Abstract
Background
The white coat's place in the medical profession is a heavily debated topic. Five years after the bare-below-the-elbow policy took effect in England, we reexamined the evidence about coats' potential to transmit infection, reviewed previous studies, and explored our patients' opinions on doctor attire.
Methods
We administered a survey at 3 locations in the Ochsner Health System (hospital clinic, satellite clinic, and inpatient ward) in 2013. The survey assessed patient preference for doctors to wear white coats and included 4 images of the same doctor in different attire: traditional white coat, bare-below-the-elbow attire, a white coat with scrubs, and scrubs alone. Respondents rated images head-to-head for their preferences and individually for their confidence in the physician's skills and for their comfort level with the physician based upon the displayed attire. Participants' attitudes were then reassessed after they were given information about potential disease transmission.
Results
Overall, 69.9% of the 153 patients surveyed preferred doctors to wear white coats. When locations were compared, a statistically higher proportion of outpatients preferred coats (P=0.001), a trend most pronounced between hospital clinic (84%) and ward inpatients (51.9%). Patients disliked bare-below-the-elbow attire, scoring it lowest on the comfort and confidence scales (0.05 and 0.09, respectively). Information regarding risks of coat-carried infections did not influence respondents' opinions; 86.9% would still feel comfortable with a doctor who wore one.
Conclusions
These findings suggest patients prefer white coats, and they contribute to greater comfort and confidence in their physicians, despite knowledge of theoretic concerns of disease transmission.
Keywords: Clothing, infection control–methods, patient preference–psychology, patient preference–statistics & numerical data, physician-patient relations, physicians–standards
INTRODUCTION
The white coat has been a symbol of the medical profession since it was borrowed from laboratory workers in the mid-19th century to lend credibility to the doctors who wore them. The white color was specifically chosen to associate physicians with purity and cleanliness.
Over the past 2 decades, however, the white coat has become a hotly debated topic with regard to its capacity to harbor and spread infectious agents. Evidence shows that coat sleeves and pockets can act as a reservoir for bacteria.1,2 Further evidence shows that pathologic microbes, particularly resistant strains, can be isolated from these locations and suggests that coats might act as a vector for patient-to-patient transmission.3 However, many physicians have pointed out that no study has conclusively linked white coats with the spread of infection to patients, including the comprehensive policy review paper prepared at the request of the United Kingdom's Department of Health to identify the sources of and decrease the rate of healthcare-associated infections in English hospitals.4,5 In fact, recent evidence has shown that the bacterial load on coat sleeves is equivalent to that found on surgical scrub sleeves after 8 hours of hospital duties.6 Despite objections and conflicting evidence,7 on September 17, 2007, the National Health Service (NHS) in England implemented the bare-below-the-elbow policy for all workers in NHS medical facilities.8
Complicating this issue are the functionality of white coats and their role in the doctor-patient relationship. Many doctors appreciate the utility of coats for keeping their clothes clean and for carrying innumerable items; additionally, both doctors and patients say the most important role of white coats is to identify physicians in the busy clinical environment.9,10
While studies have reported contradictory support from patients for and against the wearing of white coats by their doctors, results tend to be dictated by the study location and to be specific to individual specialties within medical practice. In studies reporting patient preference for white coats, patients have cited this choice of attire as conferring greater confidence and belief in a doctor's abilities, improving communication, and fostering the doctor-patient relationship.10-13
We conducted an observational study to assess our patient population's preferences for physician attire in different clinical settings by using an image comparison questionnaire. We designed our project to further define the contribution and benefits of different attire choices in medical practice and to explore the extent to which theoretical concerns regarding coat-carried infections influence patient opinion.
METHODS
After obtaining institutional review board approval, we administered an anonymous survey at 3 locations within the Ochsner Health System during a 2-week period in January 2013: a hospital-based internal medicine clinic, a community-based outpatient family practice clinic, and an inpatient hospital ward. The hospital-based locations were at Ochsner Medical Center in Jefferson, Louisiana, which supports the greater New Orleans area, and the community-based clinic was in the nearby suburb of Metairie, Louisiana.
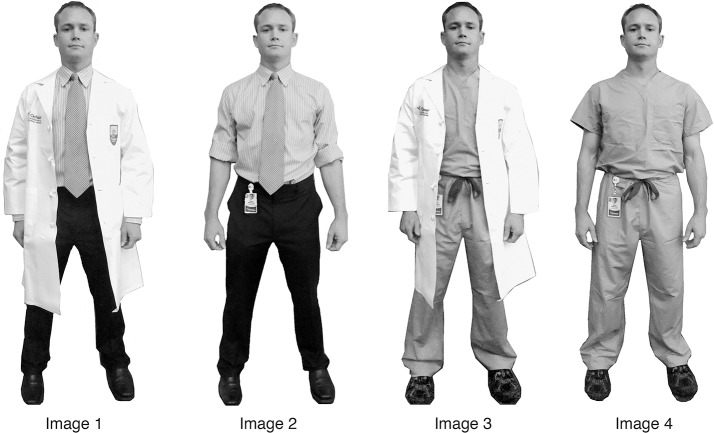
The cross-sectional, observational study used the survey to ascertain if patients preferred doctors who wore white coats and then to evaluate their initial answer with side-by-side comparisons of 4 different attire choices (Figure 1). Additionally, the study explored how this opinion varied across clinical location and quantified the confidence and comfort such attire choices provoked. The study also investigated the extent to which the surveyed patients had knowledge of the debate surrounding white coats and whether such information impacted their opinions.
