Abstract
Objective:
The presence of cranial autonomic symptoms often leads to a misdiagnosis of “sinus headache” in adult migraineurs, leading to unnecessary treatments and delaying appropriate migraine therapy. In this study, we examined the frequency of cranial autonomic symptoms in pediatric/adolescent patients with migraine.
Methods:
This cross-sectional study included all pediatric and adolescent patients with migraine evaluated by a single investigator at 4 different sites over the course of the study period.
Results:
Of 125 pediatric migraineurs, 62% had at least one cranial autonomic symptom based on current International Classification of Headache Disorders, second edition (ICHD-II) criteria, and 70% based on proposed ICHD-III criteria. The majority had more than one cranial autonomic symptom and the symptoms tended to be bilateral. Age, sex, laterality of headache, presence of aura, and whether migraine was episodic vs chronic did not influence the likelihood of having cranial autonomic symptoms.
Conclusions:
In pediatric/adolescent migraine, the presence of cranial autonomic symptoms appears to be the rule rather than the exception. Clinicians should be careful to consider migraine when evaluating a child with headache and associated ocular or nasal symptoms so as to avoid giving a misdiagnosis of sinus headache.
Cranial autonomic symptoms are typically associated with the trigeminal autonomic cephalalgias, such as cluster headache.1 The anatomy and physiology of these symptoms, consisting of the trigeminal-autonomic reflex, have been described and are well understood.2 However, it is only recently that the implications of the data have been more broadly realized with the relatively high frequency, between 27% and 73%, of cranial autonomic symptoms in adult migraineurs.3–6
Recognizing that cranial autonomic symptoms are a common component of migraine is important diagnostically and thus therapeutically. Sinusitis, which also may present with head pain, is one of the most common misdiagnoses given to migraineurs.7–10 In a pediatric study, nearly 40% of pediatric migraineurs were initially mislabeled as having “sinus headache.”11 Misdiagnosis puts these patients at risk of inappropriate treatments and procedures, and delays appropriate treatment of their migraine. In this study, we examined the frequency of cranial autonomic symptoms in pediatric patients with migraine presenting for care.
The International Classification of Headache Disorders, second edition (ICHD-II)12 includes the following cranial autonomic symptoms: 1) conjunctival injection, lacrimation, or both; 2) nasal congestion, rhinorrhea, or both; 3) eyelid edema; 4) forehead and facial sweating; 5) forehead/facial flushing; and 6) miosis, ptosis, or both. In ICHD-III, a sense of aural fullness13 will be added as a cranial autonomic symptom.14
METHODS
Standard protocol approvals, registrations, and patient consents.
This study was approved by the University of California, San Francisco (UCSF) Committee for Human Research (protocol number 11-06840) under a minimal risk protocol.
Study design and study population.
We did a cross-sectional phenotyping of pediatric patients with migraine seen in 4 clinical settings during the study period (July 1, 2010 to June 30, 2012). All pediatric patients with migraine who were seen by one of us (A.A.G.) were included in this analysis.
Inclusion criteria were 1) age younger than 18 years; 2) diagnosis of migraine with or without aura by ICHD-II criteria for children12; and 3) history regarding cranial autonomic symptoms obtained by A.A.G. at the clinical visit. Episodic migraine (<15 migraine days per month) and chronic migraine (≥15 migraine days per month for ≥3 months) were defined by ICHD-II criteria for children, except medication overuse could be present in chronic migraine. Exclusion criteria were 1) age 18 years or older at initial evaluation, and 2) diagnosis that was not migraine.
There were 4 sites where patients were evaluated: 1) a general child neurology clinic at a local county hospital (San Francisco General Hospital); 2) a general child neurology clinic at a tertiary care facility (UCSF); 3) the inpatient pediatric ward or emergency department at a tertiary care facility (UCSF Benioff Children's Hospital); and 4) a subspecialty headache clinic associated with a tertiary care facility (UCSF Headache Clinic).
