical procedures to assess the differences in drug use among children on the street versus of the street, due to the limited number of studies that reported drug use stratified by these classifications. Fourthly, it should be considered that, due to the sensitive nature of questions regarding substance use, social desirability biases as well as the relationship between the children and the interviewer and the sampling origin may have affected prevalence estimates. Children may have been less likely to answer truthfully regarding their substance use habits if it precluded their participation at a drop-in centre or expulsion from a shelter/institution or if they distrusted the interviewer. Fifthly, although in all analyses we rejected the null hypothesis of homogeneity, the varying methodological quality of the studies may have contributed to varying estimates of drug use prevalence. Sixthly, the analysis of factors associated with substance use and reasons why street children engage in substance use are from data in the 50 studies that were identified based on the review’s eligibility criteria. Therefore, it is possible that studies addressing only those topics that did not meet our eligibility criteria were excluded. Finally, it is important to note that aboriginal and First Nations youth are often street-involved and using volatile solvents and other substances [12,71,72]. However, because, technically, they live in very high HDI countries (albeit in environments often referred to as ‘Third World conditions’ [73]), they were not included in this review.
Other important considerations arising from this review are that a number of studies included children who were currently attending school and classified them as street children, and very few utilized the UNICEF definition for inclusion criteria. Children classified by various definitions as ‘street-involved children and youth’ may have altered the comparability of the studies. This finding points to the need to develop a universal and standardized definition of what constitutes being a street-involved child or youth. Additionally, many studies measuring drug use failed to define what constituted substance use in their study, and whether it was life-time or current use; nor did studies explore levels of abuse and dependency. Furthermore, in certain circumstances we were unable to extract data for inclusion in the meta-analyses due to poor reporting and combining data on different drugs. In order to obtain clear estimates of the burden of substance use and abuse in this population there is a need to define, and distinguish clearly, life-time use from abuse and dependency as well as current using patterns; ameliorating reporting and defining variables clearly will ensure that results are interpreted effectively with relevant conclusions. Although some studies (eight of 50) indicated using a validated data collection tool, it was developed by the World Health Organization in 1981 for assessing Drug Use in Non-Student Youth [74]. The development of an updated valid and reliable substance use data collection tool to use with SICY could improve data collection and comparability between studies.
CONCLUSION
This review has identified key issues requiring urgent public health action. The widespread use of inhalants is particularly concerning due to legal availability and unrestricted sales to minors, as well as detrimental health effects, and should be a major concern for law and policymakers. It is likely that the use of inhalants could impact upon the ability of street children to be integrated into society and resume a normal life. While there is a need to investigate further the link between their substance use and health outcomes, we hypothesize that due to their drug use they are at higher risk of poor health outcomes, including HIV and mortality. Additional effort and collaboration between policymakers, communities and researchers is essential to understand and implement mechanisms to reduce the harms associated with using inhalants, while also preventing and stopping substance use among this vulnerable population.
Acknowledgments
The project described was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD060478).
Footnotes
Declaration of interests
None.
