Abstract
Background
Thromboprophylaxis with oral anticoagulants is an important but underused element of atrial fibrillation (AF) treatment. Reduction of stroke risk by anticoagulants comes at the price of bleeding risk. Patients with AF receiving anticoagulants require heightened attention with transition from one care setting to another.
Methods
This review of the literature focuses on issues specific to the anticoagulation treatment of patients with AF.
Results
Patients presenting for emergency care of anticoagulant-related bleeding should be triaged for the severity and source of the bleeding using appropriate measures, such as discontinuing the oral anticoagulant, administering vitamin K when appropriate to reverse warfarin-induced bleeding, or administering clotting factors for emergent bleeding. Reversal of oral anticoagulants in patients admitted to the hospital for surgery can be managed similarly to patients with bleeding, depending on the urgency of the surgical procedure. Patients with AF who are admitted for conditions unrelated to AF should be assessed for adequacy of stroke risk prophylaxis and bleeding risk. Newly diagnosed AF should be treated in nearly all patients with either warfarin or a newer anticoagulant.
Conclusions
Patient education is critically important with all anticoagulants. Close adherence to the prescribed regimen, regular international normalized ratio testing for warfarin, and understanding the stroke risk conferred by AF and aging are goals for all patients receiving oral anticoagulants. Detailed handoff from the hospitalist to the patient's primary care physician is required for good continuity of care. Monitoring by an anticoagulation clinic is the best arrangement for most patients. The elderly, particularly frail or debilitated patients who are transferring to long-term care, need a detailed transfer of information between settings, education for the patient and family, and medication reconciliation. Communication and coordination of care among outpatient, emergency, inpatient, subacute, and long-term care settings are vital in patients with AF who are receiving anticoagulants to balance stroke prevention and bleeding risk.
Keywords: Anticoagulant drugs, atrial fibrillation, hemorrhage, stroke
INTRODUCTION
Atrial fibrillation (AF) affects an estimated 2.66 million people in the United States.1 The prevalence of this age-related condition ranges from <1% of the population aged <60 years to approximately 10% of the population aged ≥80 years.2 Approximately 70% of patients with AF are aged 65 to 85 years.3 With the aging population, the incidence of AF is expected to rise to >5.6 million by 2050.2
Symptoms of AF range from no symptoms to a significant degree of morbidity, including fatigue, palpitations, and acute pulmonary edema.4 AF is also associated with an increased risk for cognitive impairment, depression, and dementia.5,6 More important, AF is an associated factor in up to 1 in 5 strokes in the United States7,8 and increases stroke risk approximately 5-fold.9 Approximately 15% of the 795,000 new or recurrent strokes that occur each year are associated with AF.10,11 Stroke risk is most commonly assessed with the CHADS2 scoring system, which stratifies stroke risk by assigning 1 point each for the presence of congestive heart failure, hypertension, age ≥75 years, and/or diabetes mellitus, and 2 points for a history of stroke or transient ischemic attack. A score of 0 is considered low risk for stroke, 1 indicates moderate risk, and ≥2 indicates high risk.12 Recently updated guidelines for antithrombotic therapy in patients with AF use the CHADS2 system for treatment decisions. Patients with AF and a CHADS2 score of 0 should receive no antithrombotic therapy unless a patient desires antithrombotic therapy, in which case low-dose aspirin, rather than oral anticoagulation or combination therapy with aspirin and clopidogrel, should be prescribed. For a CHADS2 score of 1, oral anticoagulants, rather than aspirin or combination therapy with aspirin and clopidogrel, are appropriate. For a CHADS2 score of ≥2, oral anticoagulants should be used.13
This article reviews issues specific to anticoagulation treatment of patients with AF and the communication and coordination of care that are essential to prevent untoward outcomes.
GUIDELINES, RISK FACTORS, AND NOVEL AGENTS FOR AF
As guidelines indicate, oral anticoagulants as thromboprophylaxis are a cornerstone of AF treatment.14 Anticoagulation with warfarin is associated with a 68% relative risk reduction of stroke.15 For patients newly diagnosed with AF, current guidelines for initiation of anticoagulant therapy recommend starting warfarin with doses between 5 and 10 mg for the first 1 or 2 days for most individuals and subsequent dosing based on the international normalized ratio (INR) level response. The initial warfarin dose should be reduced when other clinical factors increase the risk for hemorrhage, including advanced age, debilitation, malnourishment, congestive heart failure, liver disease, recent major surgery, or medications known to increase the sensitivity to warfarin (eg, amiodarone). For patients with these risk factors, the starting dose of warfarin should be <5 mg, with subsequent dosing based on the INR value response.16
Among patients receiving warfarin, the time in therapeutic range varies from 29% to 75%; the wide variance may be explained by patient population differences and methods of warfarin dosing and measuring time in therapeutic range.17 Newer anticoagulants offer the advantage of more consistent anticoagulation. Dabigatran, a direct thrombin inhibitor, was approved by the U.S. Food and Drug Administration in 2010 for reduction of the risk of stroke and systemic embolism in patients with nonvalvular AF. The pivotal Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) trial compared dabigatran and dose-adjusted warfarin in >18,000 patients. Dabigatran 150 mg improved the primary outcome—stroke or systemic embolism—compared with warfarin (1.1% vs 1.7%, P<0.001 for superiority), yielding a number needed to treat (NNT) of 167 patients. Dabigatran 150 mg was associated with fewer intracranial bleeds but with similar rates of major hemorrhage.18-20 A cost-effectiveness analysis suggests that dabigatran 150 mg is cost effective in AF populations at high risk for hemorrhage or at high risk for stroke unless INR control with warfarin is excellent. In moderate-risk AF populations, warfarin may be more cost effective than dabigatran unless INR control is poor.21 Poor INR control equates to INR levels that are often outside the range of 2-3.
Guidelines for the management of AF were recently updated to include dabigatran.22 Patients with normal renal function should receive dabigatran 150 mg twice daily. For patients with a creatinine clearance (CrCl) of 15 to 30 mL/min, the recommended dose of dabigatran is 75 mg twice daily. There is no dosage recommendation for patients with CrCl <15 mL/min or for patients on dialysis.
