Abstract
Background
A need exists for constant evaluation and modification of processes within healthcare systems to achieve quality improvement. One common approach is the Model for Improvement that can be used to clearly define aims, measures, and changes that are then implemented through a plan-do-study-act (PDSA) cycle. This approach is a commonly used method for improving quality in a wide range of fields. The Model for Improvement allows for a systematic process that can be revised at set time intervals to achieve a desired result.
Methods
We used the Model for Improvement in an acute psychiatry unit (APU) to improve the screening incidence of abnormal involuntary movements in eligible patients—those starting or continuing on standing neuroleptics—with the Abnormal Involuntary Movement Scale (AIMS).
Results
After 8 weeks of using the Model for Improvement, both of the participating inpatient services in the APU showed substantial overall improvement in screening for abnormal involuntary movements using the AIMS.
Conclusion
Crucial aspects of a successful quality improvement initiative based on the Model for Improvement are well-defined goals, process measures, and structured PDSA cycles. Success also requires communication, organization, and participation of the entire team.
Keywords: Hospitalization, inpatients, mental disorders, quality improvement
INTRODUCTION
The Model for Improvement with its plan-do-study-act (PDSA) cycles can be used in all healthcare subspecialties to create improvement that is at or above the standard of care and to lay the foundation for a desired change.1 The Veterans Administration system used the model in a pilot study to decrease average waiting times for appointments from 48 days to 22 days, a 54% improvement. Additionally, the model has been used to reduce operating room errors as well as postoperative infections.1 A great advantage of the model is that it requires measurement of progress at set time intervals and the opportunity to make changes accordingly.
The Model for Improvement defines the aim (What are we trying to accomplish?), the measures (How will we know that a change is an improvement?), and the changes (What changes can we make that will result in improvement?) necessary to improve a process.
