Abstract
The present randomised trial investigated the effects of feeding Zambian infants from 6 to 18 months old either a richly or basal micronutrient-fortified complementary/replacement food on gut integrity and systemic inflammation. Blood samples were obtained from all infants (n 743) at 6 and 18 months for the assessment of serum C-reactive protein (CRP) and α1-acid glycoprotein (AGP). A subsample of 502 infants, selected from the main cohort to include a larger proportion of infants with HIV-positive mothers, was assigned to lactulose/mannitol gut permeability tests. Lactulose:mannitol (L:M) ratio analyses were adjusted for baseline urinary L:M ratio, socio-economic status, mother’s education, season of birth and baseline stunting, and stratified by maternal antenatal HIV status, child’s sex, concurrent breast-feeding status and anaemia at baseline. There was no significant difference in geometric mean L:M ratio between the richly fortified and basal-fortified porridge arms at 12 months (0·47 (95% CI 0·41, 0·55) v. 0·41 (95% CI 0·34, 0·49); P=0·16 adjusted). At 18 months, the richly fortified porridge group had a significantly higher geometric mean L:M ratio than the basal-fortified group (0·23 (95% CI 0·19, 0·28) v. 0·15 (95% CI 0·12, 0·19); P=0·02 adjusted). This effect was evident for all stratifications, significantly among boys (P=0·04), among the infants of HIV-negative mothers (P=0·01), among the infants of HIV-negative mothers not concurrently breast-fed (P=0·01) and among those who were not anaemic at baseline (P=0·03). CRP, but not AGP, was positively associated with L:M ratio, but there were no significant effects of the diet on either CRP or AGP. In conclusion, a richly fortified complementary/replacement food did not benefit and may have worsened intestinal permeability.
Keywords: Micronutrient-fortified diets, Gut permeability, Systemic inflammation, HIV exposure
Early-life nutrition, especially during the first 2 years, is critical for human development(1). Growth faltering in infancy establishes a trajectory for lifelong health of the individual and, in populations, has profound implications for societal development. Growth faltering has special pertinence in regions undergoing economic and nutrition transition(2,3) such as urban Zambia, where the ‘double-burden of malnutrition’ is emergent(4). The prevalence of stunting among children in Zambia is considered severe at 25% among 6- to 8-month-old infants and 59 % among 18- to 23-month-old children nationally(5). Micronutrient deficiencies are well documented among infants in Zambia(6-9) and are associated with linear growth retardation(10).
Stunting and micronutrient deficiencies are not simply due to inadequate food intake(1). The ‘nutrition–infection paradigm’(11) and synergism of inadequate diet and infection in childhood growth faltering are well documented. Mucosal enteropathy resulting from infection can increase nutrient loss by maldigestion and malabsorption, and can increase nutritional requirements through inflammation(12,13). The intestinal epithelium is the major interface between environmental factors (e.g. diet, pathogens) and systemic health (e.g. nutritional status, immune responses), and its integrity is a key, though often neglected, consideration in the effectiveness of nutrition interventions. Impaired gut permeability, as assessed by urinary dual-sugar permeability tests, has been associated with growth faltering(12-15), malnutrition(12) and parasitic infection(16) in developing countries. Mucosal barrier damage was associated with systemic acute-phase C-reactive protein (CRP) and lipopoly-saccharide-binding protein among adult haematology patients(17), but neither α1-acid glycoprotein (AGP) nor IgG was associated with gut permeability among Bangladeshi infants(15).
Micronutrient supplementation studies, particularly of vitamin A and Zn, have shown improvements in gut integrity as assessed by urinary dual-sugar permeability tests. Maternal vitamin A supplementation prevented the deterioration of gut integrity of HIV-infected infants in South Africa(18). McCullough et al.(14) reviewed studies documenting improvements in gut integrity following vitamin A supplementation of healthy infants in India. Zn supplementation has improved gut integrity among children with diarrhoeal disease in Bangladesh(19,20), healthy adults and those with Crohn’s disease(21,22) and in cell and animal models of gut epithelial damage(21,23). Fe repletion of anaemic infants and young children through oral Fe supplementation significantly reduced gut permeability(24). Elsewhere, Hb concentrations were negatively associated with mucosal damage among Nepalese children(13).
The aim of the present study is to investigate the effects of locally produced complementary/replacement foods, fortified with micronutrients, on gut integrity, as assessed by urinary dual-sugar permeability tests, and systemic inflammation, as assessed by acute-phase protein (APP) concentrations, among infants aged 6–18 months in the Chilenje Infant Growth, Nutrition and Infection Study (CIGNIS).
Experimental methods
Subjects and study design
The CIGNIS trial was conducted in Chilenje, a middle-class suburb of Lusaka, Zambia, between September 2005 and July 2009. Details of the study protocol, porridge composition and primary outcomes of the project have been presented elsewhere(25). Families were recruited through the child health section of a government clinic on the same site as the project clinic. Infants were eligible if they were 6 months ± 2 weeks old, in good health generally and if their parent/guardian gave written consent to attend monthly clinic visits for the next year, feed the infant the allocated project porridge, allow the infant undergo tests including blood and urine sampling at 6, 12 and 18 months and have the child tested for HIV at 18 months old. Maternal HIV status was not tested, but recorded from antenatal charts and interview as ‘positive’, ‘negative’ or ‘unknown’. Sociodemographic information was obtained by a questionnaire. Infants were randomised to either a richly fortified porridge mix to meet WHO recommendations for infants aged 9–11 months with low breast milk intakes(26) or a basal porridge mix fortified with micronutrient levels planned for maize fortification in Zambia(27). The porridges, based on maize, beans, bambaranuts and groundnuts, were locally produced by Quality Commodities Limited, Lusaka, Zambia. Micronutrient premixes were prepared by DSM, Johannesburg, South Africa. The Fe fortificant used in both porridges was ferrous fumarate.