Figure 1.
Attire choices used for head-to-head comparisons for the Patient Preference on Doctor Attire Survey.
Volunteers pretested the survey to estimate timing and to correct any ambiguity. In an attempt to reduce bias, the primary research question—Do you prefer doctors to wear a white coat?—was asked at the start of the survey before respondents viewed any images. The images used for comparison of attire choices showed the same doctor in the same pose in all 4 images. Comparison questions asked for direct patient preference of 2 images shown side by side (with an indifferent option). Questions to assess confidence and comfort with attire choices followed the comparison questions.
After the patient evaluated all permutations of direct comparison, the last section of the survey presented a summation of the debate surrounding white coats and the potential they pose for disease transmission. This information included the disclaimer that no study to date has shown that wearing a white coat contributes to patient infections. Three yes or no questions followed the summation, asking if patients had previous knowledge of these issues, if this information made them rethink their opinion on doctor attire, and if they would now be less comfortable with a doctor who chooses to wear a white coat.
We recruited participants on a convenience basis in the clinic waiting rooms after they checked in for their appointments. A researcher in plain scrubs approached patients and followed a standardized script to assess their willingness to participate. The lead investigator instructed and trained researchers to ensure internal validity was maintained in survey administration. To recruit ward inpatients, a researcher dressed in scrubs went to consecutive patient rooms on a medical ward and asked patients if they were willing to participate.
Once participants completed the survey, the researchers thanked them and provided a brief summation of the debate surrounding sleeves and infection control as well as the scope and aims of our research project if the participants requested additional information.