Acute psychiatry unit (APU) staff used the model to improve patient screening for abnormal involuntary movements such as tardive dyskinesia, a neurological disorder. These movements are usually associated with chronic use of neuroleptic medications and other agents that inhibit dopaminergic activity.2 This disorder can appear in up to 33% of patients chronically receiving neuroleptic medications. In the early stages of tardive dyskinesia, the involuntary movements can be subtle and difficult for both patients and examiners to recognize. Symptoms include involuntary movements of the lips (puckering, licking, frowning), tongue (sticking tongue out, rolling tongue around in mouth), eyes (blinking), jaw, hands, arms, feet, legs (twitching, tapping), and trunk (rocking, squirming, twisting). If left untreated, the disease can progress and affect the patient's physical abilities; these abnormalities may even become permanent. The prognosis is better if the disorder is recognized and treatment is initiated early in the course of the disease.2
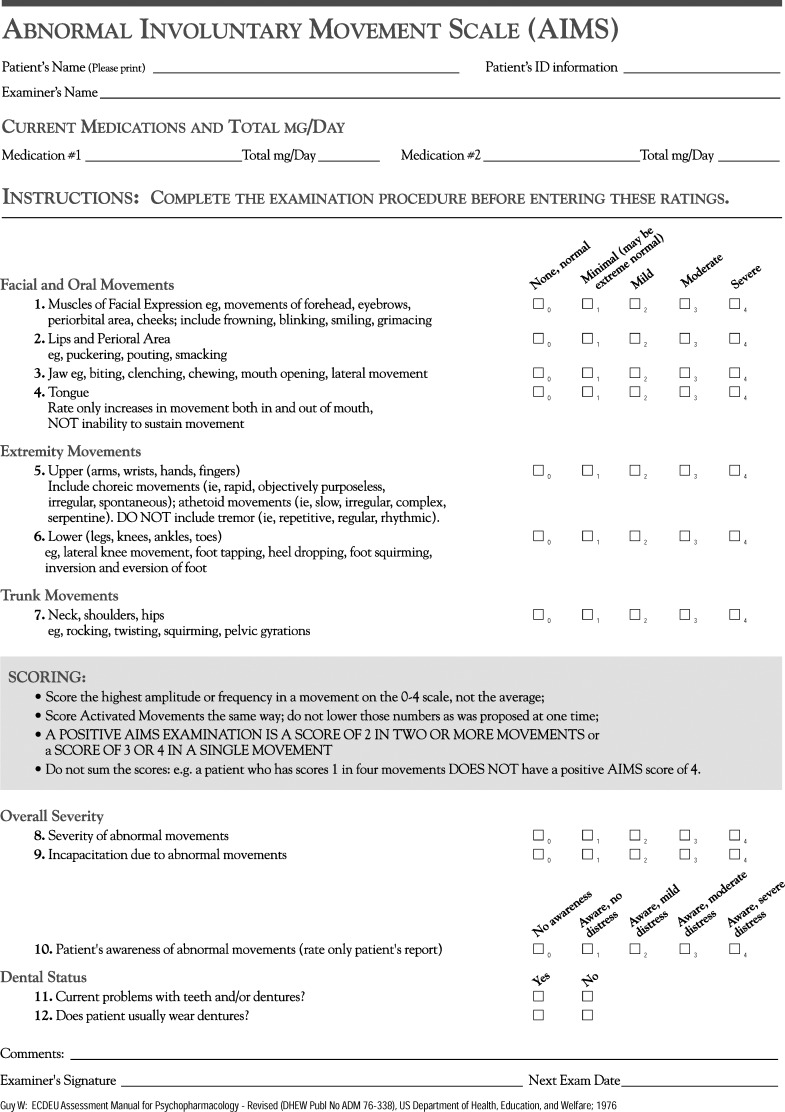
The Abnormal Involuntary Movement Scale (AIMS) (Figure 1) is the standard of care for screening. It is an objective rating scale designed to help clinicians recognize and quantify involuntary movements, including tardive dyskinesia.3 Usually administered every 3 to 6 months to both screen for and to monitor the severity of tardive dyskinesia, the test includes 12 items that the clinician rates in terms of the severity of involuntary movements of the patient's body (with 0 representing no abnormality and 4 indicating severe disability).4
Figure 1.
The Abnormal Involuntary Movement Scale.
Our goal was to determine as quickly as possible any signs of abnormalities and to treat patients early in the disease process when the treatment presents little risk compared to benefit.
METHODS
The acute inpatient psychiatric unit is composed of 2 services. Both of these services work alongside the quality improvement team and help screen patients, gather data, and treat patients as clinically indicated.
We retrospectively reviewed all cases of patients admitted to the 2 APU inpatient services over a 1-week period to evaluate how many patients starting or continuing on standing neuroleptics were screened with the AIMS. The retrospective analysis showed a lack of screening and documentation. Consequently, we sought to standardize screening with the AIMS for abnormal involuntary movements in patients treated with antipsychotic medications in the APU. To work toward the goal of 50% screening by 4 weeks, we established a quality improvement team that included the director, 2 staff attendings, the nursing manager, and 2 residents who communicated with the inpatient services. The time frame for the PDSA cycle was defined as Sunday to Saturday (7 days), allowing for weekly analysis and intervention.
