Summary
OBJECTIVE
To evaluate optic nerve sheath (ONS) ultrasound as a non-invasive method of detecting raised intracranial pressure (ICP) and to establish normal ONS diameter data for African children. method Children with acute neurological disease admitted to the Paediatric Department of Queen Elizabeth Central Hospital, Malawi had ultrasound measurements of ONS diameter. Controls were children admitted to the same department with non-neurological disease. The mean of three measurements of the ONS diameter was used for analysis. Children were assessed for clinical signs of raised ICP. Patients had CT brain scans if required for their normal clinical care.
RESULTS
In 14 children with neurological disease and clinical signs suggestive of raised ICP, the mean ONS diameter was 5.4 mm (range 4.3–6.2 mm). Radiological signs on CT scans substantiated the presence of raised ICP in eight (all those scanned). In seven children with neurological disease but no specific signs of raised ICP the mean ONS diameter was 3.6 mm (range 2.8–4.4 mm). None of four of these patients examined by CT scan had signs of elevated ICP. The mean ONS diameter in 30 controls without neurological disease was 3.5 mm (range 2.5–4.1 mm). If 4.2 mm is taken as the upper limit of normal the sensitivity and specificity of this test for elevated ICP is 100% and 86%, respectively.
CONCLUSION
ONS ultrasound is an accurate method for detecting raised ICP that can be applied in a broad range of settings. It has the advantages of being a non-invasive, bedside test, which can be repeated multiple times for re-evaluation.
Keywords: intracranial hypertension, optic nerve, ultrasound, Africa, papilloedema
Introduction
Raised intracranial pressure (ICP) complicates a range of neurological diseases in children and can lead to death from brainstem herniation. In developing countries typical causal syndromes include meningitis, encephalitis, cerebral malaria, space occupying lesions (SOL), and frequently, coma of unknown origin. ICP can be measured by lumbar puncture (LP), but this is invasive, cannot be repeated frequently and in some cases is contra-indicated. The facilities to perform computed tomography (CT) scans, which allow raised ICP to be inferred from radiological signs, are not available in most African hospitals. A simple, non-invasive method of detecting raised ICP that allows easy re-evaluation is needed to guide treatment decisions. Ultrasound measurement of the optic nerve sheath (ONS) is such a technique.
The ONS is continuous with the brain’s dura mater and expands in the presence of raised ICP transmitted through the sub-arachnoid space (Helmke & Hansen 1996a,b; Hansen & Helmke 1997). The distension is maximal 3 mm behind the eye. Several studies suggest that ultrasound measurement of ONS diameter provides accurate, reproducible information on the presence of elevated ICP (Ballantyne et al. 1999, 2002). This non-invasive technique has been used successfully in emergency rooms (Blaivas et al. 2003; Tsung et al. 2005), children with hydrocephalus (Newman et al. 2002), and with other causes of raised intracranial pressure (Malayeri et al. 2005). No studies have assessed ONS ultrasound in a resource-poor setting or described control data for African children.
In this prospective study we aimed to investigate sonographic measurement of the ONS diameter as a method for detecting raised ICP in Malawian children with neurological disease, and to establish normal values from controls.
Patients and methods
The study was undertaken in the Paediatric Department at Queen Elizabeth Central Hospital, Blantyre, Malawi, from February 2005 to May 2006. We recruited patients with acute neurological disease, with and without clinical signs to suggest raised ICP. Controls were recruited from patients with non-neurological conditions. Patients with cerebral malaria were not included as they were subject to a parallel disease-specific study. Parents or guardians were asked for verbal consent to participate in the study in their own language.
Approximately half of the patients with neurological disease had CT brain scans as part of their routine care. These were reported by a radiologist (SK) who was unaware of the results of the ONS diameter measurements. CT signs suggestive of raised ICP include compression of ventricles and effacement of basilar cisterns and cortical sulci. Where raised ICP is accompanied by cerebral oedema, the brain parenchyma shows a generalized reduction in attenuation. When the cause of the increased ICP is a unilateral mass lesion then additional signs include midline shift to the contra-lateral side and obstructive hydrocephalus in one or more ventricles.