Determination of cranial autonomic symptoms.
Pediatric patients were interviewed with at least one parent present. They were explicitly asked whether they ever experience each of the following symptoms with their headaches: 1) conjunctival injection, 2) lacrimation (apart from crying), 3) sense of grittiness or scratchiness in the eye,15 4) nasal congestion, 5) rhinorrhea, 6) eyelid edema, 7) ptosis, 8) sense of ear fullness or pressure, and 9) facial sweating or flushing. Miosis was not explicitly asked about as ptosis was thought to be more easily noticed. Although a sense of grittiness or scratchiness in the eye is not included in the proposed definitions for cranial autonomic symptoms in ICHD-III, it was included here based on the opinion of the senior author that this symptom constitutes a cranial autonomic symptom.
If a symptom was noted by the patient or their parent(s) to be present, they were then asked whether the symptom occurred on 1) one side, 2) both sides, or whether it was 3) sometimes unilateral and sometimes bilateral. Whether it was the patient, the parent, or both who confirmed each symptom was not recorded. The frequency with which the patient experienced the symptom was also not recorded.
Data analysis.
All analyses were performed using Stata 12 (StataCorp, College Station, TX). The χ2, Fisher exact, and Student t tests were used as appropriate. Odds ratios (ORs) were calculated to determine whether any combination of 2 cranial autonomic symptoms seemed to occur more frequently than would be expected by chance.
RESULTS
One hundred thirty-three pediatric/adolescent patients with migraine received initial headache evaluations during the study period. Eight were excluded because of missing data on the presence or absence of cranial autonomic symptoms. The remaining 125 patients constituted the study population. Demographic variables and clinical characteristics are shown in table 1.
