Abstract
Background
A prevalent modality to increase the amount of available bone prior to implantation is grafting of the maxillary sinus. Multiple factors such as the surgical technique, moment of implant placement as well as grafting materials and membranes are known to affect implant survival. However, the role of different factor combinations and associated reciprocal effects remain unclear. Conventional statistical methods do not consider inconsistency of study designs and do not take covariables into account. Hence, a systematic research and meta-analysis was conducted to investigate the influence of various treatment modalities on implant survival in the grafted maxillary sinus.
Materials and Methods
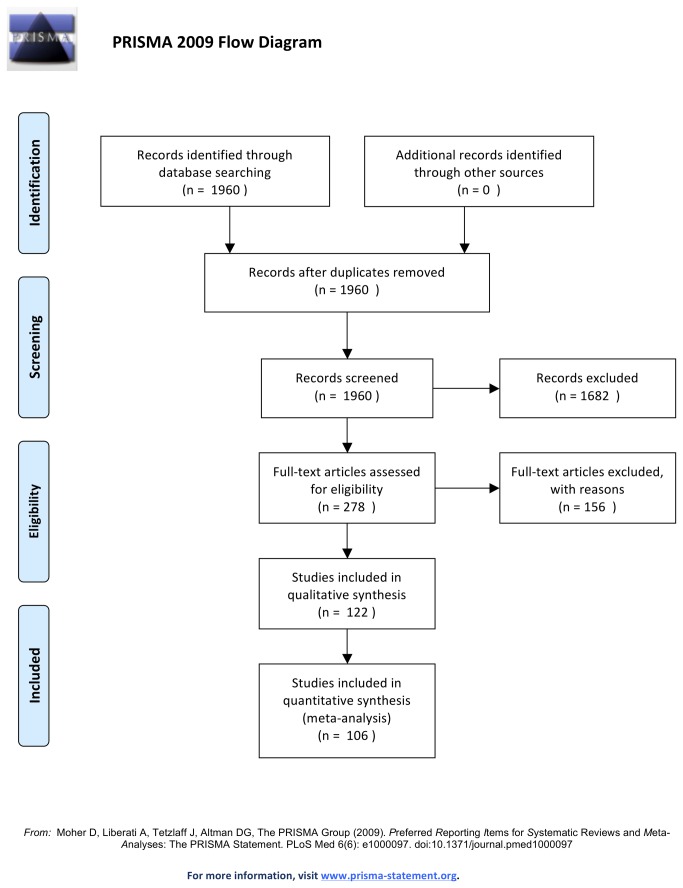
A meta-analysis was conducted according to the PRISMA guidelines. Articles published from 1980 through January 2013 were electronically and manually searched in MEDLINE (Ovid), the Cochrane Register of Controlled Trials, the Database of Abstracts of Effects, and the Cochrane Database of Systematic Reviews. Clinical reports on single intervention sinus augmentation with root-form implants, a minimum of 10 patients and 6 months of loading were eligible for inclusion if implant survival was stated or calculable. Results were calculated by non-parametric univariate Kaplan-Meier analysis and Bayesian multivariate interval-censored Cox regression.
Results
A total of 122 publications on 16268 endosseous implants placed in grafted maxillary sinus were included. The treatment parameters surgical approach, grafting material and implant type showed no selective preference. However, application of membranes showed a significantly reduced hazard-ratio, independent of other co-factors.
Conclusions
The use of membranes is the most significant factor to achieve long-term implant survival in sinus augmentation procedures. More data exceeding 3 years follow-up are needed to address prospective confounding and improve clinical evidence.
Introduction
In a continuously growing and aging society the need for implant based dento-maxillary rehabilitation is expanding. Besides aesthetic recovery, the regeneration of the physiological function of the dento-maxillary system is crucial for adequate nutrition and improvement in quality of live. Concurrently, dento-maxillary rehabilitation has a considerable effect on the overall morbidity especially in elderly people, and a resultant socio-economic impact [1,2]. Vogel et al. 2013 could directly link successful dental implantology in senior citizens with improved overall health, quality of life and decreased health care costs [3]. Still, the predominant challenge for successful dento-maxillary rehabilitation is residual bone, the pivotal factor in patients subjected to maxillary implantation. Advanced atrophy of the alveolar crest, primarily in patients with edentulous or partially edentulous posterior maxillae impairs conventional insertion of implants and restoration of the dento-maxillary system. Accordingly health-care decision-making vastly depends on valid clinical evidence to assess the most beneficial treatment modalities.
To date, based on the conventional sinus floor elevation (CSFE) developed over three decades ago [4] numerous successful techniques have been described to restore maxillary bone height [5,6]. Most techniques feature a lateral approach to the sinus cavity. A horizontal incision is made in the mucosa at the top of the alveolar crest or slightly palatally to lift a full-thickness flap that is deflected to expose the lateral antral wall of the maxillary sinus. A bony window is produced utilizing either a round bur or piezotome to expose the Schneiderian membrane. The membrane is carefully detached from the walls of the maxillary antrum creating a void for augmentation. The grafting material is firmly inserted in the cavity and subsequently the deflected mucoperiosteum flap closes the sinus window. Several approaches involve classification and treatment of membrane tearing as well as adaptations to the closure of the sinus and the time point of implantation [7-10]. Today the CSFE presents a clinically successful technique that offers good insight into the sinus cavity and the present changes in bone height [11]. However, these advantages involve a secondary surgery site when placing dental implants and thus hold several drawbacks such as the potential for infections [12], particularly in smokers [13]. To address these drawbacks Summers et al. 1994 described a crestal approach to elevate the Schneiderian membrane utilizing tapered osteotomes with increasing diameters [14]. The basic procedure involves a crestal incision at the planned implant site and a full-thickness flap that is prepared to expose the alveolar crest. The initial osteotomy is either created manually with osteotomes or by the use of a bur or a drill. The subsequent osteotomes are inserted into the initial osteotomy by hand pressure or gentle malleting until the residual bone height beneath the maxillary sinus floor is limited to about 2 mm. Simultaneously, the diameter of the osteomes is consecutively increased until the planned implant diameter is reached. The last used osteotome is reinserted and pushed upwards to fracture the sinus floor and raise the Schneiderian membrane. To minimize the risk of membrane perforation some clinicians use an inflatable device or fill the void with augmentation material prior fracturing the sinus wall [15].
Today, several modifications of the operational technique have been described [16,17] but in most cases implant insertion is performed simultaneously after the desired augmentation height is reached. Most authors make their decision whether to use a simultaneous or staged approach according to the amount of residual bone height [18-24]. The consensus for simultaneous implant placement in grafted bone is limited to a residual bone height of at least 4-5 mm. Contrary, recent studies indicated successful one-stage approaches with only 1 mm residual bone height [25,26]. Taken together, the osteotome technique may provide lower morbidity and operational time but requires greater residual bone height. Furthermore, the osteotome technique is associated with a higher possibility of membrane tearing, limited elevation of the sinus mucosa and fewer control of the operation field [11]. Apart from the different surgical approaches providing adequate structure for primary implant stability several additional parameters such as simultaneously or delayed implant placement, time of unloaded healing as well as the use of grafting materials or membranes significantly affect implant survival. The ideal graft material is described as a substance that will change into regular bone under functional loading without resorption and offers the ability to form new bone either osteoconductively or osteoinductively to enable the support of dental implants [24,27].