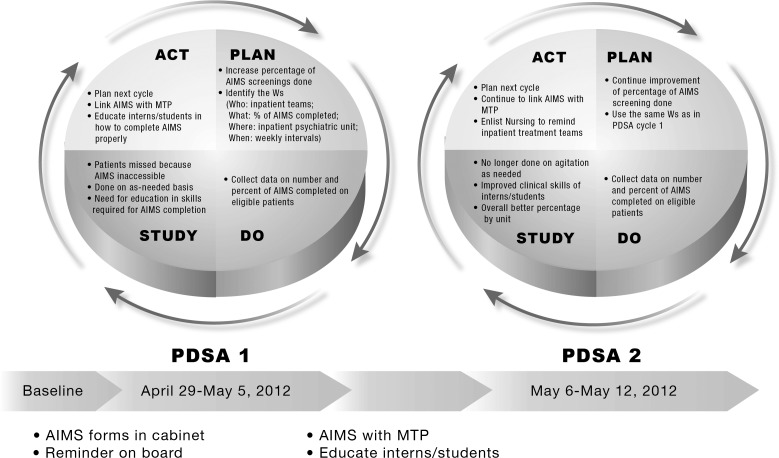
Each review of the retrospective week displayed many potential areas for improvement, including the lack of availability and accessibility of the AIMS and the need for further education of ancillary staff. Prior to each PDSA cycle, we identified clear goals to address a particular insufficiency and recommended improvements (Figure 2). After the first week, we noticed that some patients were not being screened with the AIMS because of oversight by the inpatient services. To correct this oversight, we implemented an intervention that included reminders and addressed the availability and accessibility of the AIMS. Furthermore, the AIMS was eventually linked with the mandatory master treatment plan (MTP) conducted at initial intake. After the second PDSA cycle, data about eligible patients and the number of screening AIMS completed were documented on the daily rounds list, proving quite beneficial. The benefits included the regular weekly monitoring of and documentation about eligible patients and a clear avenue for tracking completed screenings. During subsequent PDSA cycles, further enhancement of the clinical skills of rotating clerkship students, improving transition handoffs, and managing vacation coverage became a focus. Data were analyzed at regular intervals to monitor compliance with the PDSA cycles.
Figure 2.
Plan-do-study-act (PDSA) cycles.AIMS, Abnormal Involuntary Movement Scale; MTP, master treatment plan.
RESULTS
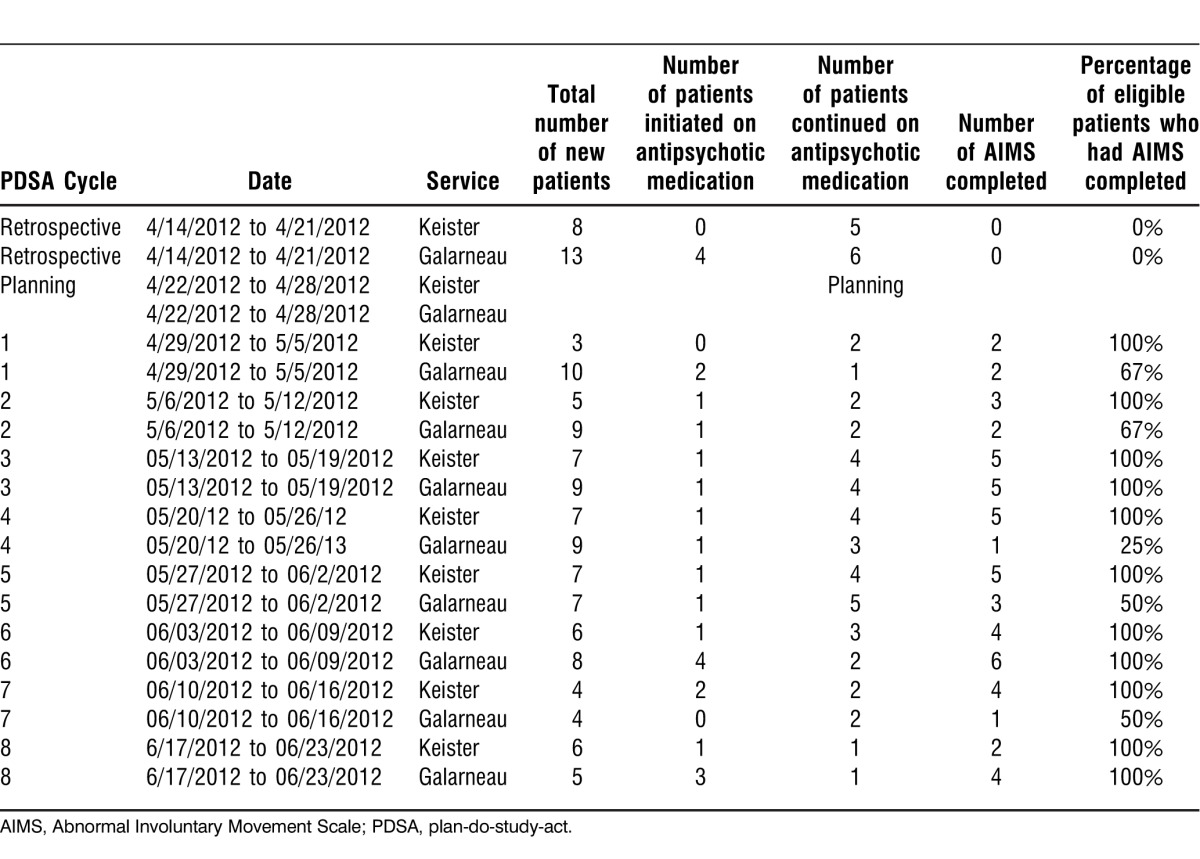
After 8 weeks of PDSA cycles, both inpatient services showed substantial overall improvement in screening for abnormal involuntary movements with the AIMS (Table). At the end of 8 PDSA cycles, 1 service successfully screened 100% of eligible patients via AIMS, and the second service screened an average 70% of eligible patients, an overall average of 85% for the APU. AIMS results for 2 patients were positive at the time of initial intake; their abnormal movements were addressed via appropriate pharmacological interventions, resulting in improvement illustrated by improved AIMS findings on repeat examination.
