Abstract
Objective. To assess the effectiveness of virtual patient cases to promote self-directed learning (SDL) in a required advanced therapeutics course.
Design. Virtual patient software based on a branched-narrative decision-making model was used to create complex patient case simulations to replace lecture-based instruction. Within each simulation, students used SDL principles to learn course objectives, apply their knowledge through clinical recommendations, and assess their progress through patient outcomes and faculty feedback linked to their individual decisions. Group discussions followed each virtual patient case to provide further interpretation, clarification, and clinical perspective.
Assessments. Students found the simulated patient cases to be organized (90%), enjoyable (82%), intellectually challenging (97%), and valuable to their understanding of course content (91%). Students further indicated that completion of the virtual patient cases prior to class permitted better use of class time (78%) and promoted SDL (84%). When assessment questions regarding material on postoperative nausea and vomiting were compared, no difference in scores were found between the students who attended the lecture on the material in 2011 (control group) and those who completed the virtual patient case on the material in 2012 (intervention group).
Conclusion. Completion of virtual patient cases, designed to replace lectures and promote SDL, was overwhelmingly supported by students and proved to be as effective as traditional teaching methods.
Keywords: virtual patients, technology, self-directed learning, simulation, virtual learning
INTRODUCTION
Empowering individuals to take responsibility for decisions related to their learning can facilitate knowledge and skill development and promote self-directed learning (SDL). In 1975, American adult educator Malcolm Knowles described SDL as a process in which educators become facilitators, and learners take the initiative to recognize knowledge deficits, determine learning goals, identify credible learning resources, implement plans, and evaluate those plans for success.1 Gibbons defined SDL as any increase in knowledge, skill, accomplishment, or personal development that an individual brings about by his or her own efforts “using any method in any circumstances at any time.”2 Self-directed learning challenges the assumption that learning can take place only in the presence of accredited teachers, and SDL efforts can meet the many challenges associated with keeping current on constantly changing knowledge. Furthermore, self-direction in one’s learning can and should be viewed as a characteristic that exists in every person.3
In medical schools, SDL is an essential methodology in the promotion of life-long learning. Curricula are to “provide opportunities to develop life-long learning skills, including self-assessment of learning needs; independent identification, analysis, and synthesis of relevant information; and the appraisal of credible information sources.”4 Medical residents are expected to be self-directed; evaluating their learning with innovative tools such as computerized diaries and portfolios.5 In pharmacy colleges and schools, programs are expected to assist students to assume responsibility for their own learning, including assessment of learning needs; development of personal learning plans; and self-assessment of the level of their skills and attitudes.6 Faculty members are urged to develop teaching and learning methods that enable students to transition from dependent to “active, self-directed, life-long learners.”7
In response to the visions set forth by accreditation and education councils of the health sciences, universities have adopted SDL as a tool to life-long learning, and a high-level objective or goal of their curricula. For example, graduates at the University of Pittsburgh School of Medicine are expected to “demonstrate a commitment to life-long pursuit of learning,”8 while University of Pittsburgh School of Pharmacy graduates, “… should be life-long learners who are able to recognize knowledge and skill deficits, formulate a learning plan, locate and interpret credible resources, and assess progress toward meeting learning goals.”9
Though faculty members are responsible for providing a climate of learning that emphasizes SDL, enforcing the skills and attitudes necessary for its wholesale adoption can be neglected, and SDL principles can become assumed rather than imposed. As a result, despite numerous examples of SDL strategies published in the literature over the past decade,10-16 trainees rarely receive explicit instruction in how to manage their own learning and their education is dominated by an “unreflective doing.”11,17 Developing competence in SDL goes beyond acquiring a set of skills that allow the learner to solve problems. It involves the installation of an androgogic attitude towards learning, and for educators, it means preparing pharmacy graduates for a lifetime of learning. While classroom lectures, a common teaching method in higher education, may allow faculty members to disseminate large amounts of information to a vast number of students, it does little to promote the skills and attitudes of SDL.