A broad variety of different grafting materials has been successfully applied in sinus augmentation, including autogenous bone, allografts, xenografts and alloplasts. Autogenous bone is highly osteogenic, provides osteoprogenitor cells, disposes osteoinductive factors [23,24,28-30], and can be harvested from various donor sites (i.e. ilium, symphysis, mandibular ramus). Still, it was shown that autogenous bone is prone to high resorption [27,31], with up to 49.5% of bone loss after six months [32]. Additionally, the use of autogenous bone usually involves a second surgery site with the potential of donor site morbidity [24,27,28,30,32-34]. Allografts such as demineralized freeze-dried bone (DFDBA) avoid a second surgical site and exhibit osteoinductive and osteoconductive properties [28,35,36]. However, it was stated that DFDBA generates unpredictable bone formation with newly-formed bone of low quality and quantity [27,34,37]. The use of xenografts such as bovine bone mineral [38] and alloplasts such as hydroxyapatite [39] alone or in combination with autogenous bone, has increased over the past decade. Suchlike bone substitute materials vary in porosity and structure (particular pieces or blocks). Supplementary, some clinicians apply resorbable or non-resorbable membranes to shield the augmented area and prevent soft tissue encleftation. Thus, membranes may provide guided bone regeneration (GBR) and increase the amount of newly-formed bone [22,40,41]. On the other hand membranes may result in lower vascular supply to the graft, increased risk of infection [42], and additional cost. Furthermore, non-resorbable membranes need to be removed in a second surgery [40]. Peleg stated in 1999, that particulated grafts, which contain autogenous bone, heal faster and implants can be placed earlier [43]. Other authors [33,44] reported about a more favourable result for the use of xenografts. More recent investigations found similar survival rates for autogenous bone and bone substitutes [23,31] or stated that autogenous bone is still the gold standard [45]. Although sinus augmentation has become a frequently used and clinically successful technique the review of clinical investigations on sinus augmentation is inconsistent and often confounding [46]. Aghaloo and Moy 2007 stated that variations in the selection of patients, the surgical procedures as well as the surgeons skill-level account for the low clinical evidence. Consequently, the aim of this meta-analysis was to detect the predictability of sinus augmentation on the basis of implant survival and to compare the impact of the various treatment modalities. Particular attention was given to the influence of the surgical approach, residual bone height, the type of implant, its surface and placement, the grafting material and the use of membranes to provide clinical evidence for prospective treatment regimes.
Materials and Methods
A MEDLINE (Ovid) search was conducted for articles published from 1980 up to January 2013. The Cochrane Register of Controlled Trials, the Database of Abstracts of Effects, and the Cochrane Database of Systematic Reviews were also electronically searched. The search terms ‘sinus’, ‘sinus floor’, ‘maxillary sinus’, ‘maxillary sinus floor’, ‘maxillary antrum’, AND ‘elevation’, ‘augmentation’, ‘graft’, ‘lift’, ‘bone transplant’, ‘bone graft’, ‘bone remodel’, ‘alveolar ridge augmentation’, AND ‘dental implant, ‘endosseous implant’, were combined with the text words ‘sinus floor elevation’, ‘sinus floor augment’, ‘sinus floor graft’, ‘sinus floor lift’, ‘sinus elevation’, ‘sinus augment’, ‘sinus graft’, and ‘sinus lift’. Limits were set to human trials. The meta-analysis was conducted according to PRISMA guidelines and the methods of the analysis and inclusion criteria were specified in advance by the reviewers and documented in a protocol (Checklist S1). The initial criteria were not subjected to any alterations throughout the study:
-
1
Clinical report
-
2
No abstract publications
-
3
Studies in English and German
-
4
Absence of multiple interventions
-
5
Root-form implants
-
6
Minimum of 6 months follow up after implant loading
-
7
Minimum of 10 patients
-
8
Implant success/survival either clearly reported or calculable
Study selection and data extraction was performed by three independent reviewers. Uncertainties were discussed among the authors.
Information was extracted from each included trial on: (1) publication year, (2) study type (including case series, case control studies, cohort studies and randomized controlled trials), (3) implant form (screw versus pressfit), (4) implant surface (rough versus machined), (5) graft material (including autogenous bone; or bone substitute; or a combination of these two; or no graft at all), (6) the use of a membrane or not, (7) placement of the implants (one-stage versus two-stage), (8) residual bone height (9), unloaded healing time of the implants (10), surgical technique (lateral window versus transcrestal approach), and (11) type of outcome measure (survival versus success criteria). The authors of 78 studies were contacted by mail to clarify missing, insufficient, inadequate or controversial data. Studies with continuous unclear or incomplete data were excluded.
Statistical analysis
Numerical analysis was done, and plots and tables were generated with R. [47] The number of surviving implants at fixed intervals up to 8 years post-implantation had been entered in an Excel (Microsoft) spread sheet. Since the exact event times were not known, the events were considered interval-censored for lost implants, and right-censored for surviving implants. For interval-censored data, it is assumed that the probability of dropout in the interval is a smooth function over the time spanned by two consecutive visits. To follow intention-to-treat principles, implant loss during surgery was coded as uncensored loss on day 1 after implant. Non-parametric univariate Kaplan-Meier analysis was done with the R package interval [48]. Multivariate analysis used a Bayesian approach as implemented in package dynsurv [49] to separate the effect of publication from that of the implantation methods. The results are given as log-hazard ratios (HR) relative to a median baseline hazard. Forest plots summarizing the results of meta-analysis were created with package meta [50]. Because survival data were available for only few of the possible combinations of the parameters, strong priors were used to stabilize Bayesian posteriors. For the log-hazard coefficients, the prior had a mean of 0 and a standard deviation of 0.3; for the lambda coefficients defining the baseline hazard, a gamma distribution with shape = 6 and rate = 10 was chosen. Base levels and all pairwise interactions of parameters Membrane, Approach and Implant were used as predictors in the multivariate Bayes model; for the 4 levels of the graft material (GraftMat), no interactions were included because too few combinations were known. In addition for each publication a relative log hazard was estimated, to correct the estimation of the method hazard for study specific effects. In terms of the R-programming language, the following model formula was used:
Means and 95%-confidence intervals of log-hazards were computed from 30000 MCMC samples after 3000 burn-in samples; a typical model run required 5 hours of computing time [50]. In practice, the natural logarithm of the hazard ratio is a more useful measure and was used throughout this paper. Positive log hazard ratios stand for steeper survival curves and shorter survival time.
Results
The electronic search provided a total of 1960 duplicate adjusted citations. Of these, 1682 were discarded because after reviewing the abstracts it appeared that these papers clearly did not meet the inclusion criteria. The full text of the remaining 278 citations was examined in more detail. It appeared that 156 studies did not meet the inclusion criteria as described. 122 studies met the inclusion criteria and were included in the systematic review.
A total of 122 publications on 16268 endosseous implants placed in grafted maxillary sinus covering publication years 1993 to 2012 were shortlisted for meta-analysis (Figure 1). The implant parameter descriptors were extracted from the publications (Table 1). In case a publication reported data from multiple methods, results were subdivided into References disambiguated by appending _a, _b or _c (table 2) and further itemized (Table 3). The included publications showed a marked annually increase in number of studies and implants after the year 2004. Follow-up time for most publications was 1 year, with only one study investigating 11 years follow-up time [51]. Information on parameters Approach, StudyType, Placement and GraftMat is available for all publications. In a preliminary one-factorial analysis, parameters StudyType and Placement showed to have no predictive value and were therefore omitted. Since only 4% of the applied implant surfaces were machined, parameter Surface was also omitted to avoid power reduction. Parameter BoneHeight was considered important, but was omitted after preliminary test showed its inclusion led to unstable estimates in the analysis. This may indicate for a selective bias in the choice of the surgical procedure chosen for the patients. Furthermore, the fact that inclusion of bone-height lead to destabilization of the numerical procedure is a likely indicator that this grouping leads to highly heterogenous combinations in correlating confounding factors.
Figure 1. PRISMA – Flow Diagram.
