Abstract
Background
One-half of Americans currently meet guideline physical activity levels. For these individuals, exceeding guideline levels may provide additional health benefits.
Methods
Incident physician-diagnosed myocardial infarction and angina, revascularization procedures (CABG, PTCA), and ischemic heart disease deaths during 7.7-year follow-up were compared to baseline usual distance run in 35,402 male runners.
Results
Men reported 467 incident CHD and the National Death Index identified an additional 54 ischemic heart disease deaths. Per km/day run, the men’s risks declined 5% for fatal and nonfatal CHD (P = 0.001), nonfatal CHD (P = 0.0008), and revascularization procedures (P = 0.002). Their risks for nonfatal myocardial infarctions and angina declined 7% (P = 0.02) and 10% (P = 0.003), respectively. Compared to <3 km/day run (upper limit guideline level), >9 km/day run produced risks 65% lower for angina (P = 0.008), 29% lower for nonfatal CHD (P = 0.04), and 26% lower for fatal and nonfatal CHD (P = 0.06).
Conclusions
Exceeding guideline physical activity levels produce important CHD-risk reductions.
Keywords: Epidemiology, physical activity, prevention, cardiovascular disease
Recent guidelines from the American Heart Association and the American College of Sports Medicine state “all healthy adults aged 18–65 years need moderate-intensity aerobic (endurance) physical activity for a minimum of 30 min on five days each week or vigorous-intensity aerobic physical activity for a minimum of 20 min on three days each week.” [1] Moderately intense activities are those that expend three- to six-fold the energy expenditure of sitting at rest (e.g., brisk walking) and vigorously intense activities are those that expend greater energy (e.g., running) [1,2]. The geographically, occupationally, and institutionally based cohorts upon which the guidelines are primarily based include relatively few vigorously active individuals, and relatively few high-volume exercisers. For this reason, the guidelines provide little specific information on the health benefits of higher doses of more vigorous physical activity [1]. This paper specifically describes the reduction in CHD risk associated with exercise doses that exceed current guideline levels using prospective follow-up data from the National Runners’ Health Study.
Methods
The National Runners’ Health Study cohort was recruited between 1991 and 1993 [3–14]. Baseline running distances were reported in usual miles run per week, which correlates strongly between repeated questionnaires (r = 0.89), and has been shown to be significantly associated with biomarkers traditionally associated with physical activity [3]. The University of California Berkeley Committee for the Protection of Human Subjects approved the study protocol and all participants provided written informed consent.
Follow-up questionnaires were mailed between 1998 and 2001. Participants reported whether they had percutaneous transluminal coronary angioplasty (PTCA) or coronary artery bypass graph (CABG), and if they had been diagnosed as having had a heart attack or angina by a physician since baseline, and the year of the procedure or diagnosis. Nonfatal CHD was defined as the earliest myocardial infarction, CABG, PTCA, or angina diagnosis. Fatal CHD was defined as an ICD-9 diagnosis of 410–414 and 429.2, or an ICD-10 diagnosis of I20–I25. The endpoint “all fatal and nonfatal CHD” includes both fatal and nonfatal CHD as described above. Cox-proportional hazard model was used with daily intakes of alcohol, meat, fish, fruit, and aspirin, pack-years of prior cigarette use, and years of education, along with age (age and age2) as covariates. We also examined the effects of adjusting for the participant’s recalled weight when they began running 12 or more km/week (BMIpre-exercise) to assess the possible effects of self- selection, and their baseline BMI (BMIbaseline) to assess whether BMI may mediate the relationship between running and CHD. The analyses of nonfatal events include only those participants with follow-up questionnaires. The analyses of all fatal and nonfatal CHD included those identified as having died from CHD while assuming all persons lost to follow-up were free of CHD at the end of follow-up (a conservative assumption).