The lead investigator entered survey responses to the primary research questions and all head-to-head comparisons into a database. If patients failed to complete these minimum components, the survey was discarded. The most common reason for an incomplete survey was patients being called for their appointments. Any missing information on completed surveys was left blank.
Statistical Analysis
Comparisons among different locations and preferences and demographic characteristics were analyzed using chi-square tests and Student t test performed by STATA v.11 (College Station, TX). P values <0.05 were considered statistically significant.
To quantify preference, we aggregated the results from a series of pairwise comparisons evaluating all iterations. While this method was less definitive than a 4-at-once direct comparison, it allowed us to garner additional information about individual comparisons in a manner that was user friendly enough for a convenience survey. From this series of direct comparisons, we were able to draw inferences about overall preference and rank order for comment.
RESULTS
A total of 153 surveys were completed at the 3 sites. The overall characteristics of the participants are shown in Table 1. The majority of the respondents were female (67.6%) and white (66.7 %). The mean age of patients was 55.5 years (range 19-90). Participants were evenly distributed across the 3 locations.
Table 1.
Demographic Characteristics of the Study Population (n=153)
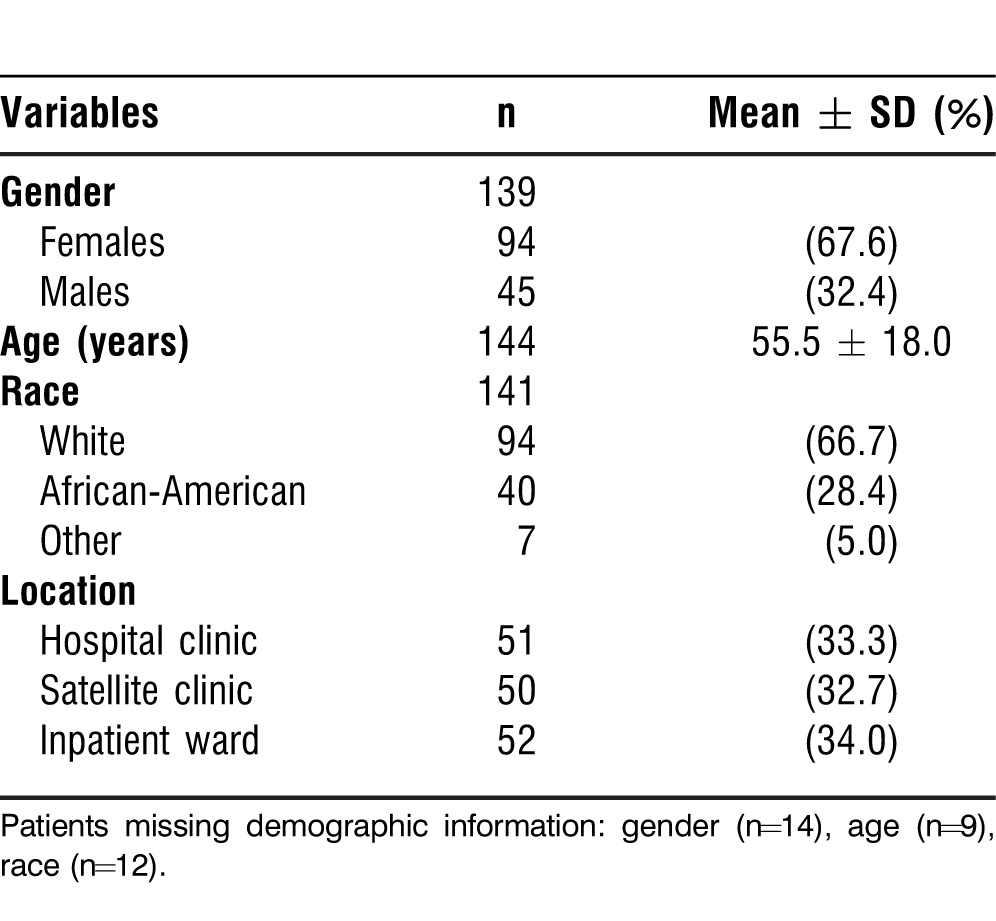
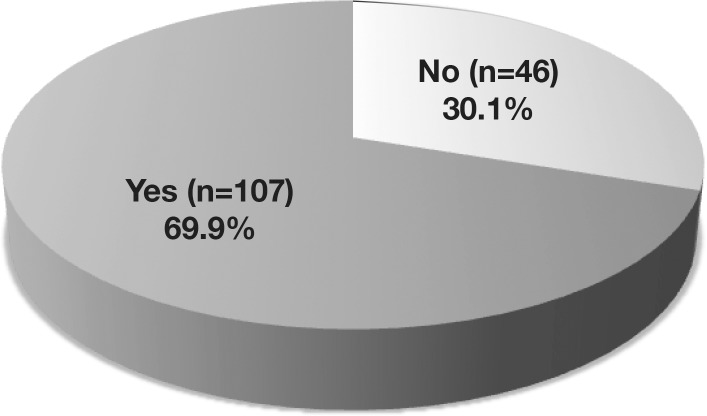
Table 2 shows participants' preferences for physician attire and how confident and comfortable they are in the abilities of the doctor to perform his medical duties according to choice of attire. Overall, 69.9% of 153 patients surveyed preferred doctors to wear white coats (Figure 2).
Table 2.
Patients' Preferences for Doctor Attire and Percentage Results for Confidence and Comfort by Image
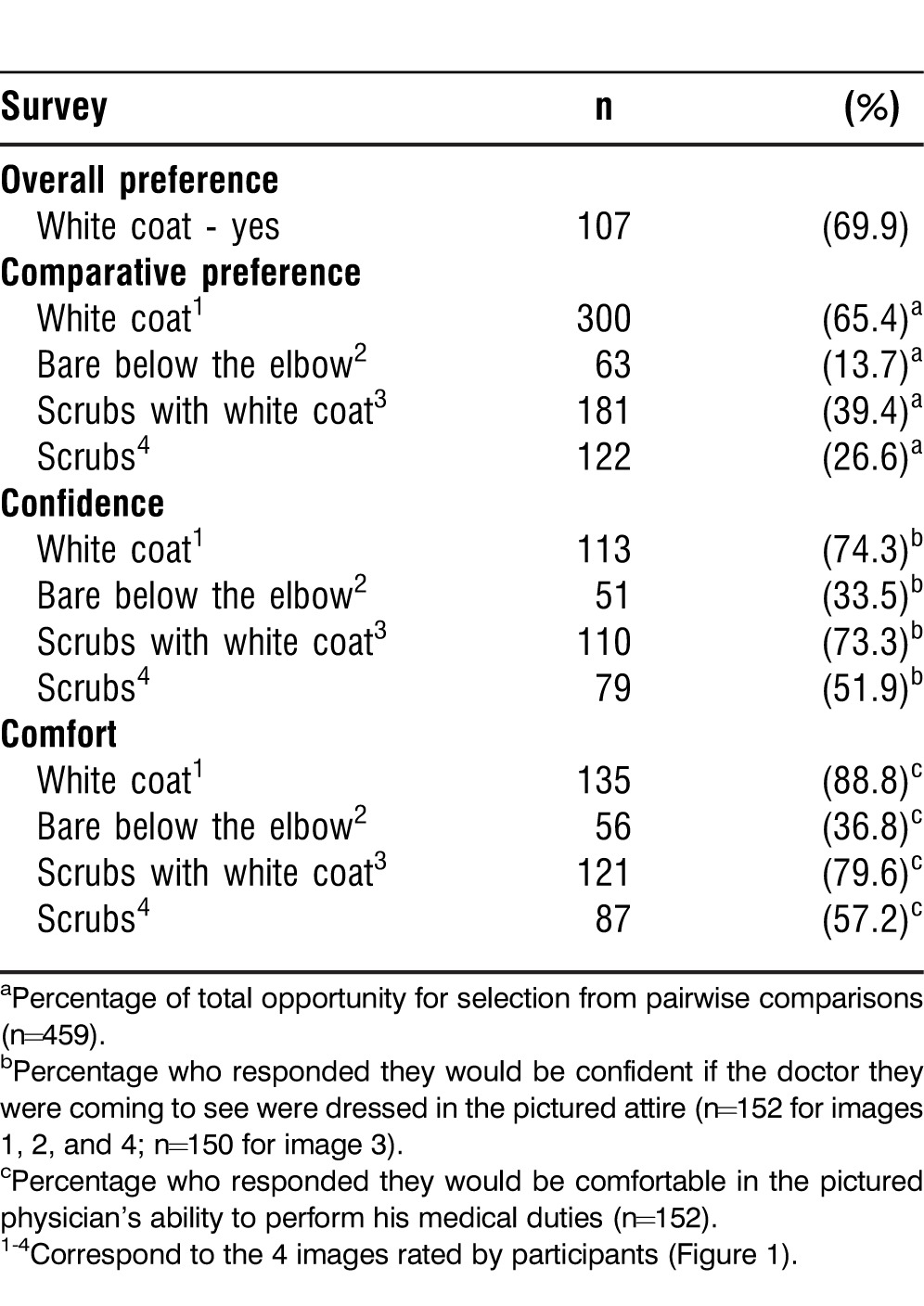
Figure 2.