Table 1. Implant parameter descriptors.
| Parameter | Levels | Complete | Implants | Used |
|---|---|---|---|---|
| Approach | lateral_window, transcrestal | 138 | 16268 | Yes |
| StudyType | CT_RCT, RS_CS | 138 | 16268 | No |
| Placement | 1stage, 2stage, either | 138 | 16268 | No |
| GraftMat | autogenous, bone_substitute, either, combination, no_graft | 138 | 16268 | Yes |
| Membrane | membrane, no_membrane | 132 | 14766 | Yes |
| Implant | either, pressfit, screw | 124 | 11974 | Yes |
| Surface | either, machined, rough | 117 | 11674 | No |
| BoneHeight | lesser_5mm, greater_5mm | 100 | 10451 | No |
The table shows the different implant parameter discriptors. Approach describes the use of either lateral window or transcrestal approach; StudyType categorizes the studies into two groups: high quality studies represented by randomized control trials (RCT) and clinical trials (CT) and studies of low quality such as case series (CS) and retrospective studies (RS). Placement evaluates the time point of implantation. GraftMat analyses possible application and type of grafting material (either: bone substitute or autogenous bone; combination: bone substitute and autogenous bone. Distribution is shown in Table 2, Special). Membrane differentiates studies using membranes from nonusers. Implant and Surface classify the type of implant and its surface and BoneHeight classifies the studies with bone height of less or more than 5mm residual bone prior implantation. The column Used describes the use of predictive parameter in modelling.
Table 2. Publications and references included in meta-analysis.
| Short_Pub | Year | Reference / n Implants | Publication | Special |
|---|---|---|---|---|
| acocella | 2011 | (3, n=31) | Acocella et al. | |
| agamy | 2010 | (10, n=47) | Agamy et al. | |
| anitua | 2009 | (3, n=43) | Anitua et al. | |
| bae | 2010 | (5, n=32) | Bae et al. | |
| barone08 | 2008 | (24, n=12) | Barone et al. | |
| barone11 | 2011 | (5, n=201) | Barone et al. | |
| bassil | 2011 | (3, n=49) | Bassil et al. | |
| bergh | 1998 | (4, n=161) | Van den Bergh et al. | |
| bernardello | 2011 | (11, n=134) | Bernardello et al. | |
| blus | 2008 | (12, n=117) | Blus et al. | |
| bornstein | 2008 | (5, n=111) | Bornstein et al. | |
| bystedt | 2009 | (3, n=23) | Bystedt et al. | |
| canniza | 2007 | a (19, n=52), b (19, n=52) | Cannizzaro et al. | |
| canniza09 | 2009 | a (5, n=44), b (6, n=38) | Cannizzaro et al. | |
| canullo | 2012 | (3, n=67) | Canullo et al. | |
| caubet | 2011 | (5, n=65) | Caubet et al. | |
| chaushu | 2009 | (2, n=72) | Chaushu et al. | |
| chen | 2007 | (9, n=47) | Chen et al. | |
| coatoam | 1997 | (20, n=85) | Coatoam et al. | Implant: 71 screw, 18 pressfit |
| cordioli | 2001 | (5, n=27) | Cordioli et al. | |
| crespi | 2010 | (13, n=30) | Crespi et al. | |
| cricchio | 2011 | (9, n=189) | Cricchio et al. | |
| dasmah | 2012 | (2, n=40) | Dasmah et al. | |
| deporter00 | 2000 | (16, n=26) | Deporter et al. | |
| deporter05 | 2005 | (16, n=103) | Deporter et al. | |
| diss | 2008 | (24, n=35) | Diss et al. | |
| engelke | 2001 | (7, n=44) | Engelke | |
| esposito | 2011 | (2, n=38) | Esposito et al. | |
| fermergard | 2012 | (10, n=53) | Fermergard et al. | |
| ferrigno | 2006 | (6, n=587) | Ferrigno et al. | Graftmat: almost all autogenous, very rarely combination |
| fugazot02 | 2002 | (13, n=137) | Fugazzotto et al. | |
| fugazot202 | 2002 | (21, n=83) | Fugazotto et al. | |
| galindo07 | 2007 | (5, n=263) | Galindo-Moreno et al. | |
| galindo10 | 2010 | (5, n=45) | Galindo-Moreno et al. | |
| guerrero | 2012 | (2, n=84) | Guerrero et al. | |
| hallman | 2002 | (7, n=74) | Hallman et al. | |
| hansen | 2011 | (12, n=58) | Hansen et al. | Graftmat: 29 autogenous, 29 combination |
| heinemann | 2009 | (2, n=37) | Heinemann et al. | |
| herzberg | 2006 | (14, n=203) | Herzberg et al. | Graftmat: 48 autogenous, 13 bone_substitute, 151 combination |
| hu | 2009 | (13, n=25) | Hu et al. | |
| irinakis | 2011 | (2, n=49) | Irinakis et al. | |
| johansso10 | 2010 | (4, n=81) | Johansson et al. (B) | |
| johansso99 | 1999 | (4, n=110) | Johansson et al. (LA) | |
| jurisic | 2008 | a (3, n=15), b (3, n=25), c (13, n=40) | Jurisic et al. | |
| kahnberg01 | 2001 | (4, n=71) | Kahnberg et al. | |
| kahnberg08 | 2008 | (4, n=153) | Kahnberg et al. | |
| kahnberg11 | 2011 | (4, n=20) | Kahnberg et al. | |
| kaneko | 2012 | (9, n=21) | Kaneko et al. | |
| keller | 1994 | (4, n=65) | Keller et al. | |
| kermalli | 2008 | b (16, n=29), c (13, n=28) | Kermalli et al. | |
| kim | 2011 | (2, n=35) | Kim et al. | |
| krenmair | 2007 | a (5, n=28), b (5, n=12), c (13, n=14) | Krennmair et al. | |
| krenmair08 | 2008 | (7, n=79) | Krennmair et al. | |
| lambert | 2010 | (2, n=102) | Lambert et al. | |
| lambrecht | 2003 | (12, n=36) | Lambrecht et al. | |
| leblebicio | 2005 | (10, n=73) | Leblebicioglu et al. | |
| lee | 2008 | (7, n=97) | Lee et al. (CY) | |
| leechen | 2012 | (2, n=12) | Lee et al. (DZ) | |
| leick | 2005 | (2, n=300) | Leick et al. | |
| lin | 2011 | (9, n=80) | Lin et al. | |
| lindgren | 2012 | (2, n=47) | Lindgren et al. | |
| lundgren | 2004 | (9, n=19) | Lundgren et al. | |
| maioran00 | 2000 | (7, n=30) | Maiorano et al. | |
| maioran05 | 2005 | (2, n=36) | Maiorano et al. | |
| mangano03 | 2003 | (3, n=28) | Mangano et al. | |
| mangano07 | 2007 | (3, n=100) | Mangano et al. | |
| marchet | 2007 | a (7, n=32), b (7, n=108) | Marchetti et al. | |
| markovic | 2011 | (10, n=40) | Markovic et al. | |
| mazor00 | 2000 | (25, n=26) | Mazor et al. | |
| mazor99 | 1999 | (8, n=10) | Mazor et al. | |
| minichetti | 2008 | (2, n=136) | Minichetti et al. | |
| nedir | 2010 | (10, n=24) | Nedir et al. | |
| peleg06 | 2006 | (1, n=2117) | Peleg et al. | Implant: 1374 screw, 758 pressfit |
| peleg98 | 1998 | (8, n=55) | Peleg et al. | |
| peleg99 | 1999 | (8, n=160) | Peleg et al. | |
| pelegetal | 1999 | (8, n=57) | Peleg et al. | |
| pieri | 2012 | (5, n=90) | Pieri et al. | |
| pjetursson | 2009 | (11, n=252) | Pjetursson et al. | Graftmat: 35% bone_substitute, 65% no_graft |