References
- 1.United Nations Children’s Fund (UNICEF) The State of the World’s Children 2012: Children in an Urban World. NewYork: UNICEF; 2012. [Google Scholar]
- 2.World Health Organization (WHO); Dependence DoMHaS, editor. A Profile of Street Children. Geneva: World Health Organization; 2000. Working With Street Children: Module 1. [Google Scholar]
- 3.le Roux J. The worldwide phenomenon of street children: conceptual analysis. Adolescence. 1996;31:965–71. [PubMed] [Google Scholar]
- 4.Hadland SE, Kerr T, Li K, Montaner JS, Wood E. Access to drug and alcohol treatment among a cohort of street-involved youth. Drug Alcohol Depend. 2009;101:1–7. doi: 10.1016/j.drugalcdep.2008.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olley BO. Social and health behaviors in youth of the streets of Ibadan, Nigeria. Child Abuse Negl. 2006;30:271–82. doi: 10.1016/j.chiabu.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 6.Ayaya SO, Esamai FO. Health problems of street children in Eldoret, Kenya. East Afr Med J. 2001;78:624–9. doi: 10.4314/eamj.v78i12.8930. [DOI] [PubMed] [Google Scholar]
- 7.Abdelgalil S, Gurgel RG, Theobald S, Cuevas LE. Household and family characteristics of street children in Aracaju, Brazil. Arch Dis Child. 2004;89:817–20. doi: 10.1136/adc.2003.032078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morakinyo J, Odejide AO. A community based study of patterns of psychoactive substance use among street children in a local government area of Nigeria. Drug Alcohol Depend. 2003;71:109–16. doi: 10.1016/s0376-8716(03)00093-0. [DOI] [PubMed] [Google Scholar]
- 9.Njord L, Merrill RM, Njord R, Lindsay R, Pachano JD. Drug use among street children and non-street children in the Philippines. Asia Pac J Public Health. 2010;22:203–11. doi: 10.1177/1010539510361515. [DOI] [PubMed] [Google Scholar]
- 10.de Carvalho FT, Neiva-Silva L, Ramos MC, Evans J, Koller SH, Piccinini CA, et al. Sexual and drug use risk behaviors among children and youth in street circumstances in Porto Alegre, Brazil. AIDS Behav. 2006;4:S57–66. doi: 10.1007/s10461-006-9124-4. [DOI] [PubMed] [Google Scholar]
- 11.Roy E, Boudreau JF, Leclerc P, Boivin JF, Godin G. Trends in injection drug use behaviors over 10 years among street youth. Drug Alcohol Depend. 2007;89:170–5. doi: 10.1016/j.drugalcdep.2006.12.025. [DOI] [PubMed] [Google Scholar]
- 12.Hadland SE, Marshall BDL, Kerr T, Zhang R, Montaner JS, Wood E. A comparison of drug use and risk behavior profiles among younger and older street youth. Subst Use Misuse. 2011;46:1486–94. doi: 10.3109/10826084.2011.561516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Embleton L, Ayuku D, Atwoli L, Vreeman R, Braitstein P. Knowledge, attitudes, and substance use practices among street children in Western kenya. Subst Use Misuse. 2012;47:1234–47. doi: 10.3109/10826084.2012.700678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Srivastava M. Drug abuse among street children. Perspect Soc Work. 1995;10:11–7. [Google Scholar]
- 15.United Nations Children’s Fund (UNICEF), Ministry of Social Afffairs. Study on Street Children in Four Selected Towns of Ethiopia. Cork, Ireland: UNICEF; 1992. [Google Scholar]
- 16.United Nations Development Programme (UNDP) [accessed 5 September 2012];Human Development Index. 2011 Available at: http://hdr.undp.org/en/statistics/hdi/
- 17.United Nations Development Programme (UNDP) Human Development Report 2010—The Real Wealth of Nations: Pathways to Human Development. New York: UNDP; 2010. [Google Scholar]
- 18.Obando P, Kliewer W, Murrelle L, Svikis DS. The comorbidity of substance abuse and depressive symptoms in Costa Rican adolescents. Drug Alcohol Depend. 2004;76:37–44. doi: 10.1016/j.drugalcdep.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 19.Opaleye ES, Noto AR, Sanchez ZM, Moura YG, Galduroz JC, Carlini EA. Recreational use of benzydamine as a hallucinogen among street youth in Brazil. Rev Bras Psiquiatr. 2009;31:208–13. doi: 10.1590/s1516-44462009000300005. [DOI] [PubMed] [Google Scholar]