Results
There were 36,537 men who had complete data on age, education, diet, aspirin use, BMI, smoking history, and running distance, of whom we excluded 527 for baseline cigarette use, 214 for baseline diabetes, and 394 for pre-existing heart disease. Of these, follow-up questionnaires were obtained for 28,462 men (80.2%), and causes of death were obtained from the National Death Index on 507 men (429 with complete baseline data who were non-smokers, non-diabetic, and without pre-existing heart disease at baseline). Men reported physician diagnoses of 155 incident myocardial infarctions, 395 revascularization procedures, and 102 incident angina. The National Death Index search identified 72 male deaths due to ischemic heart disease. Women were excluded from these analyses because only 30 reported physician diagnosis of CHD or incident anginas or died from ischemic heart disease. The women’s low incidence rate is partly due to their young age (averaging 6 years younger than the men at baseline) and the well-established sex differences in CHD risk. The baseline characteristics of this cohort are described elsewhere [4]. There was no significant interaction between reported distance run per day and loss to follow-up status for education (P = 0.13), BMI (P = 0.12), years run (P = 0.08), pack-years of cigarette use (P = 0.06) or reported intakes of meat (P = 0.15), fruit (P = 0.45) or alcohol (P = 0.34).
Table 1 presents the relative risks for CHD per km/day run. Each km/day increment in running distance was associated with a 5% risk reduction for nonfatal CHD, a 7% risk reduction for nonfatal myocardial infarction, a 5% risk reduction for revascularization procedures, and a 10% risk reduction for angina. Including ischemic heart disease deaths and presuming that those lost to follow-up were CHD-free (a conservative assumption since some of those would have had incident CHD) did not alter the risk reduction. Adjustment for men’s pre-exercise BMI had little effect on the risk reductions, i.e., the risk reductions are not due to low-risk lean men self-selecting to run longer distances. However, adjustment for baseline BMI diminished the risk reductions sufficiently to eliminate their statistical significance for all endpoints except angina, i.e., suggesting baseline BMI may mediate, in part, the CHD-risk reduction associated with physical activity.
Table 1.
Relative risk for CHD and angina by baseline running distance (km/day) from Cox-proportional hazard analyses.
| Relative risk, per km/day (95% confidence interval) and statistical significance | |||
|---|---|---|---|
| No adjustment for or BMIbaseline BMIpre-exercise | Adjusted for BMIpre-exercise | Adjusted for BMIbaseline | |
| Fatal & nonfatal CHD | 0.95 (0.92, 0.98) P=0.001 |
0.95 (0.92, 0.98) P=0.002 |
0.98 (0.94, 1.01) P=0.13 |
| Nonfatal CHD | 0.95 (0.92, 0.98) P=0.0008 |
0.95 (0.92, 0.98) P=0.001 |
0.98 (0.94, 1.01) P=0.15 |
| Nonfatal Myocardial infarction | 0.93 (0.88, 0.99) P=0.02 |
0.94 (0.89, 1.00) P=0.05 |
0.97 (0.91, 1.03) P=0.34 |
| Revascularization procedures | 0.95 (0.91, 0.98) P=0.002 |
0.95 (0.91, 0.98) P=0.003 |
0.97 (0.94, 1.01) P=0.17 |
| Angina | 0.90 (0.83, 0.97) P=0.005 |
0.91 (0.84, 0.98) P=0.01 |
0.92 (0.85, 0.99) P=0.04 |
Adjusted for age (age, age2), education, aspirin use, pack-years of past cigarette use, and intakes of meat, fruit, and alcohol. Additional adjustment for BMI when first began running 12 or more km/week (BMIpre-exercise) or BMI at baseline (BMIbaseline) where indicated. Sample sizes are 35,402 men for fatal and nonfatal endpoints combined, and 28,287 men for nonfatal endpoints.