Urinary dual-sugar permeability tests
At 6, 12 and 18 months, urinary dual-sugar tests to assess gut integrity were conducted based on methods described previously(28,29). All infants of mothers who tested HIV-positive antenatally or with unknown HIV status and every second child of mothers who tested HIV-negative antenatally were assigned to the urinary dual-sugar permeability test. Children received via a syringe 2 ml/kg body weight of an oral dose of 200 mg lactulose/ml (C12H22O11; molecular weight 342·3) and 50 mg mannitol/ml (C6H14O6; molecular weight 182·2) in sterile water. Urine bags containing cotton wool were applied and plastic pants worn while urine was collected for 5 h. Samples were mixed at the clinic before aliquoting, freezing and storage at −80°C in the University Teaching Hospital (Lusaka, Zambia). Urine samples were transported on dry ice to the UK for analysis at the London School of Hygiene and Tropical Medicine (LSHTM). Lactulose and mannitol concentrations in urine samples were measured using enzymatic colorimetric techniques, as described previously(30,31), adapted to a ninety-six-well plate format (P. Lunn; Human Nutrition Research, Cambridge, UK). All reagents, unless stated otherwise, were purchased from Sigma Aldrich (Poole, UK). Lactulose in standards, samples and quality control (QC) material was converted through a series of enzymatic reactions catalysed by β-galactosidase, hexokinase, phosphoglucoisomerase and glucose-6-phosphate dehydrogenase to glucose-6-phosphate, with NADPH as a side product. The absorbance of NADPH, measured at 340 nm, was directly proportionate to fructose concentration. Lactulose concentrations were determined by the subtraction of endogenous fructose concentrations of samples incubated without β-galactosidase from those with β-galactosidase. Mannitol in standards, samples and QC material was converted through enzymatic reactions catalysed by mannitol dehydrogenase (Biocatalysts, Cardiff, UK) and hexokinase to fructose-6-phopshate, with NADH as a side product. The absorbance of NADH, measured at 340 nm, was directly proportionate to mannitol concentration. The inter-assay CV of the 250 and 1000 mg/l QC material for the lactulose assay were 10·4 and 5·6 %, respectively. The inter-assay CV of the 250 and 1000 mg/l QC material for the mannitol assay were 9·6 and 9·8 %, respectively.
Acute-phase proteins
At 6 and 18 months, 5 ml of blood samples were collected by venepuncture (Vacutainer 23G butterfly system; Becton Dickinson, Oxford, UK) for micronutrient and APP analysis. Samples were centrifuged and serum was divided into aliquots, and stored at −80°C in the University Teaching Hospital. Samples for APP analyses were sent on dry ice to the LSHTM. CRP was measured by ELISA using antibodies from Abcam (Cambridge, UK) and standards from Dade Behring (Milton Keynes, UK) according to a protocol detailed elsewhere(32). The inter-assay CV for the National Institute for Biological Standards and Control (NIBSC) supplied QC material was 12·6 %. AGP was analysed on a COBAS FARA autoanalyser (Roche, Welwyn Garden City, UK) using a commercial immunoturbidometric assay (Kamiya Biomedical, Seattle, WA, USA). The inter-assay CV for the high and low QC material were 6·1 and 7·1 %, respectively.
Statistical analysis
Lactulose:mannitol (L:M) ratios, CRP and AGP concentrations were transformed on the natural logarithmic scale to normalise distributions of skewed raw data. A value of 1 was added to all lactulose concentrations so that logs could be calculated even for zero values; since the mean lactulose concentration was 568 mg/l, this would have had a minimal effect on the geometric mean L:M ratio. Geometric means of the L:M ratio, CRP and AGP were calculated separately for the intervention arms, and separately at 6, 12 and 18 months. Baseline characteristics and reported illness within the past 3 d were compared in those tested and not tested for L:M ratio, CRP and AGP separately using a χ2 or t test for categorical or continuous variables, respectively. Transformed L:M ratio, CRP and AGP were compared between the intervention arms using a two-sample t test at 12 and 18 months (crude analysis). Regression coefficients were transformed back to the original scale to provide a ratio of the geometric means. Baseline L:M ratio, socio-economic status determined from principal component analysis of an asset score(33), season of birth (early dry: June to August; late dry: September to November; early rainy: December to February; late rainy: March to May) and baseline stunting defined as less than −2 sd of length-for-age using the WHO child growth standards(34) were considered potential a priori confounders, and adjusted analyses using multivariable linear regression were performed including these variables. Child’s sex, maternal HIV status, concurrent breast-feeding status based on maternal HIV status and anaemia at 6 months were considered a priori to be potential effect modifiers and stratified analyses were performed for these variables. Additional non-a priori stratified analysis by child’s HIV status, tested by PCR at 18 months, was conducted at 18 months only. Tests of interaction were also performed between the intervention arm and the potential effect modifiers. A random slope, random intercept mixed-effects linear regression model was employed to explore the effect of the intervention on L:M ratio over the entire study period. The model included a priori confounding factors and covariates associated with missingness to correct the results for missing values in the outcome(35). All analyses were conducted in Stata version 11.0 (College Station, TX, USA).
Ethical approval and trial registration
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the ethics committees of the University of Zambia and LSHTM. Written informed consent was obtained from all parents/guardians. The study is registered as ISRCTN37460449 (www.controlled-trials.com/mrct).
Results
Subject recruitment and characteristics
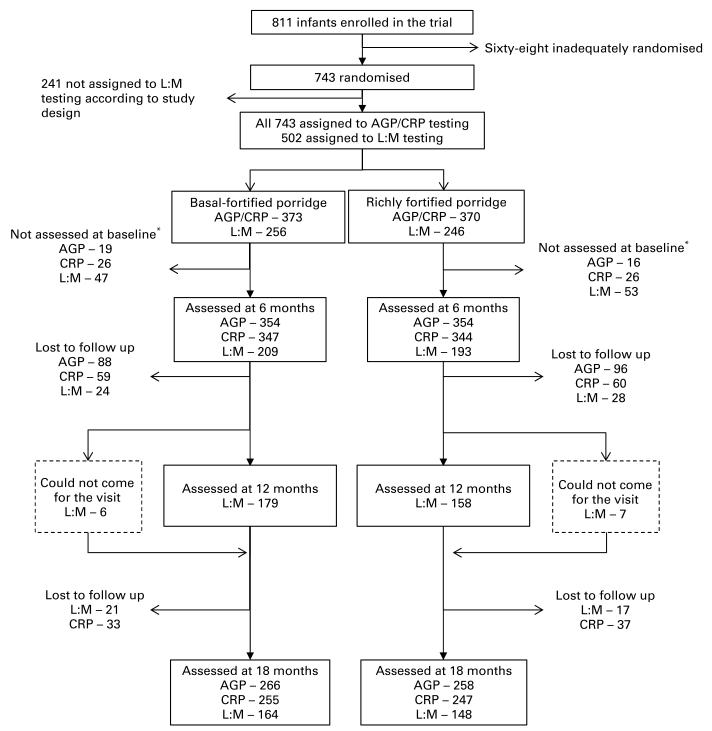
A total of 811 infants were enrolled in the CIGNIS (Fig. 1). Of these infants, sixty-eight were inadequately randomised between May and June 2007 following an inadvertent protocol violation by clinic staff. Due to temporary unavailability of one of the porridges at the clinic, infants recruited in this time period were sequentially provided with the available porridge. Following detection of this protocol violation, these sixty-eight children continued on the programme but were removed from the analysis. Of the adequately randomised infants, 502 were assigned to the urinary dual-sugar permeability test, as described above. Of these infants, 100 were not assessed at baseline for reasons including mother’s refusal and a number of occasions when dual-sugar solution was not available in the clinic. The assigned children who did and did not receive the dual-sugar permeability test were compared by baseline characteristics and reported illness within the past 3 d. The children who did not receive the dual-sugar permeability test at 6 months were less likely to have HIV-positive mothers (5·4 v. 44·3 %; P<0·001) and were more likely to be breast-fed for longer than 6 months (89·0 v. 76·9 %; P=0·007); maternal HIV status and breast-feeding duration were closely linked in this population(36). There was also weak evidence that mothers of children with missing baseline data were slightly younger (25·4 (sd 4·8) v. 26·7 (sd 5·9) years; P=0·06) and from a higher socio-economic class (P=0·07). There is no suggestion that those with missing data for the L:M ratio were more likely to be unwell or have poor growth (data not shown). At baseline, fifty-two and thirty-five infants were not assessed for CRP and AGP, respectively. These infants were compared, as above, with those who were tested for serum APP. Missing CRP data at 6 months were associated with a smaller proportion of maternally HIV-exposed infants (11·5 v. 21·9 %; P=0·04), lower maternal educational achievement (19·2 v. 35·0 % attaining primary education only; P=0·03) and a greater incidence of infant illness in the past 3 d (9·6 v. 3·9 %; P=0·05). Missing AGP data at 6 months were not associated with any baseline characteristics. Subject characteristics of infants and mothers by study arm (Table 1) were similar except that there appeared to be a slight excess of girls in the richly fortified porridge group.
