TASK FORCE CHARGES
A task force was convened by the American Association of Colleges of Pharmacy (AACP) to provide rationale for academic pharmacy engagement with organizations/institutions providing new models of team-based patient care designed to improve patient access, care quality, and affordable care. Descriptions of new care models, such as patient centered medical homes (PCMHs) and accountable care organizations (ACO), were included as well as descriptions of existing partnerships with academic pharmacy.
Specifically, this task force was charged with:
1. Providing a rationale for colleges/schools of pharmacy to engage in PCMHs and ACOs that includes a list of recommended articles and sites that could help members become informed about such organizations, corresponding professional association, regulatory bodies and government agencies.
2. Describing model partnerships of colleges of pharmacy with PCMHs and ACOs.
3. Disseminating information gathered above in a form of a white paper as a “call to arms” for the pharmacy academy.
BACKGROUND
The Patient-Centered Medical Home (PCMH)
The medical home model holds promise as a way to improve health care in the United States by transforming how primary care is organized and delivered. Building on the work of a large and growing community, the Agency for Healthcare Research and Quality (AHRQ) defines a medical home not simply as a place, but as a model of the organization of primary care that delivers the core functions of primary health care.
The Medical Home encompasses six functions and attributes:
1. Comprehensive Care. The PCMH is accountable for meeting the large majority of patient physical and mental health care needs, including prevention and wellness, acute care, and chronic care. Providing comprehensive care requires a team of care providers. This team might include multiple providers, including physicians, advanced practice nurses, physician assistants, nurses, pharmacists, nutritionists, social workers, educators, and care coordinators. Although some medical home practices may physically bring together large and diverse teams of care providers to meet the needs of their patients, others, particularly smaller practices, will build virtual teams linking patients to providers and services within specific communities.
2. Patient-Centered. The PCMH provides primary health care that is relationship-based with an orientation toward the whole person. Partnering with patients and their families requires understanding and respecting each patient’s unique needs, culture, values, and preferences. The medical home practice actively supports patient education and self care management based on their desired level. Recognizing that patients and families are core members of the care team, medical home practices ensure that they are fully informed partners in establishing and participating in their own care plans.
3. Coordinated Care. The PCMH coordinates care across all aspects of the health care system. Such coordination is particularly critical during transitions between sites of care, such as when patients are being discharged from the hospital. Medical home practices also excel at building clear and open communication among patients and families, the medical home, and other members of the care team.
4. Accessible Services. The PCMH delivers accessible services with shorter waiting times for urgent needs, enhanced in-person hours, around-the-clock telephone or electronic access to a member of the care team, and alternative methods of communication such as email and telephone care. The medical home practice is responsive to patients’ preferences regarding access.1
-
5. Quality and Safety. The PCMH demonstrates a commitment to quality improvement by ongoing engagement in activities such as utilizing evidence-based medicine and clinical decision-support tools to guide shared decision making with patients and their families, engaging in performance measurement and improvement, measuring and responding to patient experiences and satisfaction, and practicing population-based health management. Sharing robust quality and safety data as well as improvement activities publicly is also an important marker of a system-level commitment to quality patient care.
AHRQ recognizes the central role of health information technology (HIT) in successfully implementing the key features of the medical home. Additionally, AHRQ notes that creating accessible, affordable, and high-quality primary care delivery platforms will require significant workforce development and fundamental payment reform.
6. Payment. The current three-part model of reimbursement in the PCMH integrates fee-for-service, pay-for-performance, and reimbursement for coordination of patient care. Payment should be outcome-driven and reflective of case mix, enhanced technologies, quality improvements, and shared savings achieved by effective patient management. 1,2
Health Homes
The Affordable Care Act of 2010, Section 2703, created an optional Medicaid State Plan benefit for states to establish Health Homes to coordinate care for people with Medicaid who have chronic conditions by adding Section 1945 of the Social Security Act. The Centers for Medicare & Medicaid Services (CMS) expects state health home providers to operate under a “whole-person” philosophy. Providers in Health Homes will integrate and coordinate all primary and acute care, behavioral health, and long-term services and support to treat the whole person.
Health Homes are for people with Medicaid who have two or more chronic conditions, or have one chronic condition and are at risk for a second one, or have a serious and persistent mental health condition. Chronic conditions listed in the statute include mental health, substance abuse, asthma, diabetes, heart disease and being overweight. Additional chronic conditions, such as HIV/AIDS, may be considered by CMS for approval.
Health home services include comprehensive care management, care coordination, health promotion, comprehensive transitional care/follow-up, patient and family support, and referral to community/social support services. States have flexibility to determine eligible health home providers. Health home teams must include medical providers and specialists, nurses, pharmacists, nutritionists, dieticians, social workers, behavioral health providers, chiropractors, licensed complementary and alternative practitioners.3
Medical Neighborhoods
A medical neighborhood comprises PCMHs and the constellation of other clinicians (including pharmacists) who provide health care services to patients within it, along with community and social service organizations and state and local public health agencies. The PCMH and the surrounding medical neighborhood can focus on meeting the needs of the individual patient but also incorporate aspects of population health and overall community health needs in its objectives.
Within the PCMH, the primary clinician caring for the patient may be a physician, nurse practitioner, or physician assistant. Importantly, the medical neighborhood is not necessarily a geographic construct but instead a set of relationships revolving around the patient and his or her PCMH, based on that patient’s health care needs. Most medical neighborhood clinicians are likely to be in close proximity to the patient’s medical home.
The intended outcomes of a high-functioning medical neighborhood include improved patient outcomes; patient safety; patient experience; and possibly lower costs through reduced duplication of services, increased delivery of preventive services, and more evidence-based patient care (resulting in, for example, fewer readmissions, polypharmacy issues, and adverse events).4
Accountable Care Organizations (ACO)
An Accountable Care Organization (ACO) is a group of health care providers who give coordinated care and chronic disease management, improving the quality of care patients get. The organization's payment is tied to achieving health care quality goals and outcomes that result in cost savings. Alternatively, it is a set of providers associated with a defined population of patients, accountable for the quality and cost of care delivered to that population. Several different payment models exist for ACOs, including shared savings, bundled payments, capitation, partial capitation/global payments, and global payments.5-8
Community Care Organizations (CCO)
A Community Care Organization (CCO) is an ACO that is designed to focus on the needs of a community’s safety net population, with special emphasis on addressing the social determinants of health such as poverty, unemployment, homelessness, poor housing, neighborhood violence, and other factors. The focus of a CCO is to engage existing community service agencies for the purpose of improving patient outcomes, particularly in underserved populations.
Also known in some states as a Coordinated Care Organization, a CCO is a network of all types of health care providers (e.g., health care, mental health care, dental care, etc.) who have agreed to work together in their communities to serve people receiving health care coverage under Medicaid, with specific exceptions. Designed by a broad cross-section of community residents and community partners, the core of the CCO is made up of existing community service agencies, including:
• Federally Qualified Health Centers (FQHCs) and Rural Health Centers (RHCs)
• Community Mental Health and Substance Use Disorder Treatment Providers
• Recovery, Peer and Wellness Organizations
• Public Health Departments
• Hospitals
• Social Service Agencies
• Child Welfare Providers and Family Resource Centers
• Housing and Homeless Services Providers
• Oral Health Providers
• Pre-Schools and Schools
• Job Training and Employment Support Organizations
The purpose of the CCO is to organize a Healthcare Neighborhood that will help all community members move toward the triple aim: better health for the population, better care for individuals, resulting in reduced cost growth. A core objective of the CCO is to develop an integrated network of community groups that see themselves as hospital and institution prevention organizations, helping to prevent admission and readmission to acute care and psychiatric hospitals; nursing homes; youth residential treatment facilities; jails, prisons, and juvenile justice facilities; and other restrictive, high cost, non-community based institutions. Health, wellness and recovery are at the center of the CCO and major changes are needed to update the existing service delivery paradigm and payment models to support this work.