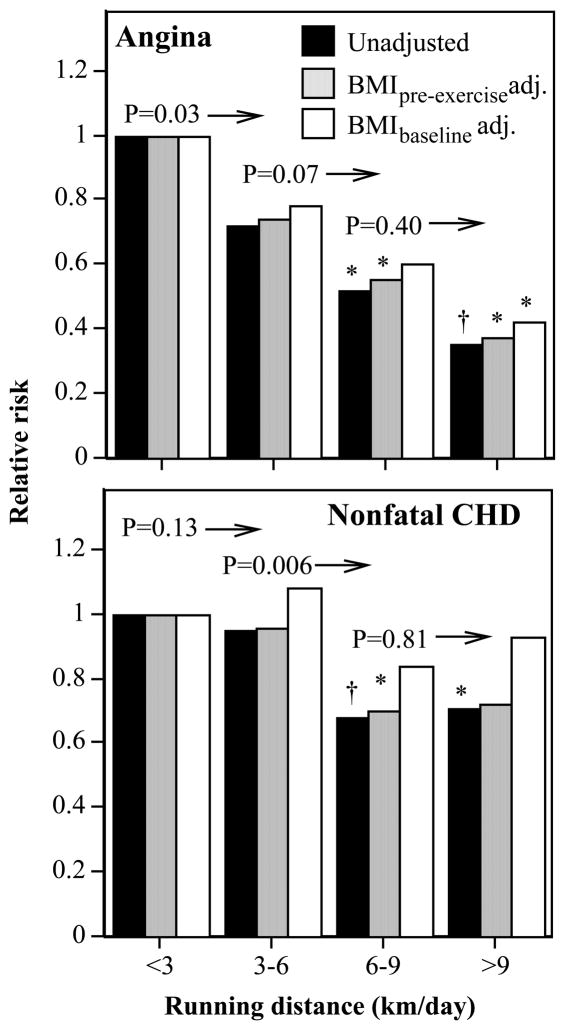
Figure 1 displays the declines in nonfatal CHD and angina risks per km/day run. Compared to men who exercise at guideline levels (<3 km/day category), those who exceeded 9 km/day had 29% lower risk for nonfatal CHD (P = 0.04), a 29% risk reduction for revascularization procedures (P = 0.07, not displayed), and a 65% risk reduction for angina (P = 0.008). There was also a 26% risk reduction for fatal plus nonfatal CHD (P = 0.06). In the figures, the probabilities above the bars and to the left of the arrows give the significance of the risk reduction for all greater distances relative to that distance category, e.g., running≥6 km/day was associated with significantly lower nonfatal CHD risk than running 3–6 km/day at P = 0.006. These bar graphs show significant risk reductions for nonfatal CHD above guideline activity levels. Adjustment for baseline BMI generally attenuated the risk reduction, whereas adjustment for pre-exercise BMI did not, again suggesting that self-selection based on initial weight did not appear to account for the attenuation in the risk reduction produced by baseline BMI adjustment.
Figure 1.
Relative risk from survival analyses of participant-reported physician-diagnosed angina and nonfatal CHD (i.e., myocardial infarction, revascularization procedures and angina) by physical activity (km/day running distance) in 28,287 men. Risks adjusted for age, education, intakes of meat, fish, fruit and alcohol, aspirin use, and pack-years of past cigarette use. Significance levels provided above the bars and to the left of the arrows are relative to all higher running distances (e.g., men who exceed 6 km/day have significantly lower risk for nonfatal CHD than men who average 3–6 km/day at P = 0.006). Significant differences relative to the lowest-mileage runners are coded *P < 0.05 and †P < 0.01.
Discussion
Meta-analyses of prior epidemiological studies collectively portray a linear decline in CHD risk with increasing population percentiles of physical activity [15], representing a reduction in CHD risk of about 30% or less [15]. The current report demonstrates clinically meaningful additional reductions in CHD risk for exercise doses that exceed guideline levels. The average energy expenditure of the lowest running category (756 METmin/week for the <3 km/day category [2], calculated as 61.2 METmin/km) falls at the upper limit of the recommended minimum activity range (450–750 METmin/week) and much above the specific recommendation for a 30 min brisk walk five days per week (495 METmin/week) [1]. Compared to guideline levels, the risk for men who ran >9 km/day was 26% lower for CHD, 29% lower for revascularization procedures, and 65% lower for angina (Fig. 1). This is comparable to the CHD-risk reduction others report for moderate doses of moderate activity versus inactivity [1]. In addition to the reductions in CHD risk reported here, other benefits to men exceeding the minimum guideline levels include 30% lower odds for hypertension [5], 47% lower odds for hypercholesterolemia [5], 68% lower odds for diabetes [5], a 60% lower risk for stroke [6], 48% lower risk for diverticular disease [7], 33% lower risk for benign prostatic hyperplasia [8], 52% lower risk for gallbladder disease [9], and 45% lower risk for gout [10].
The lower CHD risk of the higher mileage runners is consistent with the biomarkers of risk reported for a subset of these men [3]. Per km/week run, HDL-cholesterol levels increased 0.136 mg/dl, LDL-cholesterol decreased 0.085 mg/dl, triglycerides decreased 0.476 mg/dl, fasting plasma glucose decreased 0.025 mg/dl, and systolic and diastolic blood pressure decreased 0.040 and 0.027 mmHg per km/week run, respectively.