Fig. 1.
Flow diagram of participants through the Chilenje Infant Growth, Nutrition and Infection Study. * Missing lactulose:mannitol (L:M; urinary dual-sugar permeability test) ratio results at baseline are due to the following reasons: mother refused (n 62), unavailability of the L:M dose solution (n 10), infant death between recruitment and testing (n 1), mother incorrectly reported a negative HIV status (n 4), staff error or insufficient urine (n 23). Missing baseline α1-acid glycoprotein (AGP) and C-reactive protein (CRP) results are due to the insufficient availability of blood samples.
Table 1.
Characteristics of infants and mothers assigned to the urinary dual-sugar permeability test (lactulose:mannitol (L:M)) and acute-phase protein (APP) analysis (Mean values, standard deviations, number of subjects and percentages)
| Assigned to L:M ratio (n 502) |
Assigned to APP (n 743) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Basal-fortified porridge arm (n 256) |
Richly fortified porridge arm (n 246) |
Basal-fortified porridge arm (n 373) |
Richly fortified porridge arm (n 370) |
|||||||||
| n | % | n | % | n | % | n | % | |||||
| Infants’ characteristics | ||||||||||||
| Female | 124 | 48·4 | 142 | 57·7 | 182 | 488 | 204 | 55·1 | ||||
| Birth weight (kg) | ||||||||||||
| Mean | 3·1 | 3·1 | 3·1 | 3·1 | ||||||||
| SD | 0·5 | 0·5 | 0·5 | 0·5 | ||||||||
| Stunted* | 34 | 13·3 | 27 | 10·9 | 51 | 13·7 | 40 | 10·8 | ||||
| Anaemic† | 94 | 36·7 | 102 | 41·5 | 140 | 37·5 | 149 | 40·3 | ||||
| Breast-feeding duration | ||||||||||||
| Never | 22 | 8·6 | 20 | 8·1 | 22 | 5·9 | 21 | 5·7 | ||||
| < 6 months | 34 | 13·3 | 28 | 11·4 | 39 | 10·5 | 29 | 7·8 | ||||
| ≥ 6 months | 200 | 78·1 | 198 | 80·5 | 312 | 83·6 | 320 | 86·5 | ||||
| Season of birth‡ | ||||||||||||
| Early dry | 90 | 35·2 | 72 | 29·3 | 123 | 33·0 | 113 | 30·5 | ||||
| Late dry | 59 | 23·0 | 61 | 24·8 | 83 | 22·3 | 93 | 25·1 | ||||
| Early wet | 48 | 18·8 | 51 | 20·7 | 74 | 19·8 | 72 | 19·5 | ||||
| Late wet | 59 | 23·0 | 62 | 25·2 | 93 | 24·9 | 92 | 24·9 | ||||
| Mothers’ characteristics | ||||||||||||
| Age (years) | ||||||||||||
| Mean | 26·4 | 26·5 | 26·0 | 26·4 | ||||||||
| sd | 5·5 | 5·9 | 5·7 | 5·8 | ||||||||
| Antenatal HIV§ status | ||||||||||||
| Negative | 144 | 56·2 | 134 | 54·5 | 261 | 70·0 | 258 | 69·7 | ||||
| Positive | 79 | 30·9 | 78 | 31·7 | 79 | 21·2 | 78 | 21·1 | ||||
| Unknown | 33 | 12·9 | 34 | 13·8 | 33 | 8·8 | 34 | 9·2 | ||||
| Education | ||||||||||||
| Primary or less | 80 | 31·2 | 98 | 39·8 | 123 | 33·0 | 129 | 34·9 | ||||
| Secondary | 112 | 43·8 | 78 | 31·7 | 157 | 42·1 | 127 | 34·3 | ||||
| College/university | 64 | 25·0 | 70 | 28·5 | 93 | 24·9 | 114 | 30·8 | ||||
| Socio-economic score | ||||||||||||
| Low | 84 | 32·8 | 87 | 35·4 | 127 | 34·0 | 123 | 33·2 | ||||
| Middle | 107 | 41·8 | 84 | 34·1 | 151 | 40·5 | 136 | 36·8 | ||||
| High | 65 | 25·4 | 75 | 30·5 | 95 | 25·5 | 111 | 30·0 | ||||
Stunted defined as less than −2sd of length-for-age using the WHO child growth standards.
Anaemia defined as > 105 g/l.
Early dry (June to August); late dry (September to November); early rainy (December to February); late rainy (March to May).
All infants of HIV-positive mothers and mothers of unknown status and every second child of HIV-negative mothers were assigned to L:M ratio analysis. All infants enrolled in the Chilenje Infant Growth, Nutrition and Infection Study were assigned to APP analysis.
Urinary dual-sugar permeability tests
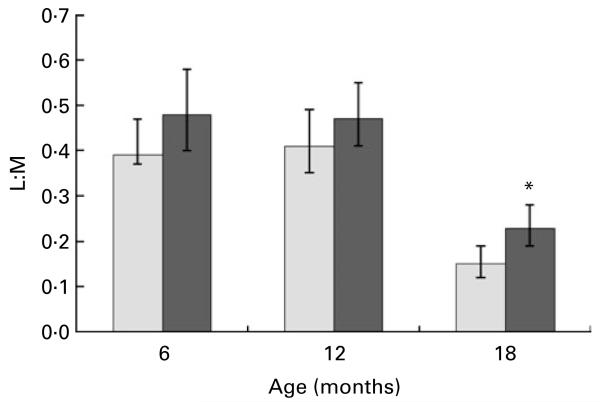
Crude analyses of dual-sugar permeability results at 6, 12 and 18 months are presented in Fig. 2. The geometric mean of the L:M ratio was similar in both trial arms at both 6 months (basal: 0·39 (95% CI 0·32, 0·49) v. richly fortified: 0·48 (95% CI 0·40, 0·58)). At 12 months, there was no difference between the geometric mean of the L:M ratio in the basal and richly fortified groups (0·41 (95% CI 0·35, 0·49) v. 0·47 (95% CI 0·41, 0·55), respectively; P=0·21 crude analysis). At 18 months, the geometric mean of the L:M ratio was lower than at younger ages and was significantly lower in the basal group (0·15 (95% CI 0·12, 0·19)) compared with the richly fortified group (0·23 (95% CI 0·19, 0·28); P=0·006 crude analysis).