Community-Based Organizations (CBO)
As defined in the Affordable Care Act (ACA), community-based organizations provide care transition services across the continuum of care through partnering arrangements with hospitals with high re-admission rates, and whose governing bodies include sufficient representation of multiple health care stakeholders, including consumers.9-11
RATIONALE FOR ACADEMIC INVOLVEMENT IN PCMHs and ACOs
As this is the new direction for health care in this country, this relationship should become a primary emphasis in the future of pharmacy education. This new alignment with these emerging health care entities will help colleges of pharmacy to identify innovative ambulatory care sites for experiential education, including new emerging models supportive of interprofessional education as well as research through practice-based research networks (PBRNs). When considering the role pharmacy faculty and student pharmacists can play, using the six functions and attributes of a PCMH noted previously (i.e., Comprehensive Care, Patient Centered, Coordinated Care, Accessible Services, Quality and Safety, and Payment), there is a strong potential for contributions to, and collaborations with the PCMH in all of the areas.
Pharmacists/pharmacy faculty offer several unique contributions to a PCMH or ACO. In particular, pharmacists: have the ability to aggregate lives (reach out to many patients), are able to influence patient behavior (adherence), can assist in managing patient risk, and have a large geographic footprint when you include community pharmacy practices. Further, as academicians, student pharmacists need to be prepared to be involved in, and become leaders in this evolving health care system.
With the advent of these new health care entities, there will be a significant need for data collection and analysis as these entities continue to roll out, providing a rich source of opportunities for scholarship. This will provide an opportunity for collaborations between colleges of pharmacy, pharmacy informatics professionals, and other HIT professionals employed by ACOs. Colleges/schools of pharmacy may be able to assist ACOs in developing new methods of gathering and analyzing medication-related data. Some of the key issues are noted below, and potential resources are contained in Appendix 1 and 2.
1. Transformation of Healthcare in the U.S.
Simply stated, this is where healthcare is heading. The Patient Protection and Affordable Care Act has created significant traction for PCMH and ACO models of care delivery. Pharmacists and student pharmacists must be prepared to participate in these emerging models of care. As medication experts, often possessing a “generalist” perspective, pharmacists provide critical and unique contributions to patient care that should be incorporated into PCMH/ACOs. Within the Academy, pharmacy faculty hold a strong perspective on what the pharmacist profession can contribute as a member of this health care team, and should have both the clinical presence and practice scholarship to position themselves well to be strong advocates for delineation of roles for the pharmacist in this setting.
2. Employer Demand and Accreditation Standards
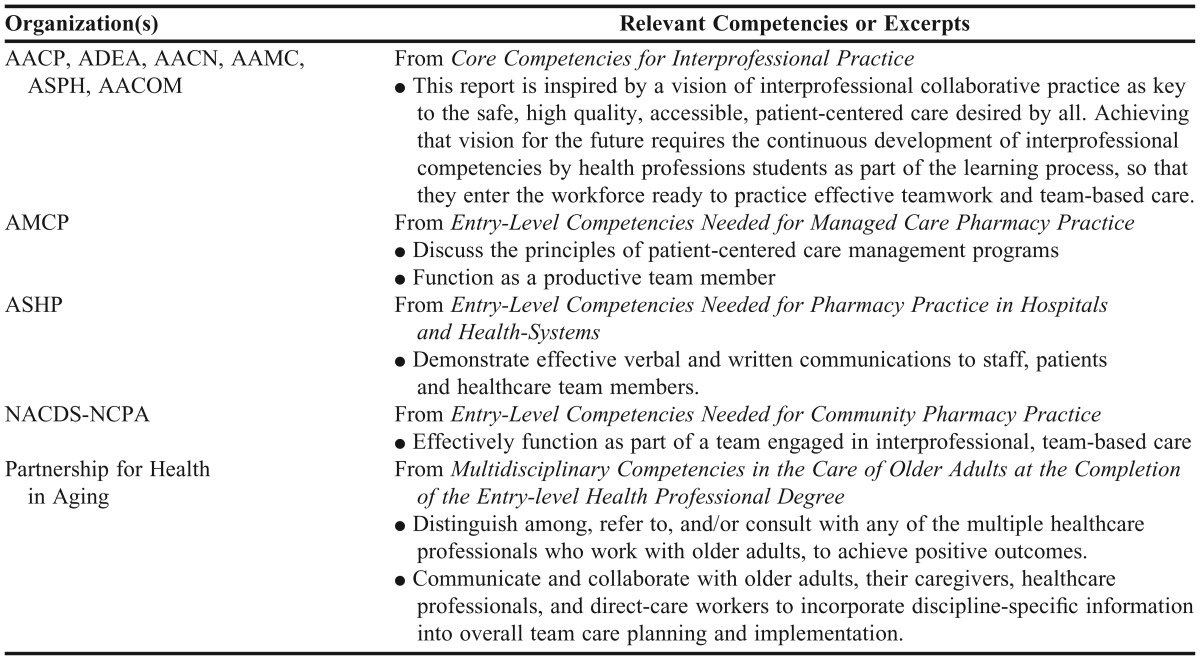
As ACPE explores revision of its standard for colleges of pharmacy, pharmacy professional and trade associations have weighed in on the competencies needed for entry-level practitioners. The ACPE invitational conference in September 2012 included the documents listed in Table 1.
Table 1.
Documents Discussed at the Accreditation Council for Pharmacy Education Meeting
In a tightened job market, employers are increasingly looking for pharmacists who are able to provide advanced patient care services; students with the aforementioned competencies and other technical certifications such as immunization, diabetes, or medication therapy management will be favorably positioned.12-16
3. Medication Management/Clinical Pharmacy Services
There are more than 3.5 billion prescriptions written annually in the U.S. accounting for about $300 billion in pharmaceutical sales, and four out of five patients who visit the physician leave with at least one prescription. There is ample evidence that drug therapy problems occur regularly and contribute to significant costs within the U.S. healthcare system approximated at just under $300 billion annually. The Institute of Medicine recognizes that while medication costs are only approximately 10% of the total health care expenditures, medications’ potential for both help and harm are enormous. Therefore, assuring the optimal use of all medications (prescribed and over-the-counter) through various monitoring and counseling services in an interdisciplinary practice is essential to ensure that the intended outcomes are achieved by all stakeholders. Medicare Part D recognized the value of medication therapy management (MTM) services, by requiring all providers of the prescription benefit to offer such services to beneficiaries. While well intended, the implementation of MTM services to Medicare beneficiaries has not been as robust as intended. In part, one of the challenges is with pharmacists not having obtained universal provider status in Medicare Part B, with open access to other important patient data such as laboratory results. Yet the benefits to MTM services has been recognized by several state Medicaid programs and other insurance carriers, as this is a benefit offered in some cases to very high risk populations (e.g., stroke, heart failure, etc.).17-19
4. Open Frontier for Research
More than 5,500 accredited PCMHs and 450 ACOs are in existence, yet few meaningfully engage pharmacists and pharmacy services as a core element. There is a significant opportunity for schools and colleges of pharmacy to serve as facilitators and connect pharmacy services to these structures by leveraging existing relationships, experiential rotations, and practice-based research networks.
