Abstract
Background
The prevalence of anemia among antiretroviral-naïve HIV-infected patients in China has not been well characterized. We conducted a cross-sectional study to estimate the prevalence of anemia among Chinese adults with newly diagnosed HIV/AIDS.
Methods
One thousand nine hundred and forty-eight newly diagnosed HIV-infected patients in China were selected during 2009 and 2010. Serum samples obtained from each individual were collected to measure hemoglobin levels. Demographics and medical histories were recorded. Factors associated with the presence of anemia were analysed by logistic regression.
Results
Among the 1948 patients, 75.8% were male. Median age was 40 years (range: 18–80 years). The overall prevalence of anemia among HIV-infected patients was 51.9% (51.5% among men, 53.2% among women). The prevalences of mild anemia, of moderate anemia, of severe anemia were 32.4%, 17.0%, and 2.5%, respectively. The prevalence of anemia was higher among ethnic minority patients than among the Han patients (70.9% versus 45.9%). The prevalence of anemia increased with increasing age (49.6%, 53.5% and 60.1% among patients who were 18–39, 40–59, and ≥60 years of age respectively) and with decreasing CD4 count (14.0%, 22.4%, 50.7%, and 74.6% among patients with CD4 count of ≥350, 200–349, 50–199, and <50 cells/mm3 respectively). The logistic regression analysis showed that older age, lower CD4 count and minority ethnicity were significantly associated with an increased risk of anemia.
Conclusions
Anemia is highly prevalent among Chinese adults with newly diagnosed HIV/AIDS, but severe anemia is less prevalent in this population. Older age, lower CD4 count and minority ethnicity are associated with an increased risk of anemia.
Introduction
Hematologic abnormalities are among the most common manifestations of advanced HIV infection and AIDS [1]–[3]. Of these abnormalities, anemia is the most common hematologic manifestation, affecting 60% to 80% of HIV-infected patients in late-stage disease [1], [4], [5]. Anemia also comprises a significant proportion of the adverse events secondary to antiretroviral therapy (ART) [6], [7]. Hematologic abnormalities have been documented as strong independent predictors of morbidity and mortality in HIV-infected patients [8]. A large epidemiological study of 32,867 HIV-infected adults and adolescents in USA found that the risk of death was 170% greater for persons with persistent anemia compared with those whose anemia had resolved [9]. This study showed that anemia, particularly anemia that does not resolve, is associated with shorter survival of HIV-infected patients [9]. Anemia is also one of the strongest predictors of HIV mortality and poor responses to ART [8]. Reduction of anemia is thus one of the key components of medical care for HIV-infected patients.
In different study settings, the prevalence of anemia in persons with AIDS has been estimated at 63% to 95%, making it more common than thrombocytopenia or leukopenia in patients with AIDS [9]. Although anemia is the most common hematologic manifestation of HIV infection, and may have considerable impact on patients’ well-being, treatment and care, so far the prevalence of anemia among newly diagnosed HIV-infected patients in China has not been extensively studied. Such information for newly diagnosed HIV-infected patients may help to inform treatment of HIV-infected individuals. Accordingly, the purpose of the present study was to estimate the prevalence of anemia among Chinese adults with newly diagnosed HIV/AIDS, and to identify demographic and HIV-related factors that were associated with the presence of anemia.
Methods
Ethics Statement
Written informed consent was obtained for all subjects; consent forms and procedures, as well as survey protocol, were approved by the Shanghai Public Health Clinical Center Ethics Committee. No patient identifiers were included in the dataset used for this analysis.
Study Population
We conducted a cross-sectional survey on HIV/AIDS in China’s HIV epidemic provinces and municipalities including Xinjiang, Jiangxi, Henan, Heilongjiang, Guangdong, Shaanxi, Guangxi, Hunan, Shanghai and Yunnan during 2009 and 2010. The survey subjects were newly diagnosed HIV-infected patients who had not received ART. Subjects aged 18 years or more at the time of enrolment with documented HIV infection were eligible for this study. Patients on ART were excluded from the study. All patients were confirmed to be positive for HIV antibody through laboratory detection, and the diagnosis was in line with national HIV/AIDS diagnostic criteria.