Table 1.
Demographic and clinical characteristics (n = 125)a
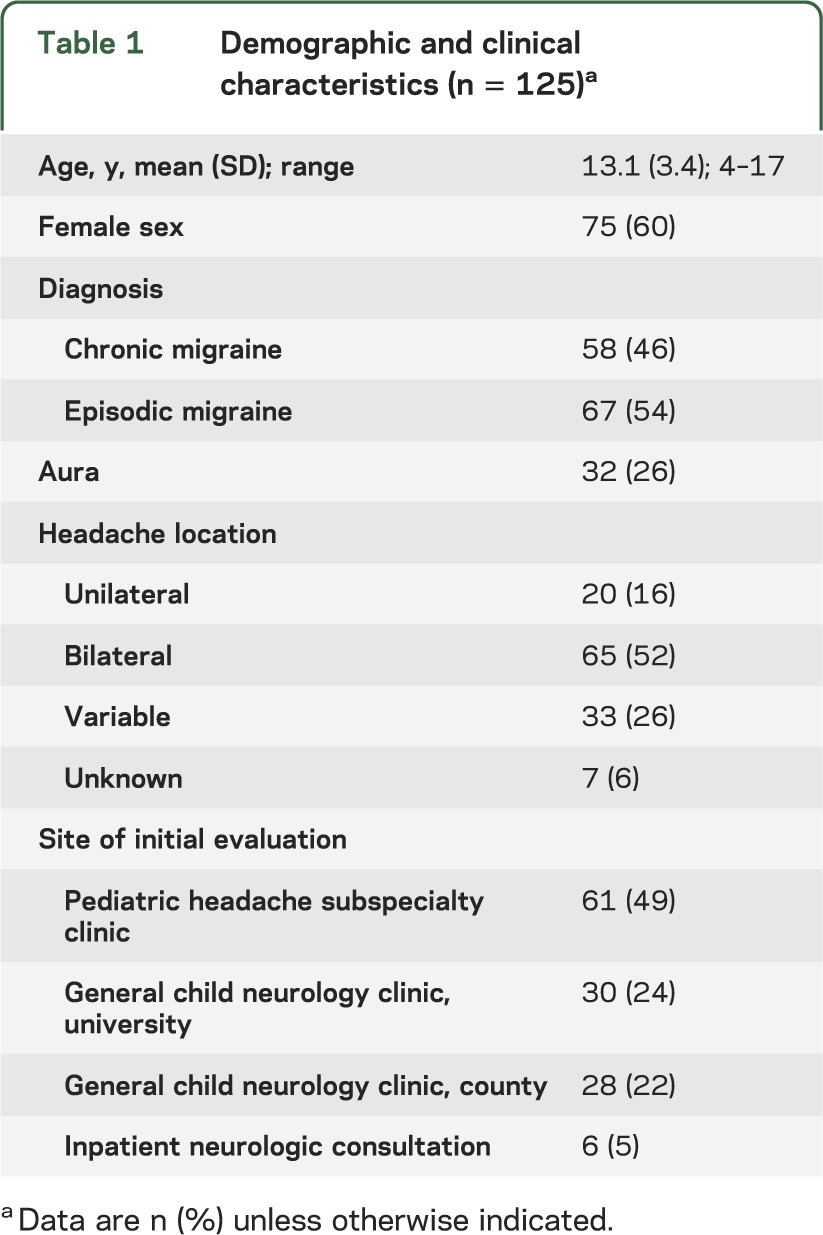
Whereas a minority of children experienced strictly unilateral migraine headache (n = 20, 16%), a more substantial group experienced unilateral headache at least some of the time (n = 33, 26%), for a total of 53 (42%) who always or sometimes had unilateral headache. Patients with persistent unilateral headache and cranial autonomic symptoms always had the diagnosis of hemicrania continua considered and excluded in order to be included in this analysis.
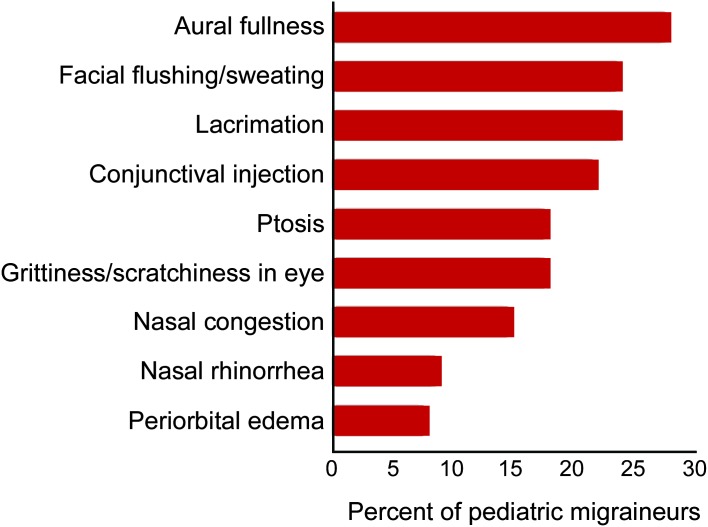
When all 9 cranial autonomic symptoms were included, 73% (n = 91) of pediatric migraineurs had at least one cranial autonomic symptom. The figure shows the prevalence of each cranial autonomic symptom.
Figure. Frequency of individual cranial autonomic symptoms.
When a sense of grit was removed from the analysis, 70% (n = 87) had at least one cranial autonomic symptom. When a sense of aural fullness was also removed, reflecting current ICHD-II criteria, 62% (n = 77) had at least one cranial autonomic symptom.
Because the upcoming ICHD-III criteria will include a sense of aural fullness as a cranial autonomic symptom, but not a sense of grit, all further analyses discussed below were performed using that group, i.e., sense of aural fullness included, sense of grit excluded.
Of these 87 patients, the majority experienced multiple cranial autonomic symptoms (n = 49, 56%). Forty-four percent (n = 38) had one cranial autonomic symptom, 28% (n = 24) had 2, 14% (n = 12) had 3, 6% (n = 5) had 4, 8% (n = 7) had 5, and 1% (n = 1) had 7.