Participant responses to the survey question “Do you prefer doctors to wear a white coat?”
For image ranking, we tallied the number of times an image was selected in a pairwise comparison against the percentage of total opportunity for selection (pTOS). This variable allowed us to quantify the overall trend of image preferences while still taking into account the indifferent responses. Using this approach, we inferred that coated attire choices were the most preferred in head-to-head comparisons, with Image 1 in Figure 1 garnering the highest preference (65.4%), followed by Image 3 (39.4%) and Image 4 (26.6%). Image 2 (13.7%) was the least preferred attire choice (Table 2). Additionally, we found that indifferent was selected in approximately 30% of all comparisons and in 30% of the individual comparisons. The lone exception to this trend was the Image 1 vs Image 2 comparison: 82% preferred Image 1, 5% preferred Image 2, and 13% were indifferent.
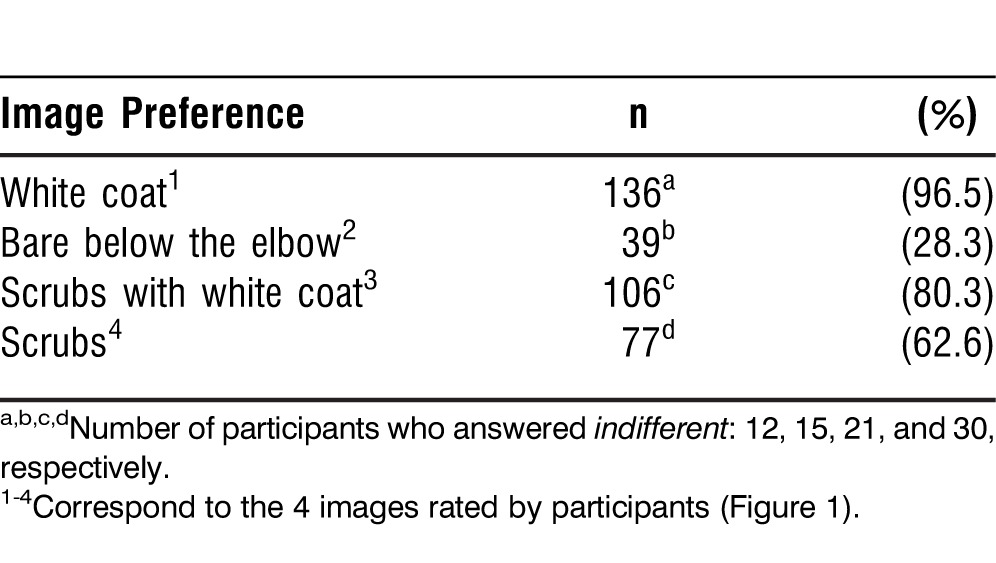
A sensitivity analysis was also performed in which we isolated each participant's response. We created an algorithm that separated each response and generated new variables for each image. For example, when comparing Image 1 to Image 2, Image 1 to Image 3, or Image 1 to Image 4, a new variable called Image 1 was set and binary codes were assigned if a respondent chose Image 1 over Image 2, Image 1 over Image 3, or Image 1 over Image 4. The same rationale was applied to all comparisons. The results of the sensitivity analysis were comparable to the results from pairwise comparison and pTOS but revealed more robust results. Image 1 was preferred by 96.5% followed by Image 3 at 80.3%, Image 4 at 62.6%, and Image 2 at 28.3%, as shown in Table 3 (indifferent responses were dropped from this method of analysis).
Table 3.
Patient Preference Analysis Using Sensitivity Analysis
Regardless of the analysis used, the results produced the same rank order (Image 1 > Image 3 > Image 4 > Image 2) for image preference. This order was consistent across all locations and maintained for all head-to-head comparisons. For example, an examination of the pairwise comparisons for Image 4 shows that Image 4 was preferred head to head only against Image 2 and was less preferred in direct comparisons with Image 1 and Image 3; these results were consistent for each location.
With both methods conferring similar results, we decided to use the pTOS for our analysis because it gave more conservative estimates of preference by taking into account indifferent responses. For the comfort and confidence questions, we converted responses into a scaled score to provide a more accurate value for comparison with separate consideration of indifferent and negative responses. Patients expressed equal confidence in doctors' abilities when they wore either a white coat (0.71) or scrubs with a white coat (0.72) Patients disliked the bare-below-the-elbow–compliant attire portrayed in Image 2, scoring it lowest on the comfort and confidence scales (0.05 and 0.09, respectively), as shown in Figure 3.
Figure 3.