Fig. 2.
Lactulose:mannitol (L:M) ratio at 6, 12 and 18 months in the basal-fortified ( ) and richly fortified (
) and richly fortified ( ) study arms. Values are geometric means of the L:M ratio, with 95% CI represented by vertical bars. * Mean values were significantly different (P=0·006; crude analysis).
) study arms. Values are geometric means of the L:M ratio, with 95% CI represented by vertical bars. * Mean values were significantly different (P=0·006; crude analysis).
There was no evidence of the differential effects of the diet on the L:M ratio at 12 months in adjusted and stratified analysis (Table 2). There was no statistical evidence of an interaction between the intervention arm and the a priori potential effect modifiers of child’s sex (P=0·77), maternal HIV status (P=0·56), current breast-feeding (P=0·90) and baseline anaemia (P=0·63) at 12 months. After adjustment, the L:M ratio at 18 months remained significantly higher in the richly fortified arm compared with the basal-fortified arm (adjusted ratio 1·42 (95% CI 1·06, 1·92); P=0·02; Table 3). When stratified by child’s sex, the effect of the intervention on the L:M ratio was significant among males (adjusted ratio 1·57 (95% CI 1·02, 2·42); P=0·04; Table 3). When stratified by maternal HIV status, there was some suggestion that the effect of the intervention on the L:M ratio was greater among children of HIV-negative mothers (adjusted ratio 1·81 (95% CI 1·15, 2·84); P=0·01; Table 3). When stratified by breast-feeding status, not currently breast-feeding infants of HIV-negative mothers who were given the richly fortified porridge had a considerably higher L:M ratio than those given the basal porridge (adjusted ratios 2·28 (95% CI 1·26, 4·13); P=0·01; Table 3). By stratified analysis, there was evidence that infants who were not anaemic at baseline in the richly fortified arm had a higher L:M ratio than those in the basal-fortified arm (adjusted ratio 1·54 (95% CI 1·05, 2·26); P=0·03; Table 3). The effect of the intervention was significant among HIV-negative children (adjusted ratio 1·40 (95% CI 1·04, 1·90); P=0·03) and was not evident among the ten HIV-positive children at 18 months (adjusted ratio 2·40 (95% CI 0·46, 12·60); P=0·30; Table 3). Tests of interaction showed no statistical evidence of an interaction between the intervention arm and the a priori potential effect modifiers of child’s sex (P=0·48), maternal HIV (P=0·18) and baseline anaemia (P=0·49) at 18 months. There was no statistical evidence of an interaction between the intervention arm and child’s HIV status at 18 months (P=0·53). There was weak evidence to suggest an interaction between diet and breast-feeding among HIV-negative mothers (P=0·09) and breast-feeding among HIV-positive mothers (P=0·10). For all subgroups tested at 18 months, point estimates of L:M ratio values for infants in the richly fortified study arm were higher than those in the basal arm.
Table 2.
Effects of basal-fortified and richly fortified porridge on lactulose:mannitol (L:M) at 12 months (Geometric means, number of subjects, ratios and 95% confidence intervals)
| Basal-fortified porridge arm |
Richly fortified porridge arm |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Geometric mean |
95% CI | n | Geometric mean |
95% CI | Crude ratio* |
95% CI | P | Adjusted ratio*†‡ |
95% CI | P | |
| All children | 178 | 0·41 | 0·35, 0·49 | 158 | 0·47 | 0·41, 0·55 | 1·16 | 0·92, 1·45 | 0·21 | 1·18 | 0·93, 1·49 | 0·16 |
| Sex | ||||||||||||
| Boys | 94 | 0·39 | 0·30, 0·49 | 65 | 0·45 | 0·36, 0·56 | 1·16 | 0·83, 1·63 | 0·38 | 1·21 | 0·86, 1·70 | 0·28 |
| Girls | 84 | 0·44 | 0·34, 0·56 | 93 | 0·49 | 0·40, 0·60 | 1·12 | 0·82, 1·54 | 0·47 | 1·13 | 0·82, 1·56 | 0·46 |
| Maternal HIV status§ | ||||||||||||
| Negative | 85 | 0·44 | 0·36, 0·53 | 67 | 0·55 | 0·44, 0·68 | 1·25 | 0·89, 1·75 | 0·20 | 1·30 | 0·91, 1·84 | 0·15 |
| Positive | 69 | 0·35 | 0·25, 0·49 | 66 | 0·39 | 0·31, 0·50 | 1·12 | 0·78, 1·60 | 0·54 | 1·13 | 0·78, 1·63 | 0·53 |
| Currently breast-feeding among HIV-negative mothers | ||||||||||||
| No | 10 | 0·22 | 0·13, 0·38 | 6 | 0·32 | 0·25, 0·40 | 1·44 | 0·59, 3·53 | 0·42 | 1·77 | 0·71, 4·45 | 0·22 |
| Yes | 74 | 0·47 | 0·39, 0·58 | 61 | 0·58 | 0·46, 0·73 | 1·22 | 0·90, 1·64 | 0·20 | 1·26 | 0·92, 1·73 | 0·15 |
| Currently breast-feeding among HIV-positive mothers | ||||||||||||
| No | 58 | 0·30 | 0·21, 0·43 | 54 | 0·36 | 0·28, 0·47 | 1·21 | 0·78, 1·89 | 0·39 | 1·27 | 0·81, 1·99 | 0·30 |
| Yes | 11 | 0·83 | 0·43, 1·60 | 12 | 0·57 | 0·33, 0·96 | 0·68 | 0·26, 1·81 | 0·44 | 0·92 | 0·33, 2·53 | 0·87 |
| Anaemia at 6 months∥ | ||||||||||||
| No | 117 | 0·36 | 0·29, 0·44 | 89 | 0·42 | 0·35, 0·50 | 1·15 | 0·86, 1·54 | 0·33 | 1·20 | 0·89, 1·61 | 0·23 |
| Yes | 60 | 0·52 | 0·39, 0·70 | 65 | 0·55 | 0·43, 0·71 | 1·07 | 0·74, 1·54 | 0·74 | 1·07 | 0·73, 1·56 | 0·74 |
Ratio in geometric means.
Adjusted for baseline L:M ratio, socio-economic status, mother's education, season of birth and stunting.
L:M ratio measured among 179 and 158 subjects in the basal-fortified and richly fortified porridge arms, but missing data on stunting for one subject in the basal arm.