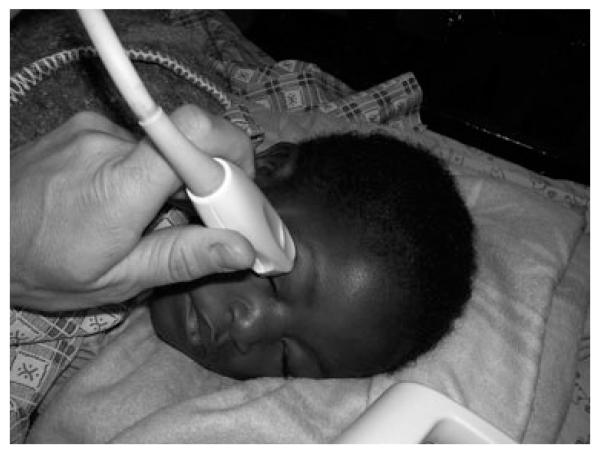
In recruited children an ultrasound examination of the ONS was undertaken by one observer (NB). A handheld Sonosite-180 ultrasound machine (Sonosite Inc., WA, USA) was used with a 7 MHz curved array transducer (4–7 MHz 11 mm array transducer set to highest resolution frequency of 7 MHz) designed for general paediatric use. The scan type was set to ‘Neonatal’ throughout, with maximum scan depth set to 4 cm and the gain control on the default setting. Ultrasound scans were undertaken through the closed eye lid from the temporal side performing an axial cut through the eye and including a longitudinal section of optic nerve (Figure 1). The left eye was usually imaged unless it was not accessible because of patient positioning. The optic disc and as long a section of optic nerve as possible was included in the freeze-frame. The option to toggle through the last 10 s of images was often used to obtain the best image. An example of normal and dilated ONSs is given in Figure 2.
Figure 1.
The technique of optic nerve sheath ultrasound using a paediatric curved array transducer through the closed eyelids.
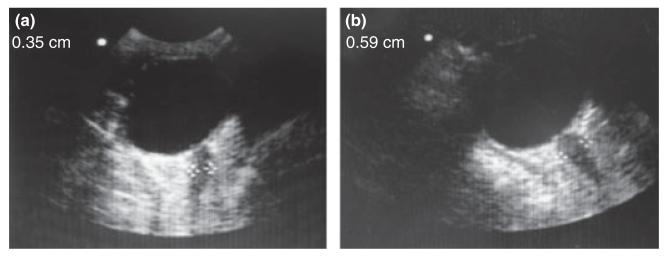
Figure 2.
Examples of the ultrasound image of a normal (a) and dilated (b) optic nerve sheath.
Measurements of the ONS diameter were made with electronic callipers 3 mm behind the posterior scleral surface of the globe. Care was taken to measure perpendicularly across the optic nerve. The mean was taken of three measurements from different scans, with the on-screen measurement masked to the scanner until each was finalized.
After ultrasound of the ONS an ophthalmological examination was undertaken including eye movements, pupil reactions and dilated fundoscopy, assessing the optic disc for papilloedema by an ophthalmologist (NB).
Ethical approval for the study was obtained from the University of Malawi College of Medicine Research Ethics Committee, and the Liverpool School of Tropical Medicine Research Ethics Committee, UK.
Results
Twenty-one patients with neurological disease were recruited to the study with a mean age of 69 months. The most frequent diagnoses were meningitis, SOL and coma of unknown origin. Raised ICP was suspected because of clinical signs in 14 patients. The most frequent clinical sign suggesting raised ICP was papilloedema, but sixth cranial nerve palsy or abnormal pupil reactions were taken as indicators of raised ICP in some patients. The depth of coma and overall condition of the patient were also considered. CT brain scans were done on eight of these patients and they all had radiological signs suggesting raised ICP. The mean ONS diameter of these patients was 5.4 mm (range 4.3–6.2 mm) (Table 1).
Table 1.