There is also a need to significantly augment research about the role and value of pharmacy in these emerging models of care, as much work to date is conceptual. There is a limited – but growing – pipeline of research, but much more can and must be done on diverse models: those that embed pharmacists in PCMHs and ACOs, and those that involve innovative partnerships between ambulatory and community pharmacists and PCMHs and ACOs. During the summer of 2012, numerous grants were awarded through the Center for Medicare and Medicaid Innovation, Health Care Innovation Award. Examples of research projects that are in progress, and are either led by or collaborating with schools and colleges of pharmacy are noted in Appendix 3.20,21
5. Faculty Development
In this new environment, faculty and academic leaders should develop key skills and practices to support and guide them in developing partnerships with PCMH/ACOs. These include:
• Modeling core interprofessional competencies as they train students
• Training on negotiation to aid in the development of mutually beneficial partnerships between colleges of pharmacy and PCMH/ACOs
• Providing a guide for faculty and academic leaders to understand the metrics used to assess PCMH/ACOs
• Making recommendations for efficient documentation systems for faculty and student contributions to PCMH/ACOs
• Providing additional training for pharmacists and pharmacy students on triage and physical assessment. With primary care provider (MD, NP, PA) shortages, pharmacists may see patients without the benefit of an integrated, local primary care physician
CONCLUSION
Advances that dramatically impact care are becoming the norm as health professions work to address the triple aim through transformation of our healthcare system. Multidisciplinary care coordination, new technologies for electronic health records, quality improvement initiatives, and outcomes-driven care are expected, particularly for a population that is living longer with more chronic diseases. Lessons learned in PCMH settings will be instructive as we look to future needs in health care education. Similar to the evolving medical home model, academic pharmacy will require a redesigned educational “home” to adequately support future practitioners and researchers.
Appendix 1. PCMH/ACO toolkit: a toolkit for colleges of pharmacy to promote developing partnerships with patient centered medical homes and accountable care organizations.
A tool kit should include, but is not limited, to the following components:
- 1. Provide PCMH/ACO leaders with the 2010 Health Affairs article, and associated articles, with a discussion of its content:
- Smith M, Bates DW, Bodenheimer T, and Cleary PD. Why pharmacists belong in the medical home. Health Affairs. 2010; 29: 906-913.
- Smith MA and Nigro S. PSAP VII - Book 8: Science and Practice of Pharmacotherapy, Chapter 2: Patient-centered Medical Home. Kansas City: American College of Clinical Pharmacy; 2011:87-101.
- Abrons JP and Smith M. Patient-centered medical homes: Primer for pharmacists. J Am Pharm Assoc. 2011; 17: 52-64.
- Smith M, Giuliano MR, Starkowski MP. In Connecticut: Improving patient medication management in primary care. Health Affairs. 2011; 30 : 646-654.
- Smith M. Pharmacists and the Primary Care Workforce. Ann Pharmacother. 2012; 46: 1568-1571. Online: http://www.hwbooks.com/pdf/articles/10/10-16-2012/aph.1R438.pdf
- Giberson S, Yoder S, Lee MP. Improving Patient and Health System Outcomes through Advanced Pharmacy Practice. A Report to the U.S. Surgeon General. Office of the Chief Pharmacist. U.S. Public Health Service. Dec 2011.
- The Patient-Centered Primary Care Collaborative (PCPCC): The Patient Centered Medical Home: Integrating Comprehensive Medication Management to Optimize Patient Outcomes - A Resource Guide http://www.pcpcc.net/files/medmanagement.pdf (free downloads).
- Centers for Disease Control and Prevention. A Program Guide for Public Health: Partnering with Pharmacists in the Prevention and Control of Chronic Diseases. http://www.cdc.gov/dhdsp/programs/nhdsp_program/docs/pharmacist_guide.pdf
2. Core Competencies for Interprofessional Practice should also be provided, so that colleges can consider holistically how interprofessionalism can be woven across the curriculum.
3. Case studies and best practices on how schools have partnered in these models. This should include a description of the common barriers to partnering and how these challenges can be overcome.
4. A literature-supported, bulleted list of the many roles that pharmacists provide in these settings, as well as in other settings (e.g., long-term care), where pharmacists have long participated in interprofessional health care teams.
5. A data-driven needs assessment for pharmacy in PCMH/ACOs, looking for opportunities to serve PCMH/ACOs. Current metrics used in these settings may not capture meaningful and unique contributions made by pharmacists.
6. Pharmacists are now trained to provide a variety of services which meet a “patient’s physical and mental health care needs, including prevention and wellness, acute care, and chronic care” (from definition of Comprehensive Care above). Pharmacists and student pharmacists may offer clinical services in some of these domains in addition to dispensing or pharmacotherapy services. These services benefit students as they learn to interact with patients. Students, well trained and well supervised, can provide some of these services as well.
7. Emphasize the need to clarify the local roles and responsibilities, and the “best use” of a pharmacotherapy expert (e.g., a pharmacist faculty member) and student pharmacists in a given setting.
8. Examples of pharmacotherapy service contracts, for the provision of the above noted services, and strategies for implementation of these services in these settings, are recommended.
Appendix 2. Selected resources for PCMH, ACO, and CCO.
A. Foundational articles on PCMH and ACO
American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, and American Osteopathic Association. Joint principles of the patient-centered medical home. 2007.
American Academy of Pediatrics ad hoc task force on definition of the medical home. The medical home. Pediatrics. 1992; 90: 774.
Berenson RA, Hammons T, Gans DN, et al. A house is not a home: keeping patients at the center of practice redesign. Health Affairs (Millwood) 2008; 27: 1219-1230.
Bodenheimer T, Grumbach K, Berenson RA. A lifeline for primary care. N Engl J Med. 2009; 360: 2693-2696.
Center for Policy Studies in Family Medicine and Primary Care. The patient centered medical home: History, seven core features, evidence and transformational change. Washington DC: Robert Graham Center, 2007.
Grumbach K. The outcomes of implementing patient-centered medical home interventions: A Review of the evidence on quality, access and costs from recent prospective evaluation studies, August 2009. Washington, DC: Patient Centered Primary Care Collaborative.
Homer CJ, Klatka K, Romm D, et al. A review of the evidence for the medical home for children with special health care needs. Pediatrics. 2008; 122(4): 922-937.
O'Malley AS, Peikes D, Ginsburg PB. Making medical homes work: moving from concept to practice. Washington, DC: Center for Studying Health System Change, 2008.
Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care - two essential elements of delivery-system reform. N Engl J Med. 2009; 361: 2301-2303.
Zuckerman S, Merrell K, Berenson R, et al. Incremental cost estimates for the patient-centered medical home. New York, NY: Commonwealth Fund; 2009.
B. Role of Pharmacists in the Patient Centered Medical Home/Accountable Care Organizations
Smith M, Bates DW, Bodenheimer T, et al. Why pharmacists belong in the medical home. Health Affairs. 2010; 29: 906-913.
Haines SL, DeHart RM, Flynn AA, et al. Academic pharmacy and patient-centered health care: a model to prepare the next generation of pharmacists. J Am Pharm Assoc. 2011; 51: 194–202.
Abrons JP and Smith M. Patient-centered medical homes: Primer for pharmacists. J Am Pharm Assoc. 2011; 17(5): 52-64.
Kozminski M, Busby R, McGivney MS, et al. Pharmacist integration into the medical home: qualitative analysis. J Am Pharm Assoc. 2011; 51: 173–183.
Smith MA and Nigro S. PSAP VII - Book 8: Science and Practice of Pharmacotherapy, Chapter 2: Patient-centered Medical Home. Kansas City: American College of Clinical Pharmacy; 2011: 87-101.
Rodriguez de Bittner M, Adams AJ, et al. Report of the 2010-2011 Professional Affairs Committee: Effective partnerships to implement pharmacists’ services in team-based, patient-centered healthcare. Am J Pharmaceut Educ. 2011; 75 (10): S11.
Scott MA, Hitch B, Ray L, Colvin G. Integration of pharmacists into a patient-centered medical home. J Am Pharm Assoc. 2011;51: 161–166.