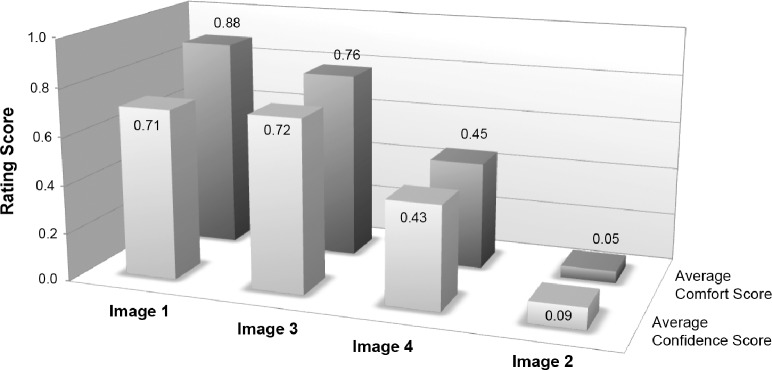
Average scale scores derived from ranking of individual images: 1 = comfortable/confident, 0 = indifferent, and −1 = not comfortable/confident.
To explore attire preferences further, we looked at whether patient demographics and survey locations were associated with respondents' stated preferences. Results are presented in Table 4. Examination of age and ethnicity showed no significant differences in white coat preference. Gender, however, was significantly associated with white coat preference. A significantly higher proportion of females preferred white coat attire than males (72.9% versus 27.1%, P=0.046). Location within the Ochsner Health System was also related to white coat preferences. Patients in the hospital clinic (84%) were more likely to prefer white coat attire than those in the satellite clinics (74.5%) and the inpatient ward (51.9%), P=0.001 (Figure 4). This instance was the only one in which location had a significant effect. For example, despite equivocal ratings on the comfort and confidence scales, Image 1 was consistently preferred in pairwise comparisons of the 2 coated attire choices.
Table 4.
Associations Between White Coat Preference, Demographic Characteristics, and Survey Locations
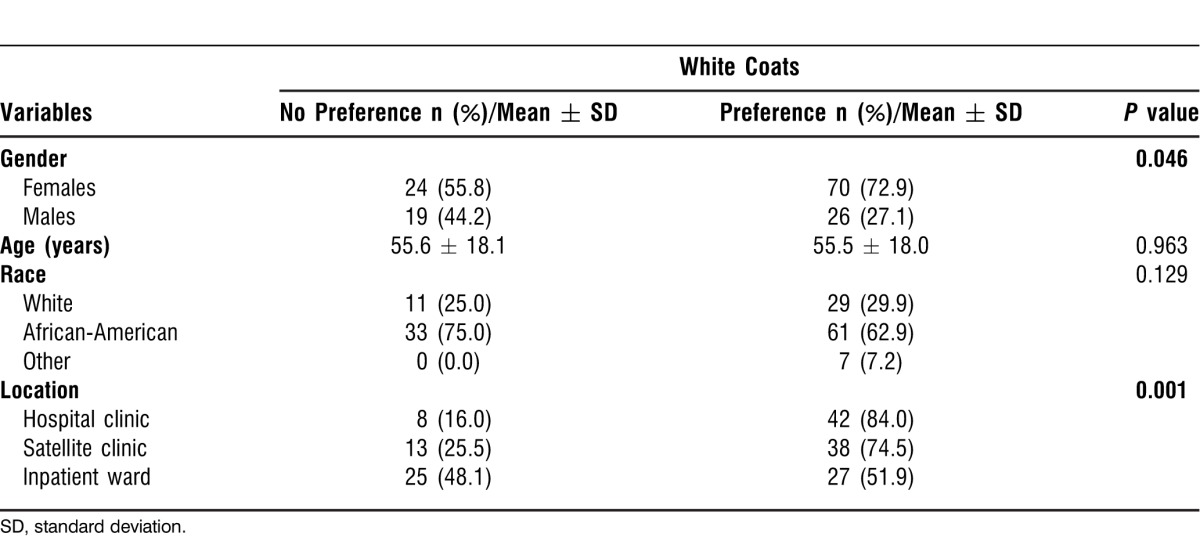
Figure 4.
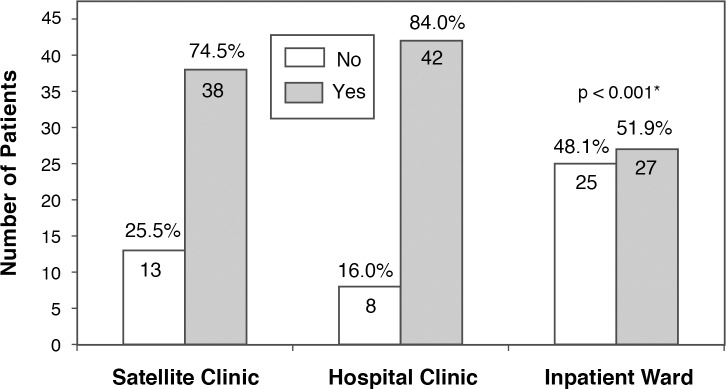
Patient preferences for white coats by location.
*P value corresponds to the comparison of white coat preferences across different locations.