The mean of three ONS diameter measurements and CT brain scan reports of paediatric patients with neurological disease
| Patient | Age (months) |
Diagnosis | ONS diameter (mm) |
Clinical signs of raised intracranial pressure |
CT scan report |
|---|---|---|---|---|---|
| Patients with clinically suspected raised ICP | |||||
| 1 | 108 | Meningitis | 5.1 | Clinical deterioration and recovered respiratory arrest |
Gross hydrocephalus. Very tight brain with loss of gyri/sulci |
| 2 | 96 | SOL | 5.7 | Moderate papilloedema Bilateral VI nerve palsies |
SOL around lateral ventricles and sella turnica. Large ventricles. Obstructive hydrocephalus |
| 3 | 30 | SOL | 5.4 | Bilateral VI nerve palsies and upbeat nystagmus |
Obstructive hydrocephaly from brainstem glioma |
| 4 | 19 | Coma unknown | 5.6 | Moderate papilloedema Dilated unreactive pupils |
Not done |
| 5 | 48 | Meningitis | 5.4 | Moderate papilloedema Right dilated unreactive pupil |
Not done |
| 6 | 72 | Coma unknown | 4.9 | Mild papilloedema | Not done |
| 7 | 108 | TB Meningitis | 5.7 | Mild papilloedema Deepening coma |
Gross hydrocephalus. Multiple granuloma in parenchyma |
| 8 | 41 | SOL | 5.0 | Dilated unreactive pupils Absent oculocephalic reflex |
Not done |
| 9 | 144 | Hydrocephalus | 5.9 | Severe papilloedema VI nerve palsy Macrocephalic Ataxic gait |
Severe hydrocephalus with aqueduct stenosis |
| 10 | 15 | Suspected poisoning | 4.3 | Mild papilloedema | Not done |
| 11 | 93 | Coma unknown | 6.2 | Mild papilloedema | Cerebral oedema with compression of ventricles and basal cistern |
| 12 | 84 | Coma unknown | 5.8 | Severe papilloedema Anisocoria |
Mild communicating hydrocephalus. Left pontine infarct |
| 13 | 111 | Meningitis | 5.5 | Moderate papilloedema VI nerve palsy Unreactive pupils |
Not done |
| 14 | 31 | Coma unknown | 5.0 | Mild papilloedema | Severe brain oedema. The ventricles and basilar cisterns are compressed |
| Patients without clinically suspected raised ICP | |||||
| 15 | 56 | Coma unknown | 4.4 | None | Normal |
| 16 | 28 | Meningitis | 4.0 | None | Not done |
| 17 | 96 | SOL. Focal seizures | 4.0 | None | SOL. Astrocytoma? No mass effect |
| 18 | 96 | Brainstem tumour | 3.2 | None | Brainstem tumour. No hydrocephalus |
| 19 | 11 | Coma unknown | 3.5 | None | Not done |
| 20 | 18 | Kwashiorkor HIV Convulsions |
2.8 | None | Normal |
| 21 | 144 | Epilepsy New ataxia |
3.6 | None | Not done |
ONS, optic nerve sheath; ICP, intracranial pressure; SOL, space occupying lesion; TB, tuberculosis.
There were seven patients with neurological disease without papilloedema or other clinical signs suggestive of raised ICP. CT brain scans were performed in four of these and none showed radiological signs of elevated ICP. The mean ONS diameter of these patients was 3.6 mm (range 2.8–4.4 mm) (Table 1).
There were 30 controls with pneumonia, gastroenteritis, sepsis and uncomplicated malaria. Their mean age was 33 months. The mean ONS diameter of controls was 3.5 mm (range 2.5–4.1 mm). The procedure was generally well tolerated, even in fully conscious young children, but was not possible in three children because of lack of cooperation.
If an ONS diameter of 4.2 mm is taken as an upper limit of normal, and assuming neurological patients without clinical or CT signs of raised ICP indeed did not have raised ICP, then an enlarged ONS diameter gives a sensitivity of 100% and a specificity of 86% for the detection of raised ICP. There is one false positive, a patient with coma of unknown origin and normal CT brain scan. If a cut-off of 4.5 mm is used then the sensitivity is 93% and the specificity is 100%.
Discussion
The gold standard for monitoring ICP is an intracranial transducer, but these are invasive and only available in well-resourced specialist units. In this study, we have used clinical and radiological signs to gauge the presence of raised ICP in neurological patients. Against these standards we have demonstrated the ultrasonic measurement of the ONS diameter to be a reliable method of detecting raised ICP in children. It also has the advantages of being non-invasive, having no radiation exposure and being accessible at the bedside without moving critically ill patients. It can therefore be easily repeated to re-evaluate a patient. It requires only basic ultrasonography skills, and can be done with standard paediatric ultrasound equipment.
We have established control data for Malawian children with a normal range from 2.5 to 4.1 mm, which is similar to Iranian children (2.0–4.3 mm) (Malayeri et al.2005) and British children (2.1–4.3 mm) (Ballantyne et al. 1999). The mean ONS diameter for controls was 3.5 mm, slightly larger than that found in Iran (3.3 mm) and UK (3.1 mm).
If 4.2 mm is taken as the upper limit of normal, then the sensitivity and specificity of the test are very acceptable. The one false positive may actually have had raised ICP without any clinical or radiological signs. Only one true positive had an ONS diameter close to this cut-off (4.3 mm), but their ONS enlarged to 4.8 mm the next day. These cases were the only two to overlap in ONS diameter between patients suspected of having raised ICP, and those not, including controls.