Blood Samples
For newly diagnosed HIV-infected patients, three-milliliter venous blood samples were obtained from each individual for the measurement of hemoglobin levels. Hemoglobin level was determined in each blood sample with a CELL DYN 3200 hematology analyzer (Abbott Laboratories, USA), at the clinical laboratories in each province. All the study laboratories successfully completed a standardization and certification program.
Study-Outcome Definitions
Results of hemoglobin level testing were categorized as follows: anemia [(hemoglobin level<120 g/l (men) or 110 g/l (women )], mild anemia [(hemoglobin level>90 g/l and <120 g/l (men) or 110 g/l (women )], moderate anemia (hemoglobin level>60 g/l and ≤90 g/l), and severe anemia (hemoglobin level≤60 g/l). Anemia was defined as either mild anemia, moderate anemia, or severe anemia.
Data Collection
Data were collected according to standardised criteria. On enrolment, standardised data collection forms were completed at the sites providing information from patients interview and patient case notes. Data collected on newly identified cases included demographic information, risk-behavior information (injection drug use, history of heterosexual or homosexual sex, receipt of blood transfusion), and laboratory test results. Variables of interest included age, sex, HIV transmission route, and CD4 count. Age was denoted as <40, 40–59, or ≥60 years. HIV transmission route was categorized as sexual contact (including homosexual or heterosexual), blood (including blood transfusion or injection drug use), or unknown transmission risk. CD4 count was denoted as <50, 50–199, 200–349 or ≥350 cells/mm3.
Statistical Analysis
SPSS software for Windows (version 11.5) was used for statistical analysis. Continuous variables were computed with standard methods and are presented as mean and standard deviations (SD). Categorical variables are reported as frequencies and percentage of each category. We performed one-way ANOVA to compare hemoglobin levels among patients with different CD4 count. Correlations between hemoglobin level and CD4 count were evaluated using the Pearson’s correlation test. A chi-square test was applied for categorical attributes. The odds ratio and 95% confidence intervals were calculated to assess the relationship between each risk factor and the risk of anemia; to adjust for the effects of potential confounders, we used a logistic regression model. All variables included in the models were determined a priori based on epidemiological importance and biological plausibility. Variables included in the models were age, sex, ethnicity, CD4 count, and HIV transmission route. The statistical test was two-tailed and performed at a level of statistical significance of 0.05.
Results
Patient Characteristics
We included a total of 1948 adults with newly diagnosed HIV/AIDS. Table 1 describes the basic characteristics of the study population. The study sample was primarily male (75.8%) (1476), the mean age was 40 years (41 years for males, 38 years for females), 24.1% (470) were ethnic minorities, and the mean CD4 count was 136 cells/mm3. Most patients acquired HIV through sexual contact (74.2%) (1446).
Table 1. Basic characteristics of 1948 newly diagnosed HIV/AIDS patients in China.