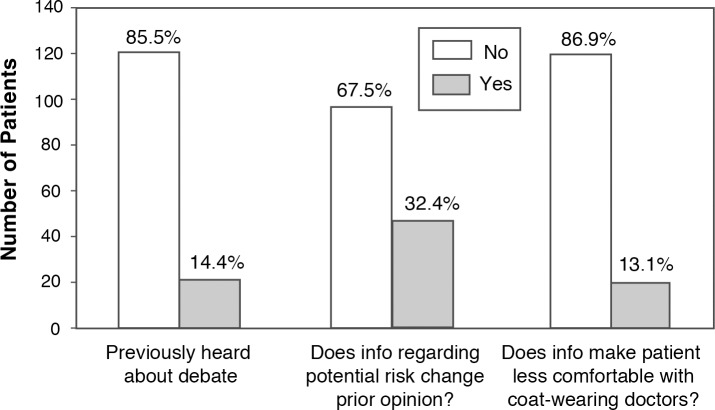
Finally, we investigated if the information about potential disease transmission by white coats would change patients' opinions about doctor attire (Figure 5). Of the patients surveyed, 85.5% were unaware of the debate surrounding white coats. Importantly, 67.5% of patients did not change their opinion about white coat attire after reading the segment and 86.9% reported still feeling comfortable with doctors who wear them.
Figure 5.
Impact on patient opinion of information about the risks of coat-carried infections.
DISCUSSION
The 2007 dress code guidelines banning white coats from hospitals in England were based on the recommendations of 2 literature reviews undertaken by researchers at Thames Valley University (referred to as TVU1 and TVU2).14 TVU1 investigated the existing evidence about the role of uniforms in the transmission of infection and the merit of laundering to remove bacterial contamination.15 TVU2 focused on the public perception of uniforms in healthcare.16 The dress code guidelines came under immediate scrutiny; critics pointed out that both reviews concluded that insufficient evidence was available at the time to support the notion that coats pose a significant risk. Objections eventually led to revision of the guidelines in 2010; the softened language removed the imposition of a standardized uniform for physicians.7
We found that patients overall prefer doctors to wear white coats. This preference was confirmed by the image comparison questions for which both coated attire choices were preferred to noncoat and bare-below-the-elbow–compliant choices in every pairwise comparison—Image 1 (65.4%) > Image 3 (39.4%) > Image 4 (26.6%) > Image 2 (13.7%). These findings are in accordance with previous findings by Rehman et al13 who found that 76% of the patients in their study preferred white coats and join the conclusions of studies from Douse et al9 and Gherardi et al17 whose patients also preferred doctors who wear white coats.
However, other studies have reported contradictory conclusions about patient preference. Gooden et al10 found that 45% of the Australian family practice patients they surveyed were indifferent to coats, Cha et al18 reported that 60% of the obstetrics and gynecology clinic patients surveyed had no preference about coats, and Hueston and Carek19 concluded that patients had no clear preference about physician attire.
Specific to the relationship between patient confidence and coated attire, Toquero et al20 concluded that patients trust health professionals regardless of attire choices, even if they dislike that attire. These findings concur with those of Edwards et al21 and Cha et al18 but are opposed to those of Rehman et al13 who found coats favorably influenced patient trust and confidence-building and facilitated communication of more personal topics. This result is consistent with Gherardi et al's finding17 showing that patients had the most confidence in doctors wearing white coats.
While the majority of investigations into this issue have taken place in the United Kingdom and abroad, multiple US-based studies have demonstrated inconsistent findings. Studies in obstetrics and gynecology and family practice settings based in Ohio and South Carolina, respectively, found no clear preference,18,19 whereas investigations specific to internal medicine and surgical patients based in South Carolina and Texas, respectively, were supportive of coat-wearing practices.13,21
These findings illustrate the complexity of investigating this issue and suggest that patients represent a heterogeneous group of evolving preferences that may be related to the type of physician they are coming to see, as well as the geographic location and manner of attire they are accustomed to associating with physicians. Our study was designed to answer questions about the specific preferences of our patient population rather than to characterize the views of a generic patient devoid of the subjective context that studies of this nature are piecing together.
Our results suggest that coats make a tangible contribution to a patient's sense of confidence and comfort with a physician. Our patients rated both choices of coated attire highly on the comfort and confidence scales. These findings concurred with some of the findings from previous studies.10,18 While these studies found that the majority of patients were indifferent to white coats, they both concluded that coats had a positive impact contrary to this stated indifference (mirroring our results in the wards). In an inpatient population, Gooden et al10 reported that patients felt more confident and communicated better with doctors who wore white coats. Likwewise, Cha et al18 reported that patients rated coated images of resident physicians higher than those of casual attire in measures for comfort and perception of competence. Given our hypothesis that wearing a white coat with professional attire would score highly on these measures of patient perception, we noted with interest that wearing a coat with scrubs had an equally strong ability to invoke confidence.
This trend was magnified by the patient scoring of bare-below-the-elbow–compliant clinic attire. While plain-scrubs attire received the second lowest ranking on comfort, confidence, and overall preference, the bare-below-the-elbow–compliant clinic attire with no coat and sleeves rolled up was rarely favored in head-to-head comparisons. Image 2 was preferred in only 63 of its 459 comparisons (13.7%). This attire choice ranked last in patient comfort and ability to inspire confidence. Only 33.5% of respondents said they would be confident in the pictured doctor's abilities, and just slightly more (36.8%) said they would feel comfortable if their doctor were dressed in a like fashion.
Only about one-third of patients reported that they would be comfortable or confident in a physician who wore the professional attire with the sleeves rolled up and no white coat. According to Ridd et al,22 the consultation experience is one of the pillars of the doctor-patient relationship. The success of this experience depends on knowledge, loyalty, trust, and regard. A patient's first impression of a physician can instill trust by inspiring confidence and can build regard by engendering comfort. According to our study findings, both of these traits seem to be already linked in patients' minds with physicians who wear white coats.