Choe HM, Farris KB, Stevenson JG, et al. Patient-centered medical home: developing, expanding, and sustaining a role for pharmacists. Am J Health-Syst Pharm. 2012; 69: 1063-71.
Smith M. Pharmacists and the primary care workforce. Ann Pharmacother. 2012; 46: 1568-1571. Online: http://www.hwbooks.com/pdf/articles/10/10-16-2012/aph.1R438.pdf
Edwards HD, Webb RD, Scheid DC, et al. A pharmacist visit improves diabetes standards in a patient-centered medical home (PCMH). Am J Med Qual. 2012; Jun 7.
Rucker NL. Medicare Part D’s Medication Therapy Management: Shifting from Neutral to Drive. Insight on the Issues, Number 64, AARP Public Policy Institute, Washington, DC, June 2012.
Pharmacists as Vital Members of Accountable Care Organizations. Academy of Managed Care Pharmacy, Alexandria, VA. http://www.amcp.org/WorkArea/DownloadAsset.aspx?id=9728.
The Patient-Centered Medical Home: Integrating Comprehensive Medication Management to Optimize Patient Outcomes. Resource Guide, Second edition. Patient-Centered Primary Care Collaborative, Washington, DC, June 2012.
The Patient-Centered Primary Care Collaborative (PCPCC): The Patient Centered Medical Home: Integrating Comprehensive Medication Management to Optimize Patient Outcomes - A Resource Guide http://www.pcpcc.net/files/medmanagement.pdf (free downloads).
This guide defines CMM and outlines the “10 critical steps” which has been added to the AHRQ Innovation Exchange – Quality Toolkit: http://www.innovations.ahrq.gov/content.aspx?id=3419. This document demonstrates the support of CMM through the PCPCC: http://www.pcpcc.net.
The PCPCC Medication Management Task-force. The Opportunity for Comprehensive Medication Management Within the Patient-Centered Medical Home Structure. http://www.pcpcc.net/files/medication_management_in_pcmh_with_practice_profiles.pdf
Isetts BJ, Schondelmeyer SW. Clinical and economic outcomes of medication therapy management services: The Minnesota experience. J Am Pharm Assoc. 2008; 48(2): 203-211.
Isetts B. Pharmaceutical Care, MTM, & Payment: The Past, Present, & Future. Ann Pharmacother. 2012; 46 (Suppl 1): S47-56.
Legislative Language/Agency Policy
The Minnesota legislation which documents support of CMM at the state level: Minn. Stat. §256B.0625, subd. 13h in 2005. https://www.revisor.mn.gov/statutes/?id=256b.0625
The National Conference of State Legislatures (NCSL) has a website keeping up with some of the MTM legislation at the state level- http://www.ncsl.org/?tabid=19064
The National Academy for State Health Policy lists PCMH activity in state Medicaid programs and multi-payer initiatives: Medical Home & Patient-Centered Care | National Academy for State Health Policy
HIPAA Compliant MTMS CPT Codes from MN- Department of Health- MHCP Provider Manual: http://www.dhs.state.mn.us/main/idcplg?IdcService=GET_DYNAMIC_CONVERSION&dDocName=dhs16_136889&RevisionSelectionMethod=LatestReleased#P157_10295
McInnis TA and Webb CE. Comprehensive Medication Management in the Patient Centered Medical Home – Is it Critical for Success? Medical Home News. April 2010, volume 2, number 4. www.MedicalHomeNews.com
Ramalho de Oliveira D, Brummel AR, Miller, DB. Medication Therapy Management: Ten years of experience in a large integrated health care system. J Manag Care Pharm. 2010; 16(3): 185-195.
Morreale A, et al. Integrating Clinical Pharmacy into the Medical Home Model: Solving a Medication Use Crisis. Medical Home News. April 2012; 4(4). www.MedicalHomeNews.com
BCBS North Dakota PCMH program results (∼75% of all members enrolled after two years): http://pcpcc.net/files/102011summit/5.hanekom_pcpcc_10-21-2011.pdf
U.S. Department of Health and Human Services. Inventory of Programs, Activities, and Initiatives Focused on Improving the Health of Individuals with Multiple Chronic Conditions. www.hhs.gov/ash/initiatives/mcc
American Academy of Family Physicians (AAFP): Current status on legislation tracked by state, including PCMH and ACOs: http://www.aafp.org/online/en/home/policy/state/statetrack.html
Websites
The following are several examples of resources for pharmacy faculty and student pharmacists:
Agency for Healthcare Research and Quality (AHRQ): http://pcmh.ahrq.gov/portal/server.pt/community/pcmh__home/1483
List of AHRQ foundational articles on the PCMH: http://pcmh.ahrq.gov/portal/server.pt/community/pcmh__home/1483/foundational_articles
National Committee Quality Assurance (NCQA): http://www.ncqa.org/tabid/631/Default.aspx
The Utilization Review Accreditation Commission (URAC) has developed Patient Centered Health Care Home (PCHCH) programs to educate and guide health care practices, and their sponsoring health plans, insurers and pilot programs: https://www.urac.org/pchch/
Patient-Centered Primary Care Collaborative: http://www.pcpcc.net
Medication Management Task Force Resources, from the Patient-Centered Primary Care Collaborative: http://www.pcpcc.net/content/pcpcc-medication-management-taskforce-resources http://www.pcpcc.net/guide/medication-management
Successful Incorporation of Comprehensive Medication Management into PCMH and ACO Coordinated Care Models, a Training Session for Pharmacists: http://www.pcpcc.net/webinar/successful-incorporation-comprehensive-medication-management-pcmh-and-aco-coordinated-care
Appendix 3. CMS Health Care Innovation Award project profiles and ACOs.
Established by the Affordable Care Act, the Center for Medicare & Medicaid Services Innovation Center (CMMI) announced the first round of awardees for the Health Care Innovation Awards on May 8 and June 15, 2012. Awardees listed below will implement projects in communities across the nation that aim to deliver better health, improved care and lower costs to people enrolled in Medicare, Medicaid and the Children’s Health Insurance Program (CHIP), particularly those with the highest health care needs. Funding for these projects is for three years. More information on the Health Care Innovation Awards can be found at: innovation.cms.gov/initiatives/innovation-awards
The following list includes short descriptions of those 2012 CMMI projects that involve pharmacists, include a medication management aspect, or have a collaboration with a college/school of pharmacy:
ASIAN AMERICANS FOR COMMUNITY INVOLVEMENT
Project Title: “Patient Navigation Center”
Geographic Reach: California
Funding Amount: $2,684,545
Estimated 3-Year Savings: $3,373,602
Summary: Asian Americans for Community Involvement (AACI), in partnership with the Career Ladders Project and three community colleges is receiving an award to train Asian and Hispanic youth and veteran AACI case workers as non-clinical health workers for a Patient Navigation Center. Serving low-income Asian and Hispanic families in Santa Clara County, the Center will provide enabling services, including translation, appointment scheduling, referrals, transportation, and application help for social services, as well as after-hours and self-care assistance. Patient navigation will lead to improved access to care, better disease screening, decreased diagnosis time, better medication adherence, a reduction in emergency room visits, and reduced anxiety for patients.
Over a three-year period, Asian Americans for Community Involvement will retrain its current staff of nurses, supervisors, and on-call clinicians and create an estimated 29 jobs. The new workers will include patient navigators, nurse and clinician advisors, and a customer service manager.