HIV status not known for twenty-three and nineteen mothers in the basal-fortified and richly fortified treatment arms.
Anaemia defined as < 105 g/l; data for six subjects were missing.
Table 3.
Effects of basal-fortified and richly fortified porridge on lactulose:mannitol (L:M) at 18 months (Geometric means, number of subjects, ratios and 95% confidence intervals)
| Basal-fortified porridge arm |
Richly fortified porridge arm |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n * | Geometric mean |
95% CI | n | Geometric mean |
95% CI | Crude ratio† |
95% CI | P | Adjusted ratio†‡ |
95% CI | P | |
| All children | 163 | 0·15 | 0·12, 0·19 | 148 | 0·23 | 0·19, 0·28 | 1·5 | 1·12, 2·00 | 0·006 | 1·42 | 1·06, 1·92 | 0·02 |
| Sex | ||||||||||||
| Boys | 89 | 0·14 | 0·10, 0·19 | 63 | 0·23 | 0·17, 0·32 | 1·68 | 1·10, 2·57 | 0·02 | 1·57 | 1·02, 2·42 | 0·04 |
| Girls | 74 | 0·17 | 0·13, 0·22 | 85 | 0·22 | 0·17, 0·29 | 1·32 | 0·88, 1·98 | 0·18 | 1·28 | 0·84, 1·94 | 0·25 |
| Maternal HIV status§ | ||||||||||||
| Negative | 78 | 0·15 | 0·10, 0·20 | 67 | 0·26 | 0·19, 0·35 | 1·78 | 1·13, 2·73 | 0·01 | 1·81 | 1·15, 2·84 | 0·01 |
| Positive | 62 | 0·15 | 0·11, 0·21 | 61 | 0·20 | 0·15, 0·28 | 1·33 | 0·82, 2·14 | 0·25 | 1·16 | 0·71, 1·89 | 0·56 |
| Currently breast-feeding among HIV-negative mothers | ||||||||||||
| No | 46 | 0·10 | 0·06, 0·15 | 42 | 0·20 | 0·13, 0·29 | 2·04 | 1·16, 3·58 | 0·01 | 2·28 | 1·26, 4·13 | 0·01 |
| Yes | 32 | 0·26 | 0·16, 0·43 | 25 | 0·39 | 0·25, 0·63 | 1·51 | 0·74, 3·05 | 0·25 | 1·57 | 0·76, 3·25 | 0·22 |
| Currently breast-feeding among HIV-positive mothers | ||||||||||||
| No | 56 | 0·14 | 0·10, 0·20 | 55 | 0·19 | 0·13, 0·26 | 1·31 | 0·81, 2·11 | 0·27 | 1·20 | 0·72, 1·99 | 0·48 |
| Yes | 6 | 0·30 | 0·12, 0·76 | 6 | 0·45 | 0·14, 1·41 | 1·52 | 0·35, 6·51 | 0·57 | 1·03 | 0·21, 5·12 | 0·97 |
| Child HIV status | ||||||||||||
| Negative | 158 | 0·15 | 0·12, 0·18 | 140 | 0·22 | 0·18, 0·26 | 1·47 | 1·09, 1·97 | 0·01 | 1·40 | 1·04, 1·90 | 0·03 |
| Positive | 4 | 0·40 | 0·10, 1·56 | 6 | 0·76 | 0·18, 3·18 | 1·90 | 0·37, 9·75 | 0·44 | 2·40 | 0·46, 12·6 | 0·30 |
| Anaemia at 6 months∥ | ||||||||||||
| No | 104 | 0·13 | 0·10, 0·18 | 83 | 0·21 | 0·16, 0·29 | 1·59 | 1·09, 2·31 | 0·02 | 1·54 | 1·05, 2·26 | 0·03 |
| Yes | 58 | 0·19 | 0·14, 0·27 | 60 | 0·26 | 0·20, 0·33 | 1·35 | 0·84, 2·17 | 0·21 | 1·24 | 0·77, 2·02 | 0·37 |
L:M ratio measured among 164 and 148 subjects in the basal-fortified and richly fortified porridge arms, but missing data on stunting for one subject in the basal arm.
Ratio in geometric means.
Adjusted for baseline L:M ratio, socio-economic status, mother’s education, season of birth and stunting.
HIV status not known for twenty-three and nineteen mothers in the basal-fortified and richly fortified treatment arms.
Anaemia defined as < 105 g/l; data for six subjects were missing.
In a random slope, random intercept mixed-effects linear regression model, after adjusting for visit, a priori confounding factors and characteristics associated with missingness (breast-feeding duration, mother’s age and HIV status), there was evidence of an effect of the rich porridge intervention on the L:M ratio over the whole study period (adjusted ratio 1·11 (95% CI 1·04, 1·19); P=0·002).
Acute-phase proteins
At baseline, the geometric means of serum concentrations of CRP in the basal-fortified (0·52 (95% CI 0·45, 0·60)) and richly fortified (0·46 (95% CI 0·40, 0·54)) groups were similar. At 6 months of age, 4·1 % of the infants had CRP concentrations in excess of 5 mg/l. The geometric means of serum AGP concentration in the basal-fortified (0·73 (95% CI 0·69, 0·77)) and richly fortified (0·72 (95% CI 0·69, 0·75)) groups were also similar at baseline. At 6 months of age, 21·1 % of the infants had AGP concentrations in excess of 1 g/l. At 18 months, there were no differences in serum CRP concentrations between the basal-fortified (0·47 (95% CI 0·39, 0·56)) and richly fortified (0·54 (95% CI 0·45, 0·64)) groups. Elevated CRP concentrations were observed in 3·6 % of the infants. There were also no differences in serum AGP concentrations between the basal-fortified (0·74 (95% CI 0·68, 0·80)) and richly fortified (0·76 (95% CI 0·70, 0·83)) groups. At 18 months, 30·5 % of the infants had elevated AGP concentrations.
The effects of the diet on the proportion of infants with elevated CRP and AGP concentrations at 18 months were also analysed by multivariate linear regression, adjusted for baseline CRP or AGP, respectively, socio-economic status, season of birth and stunting, and stratified by maternal HIV status, child’s sex, concurrent breast-feeding, and anaemia at 6 months. There were no significant effects of the diet on the proportion of infants with elevated CRP or AGP (data not shown). CRP concentrations were correlated with AGP (r 0·32; P<0·001) and L:M ratio (r 0·13; P=0·02) at 18 months. There was no evidence of an association between AGP and L:M ratio at 18 months.
Discussion
The present study investigated the effects of two locally produced complementary/replacement foods, basal-fortified and richly fortified with micronutrients, on gut integrity and systemic inflammation among Zambian infants at 6 and 18 months. Presented elsewhere, the richly fortified porridge improved Fe status at 18 months assessed by Hb, ferritin and serum transferrin receptors but had no significant effect overall on the proportion of infants stunted, rate of hospital referral or death(25). Future work will explore associations between gut integrity and other outcomes of the trial, including anthropometric indices and diarrhoeal disease.