Rivaroxaban, a factor Xa inhibitor, is the most recent addition to oral anticoagulant options. The pivotal Rivaroxaban Once Daily Oral Direct Factor Xa Inhibitor Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (ROCKET-AF) compared rivaroxaban with dose-adjusted warfarin in >14,000 patients. Rivaroxaban improved the primary outcome—stroke or systemic embolism—compared with warfarin (1.7% vs 2.3%, P<0.001 for noninferiority), yielding an NNT of 222 patients. Rivaroxaban was associated with fewer intracranial bleeds but with similar rates of major hemorrhage.23 Rivaroxaban may be a cost-effective alternative to adjusted-dose warfarin for stroke prevention in patients with AF.24 Patients with a CrCl >50 mL/min should receive rivaroxaban 20 mg with the evening meal. The dose should be reduced to 15 mg for those with a CrCl of 15 to 50 mL/min. There is no dosage recommendation for patients with a CrCl <15 mL/min.25
The benefit of reducing stroke risk must be balanced with the increased risk of bleeding. The HAS-BLED scoring system can be used to predict bleeding risk. HAS-BLED rates bleeding risk by adding 1 point each for hypertension (systolic blood pressure >160 mmHg), abnormal renal function (dialysis, renal transplant, serum creatinine level >2.3 mg/dL), abnormal hepatic function (chronic liver disease, bilirubin >2 times the upper limit of normal, liver enzymes >3 times the upper limit of normal), prior stroke, prior bleeding (major bleeding history, anemia, predisposition to bleeding), labile INRs (unstable INRs or poor time in therapeutic range), elderly (aged >65 years), drug therapy (concomitant antiplatelet drugs, nonsteroidal antiinflammatory drugs), and alcohol (>8 drinks per week) for a maximum of 9 points.26 In the HAS-BLED scoring system, a score of 0-1 indicates low risk for bleeding in AF patients, a score of 2 indicates intermediate risk, and high risk is a score of ≥3. A high HAS-BLED score should not be the cause for avoiding or stopping anticoagulation but should indicate patients who need extra review and follow-up.
Renal dysfunction is a particular concern in patients with AF. The prevalence of AF among all patients with renal dysfunction is 18% and increases to 25% in patients aged >70 years.27 Severe renal dysfunction carries the increased risk of both bleeding and thrombosis, increasing the complexity of anticoagulation management.28
Dabigatran is primarily eliminated renally. Use of dabigatran, including the 75 mg dose, has not been studied in patients with a CrCl <15 mL/min and should not be used for them. Renal excretion accounts for about two-thirds of rivaroxaban elimination; half of this is eliminated as unchanged drug. Use of rivaroxaban in patients with a CrCl <15 mL/min is not recommended.25 Renal clearance is a very minor route of warfarin elimination. Closely monitored warfarin may be the preferred anticoagulant in patients with severe renal dysfunction; however, moderate and severe renal dysfunction may reduce warfarin dose requirements to avoid bleeding risk.29
Transition of patients from one care setting to another poses additional risk.30-32 The care of patients with AF receiving antithrombotic therapy who are transitioning from the community to the hospital and back again requires consideration of multiple factors. These factors include weighing the benefits of transfer and the risks of complications, such as bleeding or thrombosis, care strategies for healthcare providers, and the additional burdens patients incur.32-37
Hospital admission is common for patients with AF. In a population of >55,000 patients aged ≥65 years with AF, more than half were admitted to the hospital for AF within the 24-month observation period; 43.7% of the admissions were for readmissions and comorbidities, notably hypertension (80.5%), structural heart disease (32.9%), coronary artery disease (23.1%), and diabetes (19%), and 60% of patients were receiving warfarin.38 Anticoagulation requires close monitoring and adjustment depending on clinical circumstances as the patient moves through various care settings.14 Good communication and the continuity of care among providers are key in mitigating risk.39-43
TRANSITION TO INPATIENT CARE
The number of warfarin-treated patients presenting for emergency care is increasing, especially elderly patients.44 Additionally, patients' INR levels are often outside of the therapeutic range.45 Warfarin use is a powerful marker of mortality risk,44 making accurate identification and anticipation of risk crucial for optimal outcomes. Patients receiving warfarin often present for emergency care with epistaxis or other minor hemorrhages (eg, bleeding from small cuts) or for asymptomatic supratherapeutic INR.46 Anticoagulated patients with bleeding should initially receive the same care as any patient with bleeding, including identification of the bleeding source with local hemostasis where possible, fluids, and red blood cells. In cases of warfarin overdose, activated charcoal may be used empirically to reduce warfarin absorption if ingestion has been within the previous 2 hours.47 In vitro research suggests that charcoal may reduce warfarin absorption.48 No research is available about the use of charcoal for rivaroxaban overdose, but could be considered.25
Reversing overanticoagulation while maintaining enough anticoagulation to reduce stroke risk is a challenging balance that requires a cautious approach. In general, a light-handed approach is best for reversing overanticoagulation. Simply stopping warfarin, monitoring the INR values, and restarting warfarin at a lower dose may be sufficient in some cases.49 For many patients, low-dose vitamin K may be appropriate to return the INR value to a therapeutic range more quickly. Simple warfarin interruption is likely to result in a slower decline in INR values in patients with recent surgery, active malignancy, or decompensated heart failure, and in elderly patients, especially those who require low weekly doses of warfarin (<15 mg) to maintain therapeutic anticoagulation.50 INR levels from 6 to 10 typically decline to <4 within 2.5 days with warfarin discontinuation alone and within 1.4 days with a 1.0-2.5 mg dose of oral vitamin K.51,52 In patients without bleeding who have an INR level of 4.5 to 10.0, 1 mg of oral vitamin K not only lowers the INR level into the therapeutic range more quickly than withholding warfarin, but also avoids the warfarin resistance seen when larger vitamin K doses are administered.51-53 For patients with INR levels >10 and no serious symptoms, 2 mg of oral vitamin K has been used safely.54 As noted above, when administered with temporary interruption of warfarin, vitamin K lowers an INR range of 6-10 to 4 in about 1.4 days.55
For cases of non–life-threatening bleeding, both oral and intravenous (IV) vitamin K will have the same effect within 24 hours. However, IV vitamin K causes INR level correction within 6 to 8 hours and may be more desirable when more rapid reversal is required.56,57 Current guidelines recommend vitamin K 1-5 mg orally for patients without serious bleeding. For serious bleeding, the guidelines recommend vitamin K 10 mg mixed in a minimum of 50 mL of IV fluid and infused over ≥20 minutes.16,55 Lower doses (1-5 mg) of IV vitamin K may be as effective as higher doses.58 In a metaanalysis of studies of patients treated with vitamin K antagonists, the case-fatality rate of major bleeding was 9.1% (95% confidence interval, 2.5%-21.7%).59 Life-threatening hemorrhages, such as intracerebral bleeds or those from a gastrointestinal source, require emergent reversal with fresh frozen plasma, prothrombin complex concentrate, or recombinant factor VIIa in addition to IV vitamin K.16
Newer anticoagulants, including the direct thrombin inhibitor dabigatran and factor Xa inhibitors such as rivaroxaban and apixaban, work differently in the coagulation cascade and therefore are not affected by vitamin K administration. All have shorter half-lives than warfarin with a shorter duration of anticoagulant effect. For minor bleeding, simply stopping dabigatran or rivaroxaban may be sufficient because of their short half-lives.
