Abstract
Background
Ochsner Health System agreed to participate in a nationwide collaboration to reduce central line infections in our intensive care units. Our outpatient peripherally inserted central catheter (PICC) infection rate was unacceptably high, so as an adjunct to the nationwide study we attempted to reduce PICC infections in the home care environment. Typically, home health nurses or outpatient infusion centers care for PICCs per protocol. However, no standardized protocol exists, and each facility may have a different way to care for PICCs, leading to varied and inconsistent maintenance.
Methods
Key members from our hospital, home health agencies, and an infusion company formulated a plan to reduce outpatient PICC infections. We hypothesized that the only way to reduce infections was to standardize line care and maintenance and to empower the patient to be an advocate for his or her care. The best avenue for achieving standardized care across multiple infusion companies and multiple home health agencies was to develop an order set for PICC care and dressing changes. We also developed a checklist for the nurse and the patient to complete together during dressing changes. The checklist and order set were linked to the hospital's home health discharge orders so that they would print automatically when the provider discharged the patient to home health care.
Results
Baseline data were collected from July 1, 2010, to June 30, 2011. During that time, the infusion company identified 20 PICC infections. In 20,773 line days, the infection rate was 0.963 per 1,000 line days. The new order sets and checklists were instituted on July 1, 2011. From July 1, 2011 through June 30, 2012, 11 PICC infections were identified with 21,021 line days. The calculated infection rate was 0.52 per 1,000 line days. PICC infections so far have been reduced by 46%.
Conclusion
By bridging the gap between inpatient and outpatient care, we reduced PICC infections by 46% in our home infusion patients. We accomplished this result through a collaborative partnership among hospital staff, an infusion company, and home health agencies and a standardized process for line care and maintenance using a PICC home care order set and a patient/nursing PICC care checklist.
Keywords: Home care services, infection control, PICC-peripherally inserted central catheter
INTRODUCTION
The Ochsner Health System (OHS) Jefferson Highway campus refers patients in the New Orleans metropolitan area and outlying regions to outpatient infusion services. Common reasons for outpatient infusion include antibiotic administration, total parenteral nutrition, and inotrope therapy. Physicians, nurses, and pharmacists for the facility found that the peripherally inserted central catheter (PICC) infection rates were unacceptably high. These infections led to the interruption of home therapy, readmission to the hospital, the use of additional antibiotics, and inconvenience for the patient.
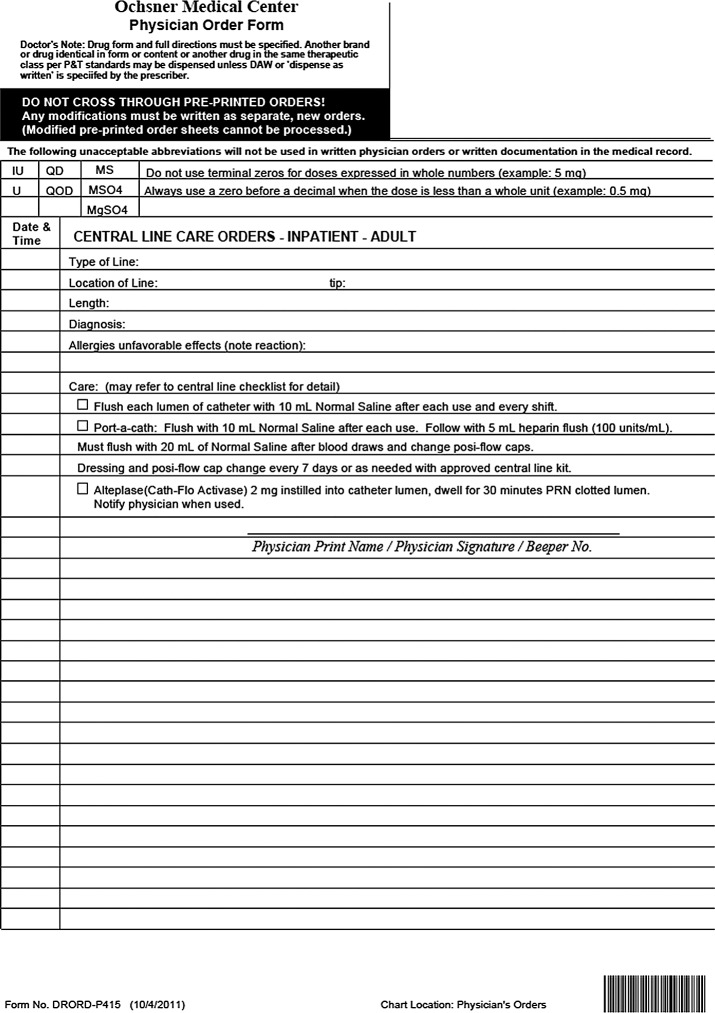
OHS agreed to participate in a nationwide initiative to reduce central line–associated bloodstream infections (CLABSIs) in intensive care units through use of the Comprehensive Unit-Based Safety Program (CUSP).1 As a result of OHS's involvement, practitioners implemented central line care strategies. Inpatient central line care was standardized using central line placement checklists, central line care order sets (Figure 1), bandage change order sets, nurse and patient central line care checklists, and a Scrub the Hub campaign.