Table.
Abnormal Involuntary Movement Scale Quality Improvement Data
DISCUSSION
The lifecycle of a quality improvement project consists of innovation (coming up with new ideas for change), a pilot (testing change on a small scale), implementation (making the change a part of daily routine), and spread (using the new process in different settings).1 Both APU services demonstrated that by using the Model for Improvement and structured PDSA cycles, they could achieve a specific quality improvement goal. Some of the challenges noted during the study were communication problems with various members of the multidisciplinary services, educating clerkship students to develop the necessary skills to correctly complete the AIMS, staffing issues related to vacations that resulted in handoffs lacking data collection, and patient cooperation.
We found it beneficial to schedule weekly PDSA cycles because the frequency allowed for timely analysis that ensured interventions for process improvement. Even after the 8 weeks of PDSA cycles had been analyzed, both APU services continued to show improvement in screening eligible patients. We noted that specific areas hindering improvement could be focused on in subsequent PDSA cycles, allowing for a timely resolution and continued improvement. The model's capabilities to yield improvement go beyond the APU and could be used in any situation in which a specific improvement is desired.
CONCLUSION
The Model for Improvement and structured PDSA cycles are essential tools for individuals or organizations attempting process improvement to advance quality. In the medical setting, some sample uses include reducing emergency department waiting times, improving compliance with safety standards in the medical and surgical units, and decreasing infections via increased hand hygiene compliance.1 Much of the success from using the Model for Improvement involves communication, organization, and participation of the entire multidisciplinary team: incorporating changes in the unit's culture rather than having a single individual attempt to implement the change.
Various organizations have tested this method and proven it effective time and time again, including in the healthcare model. Crucial aspects of the process are well-defined goals, process measures, and structured PDSA cycles with regularly scheduled meetings of the quality improvement team to discuss challenges. We hope that other departments within our organization will use the Model for Improvement and structured PDSA cycles to improve the quality of processes and to strive for excellent patient care.
Footnotes
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Practice-Based Learning and Improvement.
REFERENCES
- 1.Institute for Healthcare Improvement. How to Improve. 2013 December 4, 2012. http://www.ihi.org/knowledge/Pages/HowtoImprove/default.aspx. Accessed May 20. [Google Scholar]
- 2.Advameg, Inc. Tardive dyskinesia. Encyclopedia of Mental Disorders. 2012 http://www.minddisorders.com/Py-Z/Tardive-dyskinesia.html. Accessed July 14. [Google Scholar]
- 3.Abnormal Involuntary Movement Scale. 2012 http://www.mymsw.info/downloads/aims.pdf. Accessed September 14. [Google Scholar]
- 4.Advameg, Inc. Abnormal Involuntary Movement Scale. Encyclopedia of Mental Disorders. 2013 http://www.minddisorders.com/A-Br/Abnormal-Involuntary-Movement-Scale.html. Accessed May 20. [Google Scholar]