Many healthcare providers are concerned about the unavailability of reversal agents for the newer anticoagulants. However, this concern should be tempered with the fact that both new anticoagulants have a much shorter duration of anticoagulant effect than warfarin and that reversal of warfarin with vitamin K is not immediate. Unless immediate reversal is required, the conservative approach of simply stopping the drug (whether a newer anticoagulant or warfarin) is often prudent.
For clinically important bleeding, dabigatran can be dialyzed (protein binding is low). However, clinical data supporting this approach are limited. Consider surgical hemostasis or the transfusion of fresh frozen plasma or red blood cells. Some experimental evidence supports the role of activated prothrombin complex concentrates (eg, factor IIa inhibitor bypass activity [FEIBA recombinant factor VIIa or concentrates of coagulation factors II, IX, or X]). However, the usefulness of these concentrates in clinical settings has not been established. Platelet concentrates can be used in cases where thrombocytopenia is present or long-acting antiplatelet drugs have been used. Measurement of the activated partial thromboplastin time or ecarin clotting time may help guide therapy for a decrease in hemoglobin and/or hematocrit or hypotension. Presently, no specific reversal agent for dabigatran is available.60-62 Rivaroxaban is highly protein bound, making removal by hemodialysis unlikely. Use of reversal agents such as prothrombin complex concentrate, activated prothrombin complex concentrate, or recombinant factor VIIa may be considered but has not been evaluated in clinical trials.25
For urgent or emergent surgery, the decision of drug withdrawal or use of reversal agents is determined by the time sensitivity of the clinical situation. It is important to remember that neither warfarin nor the newer anticoagulants cause bleeding but instead limit the ability of the body to stop bleeding. Reversal of warfarin with vitamin K is not rapid, compared with reversal of heparin with protamine.63 Persistent INR level elevation may require vitamin K dosing repeated every 12 hours.16
Patients taking anticoagulants who present for emergency care for unrelated conditions should be evaluated for the intensity of anticoagulation and the risk for bleeding and thromboembolic complications. Management of anticoagulation should be transitioned to the patient's primary care physician or anticoagulation clinic for patients to be discharged, and for those requiring inpatient care, to the admitting physician or hospitalist and the hospital's anticoagulation monitoring service. Patients with AF who are admitted for inpatient care should be assessed for adequacy of stroke risk prophylaxis and bleeding risk using risk-assessment tools, such as CHADS2 and HAS-BLED. The risks for bleeding and hemorrhage are higher in warfarin-naïve patients, suggesting the need for added vigilance with initiation of anticoagulation.64
Newly prescribed drugs and maintenance medications should be reviewed for drug interactions that are common with warfarin. Newer anticoagulants are less prone to drug interactions than warfarin.65 Patients should be questioned about medication adherence. For patients receiving warfarin, INR levels should also be assessed. For patients receiving a newer anticoagulant, INR levels cannot be used to assess coagulation.
Patients requiring transition from one anticoagulant to another should be managed with consideration of each agent's half-life and onset of effect (Table 1). Patients who require surgery or who are unable to take oral medication may require transition to parenteral anticoagulants. Depending on the bleeding risk associated with the surgical procedure and patient risk of thromboembolism, warfarin is discontinued several days before the procedure, and bridging (the use of unfractionated heparin or low molecular weight heparin to prevent clots during the perioperative period and to reduce bleeding risk during and after surgery) may be necessary.66 How to switch from a newer anticoagulant to a parenteral anticoagulant and vice versa are detailed in Table 1.
Table 1.