While there has not been a study describing the use of virtual patients specifically to enforce SDL principles, studies suggesting the use of virtual patients to promote SDL have been published.18-20 Virtual patients have been defined as computer programs that simulate lifelike clinical scenarios in which the learner becomes the health care professional making therapeutic decisions.21 Virtual patients allow educators to assess student decision-making skills regarding course content in a safe, high-fidelity environment, while allowing students to learn and err in private.22 Patient simulation via virtual patient software has been used throughout higher education by multiple disciplines.23-30
The design, development, implementation, and assessment of a novel approach to integrate the skills and attitudes of SDL into an advanced therapeutics course within a pharmacy curriculum using virtual patient software is described. This teaching strategy combines educational technology with principles of social learning in order to supplant lecture and support learners in exercising autonomy related to the learning endeavor. Throughout this manuscript, SDL will be defined as the development of the skills and attitudes necessary to become an independent, confident, and life-long adult learner.
DESIGN
Faculty members of the University of Pittsburgh School of Pharmacy purposed to modify the school’s pedagogy to foster a learning environment centered on SDL. A teaching strategy was implemented that combined virtual patients that were designed to replace classroom lectures with principles of social learning. Goals developed to realize this purpose included: (1) to develop virtual patient cases that emphasized the principles of SDL and were capable of teaching course content; (2) to replace conventional teaching methods with virtual patient cases; (3) to enhance the quality of faculty contact time with students through the principles of social learning.
Faculty members used vpSim/DecisionSim virtual patient software (Decision Simulation LLC, Chadsford PA) developed by the Laboratory for Educational Technology at the University of Pittsburgh, to achieve project goals. Virtual patient cases developed through the vpSim platform make use of a branched-narrative model in which learners are presented with a challenge, given choices, and then provided with a consequence specific to their choice. Use of this model allows learner input to directly affect the outcomes of the virtual patient where appropriate recommendations will improve the simulated patient’s condition, whereas suboptimal recommendations will worsen it. In vpSim, students become healthcare providers, making recommendations in authentic clinical scenarios. A more detailed description of this platform has been published.31
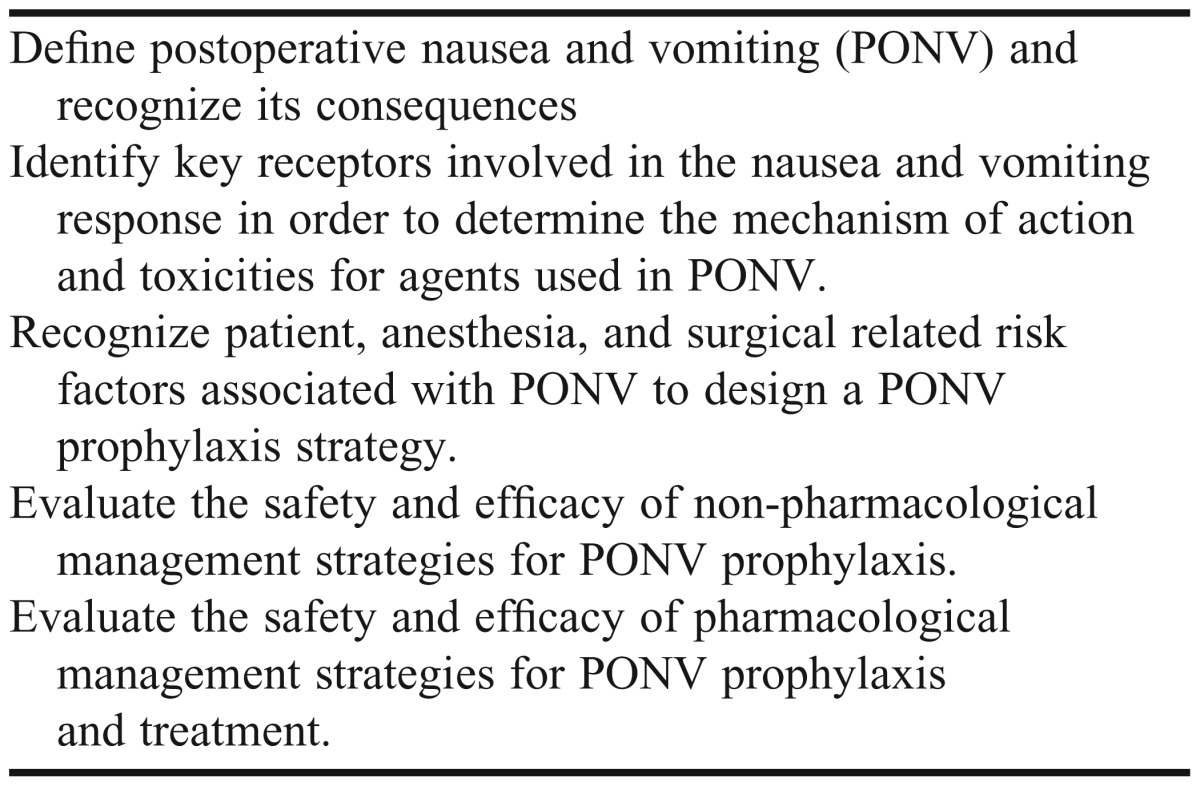