- 20.Porto S, Cardoso D, Queiroz D, Rosa H, et al. Prevalence and risk factors for HBV infection among street youth in central Brazil. J Adolesc Health. 1994;15:577–81. doi: 10.1016/1054-139x(94)90142-p. [DOI] [PubMed] [Google Scholar]
- 21.Sanderson S, Tatt ID, Higgins JPT. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliopgrahy. Int J Epidemiol. 2007;36:666–76. doi: 10.1093/ije/dym018. [DOI] [PubMed] [Google Scholar]
- 22.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 23.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–48. [PubMed] [Google Scholar]
- 24.Abdulmalik J, Omigbodun O, Beida O, Adedokun B. Psychoactive substance use among children in informal religious schools (Almajiris) in northern Nigeria. Ment Health, Relig Cult. 2009;12:527–42. [Google Scholar]
- 25.Abou-Hatab M, Okasha Y. Volatile inhalant dependence and intoxication among a sample of Egyptian street children. European Psychiatry Conference: 18th European Congress of Psychiatry; Munich, Germany. 27 February–2 March, 2010. [Google Scholar]
- 26.Adebiyi A, Owaoje O, Asuzu M. Relationships as determinants of substance use amongst street children in local government area in south-western Nigeria. South African. Fam Pract. 2008;50:S47. [Google Scholar]
- 27.Aidan M. Stress and coping strategies among street children in Lusaka. J Psychol Afr. 1997;2:24–33. [Google Scholar]
- 28.Elkoussi A, Bakheet S. Volatile substance misuse among street children in Upper Egypt. Subst Use Misuse. 2011;46:35–9. doi: 10.3109/10826084.2011.580202. [DOI] [PubMed] [Google Scholar]
- 29.Kayembe PK, Mapatano MA, Fatuma AB, Nyandwe JK, Mayala GM, Kokolomami JI, et al. Knowledge of HIV, sexual behavior and correlates of risky sex among street children in Kinshasa, Democratic Republic of Congo. East Afr J Public Health. 2008;5:186–92. [PubMed] [Google Scholar]
- 30.Kudrati M, Plummer ML, Yousif ND. Children of the sug: a study of the daily lives of street children in Khartoum, Sudan, with intervention recommendations. Child Abuse Negl. 2008;32:439–48. doi: 10.1016/j.chiabu.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 31.Nada KH, Suliman EDA. Violence, abuse, alcohol and drug use, and sexual behaviors in street children of Greater Cairo and Alexandria, Egypt. AIDS. 2010;24:S39–S44. doi: 10.1097/01.aids.0000386732.02425.d1. [DOI] [PubMed] [Google Scholar]
- 32.Nzimakwe D, Brookes H. An investigation to determine the health status of institutionalised street children in a place of safety in Durban. Curationis. 1994;17:27–31. [PubMed] [Google Scholar]
- 33.Okwaraji FE, Ebigbo PO, Akpala C. Substance use among Nigerian street children. IFE Psychologia. 1996;4:7–13. [Google Scholar]
- 34.Othieno C, Obondo A, Kathuku D, Ndetei D. Patterns of substance use among Kenyan street children. South Afr J Child Adolesc Ment Health. 2000;12:145–50. [Google Scholar]
- 35.Lemba M. Rapid Assessment of Street Children in Lusaka. Lusaka: Project Concern International Zambia; 2002. [Google Scholar]
- 36.Salem EM, Abd el-Latif F. Sociodemographic characteristics of street children in Alexandria. East Mediterr Health J. 2002;8:64–73. [PubMed] [Google Scholar]
- 37.Bezerra KF, Gurgel RQ, Ilozue C, Castaneda DN. Estimating the number of street children and adolescents in two cities of Brazil using capture–recapture. J Paediatr Child Health. 2011;47:524–9. doi: 10.1111/j.1440-1754.2011.02015.x. [DOI] [PubMed] [Google Scholar]
- 38.Campos R, Raffaelli M, Ude W. Social networks and daily activities of street youth in Belo Horizonte, Brazil. Child Dev. 1994;65:319–30. [PubMed] [Google Scholar]