| rodriguez | 2003 | (23, n=70) | Rodriguez et al. | |
| sakka | 2011 | (15, n=77) | Sakka et al. | |
| sbord11 | 2011 | a (15, n=136), b (2, n=146) | Sbordone et al. | |
| scarano | 2010 | (3, n=264) | Scarano et al. | |
| schleier06 | 2006 | (10, n=49) | Schleier et al. | |
| schleier08 | 2008 | (10, n=59) | Schleier et al. | |
| sforza | 2008 | (22, n=39) | Sforza et al. | |
| siervo | 2004 | (7, n=72) | Siervo et al. | |
| simonpieri | 2011 | (2, n=52) | Simonpieri et al. | |
| sohn | 2011 | (18, n=113) | Sohn et al. | Implant: 109 screw, 4 pressfit |
| stavropoul | 2007 | (22, n=33) | Stavropoulos et al. | |
| stricker | 2003 | (4, n=180) | Stricker et al. | |
| sungcho | 2008 | (12, n=130) | Lee et al. (JH) | |
| thor | 2007 | (9, n=44) | Thor et al. | |
| torres | 2009 | a (3, n=153), b (3, n=129) | Torres et al. | |
| vicente | 2010 | a (5, n=22), b (5, n=68) | De Vicente et al. | |
| viscioni | 2010 | (3, n=64) | Viscioni et al. | |
| voss | 2010 | a (4, n=118), b (3, n=168) | Voss et al. | |
| wannfors | 2000 | (4, n=132) | Wannfors et al. | |
| watzek | 1998 | (17, n=142) | Watzek et al. | Graftmat: 49 autogenous, 16 bone_substitute, 70 combination |
| winter | 2002 | (10, n=54) | Winter et al. | |
| yamada | 2008 | (3, n=41) | Yamada et al. | |
| yamamich | 2008 | (2, n=159) | Yamamichi et al. | |
| zetterqvis | 2004 | (7, n=64) | Hallman et al. | |
| zijderveld | 2005 | (14, n=41) | Zijderveld et al. | Graftmat: 15 autogenous, 26 bone_substitute |
| zinner | 1996 | (8, n=212) | Zinner et al. | |
| zitzman | 1998 | a (2, n=7), b (2, n=13) | Zitzmann et al. | |
| zitzmann98 | 1998 | (6, n=57) | Zitzmann et al. |
The table shows the publications and the according references used in this meta-analysis (Table S1). In column Reference, the first number in brackets refers to the row number (Combination) in table 3 that gives the combination of parameters for this reference. In case of multiple references in one publication, marker letters a, b, c were added, e.g the study Cannizzaro et al. has references to 2 combinations a and b which both happen to refer to row 19 in table 3 because they only differ by parameter Placement which is not used in this meta-analysis. Publications with simplifiying assumptions due to incomplete information are specified in column Special.
Table 3. Combinations of parameters.
| Combination | Membrane | Approach | Implant | GraftMat | n |
|---|---|---|---|---|---|
| 1 | membrane | lateral_window | either | either | 2117 |
| 2 | membrane | lateral_window | screw | bone_substitute | 1365 |
| 3 | no_membrane | lateral_window | screw | bone_substitute | 1150 |
| 4 | no_membrane | lateral_window | screw | autogenous | 1141 |
| 5 | membrane | lateral_window | screw | combination | 1008 |
| 6 | no_membrane | transcrestal | screw | autogenous | 682 |
| 7 | no_membrane | lateral_window | screw | combination | 600 |
| 8 | membrane | lateral_window | pressfit | combination | 494 |
| 9 | no_membrane | lateral_window | screw | no_graft | 400 |
| 10 | no_membrane | transcrestal | screw | no_graft | 399 |
| 11 | no_membrane | transcrestal | screw | either | 386 |
| 12 | membrane | lateral_window | screw | either | 341 |
| 13 | no_membrane | transcrestal | screw | bone_substitute | 275 |
| 14 | no_membrane | lateral_window | screw | either | 244 |
| 15 | membrane | lateral_window | screw | autogenous | 213 |
| 16 | no_membrane | transcrestal | pressfit | bone_substitute | 157 |
| 17 | no_membrane | lateral_window | pressfit | either | 142 |
| 18 | no_membrane | lateral_window | either | bone_substitute | 113 |
| 19 | membrane | lateral_window | pressfit | autogenous | 104 |
| 20 | no_membrane | transcrestal | either | combination | 85 |
| 21 | membrane | transcrestal | screw | autogenous | 83 |
| 22 | no_membrane | transcrestal | screw | combination | 72 |
| 23 | no_membrane | lateral_window | pressfit | bone_substitute | 70 |
| 24 | membrane | transcrestal | screw | bone_substitute | 47 |
| 25 | membrane | lateral_window | pressfit | bone_substitute | 26 |
The table shows the combination of parameters used in meta-analysis and the number of implants for each case, sorted by number of implants descending. Column Combination is referenced from column Reference in table 2.
A final set of 106 publications, with 119 references (i.e. groups with distinct treatments within publications) and 11714 implants was included in this meta-analysis (Table 2).
Univariate Kaplan-Meier analysis
Kaplan-Meier plots for interval-censored data were grouped by the use of membranes (Figure 2). The gray bars show regions of indetermination from the maximum likelihood estimation of interval-censored data [52]. The prolonged implant survival for the membrane-group is highly significant (p=0.002). However, the univariate analysis is misleading and given here as an illustration only, because it assumes that other factors were kept constant or at least do not co-vary strongly with the use of membranes. To correct for such correlations, a multivariate analysis was performed.
Figure 2. Univariate Kaplan-Meier analysis plots for interval-censored data and subset of publications used in this meta-analysis.
The gray bars show regions of indetermination from the maximum likelihood estimation of interval-censored data (Turnbull, 1976).
Multivariate interval-censored Cox regression
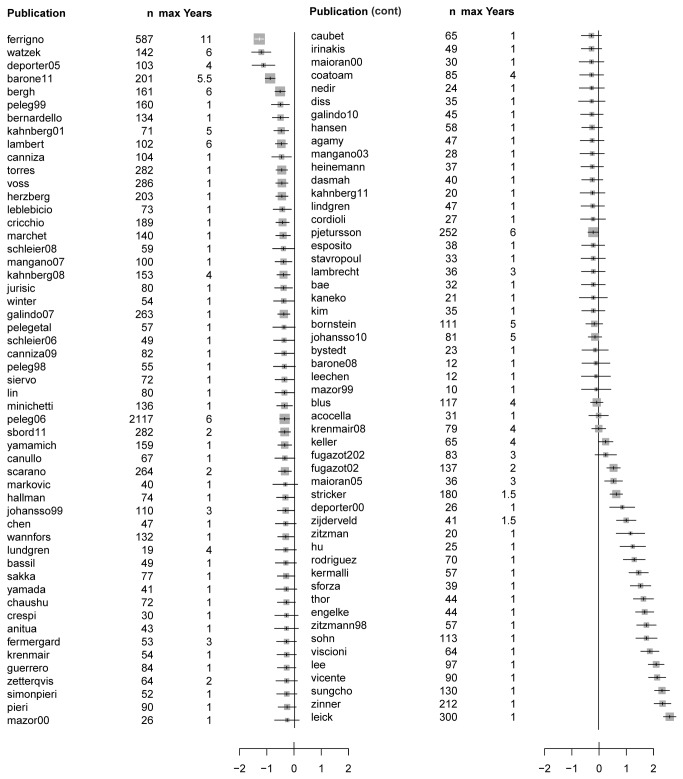
The effects of the different study groups were factored giving log hazard ratios for all publications in this meta-analysis (Figure 3). To conserve the power of planned cross-over studies, the figures do not use the references to subgroups, i.e. when two treatment combinations are reported in one publication, they are combined. The baseline-hazard was computed over the range of up to 6 years after implantation; since most studies have follow-up times of 1 year, the modelling algorithm has to make assumptions about the future survival for short records. This leads to extreme hazard ratios for the publications with short follow-up times that occur at the bottom of the list; studies with long follow-up times have smaller hazard ratios.