| Characteristic | Patient No. (%) |
| Age, years | |
| 18–39 | 1082 (55.5) |
| 40–59 | 708 (36.3) |
| ≥60 | 158 (8.2) |
| Mean age (range) | 40 (18, 80) |
| Sex | |
| Male | 1476 (75.8) |
| Female | 472 (24.2) |
| HIV transmission category | |
| Sexual contact | 1446 (74.2) |
| Blood | 340 (17.5) |
| Unknown transmission risk | 162 (8.3) |
| CD4 count, cells/mm3 | |
| <50 | 796 (40.9) |
| 50–199 | 611 (31.4) |
| 200–349 | 370 (19.0) |
| ≥350 | 171 (8.7) |
| Mean CD4 count (range) | 136 (1, 891) |
| Ethnicity | |
| Han | 1478 (75.9) |
| Other (minority) | 470 (24.1) |
| Anemia | |
| Overall | 1011 (51.9) |
| Mild | 631(32.4) |
| Moderate | 332(17.0) |
| Severe | 48(2.5) |
Hemoglobin Levels among Men and Women with HIV/AIDS
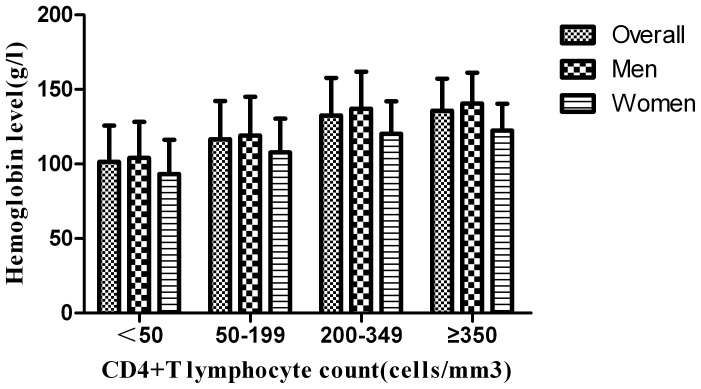
The mean hemoglobin level was 118.1±28.2 g/l among men and 105.8±25.1 g/l among women, respectively. Figure 1 describes the mean hemoglobin level among men and women according to CD4 count. The mean hemoglobin level showed an increasing trend with increasing CD4 count (P<0.001 overall, men, and women). Using the Pearson’s correlation, there was a significant and positive correlation (r2 = 0.2079; P<0.001) between hemoglobin level and CD4 count.
Figure 1. The mean hemoglobin level among men and women according to CD4 count.
The numbers of men with CD4 counts of <50, 50–199, 200–349, and ≥350 cells/mm3 were 604, 474, 272, and 126, respectively. The numbers of women with CD4 counts of <50, 50–199, 200–349, and ≥350 cells/mm3 were 192, 137, 98, and 45, respectively. One-way ANOVA was used to compare hemoglobin levels among patients with different CD4 count. The mean hemoglobin level showed an increasing trend with increasing CD4 count (P<0.001 overall, men, and women).
Prevalence of Anemia among Men and Women with HIV/AIDS
Among the 1948 patients, 1011 (51.9%) had anemia (Table 1). Among 1476 male patients, 760 (51.5%) had anemia; among 472 female patients, 251 (53.2%) had anemia. The prevalence of anemia did not differ significantly according to sex (P = 0.523). The prevalences of mild anemia, of moderate anemia, of severe anemia were 32.4%, 17.0%, and 2.5%, respectively (Table 1). The prevalences of mild anemia, of moderate anemia, of severe anemia were 33.9%, 15.7% and 1.9% among men and 27.5%, 21.4% and 4.2% among women, respectively. The prevalences of moderate anemia and of severe anemia among women were significantly higher than those among men (P = 0.004, P = 0.004), the prevalence of mild anemia was significantly higher among men than among women (P = 0.01).
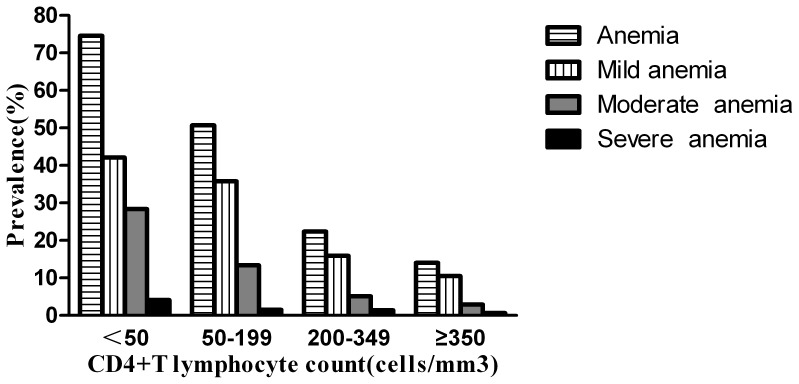
Prevalence of Anemia in Patients with Different CD4 Count
Figure 2 describes the prevalences of anemia, mild anemia, of moderate anemia, of severe anemia among patients with different CD4 counts. The overall prevalence of anemia was 14.0%, 22.4%, 50.7%, and 74.6% among patients with CD4 counts of ≥350, 200–349, 50–199, and <50 cells/mm3, respectively. The overall prevalence of anemia increased with decreasing CD4 count (P<0.001). The prevalence of mild anemia, of moderate anemia, of severe anemia increased with decreasing CD4 count (P<0.001, P<0.001, P = 0.001).