How to Switch To/From Parenteral Anticoagulants and Warfarin To/From Newer Oral Anticoagulants25,62
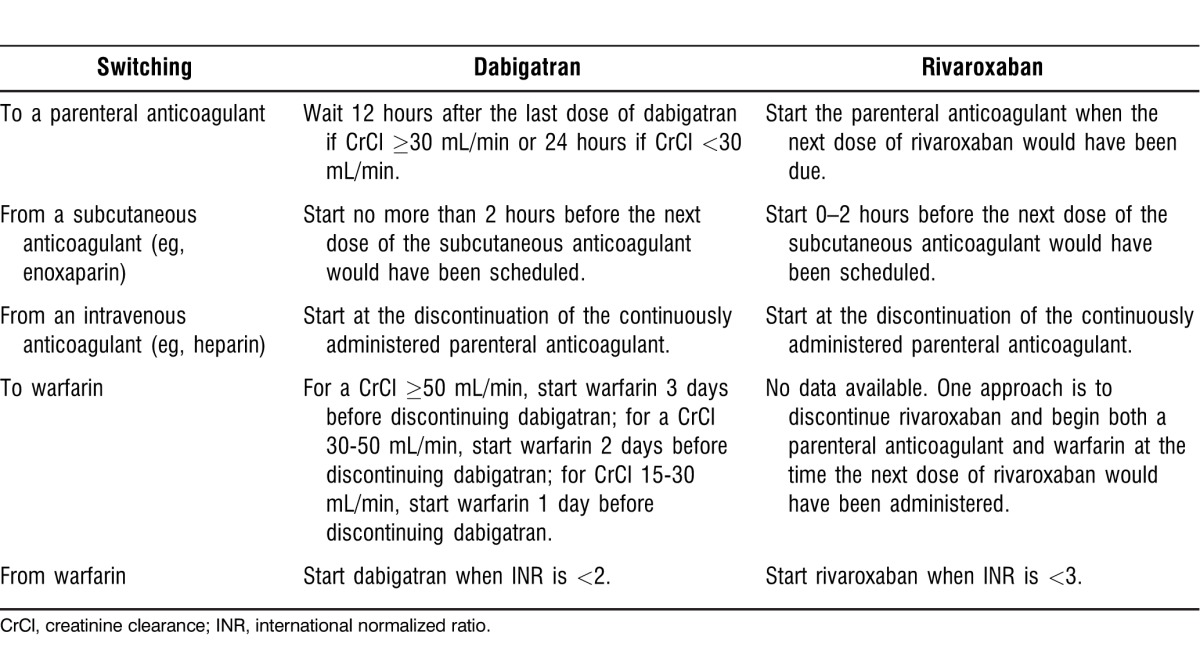
When switching from dabigatran to a parenteral anticoagulant, 12 hours should elapse after the last dose of dabigatran for patients with a CrCl ≥30 mL/min, and 24 hours should elapse after the last dose of dabigatran for patients with a CrCl <30 mL/min. When switching from a parenteral anticoagulant to dabigatran, dabigatran should be started no more than 2 hours before the next dose of the parenteral anticoagulant (eg, enoxaparin) would have been scheduled. Dabigatran has a rapid onset of anticoagulant effect and can be started at the time of discontinuation of a continuously administered parenteral anticoagulant (eg, IV heparin).
TRANSITION TO OUTPATIENT CARE
Prior to discharge, patients leaving inpatient care should be referred to the care management team to facilitate transition to at-home or long-term care. Facets of moving the patient to outpatient care include detailed transfer of information between settings, education of the patient and caregiver, medication reconciliation, and a plan for follow-up medical care that includes pending test results.67 Newer anticoagulants require the investigation of insurance coverage and the patient's ability to pay for the medication.
Patients receiving warfarin who will be discharged to self-care will require handoff to a provider for INR monitoring. Referral to a formal, structured management program, such as an anticoagulant clinic, is ideal for most patients.16 For highly motivated patients, self-monitoring may be an option.68
Patient education is critically important for both warfarin and the newer anticoagulants. Persistence and adherence to medication regimens increases with patient understanding of why medications are prescribed and of potential side effects.69,70 Education for patients receiving warfarin should include information on drug and dietary interactions and the importance of regular INR monitoring.16 Education for patients receiving the newer anticoagulants should include an explanation about the importance of taking medication as prescribed, given the short duration of anticoagulant effect compared with warfarin and dangers of abruptly stopping medication without medical advice. Patients and their caregivers should know the signs and symptoms of bleeding and how to differentiate minor bleeding from bleeding that requires medical attention.25,62 Transition to long-term care should be similar to hospital-to-hospital transfer, with systematic methods in place to ensure a complete handoff.71 Measures to ensure that anticoagulant doses are not missed or duplicated during the transition are critically important to avoid increased risk for stroke or bleeding.67
Elderly patients with AF face several related hazards that require special consideration in anticoagulation, including increased risk for stroke, bleeding, and other adverse effects, interactions with warfarin, comorbid conditions, and falls. As a result, anticoagulation is underprescribed in elderly patients with AF. The risk of falling or advanced age should not be an absolute or relative contraindication to anticoagulation; potential benefit (stroke prevention) versus bleeding risk should be carefully considered for each patient.72,73 Given that nearly 75% of the total costs associated with AF are attributed to direct and indirect hospitalization costs,74 clinical strategies that can reduce AF-related hospitalizations may optimize care by improving clinical outcomes and reducing costs.
CONCLUSIONS
Transition of care among various care settings presents multiple challenges.30,31,75 Anticoagulated patients with AF generate additional requirements for information transfer on transition to inpatient care and back to outpatient care (Table 2). Anticoagulated patients admitted with bleeding should be treated based on the severity of bleeding or for an invasive procedure. For many patients, simply withholding the anticoagulant may be the safest management strategy. Patients naïve to an anticoagulant require close monitoring, given the higher risk for both stroke and bleeding within the first several months of treatment.
Table 2.
Elements of a Good Care Transition for Patients Receiving Anticoagulation
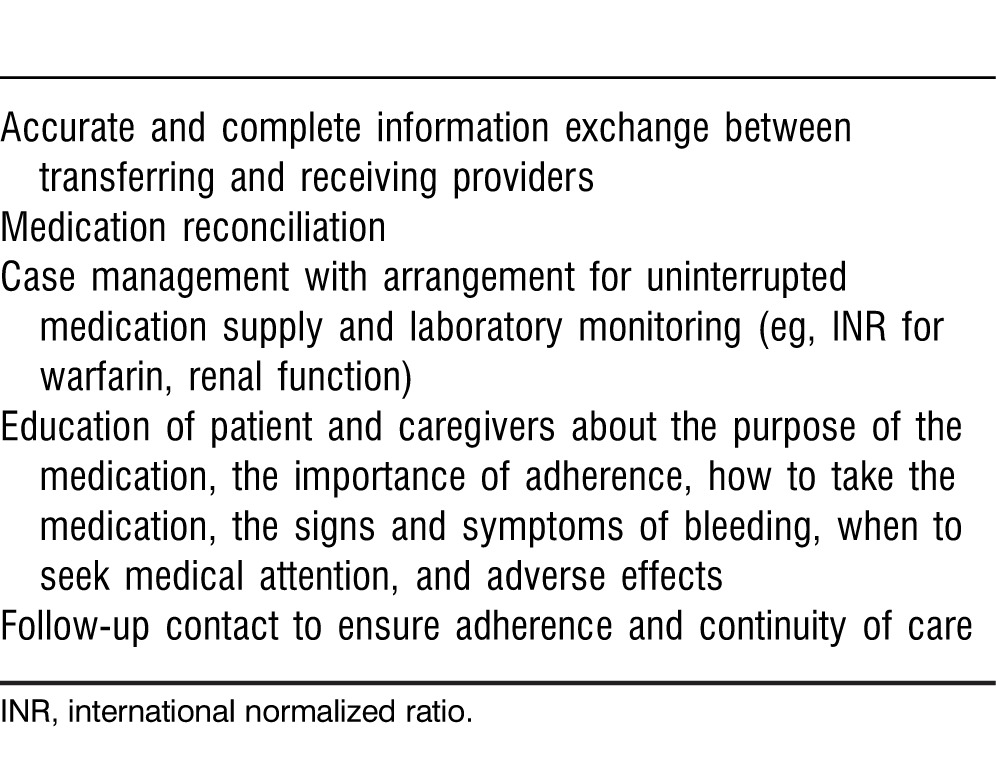
For patients transitioning to outpatient care, involvement of a care manager can ensure attention to practical issues, such as educating the patient and caregiver, securing an uninterrupted source of medication, and arranging follow-up care and laboratory tests that may decrease the risk for rehospitalization. Inadvertent discontinuation of anticoagulant therapy and poor adherence are frequent causes of hospital readmission.76 The impact of the availability of dabigatran and the new factor Xa inhibitors, such as rivaroxaban23 and apixaban,77 is yet to be seen. However, vigilant transition of care of patients receiving anticoagulation will continue to be a key element in achieving the best patient outcomes.