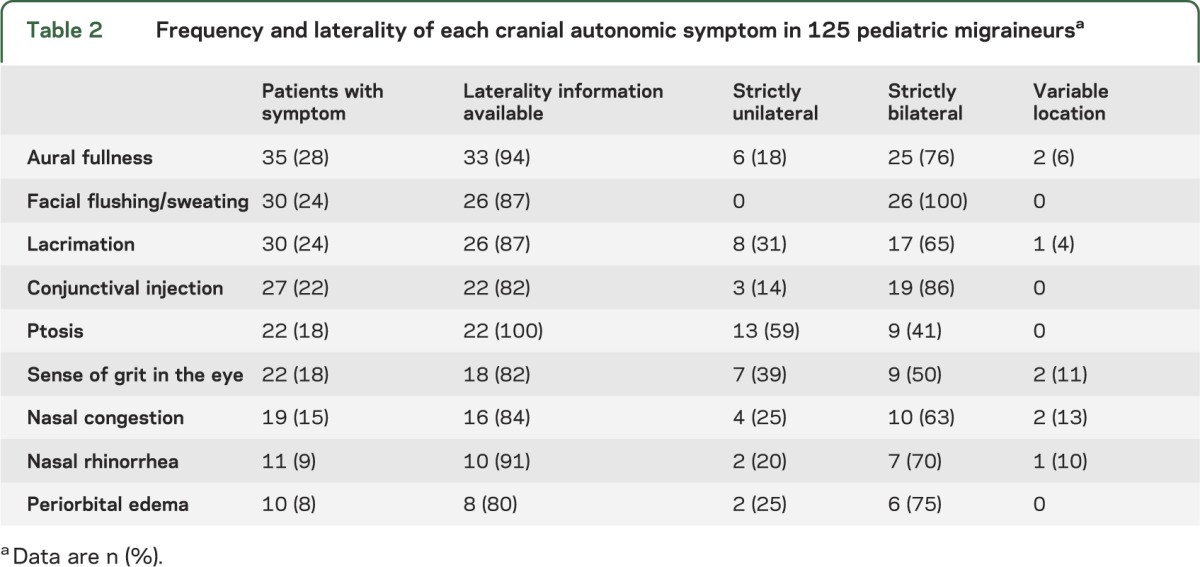
Of the 184 cranial autonomic symptoms experienced by these 87 patients, information on laterality was available for 163 of the symptoms. Twenty-three percent (n = 38) were unilateral, 73% (n = 119) bilateral, and 4% (n = 6) varied between unilateral and bilateral. Further information on the laterality of each symptom is available in table 2.
Table 2.
Frequency and laterality of each cranial autonomic symptom in 125 pediatric migraineursa
Female sex, presence of aura, and having been evaluated at the headache subspecialty clinic did not increase the likelihood of having cranial autonomic symptoms. Age, treated both as a continuous variable and as a dichotomous variable (younger than 12 years vs 12–17 years), had no effect on the likelihood of having cranial autonomic symptoms (see table e-1 on the Neurology® Web site at www.neurology.org). Those with chronic migraine were not more likely than those with episodic migraine to have cranial autonomic symptoms (74% vs 66%, p = 0.31).