Figure 1.
Physician order form for inpatient central line care.
Concurrently, our hospital, multiple home health agencies, and a local infusion company agreed to work together to bridge the gap between inpatient and outpatient line care to provide safer care for our patients and ultimately reduce PICC infection rates in the home.
METHODS
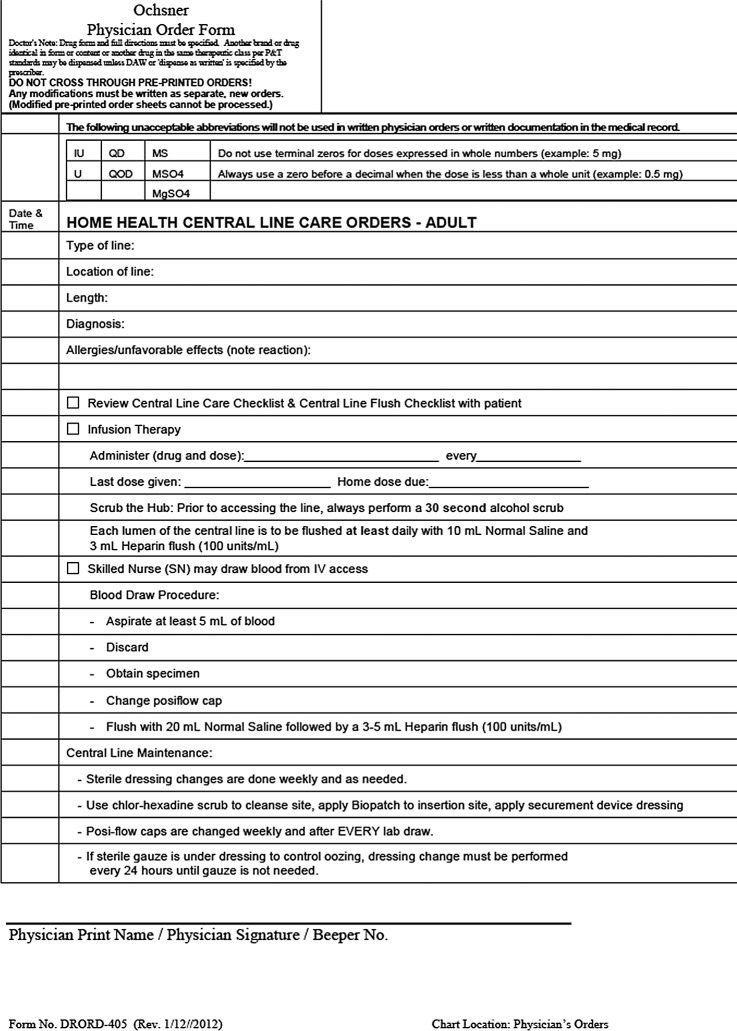
We invited nurses, physicians, pharmacists, and infection preventionists from the OHS Jefferson Highway campus, CarePoint Partners infusion company, and a few regional home health agencies to lead a task force to identify methods for eliminating PICC infections. One of the greatest challenges in the home care setting is that many infusion companies and home health agencies provide services but do not necessarily have common standards for central line care. After considering several options, we decided that the best approach was to standardize line care after patients were discharged from the hospital and back in their homes. To standardize maintenance of the central lines in a home care environment, the task force developed home health discharge order sets (Figure 2) that are linked to central line care order sets and patient/nurse checklists that the discharging provider can print. The hospital social workers and nurse navigators were encouraged to ask the discharging provider to use the central line care order sets upon discharge.