Branching throughout the simulation is unique to vpSim and was pivotal to this project. The decisions students make within the virtual patient software allowed for an individualized experience and the formation of a “learning path” specific to each student. The learning path was defined as the sequential decisions or recommendations made by the student in completing the simulation and the associated individualized feedback. By way of this learning path, students interacted with the course content and practiced SDL principles. Specifically, each learning path made available to students in the virtual patient software was structured so that course objectives (Table 1) were encountered through (1) recognition of knowledge deficits, (2) determination of learning goals, (3) identification of credible resources, (4) initiation of a plan, and (5) monitoring for the success of that plan. For example, student learning paths began with a complex patient scenario followed by a teaching tutorial meant to provide insight into the patient case and instruction of course objectives. Students were then asked to make a myriad of clinical decisions based on their understanding of tutorial content, and consequently course objectives. Students making appropriate decisions were re-challenged with more detailed questions to ensure understanding of content. Students answering incorrectly to any questions were directed to specific tutorials that allowed for further learning objective development and reinforcement of clinical skills.
Table 1.
Learning Objectives Developed for Postoperative Nausea and Vomiting Virtual Patient Case Construction
Periodic quizzes and challenge screens were embedded into the simulation to test students’ knowledge and skill levels. These assessments allowed students to gauge their progress towards course objectives and allowed faculty members to measure student learning. Additionally, a “summary” screen was presented to students at the conclusion of the simulation outlining their unique learning path. This summary screen allowed students to assess their individual progress towards course objectives as well as gauge their success with the SDL process.
Simulation content was derived from subject matter in Advanced Pharmaceutical Care II, a required 2-credit therapeutics course for third-year doctor of pharmacy (PharmD) students.23 The course had regularly used completion of virtual patient cases via vpSim as a supplement to lecture, however, a strategy to use virtual patients to replace lecture and promote SDL has not been previously implemented.
For academic year 2012, the teaching virtual patients developed by course faculty members replaced lecture as the primary means of teaching foundational knowledge and skills of specific content in the course. Student completion of the simulations was mandatory prior to scheduled lecture time, but students were not graded on their success through the session. The virtual patients provided students “on-demand” curricular content as they were able to access and practice with the virtual patients as many times as they deemed necessary throughout the semester.
Three simulations were developed, replacing 3 of the 26 lecture hours in the course. The design of all 3 simulations followed an identical template, which was briefly outlined above. Specific lectures that were converted into virtual patients included postoperative nausea and vomiting, chronic kidney disease, and anemia of chronic kidney disease. Faculty members chose these lectures based on length and position in the course’s overall lecture series. For example, 1-hour lectures were more readily transformed into a virtual patient than 2-hour lectures. Also, faculty members did not want to disrupt the continuity of a “multi-lecture series” with a new teaching methodology.