There are a number of limitations to our study. The number in each group with neurological disease is not large, but was constrained by the number presenting over the study period. The ultrasound measurement of ONS diameter and assessment of papilloedema were made by the same observer. This raises the possibility of bias in the assessment of the presence of papilloedema, which may be relevant in mild cases. In order to minimize this we used a classification system based on specific optic disc features which has been previously validated (A. Smith, N.A.V. Beare, C. Musmba, J. Lochhead, C.R.J.C. Newt, unpublished data). We were unable to compare the ONS diameter with the LP opening pressure because in many cases the ONS ultrasound was done some time later when patients had deteriorated. The opening pressure was then no longer relevant.
It should be noted that the age of the control group is much less than of the cases. This reflects the older age of children with neurological problems compared to the majority of paediatric admissions with infectious aetiologies. Newman et al. (2002) found that the mean ONS enlarged with age, but that the majority of this increase occurred in the first year of life, with a very shallow curve thereafter to age 16. The variation around this mean is 10-fold greater that the increase of the mean from 1 to 16 years. As the use of ONS diameter as a diagnostic test relies on reference to ranges rather than means, we argue that the age difference between the control children and those with neurological disease is unlikely to affect our results or conclusions.
The measurement of ONS diameter by ultrasound is a useful method of non-invasively detecting raised ICP, and is as effective in an African setting as elsewhere. It can safely and rapidly provide information on patients’ ICP at the bedside, and can be re-evaluated frequently. Our data suggest that 4.2 mm should be regarded as the upper limit of normal in African children, and 4.5 mm or greater as clearly indicative of raised ICP.
Acknowledgements
This study was funded by a project grant from The Wellcome Trust and an Iris Award from the British Eye Research Fund. These supported NB and the purchase of the Sonosite US machine. We thank the patients and parents/guardians for participating in the study and the clinicians and nurses of the Department of Paediatrics who looked after them. Bill Newman provided valuable advice for setting up the study.
References
- Ballantyne J, Hollman AS, Hamilton R, et al. Transorbital optic nerve sheath ultrasonography in normal children. Clinical Radiology. 1999;54:740–742. doi: 10.1016/s0009-9260(99)91176-5. [DOI] [PubMed] [Google Scholar]
- Ballantyne SA, O’Neill G, Hamilton R, Hollman AS. Observer variation in the sonographic measurement of optic nerve sheath diameter in normal adults. European Journal of Ultrasound. 2002;15:145–149. doi: 10.1016/s0929-8266(02)00036-8. [DOI] [PubMed] [Google Scholar]
- Blaivas M, Theodoro D, Sierzenski PR. Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Academic Emergency Medicine. 2003;10:376–381. doi: 10.1111/j.1553-2712.2003.tb01352.x. [DOI] [PubMed] [Google Scholar]
- Hansen HC, Helmke K. Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: ultrasound findings during intrathecal infusion tests. Journal of Neurosurgery. 1997;87:34–40. doi: 10.3171/jns.1997.87.1.0034. [DOI] [PubMed] [Google Scholar]
- Helmke K, Hansen HC. Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension II. Patient study. Pediatric Radiology. 1996a;26:706–710. doi: 10.1007/BF01383384. [DOI] [PubMed] [Google Scholar]
- Helmke K, Hansen HC. Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension. I. Experimental study. Pediatric Radiology. 1996b;26:701–705. doi: 10.1007/BF01383383. [DOI] [PubMed] [Google Scholar]
- Malayeri AA, Bavarian S, Mehdizadeh M. Sonographic evaluation of optic nerve diameter in children with raised intracranial pressure. Journal of Ultrasound Medicine. 2005;24:143–147. doi: 10.7863/jum.2005.24.2.143. [DOI] [PubMed] [Google Scholar]
- Newman WD, Hollman AS, Dutton GN, Carachi R. Measurement of optic nerve sheath diameter by ultrasound: a means of detecting acute raised intracranial pressure in hydrocephalus. British Journal of Ophthalmology. 2002;86:1109–1113. doi: 10.1136/bjo.86.10.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsung JW, Blaivas M, Cooper A, Levick NR. A rapid noninvasive method of detecting elevated intracranial pressure using bedside ocular ultrasound: application to 3 cases of head trauma in the pediatric emergency department. Pediatric Emergency Care. 2005;21:94–98. doi: 10.1097/01.pec.0000159052.64930.64. [DOI] [PubMed] [Google Scholar]