Figure 3. Forest plot of log hazard ratio with 95% confidence intervals for publications in meta-analysis.
n: number of implants, max Years: maximal follow-up time.
Method effect
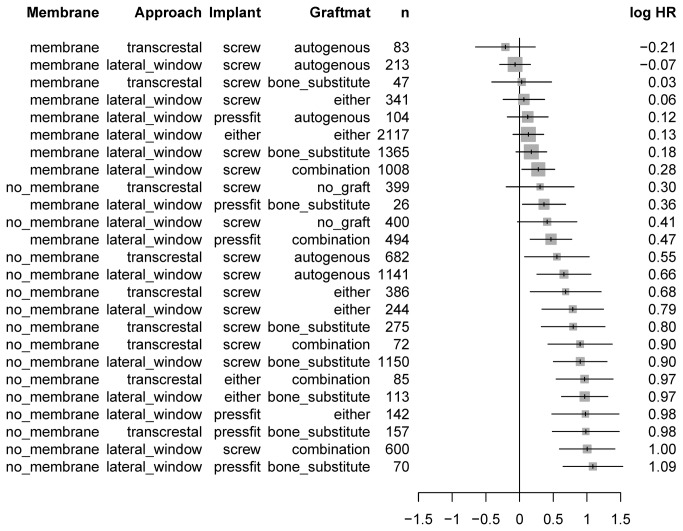
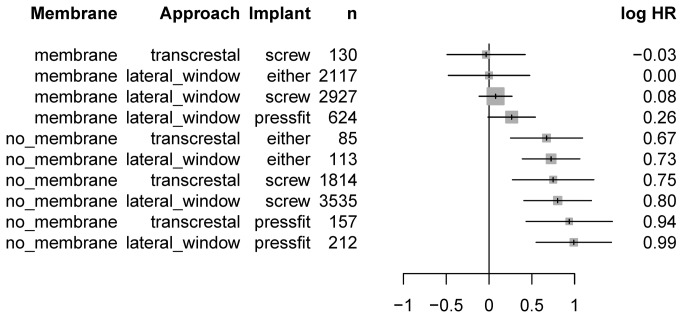
Results ranged from -0.21 to 1.09 of the logarithmic hazard ratio, from best to worst, which corresponds to a range of the hazard ratio of 3.7 (Figure 4). The most evident feature was the clustering of methods with membrane at the top of the list. The arrangement of the four levels of grafting material (GraftMat) was effectively random. To clarify the overall picture, the model was recomputed by excluding this parameter entirely (Figure 5). This simplified model corroborated that solely combinations including membranes remained at the top of the list. Furthermore, a strong increase in the hazard ratio of the no_membrane block from 0.26 to 0.67 was observed. Even in the simplified model, there was no evidence for any preference for parameters Approach and Implant.
Figure 4. Forest plot of logarithmic hazard ratios (HR) and their 95%-confidence intervals for all method combinations.
n: number of implants. Low values at the top represent longer implant survival.
Figure 5. Log hazard ratios (HR) and their 95%-confidence intervals, with simplified model omitting parameter GraftMat.
Absolute values of HR should not be compared with those in Figure 4 because reference values or HR are not comparable. n: number of implants.
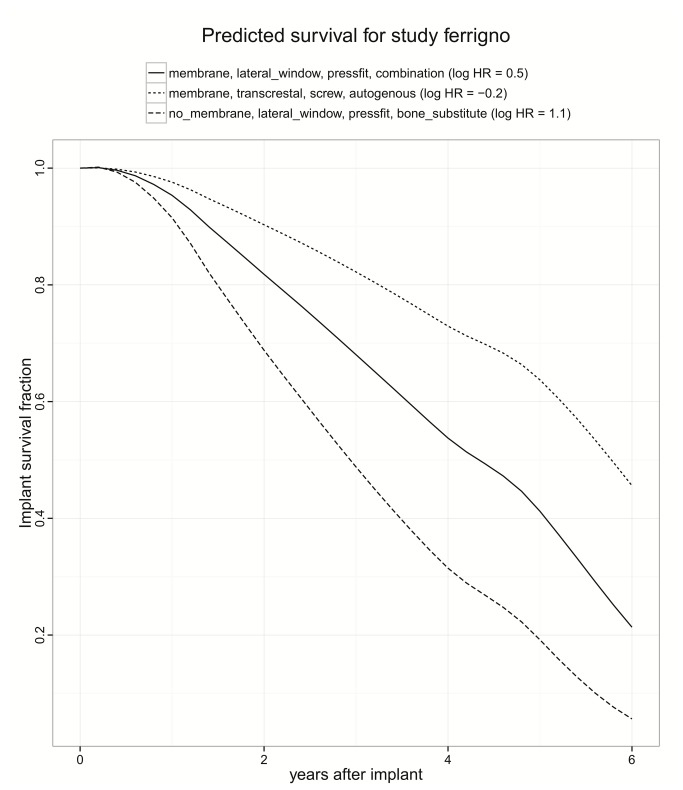
Hazard functions
To illustrate survival curves, three samples are shown, covering the range from smallest to larges hazard ratio (Figure 6). The curves are similar, and less extreme than the mono-variable survival plot; this is a feature of the Cox regression, where only one number, the hazard ratio, determines the degree of stretching. Note that this is not an average curve, but a hypothetical prediction for one study with long observation time; giving a population average is not meaningful for studies with a large range. The Cox model might be wrong in some aspects, but the simplifications are the precondition for a successful covariate analysis. However, because of the scarcity of data for post-implantation follow-up visits after 3 years, it is questionably if the change in slope after three years is real or biased by selective dropouts of studies.
Figure 6. Three samples of implant survival curves, estimated from a Cox regression model for interval-censored data.
The curves are similar, and less extreme than the mono-variable survival plot; this is a feature of the Cox regression, where only the hazard ratio determines the degree of stretching. Note that this is not an average curve, but a hypothetical prediction for one study with long observation time.
Discussion
To date, the influence of treatment modalities on survival and success rates of endosseous implants placed in the grafted maxillary sinus is not yet deciphered [6,17,53]. Accordingly, evidence-based decision-making on how to treat the patient at best possible conditions is still impaired. To address this problem the present systematic review and meta-analysis investigated the role of different factor combinations and associated reciprocal effects in sinus augmentation and successful implantation procedures. Previous meta-analyses were substantially affected by the inconsistency of study designs. Concurrently causative unsuitable statistical analysis accounted for the low clinical evidence [54,55]. Statistical methods such as multivariable Poisson regression, life table modelling and basic univariate Kaplan-Meier Analysis are a commonly used to assess implant survival and success rates. Still, this type of analysis does not take the influence of other factors or covariables such as study effects into account. To cite an example, the preliminary conducted univariate analysis on implant success indicated, in concert with recent investigations [6], that the use of membranes is highly significant. However, if membranes would be preferably used in combination with screws and autogenous material, and non-membranes preferably with press-fit implants, and bone-substitute materials the difference between the membrane groups could equally well be attributed to the effect of the implant and the graft material. Hence, meta-analysis must correct for study effects to obtain publication-independent estimates of method effects.