- 39.Carlini-Cotrim B, Carlini E. The use of solvents and other drugs among homeless and destitute children living in the city streets of Sao Paulo, Brazil. Soc Pharmacol. 1988;2:51–62. [Google Scholar]
- 40.Forster LM, Tannhauser M, Barros HM. Drug use among street children in southern Brazil. Drug Alcohol Depend. 1996;43:57–62. doi: 10.1016/s0376-8716(96)01288-4. [DOI] [PubMed] [Google Scholar]
- 41.Huang CC, Barreda P, Mendoza V, Guzman L, Gilbert P. A comparative analysis of abandoned street children and formerly abandoned street children in La Paz, Bolivia. Arch Dis Child. 2004;89:821–6. doi: 10.1136/adc.2003.042911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Noto AR, Nappo SA, Galduroz JC, Mattei R, Carlini EA. Use of drugs among street children in Brazil. J Psychoact Drugs. 1997;29:185–92. doi: 10.1080/02791072.1997.10400186. [DOI] [PubMed] [Google Scholar]
- 43.Pinto JA, Ruff AJ, Paiva JV, Antunes CM, Adams IK, Halsey NA, et al. HIV risk behavior and medical status of underprivileged youths in Belo Horizonte, Brazil. J Adolesc Health. 1994;15:179–85. doi: 10.1016/1054-139x(94)90547-9. [DOI] [PubMed] [Google Scholar]
- 44.Souza R, Porten K, Nicholas S, Grais R. Outcomes for street children and youth under multidisciplinary care in a drop-in centre in Tegucigalpa, Honduras. Int J Soc Psychiatry. 2010 Sep 14; doi: 10.1177/0020764010382367. ••: ••–••. [DOI] [PubMed] [Google Scholar]
- 45.Tyler F, Tyler S. Making it on the streets in Bogota: a psychosocial study of street youth. Genet Soc Gen Psychol Monogr. 1991;117 ••–••. [PubMed] [Google Scholar]
- 46.Wittig MC, Wright JD, Kaminsky DC. Substance use among street children in Honduras. Subst Use Misuse. 1997;32:805–27. doi: 10.3109/10826089709055860. [DOI] [PubMed] [Google Scholar]
- 47.Bal B, Mitra R, Mallick AH, Chakraborti S, Sarkar K. Nontobacco substance use, sexual abuse, HIV, and sexually transmitted infection among street children in Kolkata, India. Subst Use Misuse. 2010;45:1668–82. doi: 10.3109/10826081003674856. [DOI] [PubMed] [Google Scholar]
- 48.Benegal V, Bhushan K, Sheshadri S, Karott M. Drug abuse among street children in Bangalore. Bangalore, India: National Institute of Mental Health and Neurosciences, Bangalore and the Bangalore Forum for Street and Working Children; 1998. [Google Scholar]
- 49.Gaidhane A, Zahiruddin QS, Waghmare L, Shanbhag S, Zodpey S, Joharapurkar SR. Substance abuse amongst street children in Mumbai. Vulnerable Child Youth Stud. 2008;3:42–51. [Google Scholar]
- 50.Khurana S, Sharma M, Jena S, Saha R, Ingle GK. Mental health status of runaway adolescents. Indian J Pediatr. 2004;71:405–9. doi: 10.1007/BF02725627. [DOI] [PubMed] [Google Scholar]
- 51.Lamsal S, Walia I, Kumar R, Kaur B. Tobacco and other substance behaviours among the street children. Support Care Cancer. 2009;17:934–5. [International MASCC/IS00 Symposium. Rome, Italy; Conference 25–27 June 2009] [Google Scholar]
- 52.Njord L, Merrill RM, Njord R, Pachano JD, Hackett A. Characterizing health behaviors and infectious disease prevalence among Filipino street children. Int J Adolesc Med Health. 2008;20:367–74. doi: 10.1515/ijamh.2008.20.3.367. [DOI] [PubMed] [Google Scholar]
- 53.Pagare D, Meena GS, Singh MM, Saha R. Risk factors of substance use among street children from Delhi. Indian Pediatr. 2004;41:221–5. [PubMed] [Google Scholar]
- 54.Rai A, Ghimire KP, Shrestha P, Tuladhar S. Glue Sniffing among Street Children in Kathmandu Valley. Kathmandu, Nepal: Child Workers in Nepal Concerned Centre; 2002. [Google Scholar]
- 55.Tamesis JM, Jr, Cloma LAD, Adarlo GM. Effects of toluene inhalation on vision among Filipino street children. Neuro Ophthalmol Japan. 2003;20:259–64. [Google Scholar]
- 56.Techakasem P, Kolkijkovin V. Runaway youths and correlating factors, study in Thailand. J Med Assoc Thai. 2006;89:212–6. [PubMed] [Google Scholar]