By using the virtual patient cases to deliver foundational knowledge to students, faculty members could offer students a richer learning experience that maximized student-to-student and faculty-to-student interactions. This promoted the social learning principles of live modeling, verbal instruction, and symbolic modeling in order for students to gain further interpretation, clarification, and clinical perspective of course content.32 Social learning theorizes that learning occurs within a social context and that people learn from one another through the principles listed above.33 A large-group discussion was developed to follow completion of each virtual patient case. These discussions were designed to be led by students and facilitated by faculty members. Rather than passively learning course objectives through lecture, students actively applied the knowledge and skills that were developed through completion of the virtual patient cases. Learning was personalized as students used this time to debate aspects of course objectives and the virtual patient case. Individual students (or student groups) were called upon to elaborate on their decision making at pivotal points in the virtual patient case. The class then received feedback from faculty members as to the significance and impact of these decisions. At this point, faculty members could provide insight into how an expert might view or reason through a similar clinical scenario, promoting the live model principle of social learning.
Faculty members also endorsed the symbolic modeling principles of social learning through virtual-patient media. Specific components of the case were broken down so that students could understand the purpose behind the development of key segments. For example, faculty members were able to illustrate how an understanding of one concept (ie, risk factors) directly affected the student’s decision making regarding a seemingly unrelated concept (ie, nonpharmacological prophylaxis strategies). Additionally, faculty members were able to demonstrate the importance of “learning to understand” vs “superficial recall” and how failure to grasp specific objectives manifested in a negative virtual patient outcome. A proposal submitted to the investigational review board at the University of Pittsburgh regarding investigation into the effectiveness of this teaching methodology was approved under an exempt status.
EVALUATION AND ASSESSMENT
Learning of postoperative nausea and vomiting objectives using conventional teaching methods was collected from 106 students enrolled in the course in 2011 (Figure 1). Students’ baseline knowledge was evaluated by a multiple-choice pretest and knowledge acquisition was measured through a multiple-choice posttest. Retention of knowledge was evaluated by questions on the final examination. Pretest, posttest, and examination questions were not identical, but were designed to be similar in both content and difficulty. Similar content was achieved by constructing all tests from the same predefined learning objectives. Also, an equal number of learning objectives were measured between each set of tests. Similar question difficulty between the tests was ensured by designing each question to assess a specific learning activity level within Bloom’s Taxonomy.34 An equal number of learning activity levels were assessed between tests as well. Following the design of the pretest, posttest, and examination questions, face validity was established through (1) an expert pharmacy faculty panel and (2) testing pharmacists and student pharmacists at varying levels of training (ie, fourth-year student, first-year resident, second-year resident, and pharmacy faculty member).
Figure 1.