In the present study, intestinal permeability was significantly higher at 18 months in the richly fortified porridge arm compared with the basal-fortified porridge arm, albeit an 11% increase. This effect remained after adjustment for baseline L:M ratio, socio-economic status, mother’s education, season of birth and stunting. There was no statistical evidence that the effect of the intervention was modified by child’s sex, maternal HIV status, concurrent breast-feeding and baseline anaemia, although there was some suggestion that the effect of the intervention was greater among children of HIV-negative mothers who were breast-feeding at 18 months. It is possible that, in the CIGNIS cohort, mothers of children with illness associated with higher gut permeability chose to breast-fed for longer. Among Nepalese children weaned relatively late, a positive association between duration of breast-feeding and the L:M ratio has been found(37). There were no differences in hospital referrals for diarrhoea between the treatment groups(25) nor in clinic-treated diarrhoea or monthly maternal reports of diarrhoeal symptoms (A Mullen, N Larke and S Filteau, unpublished results) despite the increased intestinal permeability of children in the richly fortified arm. Furthermore, although raised intestinal permeability is sometimes associated with poor child growth, the richly fortified porridge did not impair the growth of CIGNIS children. There were no significant differences in APP concentrations between the porridge arms at 18 months.
Impaired intestinal permeability in infants in developing countries is associated with enteropathy, infection and growth faltering(12,15,16,38,39). No cut-off for a ‘normal’ L:M ratio has been recognised. Intestinal permeability as interpreted by the L:M ratio in the CIGNIS cohort decreased over time and values were relatively similar to those published from the Gambia (children aged 2–16 months; geometric means at 2-monthly intervals range from 0·17 to approximately 0·4)(39), Peru (children <36 months with rotaviral, cryptosporidial infects and healthy controls; geometric means of 0·67, 0·76 and 0·29, respectively)(16) and Bangladesh (children aged 3–15 months; geometric mean of 0·15)(15). Intestinal integrity in infants has been improved through supplementation with vitamin A(14,18) and Zn(19,20). Fe-deficiency anaemia may be associated with impaired intestinal integrity(13,24), although evidence suggests a complex interaction of Fe status with gut permeability, potentially mediated through innate immune responses and oxidative stress. A two-by-two factorial intervention of Fe and multi-micronutrient supplements among schoolchildren in Lusaka found that Fe supplementation significantly increased the L:M ratio compared with the control group, and that Fe supplementation was the only predictor among the variables tested (including anthropometric indices, multi-micronutrient supplementation, parasitic infection and geophagy) of the L:M ratio(40). Review of Fe supplementation or fortification of milks or cereals demonstrated that, though not of public health concern, provision of Fe was associated with an increased risk of diarrhoea(41) and gastrointestinal infections(42) among children, especially among those Fe-replete at baseline. A previous study in Sprague–Dawley rats has indicated that an Fe-sufficient diet resulted in a significantly higher L:M ratio than an Fe-deficient diet(43). Fe overload of rats by subcutaneous injection, though inducing no change in gut permeability, induced significant morphological changes including a decrease in crypt depths and tissue Fe content, including the small- and large-intestinal walls(44). In vitro membrane damage and cellular death of Caco-2 cells(45) and oxidative DNA damage of HT29 colon carcinoma cells(46) following Fe exposure has been demonstrated. Latunde-Dada(47) reviewed ‘hemunology’ and the dynamic between the host’s tightly regulated mechanisms of Fe absorption, strategies to deprive pathogens of Fe and the host’s less-well-developed adaptations to rid the body of excess Fe. Unabsorbed, or unharnessed, dietary Fe may thus favour enteric pathogen growth(48). Zimmermann et al.(48) demonstrated increased enterobacteria and faecal cal-protectin, a marker of gut inflammation, following a 6-month intervention with a poorly absorbed Fe fortificant among children in Côte d’Ivoire. It would seem plausible in the present study that a higher L:M ratio observed in the richly fortified porridge arm at 18 months compared with the basal-fortified porridge arm may be associated with Fe status which was improved in the richly fortified porridge group(25), particularly since the effect was significant among infants who were not anaemic, interpreted by Hb concentration, at baseline. This has been supported by non-a priori unpublished findings investigating the effects of the diet on gut permeability of CIGNIS children at 18 months stratified by baseline transferrin receptor and ferritin status. Although the biological significance of the 11% increase in gut permeability from the richly fortified group is questionable, further research is warranted into understanding the potential effects of Fe fortification on gut permeability in infants and children with normal indices of Fe status.
Gut permeability has been associated with systemic inflammation in a limited number of studies. Campbell et al.(39) found that plasma endotoxin and IgG-endotoxin core antibody were related to mucosal enteropathy among Gambian infants. AGP and IgG were not associated with gut permeability among Bangladeshi infants(15). Faecal neopterin, a marker of intestinal infection, was not associated with gut permeability in Gambian infants(38). In the present study, AGP and CRP concentrations correlated with each other, but only CRP was associated with the L:M ratio at 18 months. The richly fortified diet had no effect on APP. If gut permeability mediates systemic inflammation, the present finding would cast further question on the biological significance of the main finding of the study. However, since the present and other studies have demonstrated a limited association between chosen systemic mediators of inflammation and gut permeability, it is likely that the effect of the diet on gut permeability is a local effect.
Understanding the ‘nutrition–infection paradigm’(11) should be a key component in evaluating the success of any nutrition intervention. The small intestine represents the frontier of absorption and innate immunology. The CIGNIS investigated the effects of micronutrients on the function of the small intestine among infants in Zambia, a population vulnerable to growth restriction. The results of the CIGNIS, and other studies, warrant further investigation into local interactions of key micronutrients with gut integrity, particularly in micronutrient-replete infants.
Acknowledgements
The CIGNIS was funded by The Bill and Melinda Gates Foundation with micronutrient premixes provided by DSM. The authors declare that there are no conflicts of interest. M. C. and staff at the Chilenje Clinic administered dual-sugar solutions, and collected blood and urine samples. M. Kapambwe prepared urine and blood samples at the University Teaching Hospital. L. G. and A. M. determined the lactulose, mannitol, CRP and AGP concentrations at the LSHTM, and A. Jackson provided assistance. N. L., D. M., S. F. and A. M. performed the statistical analysis at the LSHTM. A. M. was involved in the manuscript preparation, with input from all authors. The other members of the CIGNIS team are as follows: R. Gibson, U. A. Gompels, S. Jaffar, E. Kafwembe, M. Monze, M. Sinkala, A. Tomkins, R. Zulu, J. Siame, H. B. Mabuda, K. Baisley, H. Dale, A. Rehman, M. Bates, H. K. Bwalya, M. Chileshe, P. K. Kowa, M. Kumwenda, M. Likando, S. Mambwe, M. Muzyamba, A. Mwale, L. Nyaywa, H. Bima, L. Hackett, E. Njunju, S. Mwanza, N. Shampwaya, C. Kabanga, J. Chobo, W. Kapumba, C. Musonda, P. Soko.