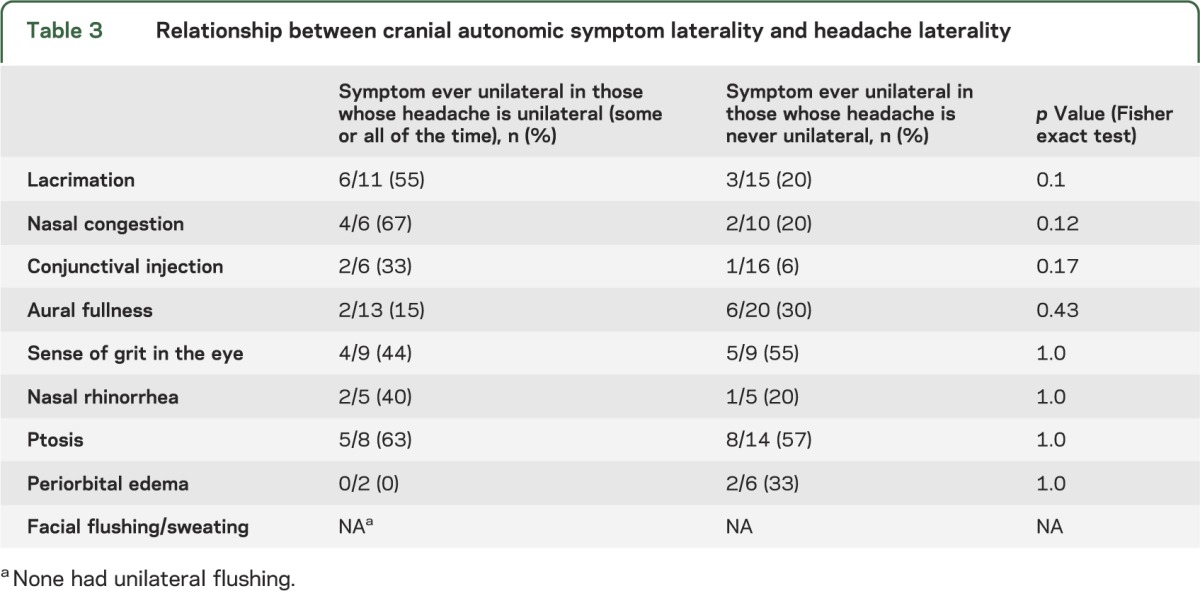
Similarly, a tendency to have unilateral headache, i.e., having headache that is sometimes or always unilateral, was not associated with increased likelihood of having cranial autonomic symptoms. The individual cranial autonomic symptoms were not more likely to be unilateral in those who had unilateral headache; however, the numbers in these analyses were quite small (table 3).
Table 3.
Relationship between cranial autonomic symptom laterality and headache laterality
Several cranial autonomic symptoms seemed more likely to co-occur (see table e-2). The OR of periorbital edema co-occurring with conjunctival injection was 6.5 (95% confidence interval [CI] 1.4–33.5), with a sense of aural fullness 7.7 (95% CI 1.6–48.5), and with facial flushing 16.4 (95% CI 2.9–163.5). The OR for ptosis and lacrimation co-occurring was 4.4 (95% CI 1.5–13), and for nasal congestion and rhinorrhea was 16.2 (95% CI 3.4–84.7).
DISCUSSION
The data show that approximately two-thirds of patients in pediatric/adolescent neurology or specialty headache practice with migraine have accompanying cranial autonomic symptoms. Given the frequent misdiagnosis of these symptoms in adults,7–10 there is a very considerable possibility of similar widespread misdiagnosis in children. In fact, in a pediatric study, nearly 40% of migraineurs were initially misdiagnosed as having sinus headache.11
Cranial autonomic symptoms arise from activation of the trigeminal-autonomic reflex, wherein nociceptive trigeminal afferents activate parasympathetic efferents carried by the seventh and eighth cranial nerves to target the lacrimal glands, nasal mucosa, and other areas.2 Knowledge of the anatomy and physiology of the trigeminal-autonomic reflex offers clinicians insight into the clinical phenomenon of cranial autonomic symptoms and a simple, yet powerful tool with which to diagnose patients accurately. In fact, it may be that eye-related cranial autonomic symptoms are more likely to co-occur and nose-related cranial autonomic symptoms are more likely to co-occur than eye symptoms are to co-occur with nose symptoms. This would make sense neuroanatomically based on the V1 afferent involvement of eye-related symptoms and the V2 afferent involvement of nose-related symptoms.16 Closer study of this issue is warranted.