Figure 2. Prevalence of anemia, mild anemia, moderate anemia, and severe anemia among patients with different CD4 count.
The numbers of patients with CD4 counts of <50, 50–199, 200–349, and ≥350 cells/mm3 were 796, 611, 370, and 171, respectively. A chi-square test was applied to compare differences in prevalence of anemia, mild anemia, moderate anemia, and severe anemia among patients with different CD4 count. The prevalence of anemia, of mild anemia, of moderate anemia, of severe anemia increased with decreasing CD4 count (P<0.001, P<0.001, P<0.001, P = 0.001).
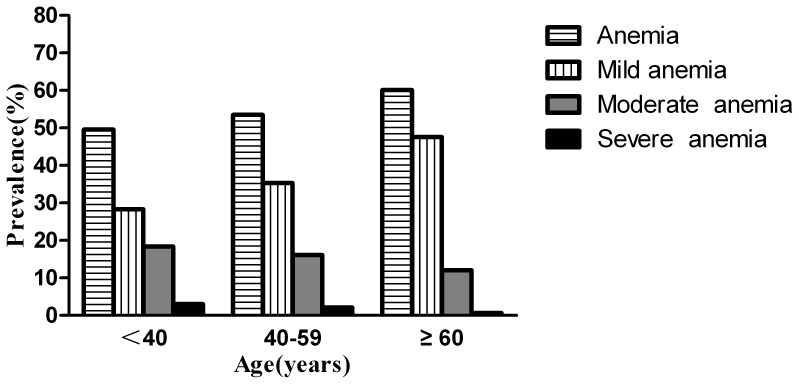
Prevalence of Anemia in Patients with Different Age
Figure 3 describes the prevalences of anemia, mild anemia, moderate anemia, and severe anemia among patients according to age. The prevalence of anemia was 49.6%, 53.5% and 60.1% among patients who were 18–39, 40–59, and ≥60 years of age, respectively. The prevalence of anemia increased with increasing age (P = 0.026). The prevalence of mild anemia increased with increasing age (P<0.001), the prevalences of moderate anemia and of severe anemia did not differ significantly according to age (P = 0.098, P = 0.154).
Figure 3. Prevalence of anemia, mild anemia, moderate anemia, and severe anemia among patients with different age.
The numbers of patients who were 18–39, 40–59, and ≥60 years of age were 1082, 708, and 158, respectively. A chi-square test was applied to compare differences in prevalence of anemia, mild anemia, moderate anemia, and severe anemia among patients with different age. The prevalence of anemia increased with increasing age (P = 0.026). The prevalence of mild anemia increased with increasing age (P<0.001). The prevalences of moderate anemia and of severe anemia did not differ significantly according to age (P = 0.098, P = 0.154).
Prevalence of Anemia in Patients according to Ethnicity
The prevalence of anemia was 45.9% and 70.9% among the Han patients and ethnic minority patients, respectively. The prevalence of anemia among ethnic minority patients was higher than that among the Han patients (P<0.001). The prevalences of mild anemia, of moderate anemia, of severe anemia were 29.5%, 14.5% and 1.8% among the Han patients and 41.5%, 24.9% and 4.5% among ethnic minority patients, respectively. The prevalences of mild anemia, moderate anemia and of severe anemia among ethnic minority patients were significantly higher than those among the Han patients (P<0.001, P<0.001, P = 0.001).