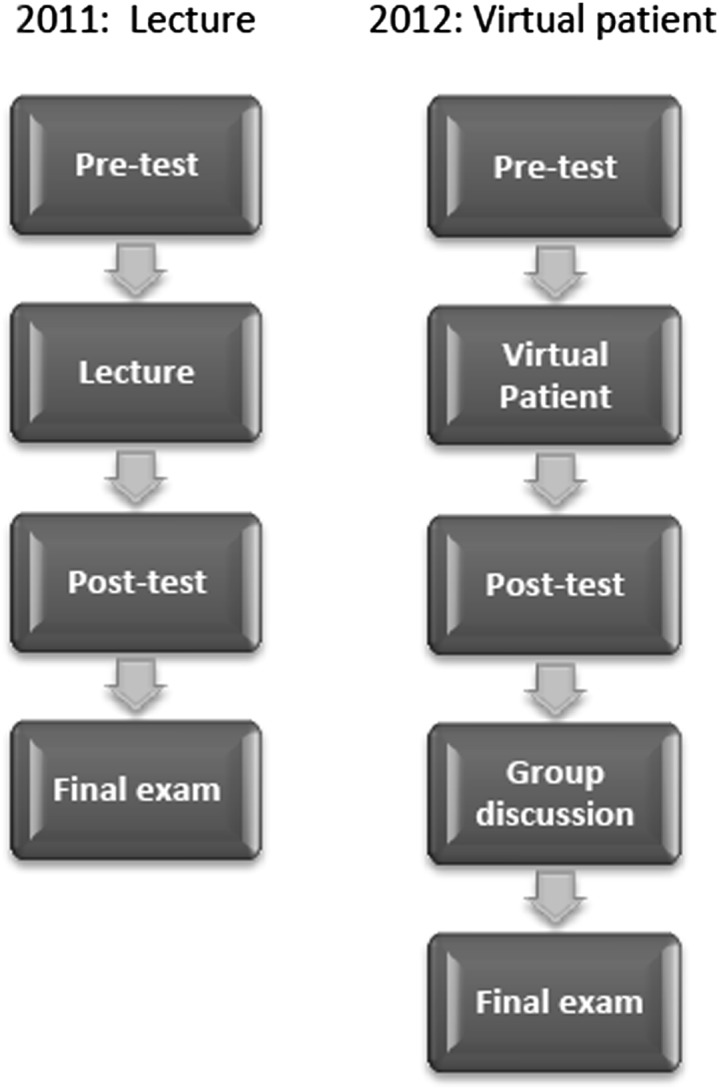
Flow diagrams depicting the evaluation and assessment of conventional teaching methods and the new teaching method.
To evaluate learning and knowledge retention using the new teaching method, identical pretest, posttest, and final examination questions were administered to 106 students in the 2012 class (Figure 1). Students in the 2012 class did not have access to tests and examinations from the previous year. Ability of the teaching strategies to promote learning and knowledge retention was evaluated by comparing the pretest, posttest, and final examination scores of academic year 2011 to corresponding scores of the 2012 class. Students’ perceptions and satisfaction were collected by survey instruments administered at the end of the term. At no point did results from pretests, posttests, or satisfaction survey instruments affect the students’ overall grade in this course. Students were mandated to complete all simulations for the course but could withdraw from the research (surveys, pretests, posttests) at any time.
Perceptions of using virtual patient cases to replace lecture were collected from 68 students (Table 2). Students were considered to be in agreement with each statement if they indicated “to a moderate degree,” “to a considerable degree,” or “to a very high degree.” The majority of students found the virtual patient modules/portion of the course to be organized (90%), appropriate in content (88%), enjoyable (82%), intellectually challenging (97%), and contributing to their understanding of course content (91%). Students also indicated that completion of the virtual patient cases prior to class permitted better use of class time (78%), in addition to allowing students to become better self-directed learners (84%). Only 7% and 5% of students answered “hardly at all” to the previous 2 statements, respectively. However, when asked to rank their preferred learning method in acquiring new knowledge (Table 3), students chose direct instruction (37%) over virtual patients (30%) and problem-based learning (PBL) (26.5%).
Table 2.