Our study specifically targeted cranial autonomic symptoms in pediatric/adolescent migraineurs. Using current ICHD-II criteria for cranial autonomic symptoms, as they are explained in section 3 of the document, 62% of pediatric migraineurs had at least one cranial autonomic symptom. What is considered a cranial autonomic symptom is evolving. A sense of aural fullness will be added to the list of cranial autonomic symptoms in ICHD-III.14 Including aural fullness in this analysis, the prevalence of cranial autonomic symptoms in pediatric migraineurs was 70%, and interestingly, it was the most common symptom. These figures are comparable to some studies in adults; for example, in one study, 73.1% of adult migraineurs had cranial autonomic symptoms.4 Of note, in one study, 75% of adults migraineurs labeled as having sinus headache experienced cranial autonomic symptoms.7 Moreover, in adult practice, such patients respond to treatment with sumatriptan.17,18
Given that sensory sensitivity symptoms, such as photophobia and phonophobia, are more often bilateral in migraineurs and unilateral in trigeminal autonomic cephalalgias,19 it might be expected that cranial autonomic symptoms would also more likely be bilateral in migraineurs. Indeed, the majority of adult migraineurs experience bilateral cranial autonomic symptoms, in contrast to patients with trigeminal autonomic cephalalgias who more often experience these symptoms unilaterally.6 In this pediatric study, the majority of pediatric cranial autonomic symptoms were also bilateral. In an adult study, strictly unilateral cranial autonomic symptoms were present in only 32% of adult migraineurs.4 Similarly, in this pediatric study, only 23% of the cranial autonomic symptoms were strictly unilateral. This tendency for bilaterality may explain why studies that examined only for unilateral cranial autonomic symptoms in adult migraineurs reported a lower prevalence of cranial autonomic symptoms (26.9%–45.8%3,5).
The majority of affected patients in this study had more than one cranial autonomic symptom. Similarly, in adult studies, the majority of migraineurs with cranial autonomic symptoms express more than one symptom.3–5 Age, sex, presence of aura, and having episodic vs chronic migraine did not predict likelihood of having cranial autonomic symptoms in this study. This is similar to adult studies wherein these variables were also not predictive.4–6 Evaluation at the subspecialty headache clinic was also not predictive of having cranial autonomic symptoms in our study. In a population-based study of adults,3 the prevalence of cranial autonomic symptoms reported was lower than in studies done in headache clinic populations4,5; however, this population-based study was limited in that only unilateral cranial autonomic symptoms were studied.
It is not surprising that a tendency for unilateral headache did not predict likelihood of having cranial autonomic symptoms in this pediatric study. In children, migraine headache is usually bilateral with the unilateral pattern more typical of adults emerging only in late adolescence or early adulthood.12 Furthermore, even in adults, the association between unilateral migraine pain and cranial autonomic symptoms is inconsistent.3–6
One limitation of this study is that because trigeminal autonomic cephalalgias, such as cluster headache, paroxysmal hemicrania, and hemicrania continua, are rare in children,20,21 at this point, we were not able to make any comparisons between the frequency and characteristics of cranial autonomic symptoms in children with trigeminal autonomic cephalalgias vs migraine.