Risk Factors for Anemia among Newly Diagnosed HIV-Infected Adults
In a multivariate analysis using a logistic regression model, we analyzed factors associated with the presence of anemia. Table 2 summarizes the results of the final regression model. Older age, lower CD4 count and minority ethnicity were significantly associated with an increased risk of anemia. HIV transmission route and sex failed to show an association with the presence of anemia.
Table 2. Identification of risk factors for the presence of anemia, results of the regression model.
| Risk factor | P value | Odds ratio | 95% Confidence interval |
| Age, per 20-year increment | 0.025 | 1.202 | (1.023, 1.411) |
| Minority ethnicity | <0.001 | 2.695 | (2.099, 3.460) |
| CD4 count, per decrease of 150 cells/mm3 | <0.001 | 2.919 | (2.585, 3.297) |
| Sex | 0.075 | 1.243 | (0.979, 1.580) |
| HIV transmission route | |||
| Sex contact | 0.070 | 1.000 | – |
| Blood | 0.057 | 1.305 | (0.993, 1.715) |
| Unknown transmission risk | 0.126 | 1.331 | (0.923, 1.920) |
Discussion
In this study, we observed a high prevalence of anemia among Chinese adults with newly diagnosed HIV/AIDS. The subjects were of broad geographic origin, which suggests that anemia is relatively prevalent among newly diagnosed HIV-infected patients in China. This constitutes further evidence of the need for monitoring hematologic parameters of HIV-infected patients, both before ART initiation and routinely during treatment, to ensure that mortality and morbidity are minimized and quality of life optimized. Routine blood tests are currently recommended for HIV-infected patients both before and after initiating HIV treatment by HIV care and treatment guidelines. In our study, the overall prevalence of anemia among newly diagnosed HIV-infected patients was 51.9%, with the majority of patients having mild to moderate anemia. Thus severe anemia appears to be less common in the study population.
There may be important biological implications to our finding that the mean hemoglobin level increased with increasing CD4 count, and that lower CD4 count was associated with an increased risk of anemia, in other words that the prevalence and severity of anemia increased with decreasing CD4 count. This suggests that the presence of anemia among newly diagnosed HIV-infected patients is related to HIV infection.
Anemia in HIV-infected patients is likely to be multifactorial [9]. Our study population was newly diagnosed HIV-infected patients who had not received ART, hence anemia among these patients was not caused by antiretroviral drugs. The pathophysiology of HIV-associated hematologic abnormalities may involve direct HIV infection of bone marrow progenitors, abnormal regulation of hematopoiesis and/or autoimmune phenomena [1]. Direct infection of marrow precursor cells has been hypothesized, but not proven [10]. HIV infection alone, without other complicating illnesses, may produce anemia in some patients [11]. The pathophysiology of HIV-associated anemia may involve three basic mechanisms: decreased red blood cell (RBC) production, increased RBC destruction, and ineffective RBC production [4]. Therefore, it is important to identify anemic patients and to consider HIV as a possible underlying cause. At the same time patients with HIV infection should be investigated and treated for anemia to reduce the morbidity of the patient.