The reduction in CHD risk with running distance appears to be mediated in part via the runners’ leanness (Table 1). This was not due to leaner men and women choosing to run further since adjusting for their pre-exercise BMI did not affect the risk reduction. Even among vigorously active, ostensibly healthy-weight men and women, greater body weight significantly increases the risks for incident hypertension [11], hypercholesterolemia [11], diabetes [11], and CHD [4]. Vigorous exercise produces greater leanness by: (1) preventing long-term, age-related weight gain in proportion to the exercise dose [12] and (2) acutely affecting body weight in relation to the change in vigorous exercise [13]. Over time, the weight gain from decreasing exercise appears to be greater than the weight loss from increasing exercise [14], suggesting that a hiatus from vigorous exercise may result in a net weight gain, ergo the importance of sustained activity without extended interruption.
It is acknowledged that additional unmeasured factors could have contributed to the associations between CHD and running distance, including other health behaviors. For example, the Health Professionals Follow-up Study reported that their more vigorously active participants had more routine medical check-ups than less active men [16]. We also do not know the changes in running or other physical activities that may have occurred prior to their CHD event.
Our current and earlier published results may support a two tiered formulation for public health physical activity guidelines: one for the 49.3% of men who fall short of the minimum recommendations; a second for the 50.7% of men who already satisfy guideline levels [1]. This two-tiered approach would satisfy the pragmatic need to promote achievable physical activity goals that provide important health benefits to mostly sedentary Americans, while not compromising the potential to maximize health in those already active.
Acknowledgments
This research was supported in part by grant AG032004 from the Institute of Aging and was conducted at the Ernest Orlando Lawrence Berkeley National Laboratory (Department of Energy DEAC03- 76SF00098 to the University of California). The author wishes to thank Ms. Kathryn Hoffman for her help in collecting the data and reviewing the manuscript.
Abbreviations
- CHD
Coronary heart disease
- BMI
body mass index
- km
kilometer
References
- 1.Haskell WL, Lee IM, Pate RR, et al. American College of Sports Medicine; American Heart Association, Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–93. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 2.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(Suppl):S498–516. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 3.Williams PT. Relationship of distance run per week to coronary heart disease risk factors in 9,920 male runners. The National Runners’ Health Study. Arch Inter Med. 1997;157:191–8. [PMC free article] [PubMed] [Google Scholar]
- 4.Williams PT, Hoffman K. Optimal body weight for the prevention of coronary heart disease in normal-weight physically active men. Obesity (Silver Spring) 2009;17:1428–34. doi: 10.1038/oby.2008.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams PT. Vigorous exercise, fitness, and incident hypertension, high cholesterol, and diabetes. Med Sci Sports Exerc. 2008;40:998–1006. doi: 10.1249/MSS.0b013e31816722a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Williams PT. Reduction in incident stroke risk with vigorous physical activity during 7.7-year follow-up of the National Runners’ Health Study. Stroke. 2009;40:1921–3. doi: 10.1161/STROKEAHA.108.535427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Williams PT. Incident diverticular disease inversely related to vigorous physical activity. Med Sci Sports Exerc. 2009;41:1042–7. doi: 10.1249/MSS.0b013e318192d02d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams PT. Effects of physical activity and cardiorespiratory fitness on incident benign prostatic hyperplasia in vigorously active men. Med Sci Sports Exerc. 2008;40:1733–9. doi: 10.1249/MSS.0b013e31817b8eba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams PT. Independent effects of cardiorespiratory fitness, vigorous physical activity, and body weight on gallbladder disease risk during 7.6 years of followup. Am J Gastroenterol. 2008;103:2239–47. doi: 10.1111/j.1572-0241.2008.01944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams PT. Effects of diet, physical activity and performance and body weight on incident gout in ostensibly healthy, vigorously active men. Am J Clin Nutr. 2008;87:1485–93. doi: 10.1093/ajcn/87.5.1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Williams PT, Hoffman K, La I. Weight-related increases in hypertension, hypercholesterolemia, and diabetes risk in normal weight male and female runners. Arterioscler Thromb Vasc Biol. 2007;27:1811–9. doi: 10.1161/ATVBAHA.107.141853. [DOI] [PubMed] [Google Scholar]