Figure 2.
Physician order form for home health central line care.
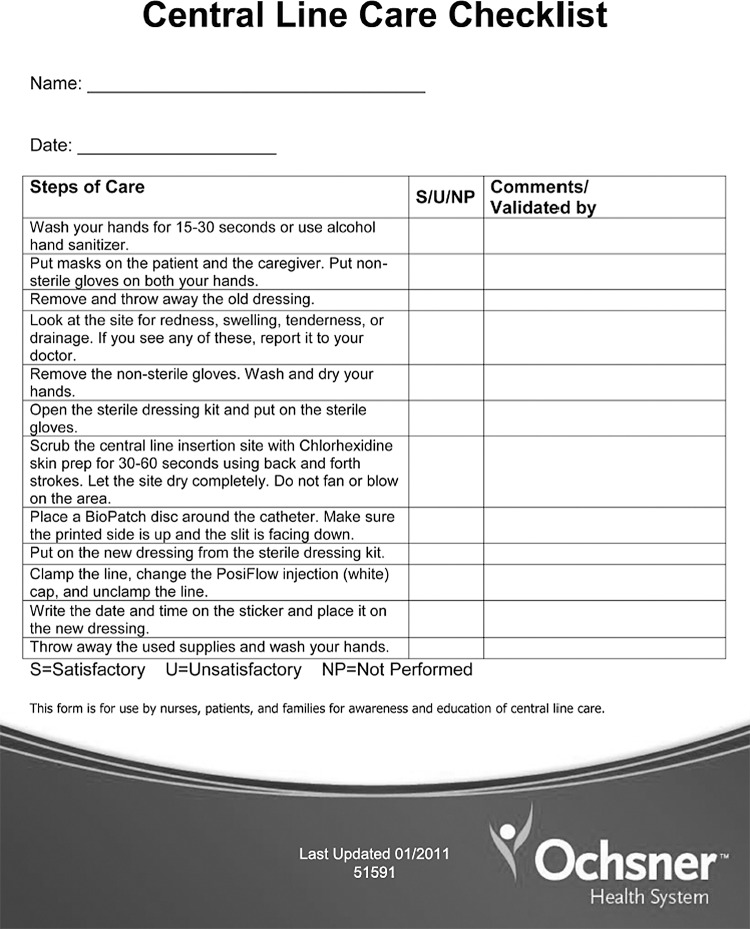
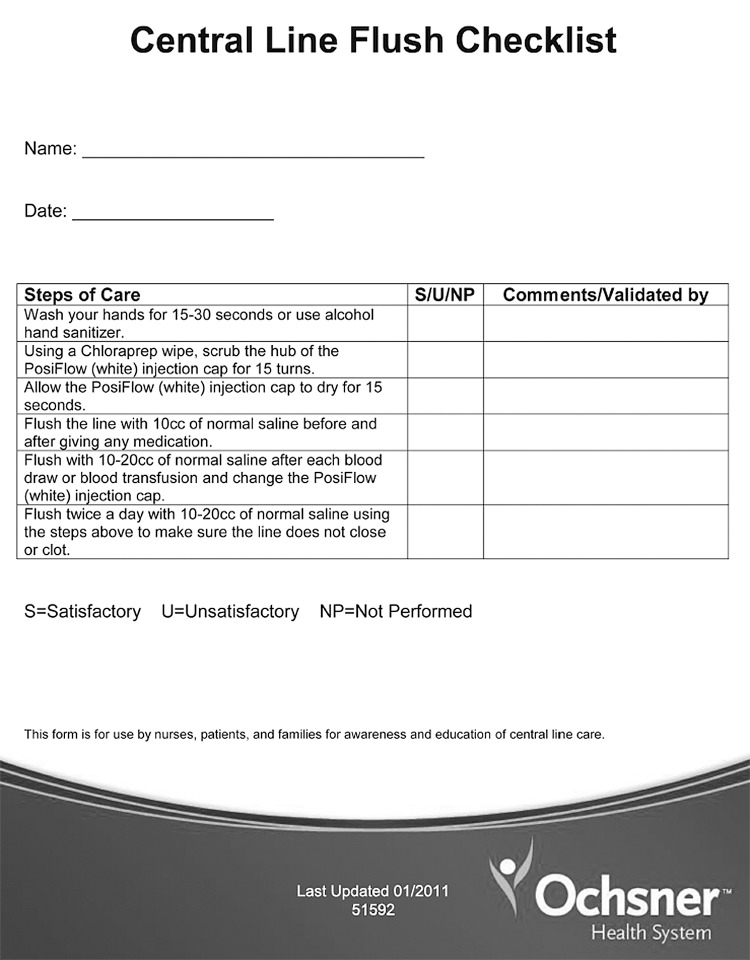
The order sets provided instructions for the care of the central line, the type of dressing, and the placement of a chlorhexidine-impregnated patch. Also included were 2 checklists for the patient and nurse to complete together to help empower the patient to be an advocate for his or her own line care (Figures 3 and 4).
Figure 3.
Central line care checklist for the nurse and the patient to complete during home care.
Figure 4.
Central line flush checklist for the nurse and the patient to complete during home care.
Prior to implementing the home care order sets, we sent letters to the directors of nursing at local home health agencies explaining the changes that would be expected. We stressed in the letter that if the companies wanted to continue to care for our patients, we expected their representatives to attend an education session. Representatives from the agencies were invited to meet at the OHS Jefferson Highway campus where we provided background about central line infections, discussed the reasons to eliminate infections, and educated the agency representatives about proper line care and dressing changes. CarePoint Partners offered an education session each week for the agencies' new nurses or nurses who wished to review the process.
Additionally, we discussed the plan with pharmacists from the 2 other major infusion companies in our area because our order sets specified particular supplies that would be more costly to the infusion companies.