Abbreviations
- AGP
α1-acid glycoprotein
- APP
acute-phase protein
- CIGNIS
Chilenje Infant Growth Nutrition and Infection Study
- CRP
C-reactive protein
- L:M
lactulose:mannitol
- LSHTM
London School of Hygiene and Tropical Medicine
- QC
quality control.
References
- 1.The World Bank . Nutrition as Central to Development: A Strategy for Large-Scale Action. The International Bank for Reconstruction and Development/The World Bank; Washington, DC: 2006. [Google Scholar]
- 2.Popkin BM. The shift in stages of the nutrition transition in the developing world differs from past experiences! Public Health Nutr. 2002;5:205–214. doi: 10.1079/PHN2001295. [DOI] [PubMed] [Google Scholar]
- 3.Prentice AM, Moore SE. Early programming of adult disease in resource poor countries. Arch Dis Child. 2005;90:429–432. doi: 10.1136/adc.2004.059030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azevedo M, Alla S. Diabetes in Sub-Saharan Africa: Kenya, Mali, Mozambique, Nigeria, South Africa and Zambia. Int J Diabetes Dev Ctries. 2008;28:101–108. doi: 10.4103/0973-3930.45268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Central Statistical Office. Ministry of Health. Tropical Diseases Research Centre. University of Zambia. Macro International Inc. Zambia Demographic and Health Survey 2007. CSO and Macro International, Inc.; Calverton, MD: 2009. [Google Scholar]
- 6.Hautvast JL, Tolboom JJ, Kafwembe EM, et al. Severe linear growth retardation in rural Zambian children: the influence of biological variables. Am J Clin Nutr. 2000;71:550–559. doi: 10.1093/ajcn/71.2.550. [DOI] [PubMed] [Google Scholar]
- 7.Gitau R, Makasa M, Kasonka L, et al. Maternal micronutrient status and decreased growth of Zambian infants born during and after the maize price increases resulting from the southern African drought of 2001-2002. Public Health Nutr. 2005;8:837–843. doi: 10.1079/phn2005746. [DOI] [PubMed] [Google Scholar]
- 8.van Rheenen PF, de Moor LT, Eschbach S, et al. A cohort study of haemoglobin and zinc protoporphyrin levels in term Zambian infants: effects of iron stores at birth, complementary food and placental malaria. Eur J Clin Nutr. 2008;62:1379–1387. doi: 10.1038/sj.ejcn.1602862. [DOI] [PubMed] [Google Scholar]
- 9.Kafwembe EM, Chipipa J, Njunju E, et al. The vitamin A status of Zambian children in a community of vitamin A supplementation and sugar fortification strategies as measured by the modified relative dose response (MRDR) test. Int J Vitam Nutr Res. 2009;79:40–47. doi: 10.1024/0300-9831.79.1.40. [DOI] [PubMed] [Google Scholar]
- 10.Engle PL, Black MM, Behrman JR, et al. International Child Development Steering Group. Strategies to avoid the loss of developmental potential in more than 200 million children in the developing world. Lancet. 2007;369:229–242. doi: 10.1016/S0140-6736(07)60112-3. [DOI] [PubMed] [Google Scholar]
- 11.Solomons NW. Malnutrition and infection: an update. Br J Nutr. 2007;98(Suppl. 1):S5–S10. doi: 10.1017/S0007114507832879. [DOI] [PubMed] [Google Scholar]
- 12.Lunn PG. The impact of infection and nutrition on gut function and growth in childhood. Proc Nutr Soc. 2000;59:147–154. doi: 10.1017/s0029665100000173. [DOI] [PubMed] [Google Scholar]
- 13.Panter-Brick C, Lunn PG, Langford RM, et al. Pathways leading to early growth faltering: an investigation into the importance of mucosal damage and immuno-stimulation in different socio-economic groups in Nepal. Br J Nutr. 2009;101:558–567. doi: 10.1017/S000711450802744X. [DOI] [PubMed] [Google Scholar]
- 14.McCullough FS, Northrop-Clewes CA, Thurnham DI. The effect of vitamin A on epithelial integrity. Proc Nutr Soc. 1999;58:289–293. doi: 10.1017/s0029665199000403. [DOI] [PubMed] [Google Scholar]
- 15.Goto R, Mascie-Taylor CG, Lunn PG. Impact of intestinal permeability, inflammation status and parasitic infections on infant growth faltering in rural Bangladesh. Br J Nutr. 2009;101:1509–1516. doi: 10.1017/S0007114508083554. [DOI] [PubMed] [Google Scholar]
- 16.Zhang Y, Lee B, Thompson M, et al. Lactulose–mannitol intestinal permeability test in children with diarrhoea caused by rotavirus and cryptosporidium. Diarrhoea Working Group, Peru. J Pediatr Gastroenterol Nutr. 2000;31:16–21. doi: 10.1097/00005176-200007000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Blijlevens NM, Donnelly JP, de Pauw BE. Prospective evaluation of gut mucosal barrier injury following various myeloablative regimens for haematopoietic stem cell transplant. Bone Marrow Transplant. 2005;35:707–711. doi: 10.1038/sj.bmt.1704863. [DOI] [PubMed] [Google Scholar]
- 18.Filteau SM, Rollins NC, Coutsoudis A, et al. The effect of antenatal vitamin A and beta-carotene supplementation on gut integrity of infants of HIV-infected South African women. J Pediatr Gastroenterol Nutr. 2001;32:464–470. doi: 10.1097/00005176-200104000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Roy SK, Behrens RH, Haider R, et al. Impact of zinc supplementation on intestinal permeability in Bangladeshi children with acute diarrhoea and persistent diarrhoea syndrome. J Pediatr Gastroenterol Nutr. 1992;15:289–296. doi: 10.1097/00005176-199210000-00010. [DOI] [PubMed] [Google Scholar]
- 20.Alam AN, Sarker SA, Wahed MA, et al. Enteric protein loss and intestinal permeability changes in children during acute shigellosis and after recovery: effect of zinc supplementation. Gut. 1994;35:1707–1711. doi: 10.1136/gut.35.12.1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahmood A, FitzGerald AJ, Marchbank T, et al. Zinc carnosine, a health food supplement that stabilises small bowel integrity and stimulates gut repair processes. Gut. 2007;56:168–175. doi: 10.1136/gut.2006.099929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sturniolo GC, Di Leo V, Ferronato A, et al. Zinc supplementation tightens “leaky gut” in Crohn’s disease. Inflamm Bowel Dis. 2001;7:94–98. doi: 10.1097/00054725-200105000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Tran CD, Howarth GS, Coyle P, et al. Dietary supplementation with zinc and a growth factor extract derived from bovine cheese whey improves methotrexate-damaged rat intestine. Am J Clin Nutr. 2003;77:1296–1303. doi: 10.1093/ajcn/77.5.1296. [DOI] [PubMed] [Google Scholar]