Although the compilation of our data was done after the fact, it has been our practice over many years to systematically seek cranial autonomic symptoms at the initial visit, so the clinical phenotyping was done prospectively. The data provide a glimpse of the frequency of cranial autonomic symptoms in pediatric/adolescent migraineurs in a range of settings. The findings are in line with previous studies in adults. It is important for pediatricians and child neurologists to be aware of the common nature of cranial autonomic symptoms in children with migraine to prevent misdiagnosis. “Sinus headache” is a common misdiagnosis given to both adult and pediatric migraineurs.7–9,11,22 It has been theorized that this may be attributable to the tendency of both physicians and patients to associate ocular and nasal symptoms with sinusitis rather than with migraine,23 together with a lack of awareness of the relevant anatomy and physiology. Misdiagnosing pediatric patients with migraine as having sinus headaches could lead to inappropriate and unnecessary treatments as well as delay in appropriate migraine therapy. In one adult study, 35% of the migraineurs had undergone previous sinus surgery, an example of the potential serious consequences of misdiagnosis.7
In caring for young children with migraine, we must also be cognizant of the potential need to infer some of these symptoms from behavior, much as we infer photophobia and phonophobia from behavior in young children. For example, a young child who is pulling on an ear during a migraine could be experiencing a sense of aural fullness. A greater awareness of the anatomy and physiology of the trigeminal-autonomic reflex, and its potential for activation in any trigeminal pain state, may save many children much suffering and numerous parents much angst.
Supplementary Material
GLOSSARY
- CI
confidence interval
- ICHD
International Classification of Headache Disorders
- OR
odds ratio
- UCSF
University of California, San Francisco
Footnotes
Supplemental data at www.neurology.org
AUTHOR CONTRIBUTIONS
Amy A. Gelfand designed and conceptualized the study, analyzed and interpreted the data, and wrote the first draft of the manuscript and revised subsequent drafts. Amanda C. Reider abstracted the data, assisted with interpreting the data, and revised the manuscript for meaningful intellectual content. Peter J. Goadsby contributed to the design and conceptualization of the study, assisted with interpreting the data, and revised the manuscript for meaningful intellectual content.
STUDY FUNDING
No targeted funding reported.
DISCLOSURE
A. Gelfand receives grant support from NIH/NINDS (K12NS001692) and the UCSF Center for Translational Science Institute. She has received honoraria from Journal Watch Neurology and personal compensation for legal consulting. A. Reider reports no disclosures. P. Goadsby is on the boards of Allergan, CoLucid, MAP Pharmaceuticals, Merck, Sharpe and Dohme, eNeura, Neuroaxon, Autonomic Technologies Inc., Boston Scientific, Eli-Lilly, Medtronic, Linde Gases, Arteaus, AlderBio, and Bristol-Myers Squibb. He has consulted for gammaCore, Pfizer, Nevro Corp., Lundbeck, Zogenix, Impax, and Dr. Reddy’s, and has been compensated for expert legal testimony. He has grant support from GlaxoSmithKline, MAP, MSD, eNeura, and Amgen. He has received honoraria for speaking from MSD, Pfizer, Allergan, and Menarini, and payment for editorial work from Journal Watch Neurology and for developing educational materials for the American Headache Society. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Goadsby PJ, Lipton RB. A review of paroxysmal hemicranias, SUNCT syndrome and other short-lasting headaches with autonomic feature, including new cases. Brain 1997;120(pt 1):193–209 [DOI] [PubMed] [Google Scholar]
- 2.May A, Goadsby PJ. The trigeminovascular system in humans: pathophysiologic implications for primary headache syndromes of the neural influences on the cerebral circulation. J Cereb Blood Flow Metab 1999;19:115–127 [DOI] [PubMed] [Google Scholar]