Footnotes
The author has no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, Systems-Based Practice, and Practice-Based Learning and Improvement.
REFERENCES
- 1.Kannel WB, Benjamin EJ. Status of the epidemiology of atrial fibrillation. Med Clin North Am. 2008 Jan;92(1):17–40. doi: 10.1016/j.mcna.2007.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001 May 9;285(18):2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 3.Feinberg WM, Blackshear JL, Laupacis A, Kronmal R, Hart RG. Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch Intern Med. 1995 Mar 13;155(5):469–473. [PubMed] [Google Scholar]
- 4.Page RL. Clinical practice. Newly diagnosed atrial fibrillation. N Engl J Med. 2004 Dec 2;351(23):2408–2416. doi: 10.1056/NEJMcp041956. [DOI] [PubMed] [Google Scholar]
- 5.Sabatini T, Frisoni GB, Barbisoni P, Bellelli G, Rozzini R, Trabucchi M. Atrial fibrillation and cognitive disorders in older people. J Am Geriatr Soc. 2000 Apr;48(4):387–390. doi: 10.1111/j.1532-5415.2000.tb04695.x. [DOI] [PubMed] [Google Scholar]
- 6.Bellomo A, De Benedetto G, Fossati C, et al. Atrial fibrillation (AF) and cognitive impairment in the elderly: a case-control study. Arch Gerontol Geriatr. 2012 Sep-Oct;55(2):247–250. doi: 10.1016/j.archger.2011.07.017. Epub 2011 Sep 22. [DOI] [PubMed] [Google Scholar]
- 7.Marini C, De Santis F, Sacco S, et al. Contribution of atrial fibrillation to incidence and outcome of ischemic stroke: results from a population-based study. Stroke. 2005 Jun;36(6):1115–1119. doi: 10.1161/01.STR.0000166053.83476.4a. Epub 2005 May 5. [DOI] [PubMed] [Google Scholar]
- 8.Romero JR, Morris J, Pikula A. Stroke prevention: modifying risk factors. Ther Adv Cardiovasc Dis. 2008 Aug;2(4):287–303. doi: 10.1177/1753944708093847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991 Aug;22(8):983–988. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 10.Roger VL, Go AS, Lloyd-Jones DM, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Executive summary: heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012 Jan 3;125(1):188–197. doi: 10.1161/CIR.0b013e3182456d46. Erratum in: Circulation. 2012 Jun 5;125(22):e1001. [DOI] [PubMed] [Google Scholar]
- 11.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation: a major contributor to stroke in the elderly. The Framingham Study. Arch Intern Med. 1987 Sep;147(9):1561–1564. [PubMed] [Google Scholar]
- 12.Olesen JB, Lip GY, Hansen ML, et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011 doi: 10.1136/bmj.d124. Jan 31;342:d124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.You JJ, Singer DE, Howard PA, et al. American College of Chest Physicians. Antithrombotic therapy for atrial fibrillation: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141((2 Suppl)):e531S–e575S. doi: 10.1378/chest.11-2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fuster V, Rydén LE, Cannom DS, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines; European Society of Cardiology Committee for Practice Guidelines; European Heart Rhythm Association; Heart Rhythm Society. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006 Aug 15;114(7):e257–e354. doi: 10.1161/CIRCULATIONAHA.106.177292. Erratum in: Circulation. 2007 Aug 7;116(6):e138. [DOI] [PubMed] [Google Scholar]
- 15.Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994 Jul 11;154(13):1449–1457. Erratum in: Arch Intern Med. 1994 Oct 10;154(19):2254. [PubMed] [Google Scholar]
- 16.Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G. American College of Chest Physicians. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008 Jun;133((6 Suppl)):160S–198S. doi: 10.1378/chest.08-0670. [DOI] [PubMed] [Google Scholar]
- 17.Wan Y, Heneghan C, Perera R, et al. Anticoagulation control and prediction of adverse events in patients with atrial fibrillation: a systematic review. Circ Cardiovasc Qual Outcomes. 2008 Nov;1(2):84–91. doi: 10.1161/CIRCOUTCOMES.108.796185. Epub 2008 Nov 5. [DOI] [PubMed] [Google Scholar]
- 18.Connolly SJ, Ezekowitz MD, Yusuf S, et al. RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009 Sep 17;361(12):1139–1151. doi: 10.1056/NEJMoa0905561. Epub 2009 Aug 30. Erratum in: N Engl J Med. 2010 Nov 4;363(19):1877. [DOI] [PubMed] [Google Scholar]
- 19.Eikelboom JW, Wallentin L, Connolly SJ, et al. Risk of bleeding with 2 doses of dabigatran compared with warfarin in older and younger patients with atrial fibrillation: an analysis of the randomized evaluation of long-term anticoagulant therapy (RE-LY) trial. Circulation. 2011 May 31;123(21):2363–2372. doi: 10.1161/CIRCULATIONAHA.110.004747. Epub 2011 May 16. [DOI] [PubMed] [Google Scholar]
- 20.Wallentin L, Yusuf S, Ezekowitz MD, et al. RE-LY investigators. Efficacy and safety of dabigatran compared with warfarin at different levels of international normalised ratio control for stroke prevention in atrial fibrillation: an analysis of the RE-LY trial. Lancet. 2010 Sep 18;376(9745):975–983. doi: 10.1016/S0140-6736(10)61194-4. [DOI] [PubMed] [Google Scholar]