To address such study effects our analytical approach was to conduct survival analysis using multivariate interval-censored Cox regression to specifically analyse method effects and corresponding hazard ratios. This modelling could correct for the fact that studies with only 25 of the 32 possible combinations were available, and that some combinations were represented only by one study. In Cox-regression [56], first a common non-parametric baseline survival curve is estimated; for each combination of parameters, only one parameter, the hazard ratio, quantifies how the survival curve is stretched or compressed compared to the baseline curve [57]. The applied Cox model is a simplification and, for example, does not allow for the crossing of survival curves. Still, simplification is the precondition for a successful covariate analysis that enables the estimation of covariable effects when not all combinations are known, which was impossible under the more general Kaplan-Meier assumption. To illustrate the basic (baseline) log hazard ratio of implant survival for each publication the different methods have been factored out to correct for study effects. Accordingly, the presented hazard ratios should be recognized as a correction to the hazard one would expect from the methods used in the publication. For example, if success with all methods improved over time, this would lead to lower hazards in more recent publications, and by including the study as a covariable in the analysis one would implicitly correct for this trend.
Notably, the total number of implants investigated in the publications had no direct effect on the basic (baseline) log hazard ratio, whereas, follow-up time of each publication emerged to be the most prominent factor. This may advocate for a prolonged follow-up time to safely assess valid implant survival in consideration of co-factors [17] such as technical complications with supra-constructions, especially screw or abutment loosening [58], marginal bone loss [59], smoking or oral hygiene [60,61]. However, the time frame of one year follow-up is prevalently used to assess implant success, predominantly the effective osseointegration of the implant irrespective of the type of functional loading [62-64]. Implant loss in the first year was found low, consequently the main information was obtained from the few studies with follow-up time between 2 years and 7 years; this selective drop-out is the most critical factor affecting the reliability of the results of this meta-analysis. Taken together it is advisable to avoid rating the quality of individual studies, but rather to consider inclusion of study effects as an overall compensation to factor out random study variations from method effects.
To decipher the hazard ratio for all methods combinations, as predicted from a model that corrects for the publication effect, was the primary endpoint of this meta-analysis. Results showed a pronounced clustering of methods that included membranes at the top of the list. None of the other columns exhibited such an asymmetry in distribution. This highlights the paramount importance of the use of membranes, independent of other details and corroborates the finding of the simpler univariate Kaplan Meier analysis. Moreover, this meta-analysis revealed a notable step in the hazard ratio between the membrane and the no_membrane group from 0.26 to 0.67, presenting an even stronger indicator of the fact that the use of membranes creates a different league. Interestingly, the arrangement of the four levels of grafting material (GraftMat) was effectively random and thus the model was recomputed excluding this parameter entirely. In this simplified model combinations using membranes were still completely at the top. Furthermore, there was no evidence for any preference for parameters Approach and Implant. Moreover, the treatment parameters surgical approach, grafting material, and implant type showed no selective preference. Recent investigations concluded similar results with the prognosis of implants unaffected by the type of graft material, residual bone height and time of implant placement [65]. Other investigations advocated that the use of autogenous bone, rough and screw-type implants as well as membranes exhibit favourable results [6]. However, combinations of solely 2 factors were statistically admissible within the limitations of life table modelling. In comparison, implant survival curves, estimated from the present Cox regression model for interval-censored data, showed the lowest hazard ratio for the combination of membrane, screw-type implant, transcrestal approach, and autogenous bone. Yet, data were interval censored and the time of event only known to be within a given range determined by the inter-visit interval. However, because of the scarcity of data for post-implantation follow-up visits after 3 years, it is questionably if the change in slope after three years is real or biased by selective dropouts of studies. In summary, with randomized designs being ethically unacceptable more complete information from split-mouth designs is crucial to negotiate prospective confounding and further improve clinical evidence.
Conclusion
Other than conventional statistical methods the Bayesian multivariate interval-censored Cox regression helps to take covariables such as study effects into account. While the present meta-analysis does not give evidence for any significant method effect besides that of membrane application, this dominance should be interpreted in the light of the correction for study-group effects factored out in the meta-analysis. It cannot be excluded that other factors in use by a team experienced with this combination might still be relevant for implant survival, because team and method effects are confounded. Consequently, more studies on follow-up visits exceeding 3 years are needed to address confounding and improve clinical evidence. Nevertheless, dominance of the membrane effect means that membranes extent implant survival independently of the surgeons’ special preferences and skills and thus may improve future decision-making in dento-maxillary rehabilitation.
Supporting Information
PRISMA Checklist. The PRISMA Checklist documents the methods of analysis and inclusion criteria that were specified in advance by the reviewers according to PRISMA guidelines.
(DOC)
Reference appendix. The table documents the full reference for the abbreviated publications listed in table 2.
(DOCX)
Acknowledgments
The authors are indebted to the help of Dr. Mareike Bösch during the collection of data and to the head of the department for oral- and maxillofacial surgery, university of Freiburg Professor Dr. Rainer Schmelzeisen for providing the necessary workstations.
Funding Statement
The authors have no support or funding to report.
References
- 1. Weyant RJ, Pandav RS, Plowman JL, Ganguli M (2004) Medical and cognitive correlates of denture wearing in older community-dwelling adults. J Am Geriatr Soc 52: 596–600. doi:10.1111/j.1532-5415.2004.52168.x. PubMed: 15066077. [DOI] [PubMed] [Google Scholar]
- 2. Yu Y-H, Lai Y-L, Cheung WS, Kuo H-K (2011) Oral health status and self-reported functional dependence in community-dwelling older adults. J Am Geriatr Soc 59: 519–523. doi:10.1111/j.1532-5415.2010.03311.x. PubMed: 21391942. [DOI] [PubMed] [Google Scholar]