Our findings are consistent with several published studies, which also indicate high anemia prevalence and similar associated risk factors in HIV-infected patients. Meidani and colleagues conducted a cross-sectional study [4] to investigate the prevalence of anemia and its related factors in HIV positive patients in Isfahan, Iran. In that study, the overall prevalence of anemia was 71%, with the majority of patients having mild to moderate anemia. Mild to moderate anemia and severe anemia occurred in 67% and 4% of patients, respectively. Mildvan et al. found that the prevalence of anemia in HIV-infected patients receiving no ART was 39.7%, and that anemia was more prevalent among patients with CD4 count <200 cells/mm3 [7]. In a cross-sectional study in the Mexican patients without ART, Mata-Marin and colleagues found a positive correlation between hemoglobin and CD4 count. That study also showed that CD4 count<200 cells/mm3 was associated with an increased risk of anemia [12]. Another study showed that the prevalence of anemia was 69.17% among ART naive patients in Benin City, Nigeria [13]. Parinitha et al. found that the prevalence of anemia was 84% among ART naive patients in India [14]. That study revealed a significant increase in the number of cases of anemia with decreasing CD4 counts. Based on the results of our study and in accordance with the literature on this topic, we conclude that anemia is highly prevalent among newly diagnosed HIV-infected patients, and it is more frequent with progression of HIV disease. The reported prevalence of anemia in HIV-infected populations differed significantly, with differences in prevalence explained by differences in the demographic characteristics and criteria of anemia used.
Our study showed that anemia was more frequent among ethnic minority patients than among the Han patients. Minority ethnicity was significantly associated with an increased risk of anemia, increasing the odds by a factor of 2.695. This association could be because of environmental and nutritional factors, socio-economic status and lifestyle or a combination of these factors. It is also possible that minority ethnicity is a marker for other factors that are associated with increased incidence of anemia but that were not included in our analysis. Mildvan et al. found that anemia in HIV-infected patients receiving no ART was more prevalent among blacks [7]. A study [9] from USA showed that the incidence of anemia is associated with black race. These findings suggest that race/ethnicity can be a factor associated with the presence of anemia among HIV-infected patients.
In this study population, we found that moderate to severe anemia was more common in women than in men, and that mild anemia was more common in men than in women. Mildvan et al. found that anemia in HIV-infected patients receiving no ART was more prevalent among men, and that marked anemia was more common in women [7]. Another two studies [15], [16] showed that female gender was significantly associated with anemia among HIV-infected individuals. Thus our findings are not inconsistent with gender influencing the frequency and severity of anemia among HIV-infected patients. However, we did not find a significant association between gender and the presence of anemia among newly diagnosed HIV-infected patients by a logistic regression model; the overall prevalence of anemia in our study population did not differ significantly according to gender. Therefore, the possible association between gender and anemia among newly diagnosed HIV-infected persons still needs further study.
In agreement with other reports [17], age is a factors influencing the prevalence of anemia in HIV-infected patients. Our study demonstrated that prevalence of anemia increased with increasing age. Older age was significantly associated with an increased risk of anemia. Injection-drug use may also influence the prevalence of anemia in HIV-infected patients [17]. However, HIV transmission route failed to show association with the presence of anemia in our study.
Some studies [18]–[20] showed that ART was associated with an improvement in HIV-associated anemia and the potential mechanisms that might be involved included a reduction in opportunistic infections and the anemia of chronic disease, and an improvement in nutritional status. However, anemia in HIV-infected patients is also associated with zidovudine use [6], [7], [21]. Zidovudine is still recommended as part of the first-line regimens in resource-limited settings. The high prevalence of anemia that we found among newly diagnosed HIV-infected patients emphasizes the need for close monitoring of patients on a zidovudine-based ART regimen. We suggest that resource-limited countries should develop a plan to move towards tenofovir-based first-line regimens to optimize treatment options, and that continuing comparisons of hematological parameters among newly diagnosed HIV-infected patients before and after ART initiation are warranted.
Some limitations to our study should be noted. First, potential sample selection bias may have affected the findings. The HIV epidemic is serious in some areas and among some most-at-risk populations in China. The study population is not representative of the entire HIV-infected population in China and so the results may not be generalizable. Second, the design of the study was observational, we were able to examine potential associations but were unable to assess causation. Third, the data which allow the classification of the causes of anemia such as reticulocyte counts, erythropoietin levels, iron turnover, and parvovirus IgM titers were not measured. Fourth, the definition of anemia chosen for this study was different from the WHO criteria for the diagnosis of anemia. Our estimates of anemia prevalence may underestimate the true impact of anemia in this population. In addition, numerous parameters (environmental and nutritional factors, socio-economic status, lifestyle and others) that may affect haemoglobin levels [22] were not assessed in our study. Therefore, we were not able to determine the association between these factors and the prevalence of anemia. Furthermore, if these variables had been controlled for, some variables such as CD4 count might not have remained significant in the logistic regression model.