BEN ARCHER HEALTH CENTER
Project Title: “A home visitation program for rural populations in Northern Dona Ana County, New Mexico”
Geographic Reach: New Mexico
Funding Amount: $1,270,845
Estimated 3-Year Savings: $6,352,888
Summary: The Ben Archer Health Center in southern New Mexico is receiving an award to implement an innovative home visitation program for individuals diagnosed with chronic disease, persons at risk of developing diabetes, vulnerable seniors, and homebound individuals, as well as young children and hard to reach county residents. Ben Archer provides primary health and dental care to rural Dona Ana County, a medically underserved area and health professional shortage area. The program will use nurse health educators and community health workers to bridge the gap between patients and medical providers, aid patient navigation of the health care system, and offer services including case management, medication management, chronic disease management, preventive care, home safety assessments, and health education, thereby preventing the onset and progression of diseases and reducing complications.
Over a three-year period, this program will train an estimated 7.5 workers and will create an estimated 7.5 jobs. The new workforce will include nurses and community care workers. Additionally, Ben Archer Health Center will be providing training to new and existing community health workers and nurses to conduct home visits in a rural farming community.
CAREFIRST
Project Title: “Medicare and CareFirst’s total care and cost improvement program in Maryland”
Geographic Reach: Maryland
Funding Amount: $24,000,000
Estimated 3-Year Savings: $29,213,838
Summary: CareFirst BlueCross/BlueShield is receiving an award to expand its Total Care and Cost Improvement Program (TCCI), a Patient-Centered Medical Home model of care delivery and payment, to 25,000 Medicare beneficiaries in Maryland per year. This approach will move the region toward a new health care financing model that is more accountable for care outcomes and less driven by the volume-inducing aspects of fee-for-service payment. The TCCI model will enhance support for primary care, empowering primary care physicians to coordinate care for multi-chronically ill Medicare beneficiaries and patients at high risk for chronic illnesses. TCCI will result in less fragmented health care, reducing avoidable hospitalizations, emergency room visits, medication interactions, and other problems caused by gaps in care and ensuring that patients receive the appropriate care for their conditions.
Over a three-year period, the CareFirst BlueCross/BlueShield program will train an estimated 672 workers and will create an estimated 28 jobs. The new workforce will include local care coordinators, specialty-based nurse case managers, hospital transition of care coordinators, program consultants, community pharmacists, pharmacy managers, clinical pathways hub operations and support workers, operational and data support positions.
CARILION NEW RIVER VALLEY MEDICAL CENTER
Project Title: “Improving health for at-risk rural patients (IHARP) in 23 southwest Virginia counties through a collaborative pharmacist practice model”
Geographic Reach: Virginia
Funding Amount: $4,162,618
Estimated 3-Year Savings: $4,308,295
Summary: Carilion New River Valley Medical Center, in partnership with Virginia Commonwealth University School of Pharmacy, Aetna Healthcare and CVS/Caremark, is receiving an award to improve medication therapy management for Medicare and Medicaid beneficiaries and other patients in 23 underserved rural counties in southwest Virginia. Their care delivery model, involving six rural hospitals and 17 primary care practices, will train pharmacists in transformative care and chronic disease management protocols. Through care coordination and shared access to electronic medical records, the project will enable pharmacists to participate in improving medication adherence and management, resulting in better health, reduced hospitalizations and emergency room visits, and fewer adverse drug events for patients with multiple chronic diseases.
CHRISTIANIA CARE HEALTH SYSTEM
Project Title: “Bridging the Divide”
Geographic Reach: Delaware
Funding Amount: $9,999,999
Estimated 3-Year Savings: $376,327
Summary: Christiania Care Health System, serving the state of Delaware, is receiving an award to create and test a system that will use a heart disease “data hub” and case managers to improve care for post-myocardial infarction and revascularization patients, the majority of them Medicare or Medicaid beneficiaries. Christiana will integrate statewide health information exchange data with cardiac care registries from the American College of Cardiology and the Society of Thoracic Surgeons, enabling more effective care/case management through near real time visibility of patient care events, lab results, and testing. This will decrease emergency room visits and avoidable readmissions to hospitals and improve interventions and care transitions. The investments made by this grant are expected to generate cost savings beyond the three year grant period.
Over a three-year period, Christiania Care Health System will create an estimated 16 health care jobs, including positions for nurse care managers, pharmacists, and social workers.
FAMILY SERVICE AGENCY OF SAN FRANCISCO
Project Title: “Prevention and Recovery in Early Psychosis (PREP)”
Geographic Reach: California
Funding Amount: $4,703,817
Estimated 3-Year Savings: $4,235,801
Summary: Family Service Agency of San Francisco is receiving an award to expand and test its model for Prevention and Recovery in Early Psychosis (PREP) for low-income, largely Latino counties in the San Francisco area. Schizophrenia is estimated to account for 2.5 to 3 percent of United States health care expenditures. Without an intervention like PREP, as many as 90 percent of the patients served would be Supplemental Security Income/Medicare recipients (up from 30 percent now) by the time they reached their 30s. Through evidence-based treatments, medication management, and care management, PREP aims to prevent the onset of full psychosis, and in cases in which full psychosis has already occurred, seeks to fully remit the disease and rehabilitate the cognitive functions it has damaged.
Over a three-year period, the Family Service Agency of San Francisco will train 56 health care providers to use their PREP intervention, while creating 19 jobs for social workers, Nurse Practitioners, vocational counselors, and peer and family aides.
FIRSTVITALS HEALTH AND WELLNESS INC.
Project Title: “Improving the health and care of low-income diabetics at reduced costs”
Geographic Reach: Hawaii
Funding Amount: $3,999,713
Estimated 3-Year Savings: $4,829,955
Summary: FirstVitals Health and Wellness Inc., in partnership with AlohaCare, is receiving an award to implement and test a care coordination and health information technology plan that will better regulate glucose levels for Medicaid-eligible patients with Type 1 and Type 2 diabetes. FirstVitals will create a secured database that will receive data feeds from wireless glucose meters. The information will be available to integrated care coordinators, patients, physicians and other approved caregivers, informing decisions about care and enabling caregivers to track and monitor glucose levels, improve medication adherence, and increase patient safety and the effectiveness of treatment. The project will reduce complications, slow the progression of the disease, and reduce emergency room visits and hospitalizations.
Over a three-year period, FirstVitals’ program will train an estimated 11 workers and will create an estimated 6 jobs. The new workforce will include integrated care coordinators, a clinical diabetes educator, and a medical director.
JOHNS HOPKINS UNIVERSITY
Project Title: “Johns Hopkins Community Health Partnership (J-CHiP)”
Geographic Reach: Maryland
Funding Amount: $19,920,338
Estimated 3-Year Savings: $52,600,000
Summary: Johns Hopkins University -- in partnership with Johns Hopkins Health System and its hospitals, community clinics and other affiliates; the Johns Hopkins Urban Health Institute; Priority Partners MCO; Baltimore Medical System, a Federally Qualified Health Center; and local skilled nursing facilities, is receiving an award to create a comprehensive and integrated program, the Johns Hopkins Community Health Partnership (J-CHiP). J-CHiP is designed to increase access to services for high-risk adults in East Baltimore, MD, especially those with chronic illness, mental illness, and/or substance abuse conditions. The intervention improves care coordination across the continuum and comprises early risk screening, interdisciplinary care planning, enhanced medication management, patient/family education, provider communication, post-discharge support and home care services, including self-management coaching, and improved access to primary care. The program will target inpatients at The Johns Hopkins Hospital and Johns Hopkins Bayview Medical Center, expanding to nearly all admissions by year 3. The intervention will also include a specific focus on high-risk Medicare and Medicaid beneficiaries who receive primary care from Johns Hopkins providers in the seven zip code area adjacent to these hospitals. The program will reduce avoidable hospitalizations, emergency room use, and complications and increase access to care and other services.