- 3.Obermann M, Yoon MS, Dommes P, et al. Prevalence of trigeminal autonomic symptoms in migraine: a population-based study. Cephalalgia 2007;27:504–509 [DOI] [PubMed] [Google Scholar]
- 4.Gupta R, Bhatia MS. A report of cranial autonomic symptoms in migraineurs. Cephalalgia 2007;27:22–28 [DOI] [PubMed] [Google Scholar]
- 5.Barbanti P, Fabbrini G, Pesare M, Vanacore N, Cerbo R. Unilateral cranial autonomic symptoms in migraine. Cephalalgia 2002;22:256–259 [DOI] [PubMed] [Google Scholar]
- 6.Lai TH, Fuh JL, Wang SJ. Cranial autonomic symptoms in migraine: characteristics and comparison with cluster headache. J Neurol Neurosurg Psychiatry 2009;80:1116–1119 [DOI] [PubMed] [Google Scholar]
- 7.Eross E, Dodick D, Eross M. The Sinus, Allergy and Migraine Study (SAMS). Headache 2007;47:213–224 [DOI] [PubMed] [Google Scholar]
- 8.Lipton RB, Diamond S, Reed M, Diamond ML, Stewart WF. Migraine diagnosis and treatment: results from the American Migraine Study II. Headache 2001;41:638–645 [DOI] [PubMed] [Google Scholar]
- 9.Schreiber CP, Hutchinson S, Webster CJ, Ames M, Richardson MS, Powers C. Prevalence of migraine in patients with a history of self-reported or physician-diagnosed “sinus” headache. Arch Intern Med 2004;164:1769–1772 [DOI] [PubMed] [Google Scholar]
- 10.Cady R, Schreiber CP, Billings C. Subjects with self-described “sinus” headache meet IHS diagnostic criteria for migraine. Cephalalgia 2001;21:291 [Google Scholar]
- 11.Senbil N, Gurer YK, Uner C, Barut Y. Sinusitis in children and adolescents with chronic or recurrent headache: a case-control study. J Headache Pain 2008;9:33–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Headache Classification Subcommittee of the International Headache Society The International Classification of Headache Disorders: 2nd edition. Cephalalgia 2004;24(suppl 1):9–160 [DOI] [PubMed] [Google Scholar]
- 13.Boes CJ, Swanson JW, Dodick DW. Chronic paroxysmal hemicrania presenting as otalgia with a sensation of external acoustic meatus obstruction: two cases and a pathophysiologic hypothesis. Headache 1998;38:787–791 [DOI] [PubMed] [Google Scholar]
- 14.International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33:629–808 [DOI] [PubMed] [Google Scholar]
- 15.Newman LC, Lipton RB, Solomon S. Hemicrania continua: ten new cases and a review of the literature. Neurology 1994;44:2111–2114 [DOI] [PubMed] [Google Scholar]
- 16.May A, Buchel C, Turner R, Goadsby PJ. Magnetic resonance angiography in facial and other pain: neurovascular mechanisms of trigeminal sensation. J Cereb Blood Flow Metab 2001;21:1171–1176 [DOI] [PubMed] [Google Scholar]
- 17.Ishkanian G, Blumenthal H, Webster CJ, Richardson MS, Ames M. Efficacy of sumatriptan tablets in migraineurs self-described or physician-diagnosed as having sinus headache: a randomized, double-blind, placebo-controlled study. Clin Ther 2007;29:99–109 [DOI] [PubMed] [Google Scholar]
- 18.Schreiber C, Cady R, Billings C. Oral sumatriptan for self-described “sinus” headache. Cephalalgia 2001;21:291 [Google Scholar]
- 19.Irimia P, Cittadini E, Paemeleire K, Cohen AS, Goadsby PJ. Unilateral photophobia or phonophobia in migraine compared with trigeminal autonomic cephalalgias. Cephalalgia 2008;28:626–630 [DOI] [PubMed] [Google Scholar]
- 20.Tarantino S, Vollono C, Capuano A, Vigevano F, Valeriani M. Chronic paroxysmal hemicrania in paediatric age: report of two cases. J Headache Pain 2011;12:263–267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Antonaci F, Alfei E, Piazza F, De Cillis I, Balottin U. Therapy-resistant cluster headache in childhood: case report and literature review. Cephalalgia 2010;30:233–238 [DOI] [PubMed] [Google Scholar]
- 22.Diamond ML. The role of concomitant headache types and non-headache co-morbidities in the underdiagnosis of migraine. Neurology 2002;58:S3–S9 [DOI] [PubMed] [Google Scholar]
- 23.Cady RK, Schreiber CP. Sinus headache: a clinical conundrum. Otolaryngol Clin North Am 2004;37:267–288 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.