- 21.Shah SV, Gage BF. Cost-effectiveness of dabigatran for stroke prophylaxis in atrial fibrillation. Circulation. 2011 Jun 7;123(22):2562–2570. doi: 10.1161/CIRCULATIONAHA.110.985655. Epub 2011 May 23. [DOI] [PubMed] [Google Scholar]
- 22.Wann LS, Curtis AB, January CT, et al. 2006 Writing Committee Members. Jacobs AK, JL Anderson, Albert N, et al., editors. ACCF/AHA Task Force Members. ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (updating the 2006 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011 Jan 4. 2011;123(1):104–123. doi: 10.1161/CIR.0b013e3181fa3cf4. Epub 2010 Dec 20. Erratum in: Circulation. 2011 Aug 2;124(5):e173. [DOI] [PubMed] [Google Scholar]
- 23.Patel MR, Mahaffey KW, Garg J, et al. ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011 Sep 8;365(10):883–891. doi: 10.1056/NEJMoa1009638. Epub 2011 Aug 10. [DOI] [PubMed] [Google Scholar]
- 24.Lee S, Anglade MW, Pham D, Pisacane R, Kluger J, Coleman CI. Cost-effectiveness of rivaroxaban compared to warfarin for stroke prevention in atrial fibrillation. Am J Cardiol. 2012 Sep 15;110(6):845–851. doi: 10.1016/j.amjcard.2012.05.011. Epub 2012 May 30. [DOI] [PubMed] [Google Scholar]
- 25.Xarelto (rivaroxaban) [package insert. 2012 http://www.xareltohcp.com/sites/default/files/pdf/xarelto_0.pdf#zoom=100. Accessed September 6. [Google Scholar]
- 26.Lip GY, Frison L, Halperin JL, Lane DA. Comparative validation of a novel risk score for predicting bleeding risk in anticoagulated patients with atrial fibrillation: the HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile INR, Elderly, Drugs/Alcohol Concomitantly) score. J Am Coll Cardiol. 2011 Jan 11;57(2):173–180. doi: 10.1016/j.jacc.2010.09.024. Epub 2010 Nov 24. [DOI] [PubMed] [Google Scholar]
- 27.Soliman EZ, Prineas RJ, Go AS, et al. Chronic Renal Insufficiency Cohort (CRIC) Study Group. Chronic kidney disease and prevalent atrial fibrillation: the Chronic Renal Insufficiency Cohort (CRIC) Am Heart J. 2010 Jun;159(6):1102–1107. doi: 10.1016/j.ahj.2010.03.027. Erratum in: Am Heart J. 2010 Dec;160(6):1190; Am Heart J. 2011 Oct;162(4):794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marinigh R, Lane DA, Lip GY. Severe renal impairment and stroke prevention in atrial fibrillation: implications for thromboprophylaxis and bleeding risk. J Am Coll Cardiol. 2011 Mar 22;57(12):1339–1348. doi: 10.1016/j.jacc.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 29.Limdi NA, Limdi MA, Cavallari L, et al. Warfarin dosing in patients with impaired kidney function. Am J Kidney Dis. 2010 Nov;56(5):823–831. doi: 10.1053/j.ajkd.2010.05.023. Epub 2010 Aug 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boling PA. Care transitions and home health care. Clin Geriatr Med. 2009 Feb;25(1):135–148. doi: 10.1016/j.cger.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 31.Perry SJ, Wears RL, Patterson ES. Henriksen K, Battles JB, Keyes MA, et al, eds. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 3: Performance and Tools) Rockville, MD: Agency for Healthcare Research and Quality;; 2008. High-hanging fruit: improving transitions in health care performance and tools. In. [PubMed] [Google Scholar]
- 32.Voss R, Gardner R, Baier R, Butterfield K, Lehrman S, Gravenstein S. The care transitions intervention: translating from efficacy to effectiveness. Arch Intern Med. 2011 Jul 25;171(14):1232–1237. doi: 10.1001/archinternmed.2011.278. [DOI] [PubMed] [Google Scholar]
- 33.Baker WL, Cios DA, Sander SD, Coleman CI. Meta-analysis to assess the quality of warfarin control in atrial fibrillation patients in the United States. J Manag Care Pharm. 2009 Apr;15(3):244–252. doi: 10.18553/jmcp.2009.15.3.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.El Rouby S, Mestres CA, LaDuca FM, Zucker ML. Racial and ethnic differences in warfarin response. J Heart Valve Dis. 2004 Jan;13(1):15–21. [PubMed] [Google Scholar]
- 35.Reynolds MR, Lavelle T, Essebag V, Cohen DJ, Zimetbaum P. Influence of age, sex, and atrial fibrillation recurrence on quality of life outcomes in a population of patients with new-onset atrial fibrillation: the Fibrillation Registry Assessing Costs, Therapies, Adverse events and Lifestyle (FRACTAL) study. Am Heart J. 2006 Dec;152(6):1097–1103. doi: 10.1016/j.ahj.2006.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Walraven C, Jennings A, Oake N, Fergusson D, Forster AJ. Effect of study setting on anticoagulation control: a systematic review and metaregression. Chest. 2006 May;129(5):1155–1166. doi: 10.1378/chest.129.5.1155. [DOI] [PubMed] [Google Scholar]
- 37.Hohnloser SH, Connolly SJ. Atrial fibrillation, moderate chronic kidney disease, and stroke prevention: new anticoagulants, new hope. Eur Heart J. 2011 Oct;32(19):2347–2349. doi: 10.1093/eurheartj/ehr344. Epub 2011 Aug 28. [DOI] [PubMed] [Google Scholar]
- 38.Naccarelli GV, Johnston SS, Dalal M, Lin J, Patel PP. Rates and implications for hospitalization of patients ≥65 years of age with atrial fibrillation/flutter. Am J Cardiol. 2012 Feb 15;109(4):543–549. doi: 10.1016/j.amjcard.2011.10.009. Epub 2011 Nov 24. [DOI] [PubMed] [Google Scholar]