- 3. Vogel R, Smith-Palmer J, Valentine W (2013) Evaluating the health economic implications and cost-effectiveness of dental implants: a literature review. Int J Oral Maxillofac Implants 28: 343–356. doi:10.11607/jomi.2921. PubMed: 23527335. [DOI] [PubMed] [Google Scholar]
- 4. Tatum H (1986) Maxillary and sinus implant reconstructions. Dent Clin North Am 30: 207–229. PubMed: 3516738. [PubMed] [Google Scholar]
- 5. Smiler DG (1997) The sinus lift graft: basic technique and variations. Pract Periodontics Aesthet Dent 9: 885–895. PubMed: 9573843. [PubMed] [Google Scholar]
- 6. Pjetursson BE, Tan WC, Zwahlen M, Lang NP (2008) A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol 35: 216–240. doi:10.1111/j.1600-051X.2008.01272.x. PubMed: 18724852. [DOI] [PubMed] [Google Scholar]
- 7. Vlassis JM, Fugazzotto PA (1999) A classification system for sinus membrane perforations during augmentation procedures with options for repair. J Periodontol 70: 692–699. doi:10.1902/jop.1999.70.6.692. PubMed: 10397526. [DOI] [PubMed] [Google Scholar]
- 8. Ardekian L, Oved-Peleg E, Mactei EE, Peled M (2006) The clinical significance of sinus membrane perforation during augmentation of the maxillary sinus. YJOMS 64: 277–282. PubMed: 16413901. [DOI] [PubMed] [Google Scholar]
- 9. Mardinger O, Nissan J, Chaushu G (2007) Sinus floor augmentation with simultaneous implant placement in the severely atrophic maxilla: technical problems and complications. J Periodontol 78: 1872–1877. doi:10.1902/jop.2007.070175. PubMed: 18062109. [DOI] [PubMed] [Google Scholar]
- 10. Timmenga NM, Raghoebar GM, Boering G, van Weissenbruch R (1997) Maxillary sinus function after sinus lifts for the insertion of dental implants. YJOMS 55: 936–940. PubMed: 9294502. [DOI] [PubMed] [Google Scholar]
- 11. Chiapasco M, Ronchi P (1994) Sinus lift and endosseous implants--preliminary surgical and prosthetic results. Eur J Prosthodont Restor Dent 3: 15–21. PubMed: 8603146. [PubMed] [Google Scholar]
- 12. Schwartz-Arad D, Herzberg R, Dolev E (2004) The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol 75: 511–516. doi:10.1902/jop.2004.75.4.511. PubMed: 15152813. [DOI] [PubMed] [Google Scholar]
- 13. Barone A, Santini S, Sbordone L, Crespi R, Covani U (2006) A clinical study of the outcomes and complications associated with maxillary sinus augmentation. Int J Oral Maxillofac Implants 21: 81–85. PubMed: 16519185. [PubMed] [Google Scholar]
- 14. Summers RB (1994) A new concept in maxillary implant surgery: the osteotome technique. Compendium 15: 152–162. PubMed: 8055503. [PubMed] [Google Scholar]
- 15. Stelzle F, Benner K-U (2011) Evaluation of different methods of indirect sinus floor elevation for elevation heights of 10mm: an experimental ex vivo study. Clin Implant Dent Relat Res 13: 124–133. doi:10.1111/j.1708-8208.2009.00190.x. PubMed: 19681924. [DOI] [PubMed] [Google Scholar]
- 16. Chen L, Cha J (2005) An 8-year retrospective study: 1,100 patients receiving 1,557 implants using the minimally invasive hydraulic sinus condensing technique. J Periodontol 76: 482–491. doi:10.1902/jop.2005.76.3.482. PubMed: 15857085. [DOI] [PubMed] [Google Scholar]
- 17. Tan WC, Lang NP, Zwahlen M, Pjetursson BE (2008) A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevationPart II: Transalveolar technique. J Clin Periodontol 35: 241–254. doi:10.1111/j.1600-051X.2008.01273.x. PubMed: 18724853. [DOI] [PubMed] [Google Scholar]
- 18. Shlomi B, Horowitz I, Kahn A, Dobriyan A, Chaushu G (2004) The effect of sinus membrane perforation and repair with Lambone on the outcome of maxillary sinus floor augmentation: a radiographic assessment. Int J Oral Maxillofac Implants 19: 559–562. PubMed: 15346754. [PubMed] [Google Scholar]
- 19. Valentini P, Abensur DJ (2003) Maxillary sinus grafting with anorganic bovine bone: a clinical report of long-term results. Int J Oral Maxillofac Implants 18: 556–560. PubMed: 12939008. [PubMed] [Google Scholar]
- 20. Stricker A, Voss PJ, Gutwald R, Schramm A, Schmelzeisen R (2003) Maxillary sinus floor augmention with autogenous bone grafts to enable placement of SLA-surfaced implants: preliminary results after 15-40 months. Clin Oral Implants Res 14: 207–212. doi:10.1034/j.1600-0501.2003.140211.x. PubMed: 12656881. [DOI] [PubMed] [Google Scholar]
- 21. Zitzmann NU, Schärer P (1998) Sinus elevation procedures in the resorbed posterior maxilla. Comparison Crestal And Lateral APproaches YMOE 85: 8–17. [DOI] [PubMed] [Google Scholar]
- 22. Strietzel FP (2004) Sinus floor elevation and augmentation. Evidence-based analysis of prognosis and risk factors. Mund Kiefer Gesichtschir 8: 93–105. doi:10.1007/s10006-004-0530-3. PubMed: 15045532. [DOI] [PubMed] [Google Scholar]
- 23. Del Fabbro M, Testori T, Francetti L, Weinstein R (2004) Systematic review of survival rates for implants placed in the grafted maxillary sinus. Int J Periodontics Restorative Dent 24: 565–577. PubMed: 15626319. [PubMed] [Google Scholar]
- 24. Smiler DG, Holmes RE (1987) Sinus lift procedure using porous hydroxyapatite: a preliminary clinical report. J Oral Implantol 13: 239–253. PubMed: 2855842. [PubMed] [Google Scholar]
- 25. Peleg M, Mazor Z, Chaushu G, Garg AK (1998) Sinus floor augmentation with simultaneous implant placement in the severely atrophic maxilla. J Periodontol 69: 1397–1403. doi:10.1902/jop.1998.69.12.1397. PubMed: 9926770. [DOI] [PubMed] [Google Scholar]
- 26. Winter AA, Pollack AS, Odrich RB (2002) Placement of implants in the severely atrophic posterior maxilla using localized management of the sinus floor: a preliminary study. Int J Oral Maxillofac Implants 17: 687–695. PubMed: 12381069. [PubMed] [Google Scholar]
- 27. Block MS, Kent JN (1997) Sinus augmentation for dental implants: the use of autogenous bone. YJOMS 55: 1281–1286. [DOI] [PubMed] [Google Scholar]
- 28. Tong DC, Rioux K, Drangsholt M, Beirne OR (1998) A review of survival rates for implants placed in grafted maxillary sinuses using meta-analysis. Int J Oral Maxillofac Implants 13. [PubMed] [Google Scholar]
- 29. Lindenmüller IH, Lambrecht JT (2006) [Sinus floor elevation and implantation--a retrospective study]. Schweiz Monatsschr Zahnmed 116: 142–149. PubMed: 16524217. [PubMed] [Google Scholar]
- 30. Guarnieri R, Grassi R, Ripari M, Pecora G (2006) Maxillary sinus augmentation using granular calcium sulfate (surgiplaster sinus): radiographic and histologic study at 2 years. Int J Periodontics Restorative Dent 26: 79–85. PubMed: 16515099. [PubMed] [Google Scholar]
- 31. Wallace SS, Froum SJ (2003) Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol 8: 328–343. doi:10.1902/annals.2003.8.1.328. PubMed: 14971260. [DOI] [PubMed] [Google Scholar]
- 32. Ewers R (2005) Maxilla sinus grafting with marine algae derived bone forming material: a clinical report of long-term results. YJOMS 63: 1712–1723. PubMed: 16297691. [DOI] [PubMed] [Google Scholar]
- 33. Hallman M, Sennerby L, Lundgren S (2002) A clinical and histologic evaluation of implant integration in the posterior maxilla after sinus floor augmentation with autogenous bone, bovine hydroxyapatite, or a 20:80 mixture. Int J Oral Maxillofac Implants 17: 635–643. PubMed: 12381063. [PubMed] [Google Scholar]
- 34. Valentini P, Abensur D (1997) Maxillary sinus floor elevation for implant placement with demineralized freeze-dried bone and bovine bone (Bio-Oss): a clinical study of 20 patients. Int J Periodontics Restorative Dent 17: 232–241. PubMed: 9497715. [PubMed] [Google Scholar]
- 35. Zinner ID, Small SA (1996) Sinus-lift graft: using the maxillary sinuses to support implants. J Am Dent Assoc 127: 51–57. PubMed: 8568098. [DOI] [PubMed] [Google Scholar]