Over a three-year period, Johns Hopkins University will train and hire 111 new health care workers, including patient/family educators, care coordinators, and behavioral coaches, and will retrain nurse case managers, nurse transition guides, nurse screeners, pharmacists, and physicians already on staff.
MEMORIAL HOSPITAL OF LARAMIE COUNTY DBA CHEYENNE REGIONAL
Project Title: “Wyoming: a frontier state's strategic partnership for transforming care delivery”
Geographic Reach: Wyoming
Funding Amount: $14,246,153
Estimated 3-Year Savings: $33,227,238
Summary: Memorial Hospital of Laramie County (the Cheyenne Regional Medical Center) is receiving an award to transform primary care delivery across Wyoming, a State which faces special challenges because of its low population density and limited health care resources. Memorial Hospital and its partners will retool primary care education, enhance connectivity between hospitals and primary care providers, improve pharmaceutical management of high cost populations, increase medication availability and provider access for vulnerable patients, and address the complex social issues affecting the health of vulnerable populations. Through care redesign, care coordination, and the creation of a State-wide referral database, the project will reduce dependency on hospitals for primary care, increase access to primary care, improve care transitions, and enhance community-based, health-related social service delivery for the comprehensive care of vulnerable populations. The result will be better and more cost-effective use of health care resources and better quality health care.
Over a three-year period, the Cheyenne Regional Medical Center’s program will train an estimated 90 workers and create an estimated 33 jobs. The new workforce will include a strategic initiatives director, a strategic performance manager, a financial analyst, support staff, 28 RN care transition coaches, six telehealth registered nurses, and a technical support coordinator.
MOUNT SINAI SCHOOL OF MEDICINE
Project Title: “Geriatric emergency department innovations in care through workforce, informatics, and structural enhancements (GEDI WISE)”
Geographic Reach: Illinois, New Jersey, New York
Funding Amount: $12,728,753
Estimated 3-Year Savings: $40,124,805
Summary: Mount Sinai School of Medicine is receiving an award to integrate geriatric care with emergency department (ED) care in three large, urban acute care hospitals in New York, New Jersey, and Illinois. Emergency room use by older adults has doubled in the past decade and is expected to continue to increase. The Mount Sinai care model will use evidence-based geriatric clinical protocols, informatics support for patient monitoring and clinical decision support, and structural enhancements to improve patient safety and satisfaction while decreasing hospitalizations, return ED visits, unnecessary diagnostic and therapeutic services, medication errors, and adverse events, such as falls and avoidable complications.
Over a three-year period, Mount Sinai School of Medicine's GEDI WISE program will train more than 400 current health care workers and create 22 new jobs. The new hires will include nurses, nurse practitioners, physician assistants, pharmacists, physical therapy, project coordinators, research assistants, data analysts and geriatric transitional care managers.
NORTH CAROLINA COMMUNITY NETWORKS
Project Title: “Building a statewide child health accountable care collaborative: the North Carolina strategy for improving health, improving quality, reducing costs, and enhancing the workforce”
Geographic Reach: North Carolina
Funding Amount: $9,343,670
Estimated 3-Year Savings: $24,089,682
Summary: North Carolina Community Care Networks, Inc., in partnership with the academic medical centers at Carolinas Medical Center-Charlotte, Duke University Health System, University of North Carolina Hospitals, Vidant Medical Center-East Carolina, and Wake Forest Baptist Health, as well as the children’s units at Cape Fear Valley Health, Cone Health, Mission Hospital, New Hanover Regional Medical Center, Presbyterian Healthcare, and WakeMed Hospitals, is receiving an award to form a Child Health Accountable Care Collaborative. This Collaborative will provide care coordination through embedded specialty care managers in the offices of specialists and through “parent navigators” who will work with patients in their homes. The program addresses the shortage of both pediatric primary care physicians and subspecialists, and will serve 50,000 Medicaid and CHIP children with chronic disease for whom care is costly and fragmented. The result will be reductions in avoidable emergency room visits, hospitalizations, and pharmacy costs, with improved access to care and better quality of life for the children served.
Over a three-year period, North Carolina Community Care Networks Inc. will train an estimated 42 workers and will create an estimated 44 jobs. The new workforce will include children's specialty care managers and parent navigators. Parent navigators are trained to aid families in navigating the complex medical services needed by their children.
OCHSNER CLINIC FOUNDATION
Project Title: “Comprehensive stroke care model through the continuum of care” Geographic Reach: Louisiana Funding Amount: $3,867,944 Estimated 3-Year Savings: $4.9 million
Summary: Ochsner Clinic Foundation is receiving an award to better serve almost 1000 acute care stroke patients in Jefferson and St. Tammany parishes in Louisiana. The model will employ a stroke management and quality assurance through a telemedicine system called “Stroke Central.” This system will enable care providers to monitor patients, evaluate outcomes, and check on medication and treatment adherence on a real time basis. This process will allow care providers to give telemedical “check-ups” to their patients, improving acute stroke management, improving patients’ quality of life, and lowering cost by reducing complications from urinary tract infections and pneumonia, preventing readmissions, and replacing outpatient visits with estimated savings of almost $5 million. Over the three-year period, Ochsner Clinic Foundation’s program will train an estimated 38.2 health care workers and create an estimated 12 new jobs. These workers will provide tele-consultation, assessment, and monitoring support for stroke care.
PHARMACY SOCIETY OF WISCONSIN
Project title: “Retooling the pharmacist’s role in improving health outcomes and reducing health care costs”
Geographic Reach: Wisconsin
Funding Amount: $4,165,191
Estimated 3-Year Savings: $20,448,864
Summary: The Pharmacy Society of Wisconsin is receiving an award to better integrate pharmacists into clinical care teams. This project, expanding the successful Wisconsin Pharmacy Quality Collaborative (WPQC), will transform the pharmacist’s role from drug dispensers to drug therapy coordinator and manager. Participating pharmacists will work collaboratively with physicians and other prescribers to revise prescription drug therapies in accord with evidence-based standards of care, targeting participants with diabetes, chronic heart failure, asthma, and geriatric syndromes. These patients are typically prescribed numerous medications, change locations of care, and/or are non-adherent to evidence-based therapies prescribed for them. The result of the intervention will be better medication adherence, better medication therapy management, and better health, with a decrease in adverse events and complications and more appropriate, evidence-based medication therapy.
Over a three-year period, the Pharmacy Society of Wisconsin’s program will train an estimated 1,200 workers and will create an estimated 7 jobs. Regional implementation specialists and clinical pharmacists will train community pharmacists across the state.
PITTSBURGH REGIONAL HEALTH INITIATIVE
Project Title: Creating a Virtual Accountable Care Network for Complex Medicare Patients Geographic Reach: Pennsylvania Funding Amount: $10,419,511 Estimated 3-Year Savings: $74.1 million
Summary: Pittsburgh Regional Health Initiative is receiving an award for a plan to create specialized support centers, staffed by nurse care managers and pharmacists, to help small primary care practices offer more integrated care within the service areas of seven regional hospitals in Western Pennsylvania. The project will focus not only on approximately 25,000 Medicare beneficiaries with COPD, CHF, and CAD, but also the general primary care population of this area. The resulting teams will provide support for care transitions, intensive chronic disease management, medication adherence, and other problems associated with a lack of communication in health care systems at large and the resulting fragmentation of health care for patients. This approach is expected to reduce 30-day readmissions and avoidable disease-specific admissions with estimated savings of approximately $74 million.
Over the three-year period, Pittsburgh Regional Health Initiative’s program will train an estimated 450 health care workers and create an estimated 26 new jobs. These workers will combine core competencies in the management of specific diseases with primary care support skills, and will be trained in evidence-based pathways of care.