- 39.Balaban RB, Williams MV. Improving care transitions: hospitalists partnering with primary care. J Hosp Med. 2010 Sep;5(7):375–377. doi: 10.1002/jhm.824. [DOI] [PubMed] [Google Scholar]
- 40.Guthrie B, Saultz JW, Freeman GK, Haggerty JL. Continuity of care matters. BMJ. 2008 Aug 7;337:a867. doi: 10.1136/bmj.a867. [DOI] [PubMed] [Google Scholar]
- 41.Horwitz LI, Meredith T, Schuur JD, Shah NR, Kulkarni RG, Jenq GY. Dropping the baton: a qualitative analysis of failures during the transition from emergency department to inpatient care. Ann Emerg Med. 2009 Jun;53(6):701.e4–710.e4. doi: 10.1016/j.annemergmed.2008.05.007. Epub 2008 Jun 16. [DOI] [PubMed] [Google Scholar]
- 42.Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007 Sep;2(5):314–323. doi: 10.1002/jhm.228. [DOI] [PubMed] [Google Scholar]
- 43.Michaels AD, Spinler SA, Leeper B, et al. American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology, Council on Quality of Care and Outcomes Research; Council on Cardiopulmonary, Critical Care, Perioperative, and Resuscitation; Council on Cardiovascular Nursing; Stroke Council. Medication errors in acute cardiovascular and stroke patients: a scientific statement from the American Heart Association. Circulation. 2010 Apr 13;121(14):1664–1682. doi: 10.1161/CIR.0b013e3181d4b43e. Epub 2010 Mar 22. [DOI] [PubMed] [Google Scholar]
- 44.Dossett LA, Riesel JN, Griffin MR, Cotton BA. Prevalence and implications of preinjury warfarin use: an analysis of the National Trauma Databank. Arch Surg. 2011 May;146(5):565–570. doi: 10.1001/archsurg.2010.313. Epub 2011 Jan 17. [DOI] [PubMed] [Google Scholar]
- 45.Anthony CJ, Karim S, Ackroyd-Stolarz S, et al. Intensity of anticoagulation with warfarin and risk of adverse events in patients presenting to the emergency department. Ann Pharmacother. 2011 Jul;45((7-8)):881–887. doi: 10.1345/aph.1P670. Epub 2011 Jul 12. [DOI] [PubMed] [Google Scholar]
- 46.Shehab N, Sperling LS, Kegler SR, Budnitz DS. National estimates of emergency department visits for hemorrhage-related adverse events from clopidogrel plus aspirin and from warfarin. Arch Intern Med. 2010 Nov 22;170(21):1926–1933. doi: 10.1001/archinternmed.2010.407. [DOI] [PubMed] [Google Scholar]
- 47.Spahr JE, Maul JS, Rodgers GM. Superwarfarin poisoning: a report of two cases and review of the literature. Am J Hematol. 2007 Jul;82(7):656–660. doi: 10.1002/ajh.20784. [DOI] [PubMed] [Google Scholar]
- 48.van Ryn J, Stangier J, Haertter S, et al. Dabigatran etexilate—a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity. Thromb Haemost. 2010 Jun;103(6):1116–1127. doi: 10.1160/TH09-11-0758. Epub 2010 Mar 29. [DOI] [PubMed] [Google Scholar]
- 49.Crowther MA, Ageno W, Garcia D, et al. Oral vitamin K versus placebo to correct excessive anticoagulation in patients receiving warfarin: a randomized trial. Ann Intern Med. 2009 Mar 3;150(5):293–300. doi: 10.7326/0003-4819-150-5-200903030-00005. [DOI] [PubMed] [Google Scholar]
- 50.Hylek EM, Regan S, Go AS, Hughes RA, Singer DE, Skates SJ. Clinical predictors of prolonged delay in return of the international normalized ratio to within the therapeutic range after excessive anticoagulation with warfarin. Ann Intern Med. 2001 Sep 18;135(6):393–400. doi: 10.7326/0003-4819-135-6-200109180-00008. [DOI] [PubMed] [Google Scholar]
- 51.Crowther MA, Julian J, McCarty D, et al. Treatment of warfarin-associated coagulopathy with oral vitamin K: a randomised controlled trial. Lancet. 2000 Nov 4;356(9241):1551–1553. doi: 10.1016/S0140-6736(00)03125-1. [DOI] [PubMed] [Google Scholar]
- 52.Patel RJ, Witt DM, Saseen JJ, Tillman DJ, Wilkinson DS. Randomized, placebo-controlled trial of oral phytonadione for excessive anticoagulation. Pharmacotherapy. 2000 Oct;20(10):1159–1166. doi: 10.1592/phco.20.15.1159.34585. [DOI] [PubMed] [Google Scholar]
- 53.Holbrook A, Schulman S, Witt DM, et al. American College of Chest Physicians. Evidence-based management of anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141((2 Suppl)):e152S–e184S. doi: 10.1378/chest.11-2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gunther KE, Conway G, Leibach L, Crowther MA. Low-dose oral vitamin K is safe and effective for outpatient management of patients with an INR>10. Thromb Res. 2004;113((3-4)):205–209. doi: 10.1016/j.thromres.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 55.Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G. American College of Chest Physicians. Oral anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012 Feb;141((2 Suppl)):e44S–e88S. doi: 10.1378/chest.11-2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Watson HG, Baglin T, Laidlaw SL, Makris M, Preston FE. A comparison of the efficacy and rate of response to oral and intravenous Vitamin K in reversal of over-anticoagulation with warfarin. Br J Haematol. 2001 Oct;115(1):145–149. doi: 10.1046/j.1365-2141.2001.03070.x. [DOI] [PubMed] [Google Scholar]