While we did not assess the precise reasons for such strong dislike of the bare-below-the-elbow–compliant attire option, some patients made similar remarks to the surveyors during debriefing. A common observation was that patients would not be able to tell if the individual were a doctor and that he looked more like a salesman. Respondents also noted that the individual appeared “unclean,” “sloppy,” and “unprofessional” without the white coat attire. While the modeled attire was compliant with bare-below-the-elbow policy and consistent with actual physician dress practices, future investigations should be cautious of this potential source of bias. We recommend prescreening all image choices prior to future study to rule out poorly perceived images ahead of selection for study inclusion as a comparator.
Previous studies indicate several possible explanations for the preference for white coats. Coats are perceived as clean and professional, help identify doctors in a busy clinical environment, and contribute to patient care by improving the doctor-patient relationship and aiding communication.10,23
Although most patients were unaware of the debate surrounding dress code policy, when given information about the theoretical risks of infection, the majority reported that this information did not change their opinion. Furthermore, most patients reported that this information did not make them less comfortable with doctors who wear a white coat. These responses support previous findings9,24 and suggest the majority of patients would not support a bare-below-the-elbow policy change based on existing evidence.
Our study unveiled an interesting nuance regarding hospitalized patient preferences. Inpatients were evenly divided on preference, with 51.9% of respondents reporting they preferred doctors to wear a white coat and 48.1% reporting no preference. This finding seems logical given that sicker patients may be more concerned with feeling better than with physician attire in general.
To evaluate this discrepancy more fully, we looked deeper into our patients' opinions. Overall, patients rated coated attire significantly higher for confidence and comfort, regardless if the coats were worn over shirt and tie or scrubs. Furthermore, patients on the wards rated the influence of coats on comfort and confidence greater than the respondents in the 2 clinical locations. These results suggest that inpatients attach significance to the white coat and desire physicians to wear them, contrary to their stated preferences and regardless of what doctors wear beneath.
A limitation of this project is potential self-selection bias. Because these patients were accustomed to seeing doctors wearing white coats at our institution, that familiarity may have influenced their opinion of what a doctor should look like. Study participants were all patients of a large private facility in a mid-size American city, which may affect generalizability of the results. Additionally, the survey was created for this project and was not externally validated although it incorporated elements utilized by similar studies.
Future studies might focus on other clinical locations, such as the perioperative setting or the emergency department where scrubs are the expected attire. This different context would allow researchers to delineate the role of white coats throughout the hospital and answer questions regarding how much significance, either consciously or inferred from responses contrary to initially stated opinion, patients assign to white coats once they are removed from settings with connotations of what a doctor should look like. According to a large study administered in the surgery department at William Beaumont Army Medical Center in Texas, the majority of patients responded that scrubs were appropriate attire for physicians and said attire choice would not affect their opinion of the care they received.21 However, half of the patients in the study also reported that doctors wearing white coats is a necessary practice, and that finding supports our data showing that wearing a coat appears to be more important to patients than what one wears underneath. Further investigation might be able to provide guidance within specific hospital settings.
Further investigation is warranted into alternative attire options—such as sleeveless coats or the traditional doctor bag—on the same survey to see how readily patients would accept changes that can provide similar function (utility and identification) while removing the potential risks of coat-carried infections. Studies could also investigate the perception of novel solutions such as messenger-style shoulder bags and vests made of advanced antimicrobial fabrics.
CONCLUSIONS
Our findings suggest patients prefer white coats and they contribute to greater comfort and confidence in their physicians. While our participants' knowledge about coat-carried infection risk was low, information about this theoretic risk had only a minimal influence on their opinions. The current available evidence has not conclusively linked white coats with increased infection rates; consequently, the contribution white coats make to medical practice should be taken into consideration before making uniform policy recommendations. We hope that our results can help guide the direction for future uniform policies.
Footnotes
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Interpersonal and Communication Skills, and Professionalism.