- 57.Tiwari P. Life on streets. Indian J Pediatr. 2007;74:283–6. doi: 10.1007/s12098-007-0045-7. [DOI] [PubMed] [Google Scholar]
- 58.Sherman SS, Plitt S, ul Hassan S, Cheng Y, Zafar ST. Drug use, street survival, and risk behaviors among street children in Lahore, Pakistan. J Urban Health. 2005;82:iv113–24. doi: 10.1093/jurban/jti113. [DOI] [PubMed] [Google Scholar]
- 59.Ataei B, Nokhodian Z, Babak A, Shoaei P, Kassaian N, Ataie M. Seroprevalence and associated risk factors of hepatitis B virus among street children in Isfahan, Iran (2005–2007) Int J Infect Dis. 2010;14:e230. [14th International Congress on Infectious Diseases (ICID) Miami, FL, USA. Conference 9–12 March 2010 Sponsor: Pfizer, Sanofi-Pasteur, American Society for Microbiology (ASM), Associacion Panamericana de Infectologia (API), Astellas Pharma Global Development, Inc.] [Google Scholar]
- 60.Alexandrescu G. Street children in Bucharest. Childhood Global J Child Res. 1996;3:267–70. [Google Scholar]
- 61.Kissin DM, Zapata L, Yorick R, Vinogradova EN, Volkova GV, Cherkassova E, et al. HIV seroprevalence in street youth, St. Petersburg, Russia. AIDS. 2007;21:2333–40. doi: 10.1097/QAD.0b013e3282f125b3. [DOI] [PubMed] [Google Scholar]
- 62.Olgar S, Oktem F, Dindar A, Kilbas A, Turkoglu UD, Cetin H, et al. Volatile solvent abuse caused glomerulopathy and tubulopathy in street children. Hum Exp Toxicol. 2008;27:477–83. doi: 10.1177/0960327108092292. [DOI] [PubMed] [Google Scholar]
- 63.Robbins CL, Zapata L, Kissin DM, Shevchenko N, Yorick R, Skipalska H, et al. Multicity HIV seroprevalence in street youth, Ukraine. Int J STD AIDS. 2010;21:489–96. doi: 10.1258/ijsa.2010.010097. [DOI] [PubMed] [Google Scholar]
- 64.Turkmen M, Okyay P, Ata O, Okuyanoglu S. A descriptive study of street children living in a southern city of Turkey. Turk J Pediatr. 2004;46:131–46. [PubMed] [Google Scholar]
- 65.Towe VL, ul Hasan S, Zafar ST, Sherman SG. Street life and drug risk behaviors associated with exchanging sex among male street children in Lahore, Pakistan. J Adolesc Health. 2009;44:222–8. doi: 10.1016/j.jadohealth.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kurtzman T, Otsuka K, Wahl R. Inhalant abuse by adolescents. J Adolesc Health. 2001;28:170–80. doi: 10.1016/s1054-139x(00)00159-2. [DOI] [PubMed] [Google Scholar]
- 67.World Health Organization (WHO) [accessed 19 March 2013];Psychoactive Substance Use Among Adolescents. ••. Available at: http://www.who.int/substance_abuse/activities/prevention_factsheets/en/index.htmln.d. Available at: http://www.who.int/substance_abuse/activities/prevention_factsheets/en/index.html.
- 68.Dell CA, Gust SW, MacLean S. Global issues in volatile substance misuse. Subst Use Misuse. 2011;46:1–7. doi: 10.3109/10826084.2011.580169. [DOI] [PubMed] [Google Scholar]
- 69.Dell CA. Youth Volatile Solvent Abuse Frequently Asked Questions. Ottawa, Ontario: Canadian Centre for Substance Abuse; 2006. [Google Scholar]
- 70.Baskin-Sommers A, Sommers I. The co-occurrence of substance use and high-risk behaviors. J Adolesc Health Care. 2006;38:609–11. doi: 10.1016/j.jadohealth.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 71.Duncan KC, Reading C, Borwein AM, Murray MC, Palmer A, Michelow W, et al. HIV incidence and prevalence among aboriginal peoples in Canada. AIDS Behav. 2011;15:214–27. doi: 10.1007/s10461-010-9792-y. [DOI] [PubMed] [Google Scholar]
- 72.Dell D, Hopkins C. Residential volatile substance misuse treatment for indigenous youth in Canada. Subst Use Misuse. 2011;46:107–13. doi: 10.3109/10826084.2011.580225. [DOI] [PubMed] [Google Scholar]
- 73.CBC News. Living conditions for First Nations ‘unacceptable’: Fontaine. Feb 6, 2007. [Google Scholar]
- 74.Smart RG, Arif A, Hughes PH, Medina-Mora ME, Navaratnam V, Varma VK, et al. Drug Use Among Non-Student Youth. Geneva: World Health Organization; 1981. [PubMed] [Google Scholar]