- 57.Lubetsky A, Yonath H, Olchovsky D, Loebstein R, Halkin H, Ezra D. Comparison of oral vs intravenous phytonadione (vitamin K1) in patients with excessive anticoagulation: a prospective randomized controlled study. Arch Intern Med. 2003 Nov 10;163(20):2469–2473. doi: 10.1001/archinte.163.20.2469. [DOI] [PubMed] [Google Scholar]
- 58.Meehan R, Tavares M, Sweeney J. Clinical experience with oral versus intravenous vitamin K for warfarin reversal. Transfusion. 2013 Mar;53(3):491–498. doi: 10.1111/j.1537-2995.2012.03755.x. quiz 490. Epub 2012 Jun 28. [DOI] [PubMed] [Google Scholar]
- 59.Linkins LA, Choi PT, Douketis JD. Clinical impact of bleeding in patients taking oral anticoagulant therapy for venous thromboembolism: a meta-analysis. Ann Intern Med. 2003 Dec 2;139(11):893–900. doi: 10.7326/0003-4819-139-11-200312020-00007. [DOI] [PubMed] [Google Scholar]
- 60.Zhou W, Schwarting S, Illanes S, et al. Hemostatic therapy in experimental intracerebral hemorrhage associated with the direct thrombin inhibitor dabigatran. Stroke. 2011 Dec;42(12):3594–3599. doi: 10.1161/STROKEAHA.111.624650. Epub 2011 Oct 13. [DOI] [PubMed] [Google Scholar]
- 61.Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation. 2011 Oct 4;124(14):1573–1579. doi: 10.1161/CIRCULATIONAHA.111.029017. Epub 2011 Sep 6. [DOI] [PubMed] [Google Scholar]
- 62.Pradaxa (dabigatran etexilate) [package insert. 2012 http://bidocs.boehringer-ingelheim.com/BIWebAccess/ViewServlet.ser?docBase=renetnt&folderPath=/Prescribing%20Information/PIs/Pradaxa/Pradaxa.pdf. Accessed September 6. [Google Scholar]
- 63.Levy JH, Tanaka KA. Prohemostatic agents to prevent perioperative blood loss. Semin Thromb Hemost. 2008 Jul;34(5):439–444. doi: 10.1055/s-0028-1092873. Epub 2008 Oct 27. [DOI] [PubMed] [Google Scholar]
- 64.Garcia DA, Lopes RD, Hylek EM. New-onset atrial fibrillation and warfarin initiation: high risk periods and implications for new antithrombotic drugs. Thromb Haemost. 2010 Dec;104(6):1099–1105. doi: 10.1160/TH10-07-0491. Epub 2010 Sep 30. [DOI] [PubMed] [Google Scholar]
- 65.Nutescu E, Chuatrisorn I, Hellenbart E. Drug and dietary interactions of warfarin and novel oral anticoagulants: an update. J Thromb Thrombolysis. 2011 Apr;31(3):326–343. doi: 10.1007/s11239-011-0561-1. [DOI] [PubMed] [Google Scholar]
- 66.Kaatz S, Paje D. Update in bridging anticoagulation. J Thromb Thrombolysis. 2011 Apr;31(3):259–264. doi: 10.1007/s11239-011-0571-z. [DOI] [PubMed] [Google Scholar]
- 67.Cibulskis CC, Giardino AP, Moyer VA. Care transitions from inpatient to outpatient settings: ongoing challenges and emerging best practices. Hosp Pract (1995) 2011 Aug;39(3):128–139. doi: 10.3810/hp.2011.08.588. [DOI] [PubMed] [Google Scholar]
- 68.Matchar DB, Jacobson A, Dolor R, et al. THINRS Executive Committee and Site Investigators. Effect of home testing of international normalized ratio on clinical events. N Engl J Med. 2010 Oct 21;363(17):1608–1620. doi: 10.1056/NEJMoa1002617. Erratum in: N Engl J Med. 2011 Jan 6;364(1):93. [DOI] [PubMed] [Google Scholar]
- 69.Bushnell CD, Zimmer LO, Pan W, et al. Adherence Evaluation After Ischemic Stroke–Longitudinal Investigators. Persistence with stroke prevention medications 3 months after hospitalization. Arch Neurol. 2010 Dec;67(12):1456–1463. doi: 10.1001/archneurol.2010.190. Epub 2010 Aug 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005 Aug 4;353(5):487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 71.Terrell KM, Miller DK. Strategies to improve care transitions between nursing homes and emergency departments. J Am Med Dir Assoc. 2011 Oct;12(8):602–605. doi: 10.1016/j.jamda.2010.09.007. Epub 2010 Nov 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sellers MB, Newby LK. Atrial fibrillation, anticoagulation, fall risk, and outcomes in elderly patients. Am Heart J. 2011 Feb;161(2):241–246. doi: 10.1016/j.ahj.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 73.Gage BF, Birman-Deych E, Kerzner R, Radford MJ, Nilasena DS, Rich MW. Incidence of intracranial hemorrhage in patients with atrial fibrillation who are prone to fall. Am J Med. 2005 Jun;118(6):612–617. doi: 10.1016/j.amjmed.2005.02.022. [DOI] [PubMed] [Google Scholar]
- 74.Coyne KS, Paramore C, Grandy S, Mercader M, Reynolds M, Zimetbaum P. Assessing the direct costs of treating nonvalvular atrial fibrillation in the United States. Value Health. 2006 Sep-Oct;9(5):348–356. doi: 10.1111/j.1524-4733.2006.00124.x. [DOI] [PubMed] [Google Scholar]
- 75.Woods DM, Holl JL, Angst D, et al. Henriksen K, Battles JB, Keyes MA, et al, eds. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 3: Performance and Tools) Rockville, MD: Agency for Healthcare Research and Quality;; 2008. Improving clinical communication and patient safety: clinician-recommended solutions. In. [PubMed] [Google Scholar]
- 76.Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011 Aug 24;306(8):840–847. doi: 10.1001/jama.2011.1206. [DOI] [PubMed] [Google Scholar]
- 77.Granger CB, Alexander JH, McMurray JJ, et al. ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011 Sep 15;365(11):981–992. doi: 10.1056/NEJMoa1107039. Epub 2011 Aug 27. [DOI] [PubMed] [Google Scholar]