REFERENCES
- 1.Wong D, Nye K, Hollis P. Microbial flora on doctors' white coats. BMJ. 1991 Dec 21-28;303(6817):1602–1604. doi: 10.1136/bmj.303.6817.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loh W, Ng VV, Holton J. Bacterial flora on the white coats of medical students. J Hosp Infect. 2000 May;45(1):65–68. doi: 10.1053/jhin.1999.0702. [DOI] [PubMed] [Google Scholar]
- 3.Treakle AM, Thom KA, Furuno JP, Strauss SM, Harris AD, Perencevich EN. Bacterial contamination of health care workers' white coats. Am J Infect Control. 2009 Mar;37(2):101–105. doi: 10.1016/j.ajic.2008.03.009. Epub 2008 Oct 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Henderson J. The endangered white coat. Clin Infect Dis. 2010 Apr 1;50(7):1073–1074. doi: 10.1086/651163. [DOI] [PubMed] [Google Scholar]
- 5.Pratt RJ, Pellowe CM, Wilson JA, et al. epic2: National evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect. 2007 Feb;65((Suppl 1)):S1–S64. doi: 10.1016/S0195-6701(07)60002-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burden M, Cervantes L, Weed D, Keniston A, Price CS, Albert RK. Newly cleaned physician uniforms and infrequently washed white coats have similar rates of bacterial contamination after an 8-hour workday: a randomized controlled trial. J Hosp Med. 2011 Apr;6(4):177–182. doi: 10.1002/jhm.864. Epub 2011 Feb 10. [DOI] [PubMed] [Google Scholar]
- 7.Clement R. Is it time for an evidence based uniform for doctors? BMJ. 2012 Dec 18;345:e8286. doi: 10.1136/bmj.e8286. [DOI] [PubMed] [Google Scholar]
- 8.Graham J. Department of Health; UK: 2007. Uniforms and workwear: an evidence base for developing local policy. 17 September. http://webarchive.nationalarchives.gov.uk/+/www. dh.gov.uk/en/publicationsandstatistics/publications/publicationspolicyandguidance/dh_078433. Accessed January 15, 2013. [Google Scholar]
- 9.Douse J, Derrett-Smith E, Dheda K, Dilworth JP. Should doctors wear white coats? Postgrad Med J. 2004 May;80(943):284–286. doi: 10.1136/pgmj.2003.017483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gooden BR, Smith MJ, Tattersall SJ, Stockler MR. Hospitalised patients' views on doctors and white coats. Med J Aust. 2001 Aug 20;175(4):219–222. doi: 10.5694/j.1326-5377.2001.tb143103.x. [DOI] [PubMed] [Google Scholar]
- 11.Aggarwal R. The withering shine of white coat. Ann Indian Acad Neurol. 2012 Jan;15(1):63. doi: 10.4103/0972-2327.93286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bond L, Clamp PJ, Gray K, Van Dam V. Patients' perceptions of doctors' clothing: should we really be 'bare below the elbow'? J Laryngol Otol. 2010 Sep;124(9):963–966. doi: 10.1017/S0022215110001167. Epub 2010 Jun 2. [DOI] [PubMed] [Google Scholar]
- 13.Rehman SU, Nietert PJ, Cope DW, Kilpatrick AO. What to wear today? Effect of doctor's attire on the trust and confidence of patients. Am J Med. 2005 Nov;118(11):1279–1286. doi: 10.1016/j.amjmed.2005.04.026. [DOI] [PubMed] [Google Scholar]
- 14.Baxter JA, Dale O, Morritt A, Pollock JC. Bare below the elbows: professionalism vs infection risk. Bull R Coll Surg Engl. 2010 Jul;92(7):248–251. [Google Scholar]
- 15.Wilson JA, Loveday HP, Hoffman PN, Pratt RJ. Uniform: an evidence review of the microbiological significance of uniforms and uniform policy in the prevention and control of healthcare-associated infections. Report to the Department of Health (England) J Hosp Infect. 2007 Aug;66(4):301–307. doi: 10.1016/j.jhin.2007.03.026. Epub 2007 Jun 28. [DOI] [PubMed] [Google Scholar]
- 16.Loveday HP, Wilson JA, Hoffman PN, Pratt RJ. Public perception and the social and microbiological significance of uniforms in the prevention and control of healthcare-associated infections: an evidence review. J Infect Prev. 2007 Sep;8(4):10–21. doi: 10.1016/j.jhin.2007.03.026. [DOI] [PubMed] [Google Scholar]
- 17.Gherardi G, Cameron J, West A, Crossley M. Are we dressed to impress? A descriptive survey assessing patients' preference of doctors' attire in the hospital setting. Clin Med. 2009 Dec;9(6):519–524. doi: 10.7861/clinmedicine.9-6-519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cha A, Hecht BR, Nelson K, Hopkins MP. Resident physician attire: does it make a difference to our patients? Am J Obstet Gynecol. 2004 May;190(5):1484–1488. doi: 10.1016/j.ajog.2004.02.022. [DOI] [PubMed] [Google Scholar]
- 19.Hueston WJ, Carek SM. Patients' preference for physician attire: a survey of patients in family medicine training practices. Fam Med. 2011 Oct;43(9):643–647. [PubMed] [Google Scholar]
- 20.Toquero L, Aboumarzouk O, Owers C, Chiang R, Thiagarajah S, Amin S. Bare Below The Elbows- The Patient's Perspective. WebmedCentral QUALITY AND PATIENT SAFETY. 2011;2(4) WMC001401. http://www.webmedcentral.com/article_view/1401. Accessed June 17, 2013. [Google Scholar]
- 21.Edwards RD, Saladyga AT, Schriver JP, Davis KG. Patient attitudes to surgeons' attire in an outpatient clinic setting: substance over style. Am J Surg. 2012;Nov(5):663–665. doi: 10.1016/j.amjsurg.2009.09.001. Epub 2010 Jun 29. [DOI] [PubMed] [Google Scholar]
- 22.Ridd M, Shaw A, Lewis G, Salisbury C. The patient-doctor relationship: a synthesis of the qualitative literature on patients' perspectives. Br J Gen Pract. 2009 Apr;59(561):e116–e133. doi: 10.3399/bjgp09X420248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Farraj R, Baron JH. Why do hospital doctors wear white coats? J R Soc Med. 1991 Jan;84(1):43. doi: 10.1177/014107689108400116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palazzo S, Hocken DB. Patients' perspectives on how doctors dress. J Hosp Infect. 2010 Jan;74(1):30–34. doi: 10.1016/j.jhin.2009.08.021. Epub 2009 Nov 14. [DOI] [PubMed] [Google Scholar]