RUTGERS, THE STATE UNIVERSITY OF NEW JERSEY
Project Title: “Sustainable high-utilization team model”
Geographic Reach: California, Colorado, Missouri, Pennsylvania
Funding Amount: $14,347,808
Estimated 3-Year Savings: $67,719,052
Summary: Rutgers, The State University of New Jersey, is receiving an award to expand and test a team-based care management strategy for high-cost, high-need, low-income populations served by safety-net provider organizations in Allentown, PA, Aurora, CO, Kansas City, MO, and San Diego, CA. Led by Rutgers’ Center for State Health Policy, the project will use care management teams (including nurses, pharmacists, social workers, and community health workers) to provide clients with patient-centered support that addresses both health care needs and the underlying determinants of health. Teams will assist patients in filling prescriptions, finding housing or shelter, applying for health coverage or disability benefits, handling legal issues, finding transportation, treating depression, managing chronic illness, and coordinating appropriate specialty care. After patients are stabilized, the care management team will transition them to local primary care medical homes. By improving beneficiaries’ access to ambulatory medical and social services, the project will improve patient outcomes and reduce preventable hospital inpatient and emergency room utilization.
Over a three-year period, Rutgers’ program will train an estimated 155 workers and will create an estimated 43 jobs. The new workforce will include community health workers.
EAU CLAIRE COOPERATIVE HEALTH CENTERS, INC.
Project Title: “Healthy Columbia: recruiting, training, organizing, deploying, and supporting community health teams in low income area of Columbia, South Carolina”
Geographic Reach: South Carolina
Funding Amount: $2,330,000
Estimated 3-Year Savings: $14,817,600
Summary: Eau Claire Cooperative Health Centers, Inc., in partnership with the Select Health Managed Care Organization, is receiving an award for a project aimed at improving health outcomes for populations in underserved, low-income areas of Columbia, South Carolina. Eau Claire will use health care teams of nurse practitioners, registered nurses, and community health workers affiliated with a Federally Qualified Health Center to provide patient education, home visits, and care coordination, leading to reduced use of high cost health care services, including emergency room visits and hospitalizations, improved self-management for patients with chronic conditions, a decrease in low birth weight infant care, and improved health outcomes in general. Payers have agreed to reimburse a portion of cost savings.
Over a three-year period, Eau Claire Cooperative Health Centers will create an estimated 22 health care-related jobs, including positions for peer health workers, registered nurses, Nurse Practitioners, a project director, and a community organizer.
SUTTER HEALTH
Project Title: “Advanced Illness Management (AIM)”
Geographic Reach: California
Funding Amount: $13,000,000
Estimated 3-Year Savings: $29,388,894
Summary: Sutter Health is receiving an award to expand their Advanced Illness
Management program (AIM) across the entire Sutter Health system in Northern California, serving patients who have severe chronic illness but are not ready for hospice care, are in clinical, functional, or nutritional decline, and are high-level consumers of health care. Such patients generally experience poor care quality, but account for a disproportionate share of Medicare spending. AIM addresses these issues through a complex medical home model that uses nurse-led interdisciplinary teams to coordinate and deliver care that encourages patient self-management of chronic illness that modifies disease course and provides symptomatic relief. The program will improve care and patient quality of life, increase physician, caregiver, and patient satisfaction, and reduce Medicare costs associated with avoidable hospital stays, emergency room visits, and days spent in intensive care units and skilled nursing facilities.
Over a three-year period, the Sutter Health’s program will train an estimated 192 workers and will create an estimated 89 jobs. The new workforce will include training care transition teams comprised of social workers, nurse practitioners, clinical pharmacists, and home care aides.
THE TRUSTEES OF THE UNIVERSITY OF PENNSYLVANIA
Project Title: “A rapid cycle approach to improving medication adherence through incentives and remote monitoring for coronary artery disease patients”
Geographic Reach: New Jersey, Pennsylvania
Funding Amount: $4,841,221
Estimated 3-Year Savings: $2,787,030
Summary: The University of Pennsylvania is receiving an award for a program to improve medication adherence and health outcomes in post-discharge patients who are recovering from acute myocardial infarctions in metropolitan Philadelphia and adjoining areas of New Jersey. Such patients typically have high rates of poor medication adherence and hospital readmissions and are costly to monitor through intensive case management. The intervention will increase medication adherence through telemonitoring and a visual and audible “reminder” system. It will also retrain social workers as engagement advisors to monitor adherence, offer incentives, and enlist patient support from family and friends. The result will be improved health outcomes and lower cost. The investments made by this grant are expected to generate cost savings beyond the three year grant period.
Over a three-year period, the Trustees of the University of Pennsylvania’s program will train an estimated 21 workers, while creating an estimated seven jobs for investigators, clinical social workers, clinical nurses, software programmers, project co-directors, and a project director.
UNIVERSITY OF HAWAII AT HILO
Project Title: “Pharm2Pharm, a formal hospital pharmacist to community pharmacist collaboration”
Geographic Reach: Hawaii
Funding Amount: $14,346,043
Estimated 3-Year Savings: $27,114,939
Summary: The University of Hawaii at Hilo and its College of Pharmacy, in partnership with Hawaii Health Systems Corporation and Hawaii Pacific Health, community pharmacies in rural counties of Hawaii, the Hawaii Health Information Exchange, and Hawaii Health Information Corporation, is receiving an award to improve medication reconciliation and management for the elderly in three rural counties of Hawaii. The program will integrate pharmacists into hospital and ambulatory care teams and use health information technology for decision-making support and to enhance communication, particularly between hospital pharmacists and community pharmacists. The result will be better care transitions, a reduction in adverse events, improved medication adherence, and better-informed, more patient-centered decisions about medication therapies, leading to reduced hospitalizations, readmissions, and emergency room visits and better health care and health for the patients served. Over a three-year period, the University of Hawaii at Hilo’s program will train new workers including a pharmacist project coordinator, a certified project management professional, a physician leader/care transition expert, a measurement and evaluation expert, a contracts administrator, and an administrative assistant.
UNIVERSITY OF IOWA
Project Title: “Transitional care teams to improve quality and reduce costs for rural patients with complex illness”
Geographic Reach: Iowa
Funding Amount: $7,662,278
Estimated 3-Year Savings: $12,500,000
Summary: The University of Iowa, in partnership with the 11 hospitals comprising its Critical Access Hospital Network, is receiving an award to improve care coordination and communication with practitioners in ten rural Iowa counties. The program will serve Medicare, Medicaid, and Medicare/Medicaid dual-eligible beneficiaries and privately insured and uninsured patients who have complex illness, including psychiatric disorders, heart disease, kidney disease, cancer, endocrine and gastrointestinal disorders, and geriatric issues. The program will coordinate care through teams comprised of nurses, social workers, and pharmacists along with specialty physicians (including psychiatrists) using telehealth and web-based personal health records. The program is based on the University of Iowa's significant past experience in creating telehealth care teams for patients with diabetes, chronic obstructive pulmonary disease, and heart failure. It will increase access to services and specialty care, improve care transitions and care coordination, and decrease avoidable hospital readmissions of complex patients in rural counties in Iowa.
Over a three-year period, the University of Iowa's program will train an estimated 22 workers and will create an estimated 28 jobs. The new hires will include eleven community coordinators, two project managers, a program secretary, an outcomes analyst, a qualitative analyst, a database manager, nurse team leaders, social workers, and an informatics director.
UNIVERSITY OF SOUTHERN CALIFORNIA
Project Title: “Integrating clinical pharmacy services in safety-net clinics”
Geographic Reach: California
Funding Amount: $12,007,677
Estimated 3-Year Savings: $43,716,000
Summary: The University of Southern California is receiving an award to integrate clinical pharmacy services into safety net clinics, providing medication therapy management, disease state management, medicine reconciliation, medication access services, patient counseling, drug information education, preventive care programs, provider education, and quality improvement review for care providers and for the underserved and vulnerable populations of Santa Ana, Huntington Beach, and Garden Grove. This will improve medication adherence, confirm the appropriateness and safety of medication use, and reduce avoidable hospitalizations and emergency room visits, while improving patient and population health.