- 36. Hallman M, Sennerby L, Zetterqvist L, Lundgren S (2005) A 3-year prospective follow-up study of implant-supported fixed prostheses in patients subjected to maxillary sinus floor augmentation with a 80:20 mixture of deproteinized bovine bone and autogenous bone Clinical, radiographic and resonance frequency analysis. Int J Oral Maxillofac Surg 34: 273–280. doi:10.1016/j.ijom.2004.09.009. PubMed: 15741036. [DOI] [PubMed] [Google Scholar]
- 37. Daelemans P, Hermans M, Godet F, Malevez C (1997) Autologous bone graft to augment the maxillary sinus in conjunction with immediate endosseous implants: a retrospective study up to 5 years. Int J Periodontics Restorative Dent 17: 27–39. PubMed: 10332251. [PubMed] [Google Scholar]
- 38. Sauerbier S, Rickert D, Gutwald R, Nagursky H, Oshima T et al. (2011) Bone Marrow Concentrate and Bovine Bone Mineral for Sinus Floor Augmentation: A Controlled, Randomized, Single-Blinded Clinical and Histological Trial-Per-Protocol Analysis. Tissue Eng A. [DOI] [PubMed] [Google Scholar]
- 39. Mangano C, Bartolucci EG, Mazzocco C (2003) A new porous hydroxyapatite for promotion of bone regeneration in maxillary sinus augmentation: clinical and histologic study in humans. Int J Oral Maxillofac Implants 18: 23–30. PubMed: 12608665. [PubMed] [Google Scholar]
- 40. Tarnow DP, Wallace SS, Froum SJ, Rohrer MD, Cho SC (2000) Histologic and clinical comparison of bilateral sinus floor elevations with and without barrier membrane placement in 12 patients: Part 3 of an ongoing prospective study. Int J Periodontics Restorative Dent 20: 117–125. PubMed: 11203554. [PubMed] [Google Scholar]
- 41. Wallace SSS, Froum SJS, Cho S-CS, Elian NN, Monteiro DD et al. (2005) Sinus augmentation utilizing anorganic bovine bone (Bio-Oss) with absorbable and nonabsorbable membranes placed over the lateral window: histomorphometric and clinical analyses. Int J Periodontics Restorative Dent 25: 551–559. PubMed: 16353530. [PubMed] [Google Scholar]
- 42. Tawil G, Mawla M (2001) Sinus floor elevation using a bovine bone mineral (Bio-Oss) with or without the concomitant use of a bilayered collagen barrier (Bio-Gide): a clinical report of immediate and delayed implant placement. Int J Oral Maxillofac Implants 16: 713–721. PubMed: 11669254. [PubMed] [Google Scholar]
- 43. Peleg M, Mazor Z, Garg AK (1999) Augmentation grafting of the maxillary sinus and simultaneous implant placement in patients with 3 to 5 mm of residual alveolar bone height. Int J Oral Maxillofac Implants 14: 549–556. PubMed: 10453671. [PubMed] [Google Scholar]
- 44. Hising P, Bolin A, Branting C (2001) Reconstruction of severely resorbed alveolar ridge crests with dental implants using a bovine bone mineral for augmentation. Int J Oral Maxillofac Implants 16: 90–97. PubMed: 11280367. [PubMed] [Google Scholar]
- 45. Klijn RJ, Meijer GJ, Bronkhorst EM, Jansen JA (2010) A meta-analysis of histomorphometric results and graft healing time of various biomaterials compared to autologous bone used as sinus floor augmentation material in humans. Tissue Eng B Rev 16: 493–507. doi:10.1089/ten.teb.2010.0035. [DOI] [PubMed] [Google Scholar]
- 46. Javed F, Romanos GE (2010) The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent 38: 612–620. doi:10.1016/j.jdent.2010.05.013. PubMed: 20546821. [DOI] [PubMed] [Google Scholar]
- 47. RCT (2010) R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; Available: http://www.R-project.org/. Accessed 23 March 2013. [Google Scholar]
- 48. Fay MP, Shaw PA (2010) Exact and asymptotic weighted logrank tests for interval censored data: the interval R package. J Stat Softw. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wang X, Yan J, Chen M-H Package “dynsurv”: Dynamic models for survival data. dynsurv: Dynamic models for survival data. Available: http://cran.r-project.org/web/packages/dynsurv/index.html. Accessed 23 March 2013.
- 50. Schwarzer G, Schwarzer MG (2012) Package “meta”: Meta-Analysis with R.
- 51. Ferrigno N, Laureti M, Fanali S (2006) Dental implants placement in conjunction with osteotome sinus floor elevation: a 12-year life-table analysis from a prospective study on 588 ITIRimplants. Clin Oral Implants Res 17: 194–205. doi:10.1111/j.1600-0501.2005.01192.x. PubMed: 16584416. [DOI] [PubMed] [Google Scholar]
- 52. Turnbull BW (1976) The Empirical Distribution Function with Arbitrarily Grouped, Censored, and Truncated Data. 1 pp. [Google Scholar]
- 53. Aghaloo TLT, Moy PKP (2007) Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Vol. 22 Suppl: pp. 49–70. [PubMed] [Google Scholar]
- 54. Esposito M, Grusovin MG, Rees J, Karasoulos D, Felice P et al. (2010) Effectiveness of sinus lift procedures for dental implant rehabilitation: a Cochrane systematic review. Eur J Oral Implantol 3: 7–26. PubMed: 20467595. [PubMed] [Google Scholar]
- 55. Esposito M, Grusovin MG, Kwan S, Worthington HV, Coulthard P (2008) Interventions for replacing missing teeth: bone augmentation techniques for dental implant treatment. Cochrane Database Syst Rev CD: 003607. [DOI] [PubMed] [Google Scholar]
- 56. Cox DR (1972) Regression models and life-tables. J R Stat Soc B Stat Methodol. [Google Scholar]
- 57. Therneau TM, Grambsch PM (2000) Modeling Survival Data: Extending the Cox Model.
- 58. Balevi B (2010) Implant-supported cantilevered fixed partial dentures. Evid Based Dent 11: 48–49. doi:10.1038/sj.ebd.6400721. PubMed: 20577285. [DOI] [PubMed] [Google Scholar]
- 59. Albrektsson T, Jansson T, Lekholm U (1986) Osseointegrated dental implants. Dent Clin North Am 30: 151–174. PubMed: 3514290. [PubMed] [Google Scholar]
- 60. Hallman M, Hedin M, Sennerby L, Lundgren S (2002) A prospective 1-year clinical and radiographic study of implants placed after maxillary sinus floor augmentation with bovine hydroxyapatite and autogenous bone. YJOMS 60: 277–285. [DOI] [PubMed] [Google Scholar]
- 61. Peleg M, Garg AK, Mazor Z (2006) Healing in smokers versus nonsmokers: survival rates for sinus floor augmentation with simultaneous implant placement. Int J Oral Maxillofac Implants 21: 551–559. PubMed: 16955605. [PubMed] [Google Scholar]
- 62. Fugazzotto PA (2002) Immediate implant placement following a modified trephine/osteotome approach: success rates of 116 implants to 4 years in function. Int J Oral Maxillofac Implants 17: 113–120. PubMed: 11858567. [PubMed] [Google Scholar]
- 63. Hallman M, Nordin T (2004) Sinus floor augmentation with bovine hydroxyapatite mixed with fibrin glue and later placement of nonsubmerged implants: a retrospective study in 50 patients. Int J Oral Maxillofac Implants 19: 222–227. PubMed: 15101593. [PubMed] [Google Scholar]
- 64. Rodriguez A, Anastassov GE, Lee H, Buchbinder D, Wettan H (2003) Maxillary sinus augmentation with deproteinated bovine bone and platelet rich plasma with simultaneous insertion of endosseous implants. J Oral Maxillofac Surg 61: 157–163. doi:10.1053/joms.2003.50041. PubMed: 12618990. [DOI] [PubMed] [Google Scholar]
- 65. Tuna T, Yorgidis M, Strub JR (2011) Prognosis of implants and fixed restorations after lateral sinus elevation: a literature review. J Oral Rehabil 39: 226–238. PubMed: 21972928. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA Checklist. The PRISMA Checklist documents the methods of analysis and inclusion criteria that were specified in advance by the reviewers according to PRISMA guidelines.
(DOC)
Reference appendix. The table documents the full reference for the abbreviated publications listed in table 2.
(DOCX)