- 24.Berant M, Khourie M, Menzies IS. Effect of iron deficiency on small intestinal permeability in infants and young children. J Pediatr Gastroenterol Nutr. 1992;14:17–20. doi: 10.1097/00005176-199201000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Chilenje Infant Growth, Nutrition and Infection (CIGNIS) Study Team Micronutrient fortification to improve growth and health of maternally HIV-unexposed and exposed Zambian infants: a randomised controlled trial. PLoS One. 2010;5:e11165. doi: 10.1371/journal.pone.0011165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dewey KG, Brown KH. Update on technical issues concerning complementary feeding of young children in developing countries and implications for intervention programs. Food Nutr Bull. 2003;24:5–28. doi: 10.1177/156482650302400102. [DOI] [PubMed] [Google Scholar]
- 27.Famine Early Warning Systems . Zambia Food Security Update. FEWS NET Zambia; Lusaka: 2006. [Google Scholar]
- 28.Willumsen JF, Simmank K, Filteau SM, et al. Toxic damage to the respiratory epithelium induces acute phase changes in vitamin A metabolism without depleting retinol stores of South African children. J Nutr. 1997;127:1339–1343. doi: 10.1093/jn/127.7.1339. [DOI] [PubMed] [Google Scholar]
- 29.Rollins NC, Filteau SM, Elson I, et al. Vitamin A supplementation of South African children with severe diarrhoea: optimum timing for improving biochemical and clinical recovery and subsequent vitamin A status. Pediatr Infect Dis J. 2000;19:284–289. doi: 10.1097/00006454-200004000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Lunn PG, Northrop CA, Northrop AJ. Automated enzymatic assays for the determination of intestinal permeability probes in urine. 2. Mannitol. Clin Chim Acta. 1989;183:163–170. doi: 10.1016/0009-8981(89)90332-x. [DOI] [PubMed] [Google Scholar]
- 31.Northrop CA, Lunn PG, Behrens RH. Automated enzymatic assays for the determination of intestinal permeability probes in urine. 1. Lactulose and lactose. Clin Chim Acta. 1990;187:79–87. doi: 10.1016/0009-8981(90)90333-n. [DOI] [PubMed] [Google Scholar]
- 32.Beesley R, Filteau S, Tomkins A, et al. Impact of acute malaria on plasma concentrations of transferrin receptors. Trans R Soc Trop Med Hyg. 2000;94:295–298. doi: 10.1016/s0035-9203(00)90329-8. [DOI] [PubMed] [Google Scholar]
- 33.Filmer D, Pritchett L. Estimating wealth effects without expenditure data – or tears: an application to educational enrolments in states of India. Demography. 2001;38:115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization . WHO Child Growth Standards. WHO; Geneva: 2006. [Google Scholar]
- 35.Carpenter JR, Kenward MG. Missing Data in Randomized Controlled Trials – A Practical Guide. Medical Statistics Unit, London School of Hygiene and Tropical Medicine; London: 2007. [Google Scholar]
- 36.Chisenga M, Siame J, Baisley K, et al. Determinants of infant feeding choices by Zambian mothers: a mixed quantitative and qualitative study. Matern Child Nutr. 2011;7:148–159. doi: 10.1111/j.1740-8709.2010.00264.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goto R, Panter-Brick C, Northrop-Clewes CA, et al. Poor intestinal permeability in mildly stunted Nepali children: associations with weaning practices and Giardia lamblia infection. Br J Nutr. 2002;88:141–149. doi: 10.1079/bjnbjn2002599. [DOI] [PubMed] [Google Scholar]
- 38.Campbell DI, McPhail G, Lunn PG, et al. Intestinal inflammation measured by fecal neopterin in Gambian children with enteropathy: association with growth failure, Giardia lamblia and intestinal permability. J Pediatr Gastroenterol Nutr. 2004;39:153–157. doi: 10.1097/00005176-200408000-00005. [DOI] [PubMed] [Google Scholar]
- 39.Campbell DI, Elia M, Lunn PG. Growth faltering in rural Gambian infants is associated with impaired small intestinal barrier function, leading to endotoxemia and systemic inflammation. J Nutr. 2003;133:1332–1338. doi: 10.1093/jn/133.5.1332. [DOI] [PubMed] [Google Scholar]
- 40.Nchito M, Friis H, Michaelsen KF, et al. Iron supplementation increases small intestine permeability in primary schoolchildren in Lusaka, Zambia. Trans R Soc Trop Med Hyg. 2006;100:791–794. doi: 10.1016/j.trstmh.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 41.Gera T, Sachdev HP. Effect of iron supplementation on incidence of infectious illness in children: systematic review. BMJ. 2002;325:1142. doi: 10.1136/bmj.325.7373.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dewey KG, Domellöf M, Cohen RJ, et al. Iron supplementation affects growth and morbidity of breast-fed infants: results of a randomized trial in Sweden and Honduras. J Nutr. 2002;132:3249–3255. doi: 10.1093/jn/132.11.3249. [DOI] [PubMed] [Google Scholar]
- 43.de Morais MB, Lifschitz CH. Intestinal permeability to lactulose and mannitol in growing rats with iron-deficiency anemia. Biol Trace Elem Res. 2004;99:233–240. doi: 10.1385/BTER:99:1-3:233. [DOI] [PubMed] [Google Scholar]
- 44.Meshkinpour H, Vaziri ND, Zhou XJ, et al. Effects of experimental hemosiderosis on intestinal morphology, permeability, and tissue iron content. Dig Dis Sci. 1996;41:984–988. doi: 10.1007/BF02091541. [DOI] [PubMed] [Google Scholar]
- 45.Ferruzza S, Scarino ML, Gambling L, et al. Biphasic effect of iron on human intestinal Caco-2 cells: early effect on tight junction permeability with delayed onset of oxidative cytotoxic damage. Cell Mol Biol. 2003;49:89–99. [PubMed] [Google Scholar]
- 46.Glei M, Latunde-Dada GO, Klinder A, et al. Iron-overload induces oxidative DNA damage in the human colon carcinoma cell line HT29 clone 19A. Mutat Res. 2002;519:151–161. doi: 10.1016/s1383-5718(02)00135-3. [DOI] [PubMed] [Google Scholar]
- 47.LatundeDada GO. Iron metabolism: microbes, mouse, and man. Bioessays. 2009;31:1309–1317. doi: 10.1002/bies.200900101. [DOI] [PubMed] [Google Scholar]
- 48.Zimmermann MB, Chassard C, Rohner F, et al. The effects of iron fortification on the gut microbiota in African children: a randomized controlled trial in Côte d’Ivoire. Am J Clin Nutr. 2010;92:1406–1415. doi: 10.3945/ajcn.110.004564. [DOI] [PubMed] [Google Scholar]