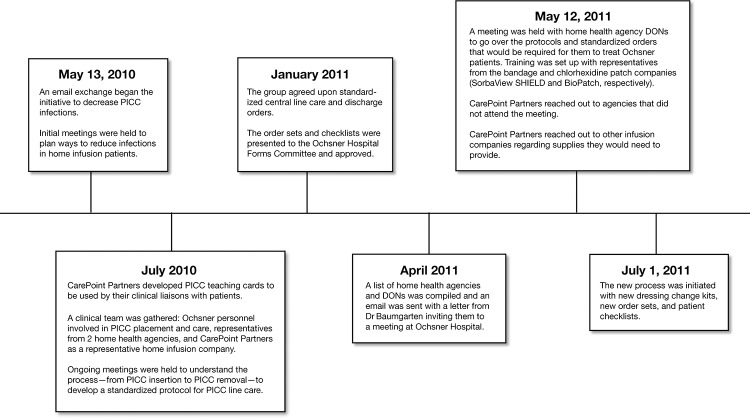
To compile baseline data, CarePoint Partners monitored outpatient PICC infection rates from July 1, 2010, to June 30, 2011. On July 1, 2011, we began using the new order sets, including the modified bandage change kit. CarePoint Partners then monitored outpatient line infection rates until June 30, 2012. Figure 5 shows the project timeline.
Figure 5.
Timeline of the central line care improvement process.
DON, director of nursing; PICC, peripherally inserted central catheter.
The definition of a line infection was consistent and did not change throughout the 2-year study period. Outpatient criteria for central line infections are not standardized as the Centers for Disease Control and Prevention inpatient CLABSI definitions are.
The outpatient infusion pharmacy depended on information received verbally from home health nurses, physicians, and patients regarding PICC infections. The pharmacy documented patient symptoms—eg, redness, swelling, drainage at the insertion site, or fever. Medical records also often contained a report that the PICC had been removed because of infection and that antibiotic treatment had been begun. If PICC cultures or blood cultures were available and an organism was obtained, the pharmacy staff documented that information. However, the majority of infections reported were identified not by cultures but rather by symptomatology.