Over a three-year period, The University of Southern California program will train an estimated 17 workers and will create an estimated 27 jobs. The new workforce will include a programmer, a project manager, six pharmacists, and six pharmacy residents. Additionally, this program will partner with the East Los Angeles Occupational Center technician training program to develop curricula that will expand the roles of the 11 pharmacy technicians who will be trained to perform patient navigator and data management duties in clinical pharmacy teams.
UNIVERSITY OF TENNESSEE HEALTH SCIENCE CENTER
Project Title: “Project SAFEMED”
Geographic Reach: Tennessee
Funding Amount: $2,977,865.
Estimated 3-Year Savings: $3,160,844
Summary: The University of Tennessee Health Science Center, in partnership with Methodist LeBonheur Healthcare's Methodist North Hospital and Methodist South Hospital, QSource, United Healthcare, BlueCross BlueShield and its BlueCare Medicaid plan, Southwest Tennessee Community College, the Tennessee Pharmacists Association, and the Bluff City, Bin Sina, and Memphis Medical Societies, is receiving an award to improve medication adherence and effective medication usage among high-risk patients in the northwest and southwest sections of Memphis, TN. The program will serve vulnerable adults (20-64) and seniors 65+ insured by Medicaid and/or Medicare who have multiple chronic diseases, including hypertension, diabetes, coronary artery disease, congestive heart failure, and chronic lung disease, as well as polypharmacy and high-inpatient utilization. Through care teams of pharmacists, nurse practitioners, pharmacy technicians, and licensed practical nurse outreach workers based in outpatient centers, the program will work with primary care physicians and local pharmacies to provide comprehensive medication management. This approach will reduce avoidable prescription drug utilization, prevent adverse drug events, reduce resulting patient morbidity and mortality, reduce avoidable hospital admissions, and lower cost. At the same time, it will improve medication adherence, disease management, and patient health. Over a three-year period, the University of Tennessee Health Science Center's program will train an estimated 8 workers, while creating an estimated 11 jobs. The new positions will include outreach workers, outreach directors, and pharmacy technicians.
In addition to the HCIA awards, CMMI has established several ACO programs that integrate pharmacists as clinical practitioners or involve a pharmacy organization, including but not limited to, Fairview Health System (MN), Park Nicollet (MN), Coastal Medical (RI), and Walgreens (TX, NJ, FL).
REFERENCES
- 1.Agency for Healthcare Research and Quality. Patient Centered Medical Home Resource Center. Defining the PCMH. http://pcmh.ahrq.gov/portal/server.pt/community/pcmh__home/1483/PCMH_Defining%20the%20PCMH_v2. Accessed July 29, 2013.
- 2.AcademyHealth. AcademyHealth Research Insights Project. Medical homes and accountable care organizations: if we build it, will they come? http://www.academyhealth.org/files/publications/RschInsightMedHomes.pdf. Accessed July 29, 2013.
- 3.Medicaid.gov. Health Homes. http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Long-Term-Services-and-Support/Integrating-Care/Health-Homes/Health-Homes.html. Accessed July 29, 2013.
- 4.Taylor EF, Lake T, Nysenbaum J, Peterson G, Meyers D. Coordinating Care in the Medical Neighborhood: Critical Components and Available Mechanisms. White Paper (Prepared by Mathematica Policy Research under Contract No. HHSA290200900019I TO2). AHRQ Publication No. 11–0064. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [Google Scholar]
- 5.HealthCare.gov Glossary. http://www.healthcare.gov/glossary/a/accountable.html. Accessed July 29, 2013.
- 6.HealthAffairs.org. Health Policy Briefs. Next steps for ACOs. http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=61. Accessed July 29, 2013.
- 7.Medicare Payment Advisory Commission Report to the Congress, June 2009. Improving Incentives in the Medicare Program. Chapter 2. Accountable care organizations. http://www.medpac.gov/chapters/Jun09_Ch02.pdf. Accessed July 29, 2013.
- 8.Punke H. Five payment models for ACO providers. Becker’s Hospital Review. ASC Communications, December 28, 2012. http://www.beckershospitalreview.com/hospital-physician-relationships/5-payment-models-for-aco-providers.html. Accessed July 29, 2013.
- 9.Farley R. Community care organizations (ACOs for the rest of us). Mental Healthcare Reform. National Council for Community Behavioral Healthcare. August 16, 2011. http://mentalhealthcarereform.org/community-care-organizations-acos-for-the-rest-of-us/. Accessed July 29, 2013.
- 10.Centers for Medicare and Medicaid Services Demonstration Projects. Solicitation for applications community-based care transitions program. 2011 http://www.cms.gov/Medicare/Demonstration-Projects/DemoProjectsEvalRpts/downloads/CCTP_Solicitation.pdf. Accessed July 29, 2013. [Google Scholar]
- 11.Oregon Health Policy Board. Coordinated care organizations. http://www.oregon.gov/oha/OHPB/Pages/health-reform/certification/index.aspx. Accessed July 29, 2013.
- 12.Interprofessional Education Collaborative. Core competencies for interprofessional collaborative practice. Report of an Expert Panel. May 2011. http://www.aacn.nche.edu/education-resources/ipecreport.pdf. Accessed July 29, 2013.
- 13.AMCP-ACPE Task Force. Entry-level competencies needed for managed care pharmacy practice. Spring 2012. https://www.acpe-accredit.org/pdf/AMCPACPETaskForce2012.pdf. Accessed July 29, 2013.
- 14.ASHP-ACPE Task Force. Entry-level competencies needed for pharmacy practice in hospitals and health-systems. Fall 2010. https://www.acpe-accredit.org/pdf/EntryLevelCompetenciesNeededForPharmacyPracticeHospitalsandHealthSystems.pdf. Accessed July 29, 2013.
- 15.NACDS Foundation-NCPA-ACPE Task Force. Entry-level competencies needed for community pharmacy practice. Spring-Summer 2012. https://www.acpe-accredit.org/pdf/NACDSFoundation-NCPA-ACPETaskForce2012.pdf. Accessed July 29, 2013.
- 16.Partnership for Health in Aging. Multidisciplinary competencies in the care of older adults at the completion of the entry-level health professional degree. http://www.americangeriatrics.org/files/documents/health_care_pros/PHA_Multidisc_Competencies.pdf. Accessed July 29, 2013.
- 17.Giberson S, Yoder S, Lee MP. Improving patient and health system outcomes through advanced pharmacy practice: a report to the U.S. Surgeon General 2001. Office of the Chief Pharmacist. U.S. Public Health Service. December 2011. [Google Scholar]
- 18.Patient-Centered Primary Care Collaborative. The opportunity for comprehensive medication management within the patient-centered medical home structure. http://wwww.pcpcc.net/files/Opportunity-for-Comprehensive-Medication-Management.pdf. Accessed July 29, 2013.
- 19.Centers for Medicare & Medicaid Services. Health, United States, 2008: with special feature on the health of young adults. http://www.cdc.gov/nchs/data/hus/hus08.pdf. Accessed July 29, 2013. [PubMed]
- 20.National Committee for Quality Assurance. NCQA certifies first medical home content experts. May 10, 2013. http://www.ncqa.org/Newsroom/2013NewsArchives/NewsReleaseMay102013.aspx. Accessed July 29, 2013.
- 21.Leavitt Partners. Center for Accountable Care Intelligence [home page] http://leavittpartners.com/aco-consulting/. Accessed July 29, 2013.