Conclusions
Anemia is highly prevalent among adults with newly diagnosed HIV/AIDS in China. Older age, lower CD4 count and minority ethnicity are associated with an increased risk of anemia. It is important to routinely screen anemia for timely and adequate clinical management to reduce the morbidity of the patient. Further research is needed to evaluate the effects of treating anemia and the impact of anemia on ART and survival in HIV-infected patients.
Acknowledgments
We thank Dr. Xinhong Li (Shaanxi), Dr. Zhihao Meng (Guangxi), Dr. Xiangchan Lu (Guangxi), Dr. Fuxiang Wang (Heilongjiang), Dr. Yan Sun (Henan), Dr. Aihua Deng (Jiangxi), Dr. Hui Wang (Guangdong), Dr. Yuhuang Zhen (Hunan), Dr. Yuxia Song (Xinjiang), and Dr. Zengquan Zhou (Yunnan) for assistance with data collection. We thank Professor Douglas Lowrie (Shanghai Public Health Clinical Center, Fudan University) for reviewing this manuscript.
Funding Statement
This work was supported by Key Research grants from the Ministry of Science and Technolgy, the People’s Republic of China (NO: 2012ZX10001-003, 2011ZX09302-016). Website:http://www.most.gov.cn. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Zon LI, Arkin C, Groopman JE (1987) Haematologic manifestations of the human immune deficiency virus (HIV). Br J Haematol. 66: 251–256. [DOI] [PubMed] [Google Scholar]
- 2. Erhabor O, Ejele OA, Nwauche CA, Buseri FI (2005) Some haematological parameters in human immunodeficiency virus (HIV) infected Africans: the Nigerian perspective. Niger J Med. 14: 33–38. [DOI] [PubMed] [Google Scholar]
- 3. Bello JL, Burgaleta C, Magallon M, Herruzo R, Villar JM (1990) Hematological abnormalities in hemophilic patients with human immunodeficiency virus infection. Am J Hematol. 33: 230–233. [DOI] [PubMed] [Google Scholar]
- 4. Meidani M, Rezaei F, Maracy MR, Avijgan M, Tayeri K (2012) Prevalence, severity, and related factors of anemia in HIV/AIDS patients. J Res Med Sci. 17: 138–142. [PMC free article] [PubMed] [Google Scholar]
- 5.Munyazesa E, Emile I, Mutimura E, Hoover DR, Shi Q, et al. (2012) Assessment of haematological parameters in HIV-infected and uninfected Rwandan women: a cross-sectional study. BMJ Open. 2. pii: e001600. Available: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3533001. Accessed 21 March 2013. [DOI] [PMC free article] [PubMed]
- 6.Wills TS, Nadler JP, Somboonwit C, Vincent A, Leitz G, et al.. (2004) Anemia prevalence and associated risk factors in a single-center ambulatory HIV clinical cohort. AIDS Read. 14: 305–310, 313–315. [PubMed]
- 7. Mildvan D, Creagh T, Leitz G (2007) Anemia Prevalence Study Group (2007) Prevalence of anemia and correlation with biomarkers and specific antiretroviral regimens in 9690 human-immunodeficiency-virus-infected patients: findings of the Anemia Prevalence Study. Curr Med Res Opin. 23: 343–355. [DOI] [PubMed] [Google Scholar]
- 8. Anastos K, Shi Q, French AL, Levine A, Greenblatt RM, et al. (2004) Total lymphocyte count, hemoglobin, and delayed-type hypersensitivity as predictors of death and AIDS illness in HIV-1-infected women receiving highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 35: 383–392. [DOI] [PubMed] [Google Scholar]