Statistical Methods
We used a 2-sample proportions test to assess whether infection rates were statistically different between the baseline period and the follow-up period. P values <0.05 were considered statistically significant. All statistical analyses were performed using STATA v.11 (College Station, TX).
RESULTS
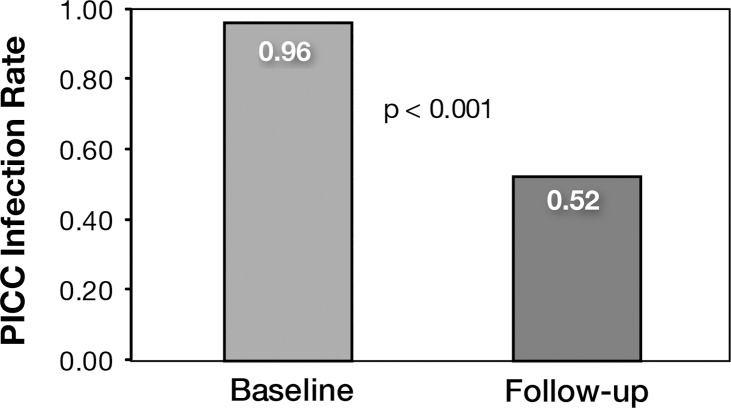
During the baseline data collection period (July 1, 2010-June 30, 2011), the infusion company identified 20 PICC infections. With 20,773 line days, we had a rate of 0.963 infections per 1,000 line days. After the new order sets and checklists were instituted (July 1, 2011-June 30, 2012), CarePoint Partners identified 11 PICC infections during 21,021 line days: 0.52 infections per 1,000 line days. The 46% reduction in PICC infection rate between baseline and follow-up was statistically significant (P<0.001) (Figure 6).
Figure 6.
Peripherally inserted central catheter (PICC) infection rates, per 1,000 line days. Baseline data were collected July 1, 2010-June 30, 2011, and follow-up data were collected July 1, 2011-June 30, 2012.
DISCUSSION
To our knowledge, this study is the first to use order sets to influence outpatient PICC care and thus significantly reduce outpatient PICC infections. We were able to overcome barriers that we faced trying to standardize care with multiple home health agencies and infusion companies by using an order set that specified how to care for central lines.
A recognized weakness of the study was the lack of an accepted definition of outpatient PICC infections. Additionally, some barriers remain because hospital medical records and results regarding PICC infections are not available to infusion companies or home health agencies. Only when an integrated medical record exists for all aspects of a patient's continuum of care will those problems be solved.
CONCLUSION
We demonstrated that outpatient PICC infections can be reduced by instituting a standardized central line care order set and patient/nurse checklists. In our patients, we reduced the PICC infection rate by 46%. Through collaboration and coordination of care, we bridged the gap that typically occurs when infusion patients are discharged home. Even though multiple nursing agencies provided care to our patients, by using an order set that detailed how we expected our PICCs to be cared for and maintained, we successfully forced standardization, improved line care, and ultimately reduced infection rates. We were able to effectively provide benefits to our patients by avoiding medical costs of readmission, additional antibiotics, and morbidity associated with PICC infections.
ACKNOWLEDGMENTS
We would like to recognize the additional members of PICC Care Team: Elaine Bergeron, Kathy Berstein, Julie Castex, Janine Chapman, Kim Duvalle, Tina Gibson, Jan Juneau, Sandy Lemoine, Craig Pennington, Michelle Poole, Judy Pons, Chris Ricord, and Fiona Winterbottom. Also, thank you to all the Ochsner healthcare teams and patients who helped make this study possible. Special thanks to Barbara Siede, medical illustrator, and Adriana Dornelles, ScD, MPH, biostatistician.
Footnotes
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, Systems-Based Practice, and Practice-Based Learning and Improvement.
REFERENCE
- 1.2013 On the CUSP: Stop HAI. http://www.onthecuspstophai.org. Accessed April 5, [Google Scholar]