- 9. Sullivan PS, Hanson DL, Chu SY, Jones JL, Ward JW (1998) Epidemiology of anemia in human immunodeficiency virus (HIV)-infected persons: results from the multistate adult and adolescent spectrum of HIV disease surveillance project. Blood. 91: 301–308. [PubMed] [Google Scholar]
- 10. Cleveland RP, Liu YC (1996) CD4 expression by erythroid precursor cells in human bone marrow. Blood. 87: 2275–2282. [PubMed] [Google Scholar]
- 11. Spivak JL, Barnes DC, Fuchs E, Quinn TC (1989) Serum immunoreactive erythropoietin in HIV-infected patients. JAMA. 261: 3104–3107. [PubMed] [Google Scholar]
- 12.Mata-Marín JA, Gaytán-Martínez JE, Martínez-Martínez RE, Arroyo-Anduiza CI, Fuentes-Allen JL, et al. (2010) Risk factors and correlates for anemia in HIV treatment-naïve infected patients: a cross-sectional analytical study. BMC Res Notes. 3: 230. Available: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2941498. Accessed 21 March 2013. [DOI] [PMC free article] [PubMed]
- 13. Omoregie R, Omokaro EU, Palmer O, Ogefere HO, Egbeobauwaye A, et al. (2009) Prevalence of anaemia among HIV-infected patients in Benin City, Nigeria. Tanzan J Health Res. 11: 1–4. [DOI] [PubMed] [Google Scholar]
- 14.Parinitha S, Kulkarni M (2012) Haematological changes in HIV infection with correlation to CD4 cell count. Australas Med J. 5: 157–162. Available: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3433730. Accessed 21 February 2013. [DOI] [PMC free article] [PubMed]
- 15. Subbaraman R, Devaleenal B, Selvamuthu P, Yepthomi T, Solomon SS, et al. (2009) Factors associated with anaemia in HIV-infected individuals in southern India. Int J STD AIDS. 20: 489–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mugisha JO, Shafer LA, Van der Paal L, Mayanja BN, Eotu H, et al. (2008) Anaemia in a rural Ugandan HIV cohort: prevalence at enrolment, incidence, diagnosis and associated factors. Trop Med Int Health. 13: 788–794. [DOI] [PubMed] [Google Scholar]
- 17. Belperio PS, Rhew DC (2004) Prevalence and outcomes of anemia in individuals with human immunodeficiency virus: a systematic review of the literature. Am J Med. 116 Suppl 7A27S–43S. [DOI] [PubMed] [Google Scholar]
- 18. Semba RD, Shah N, Vlahov D (2001) Improvement of anemia among HIV-infected injection drug users receiving highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 26: 315–319. [DOI] [PubMed] [Google Scholar]
- 19. Berhane K, Karim R, Cohen MH, Masri-Lavine L, Young M, et al. (2004) Impact of highly active antiretroviral therapy on anemia and relationship between anemia and survival in a large cohort of HIV-infected women: Women’s Interagency HIV Study. J Acquir Immune Defic Syndr. 37: 1245–1252. [DOI] [PubMed] [Google Scholar]
- 20. Moore RD, Forney D (2002) Anemia in HIV-infected patients receiving highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 29: 54–57. [DOI] [PubMed] [Google Scholar]
- 21. Richman DD, Fischl MA, Grieco MH, Gottlieb MS, Volberding PA, et al. (1987) The toxicity of azidothymidine (AZT) in the treatment of patients with AIDS and AIDS-related complex. A double-blind, placebo-controlled trial. N Engl J Med. 317: 192–197. [DOI] [PubMed] [Google Scholar]
- 22. Gonzalez L, Seley C, Martorano J, Garcia-Moreno I, Troncoso A (2012) Infections and inequalities: anemia in AIDS, the disadvantages of poverty. Asian Pac J Trop Biomed. 2: 485–488. [DOI] [PMC free article] [PubMed] [Google Scholar]