Third-Year Pharmacy Students’ Perceptions of Teaching Methodology That Included Virtual Patient Casework and Large Group Discussion
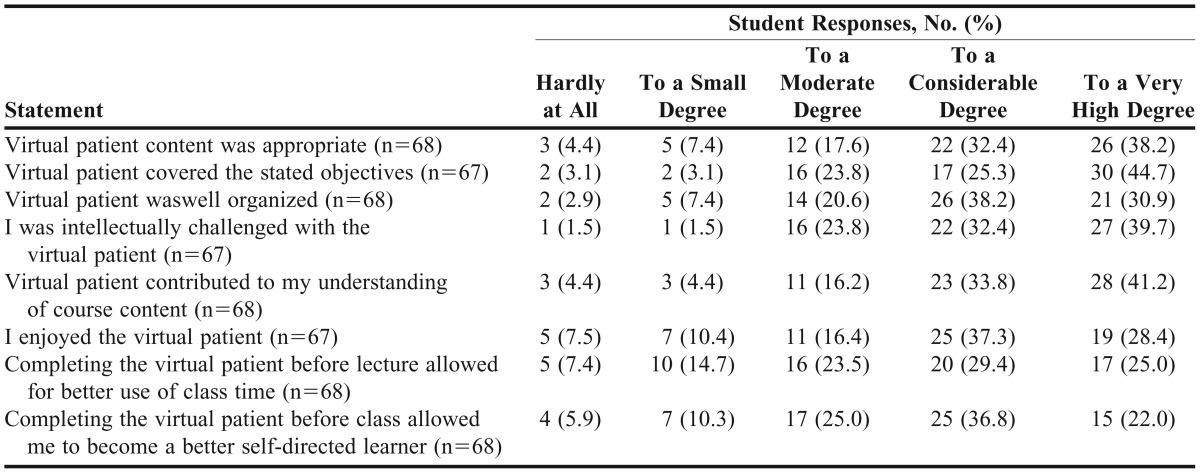
Table 3.
Learning Preferences for Knowledge Acquisition Reported by Students After Exposure to Virtual Patient Casework and Large Group Discussions (n=68)
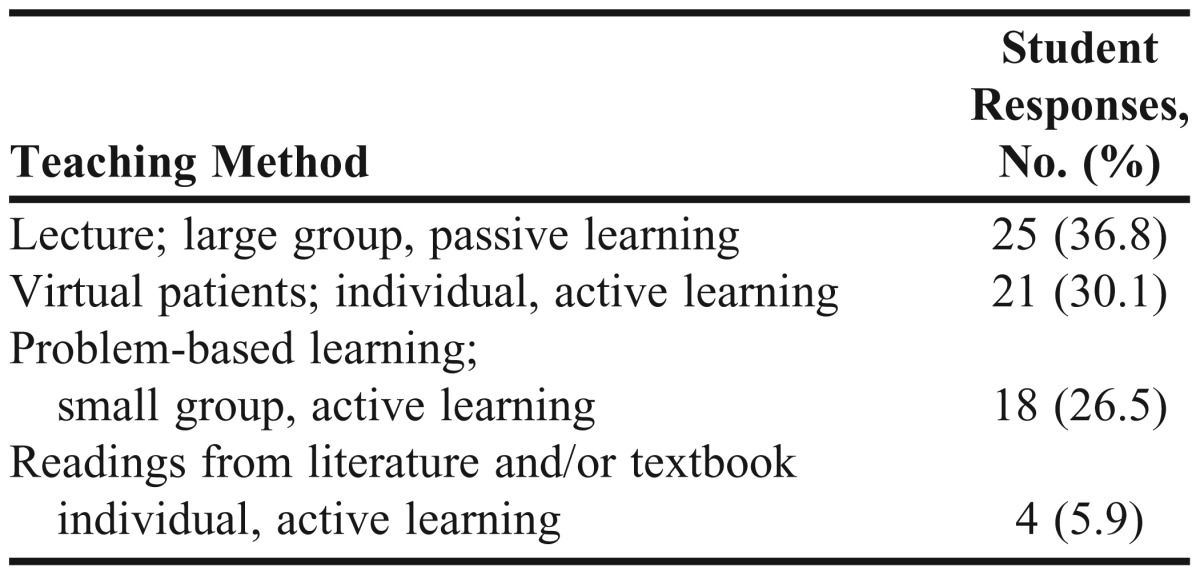
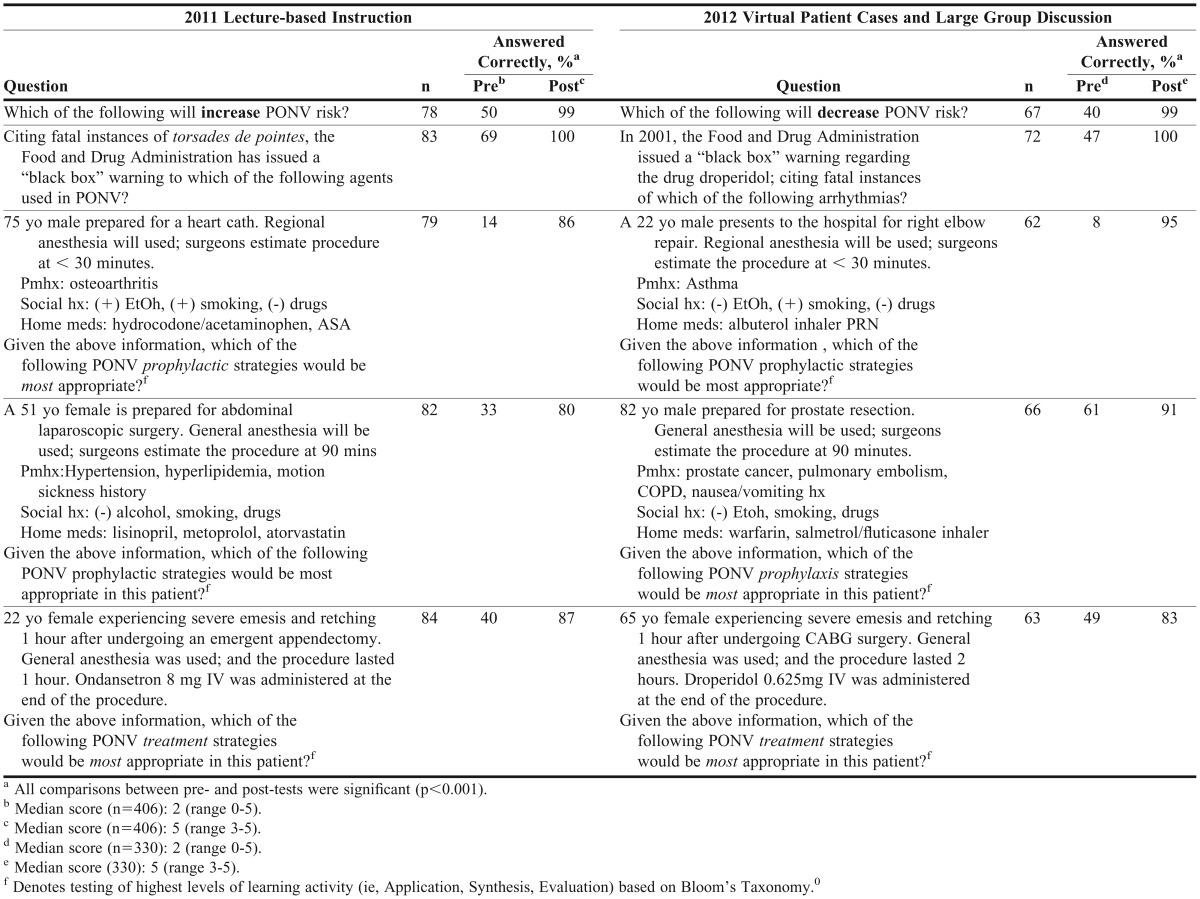
Table 4 summarizes the effectiveness of the teaching methodology in comparison to classroom lectures. Pretest and posttest scores with each teaching methodology for postoperative nausea and vomiting were evaluated. All students’ scores on each question improved significantly (p<0.001) from pretest to posttest for both academic years 2011 and 2012. Median scores increased significantly (2 to 5; p<0.001) from pretest to posttest in both academic years as well.
Table 4.
Comparison of Correct Responses on Examination Questions Between Third-Year Pharmacy Students Learning Through Lectures and Those Learning Through Virtual Patient Casework With Large Group Discussion
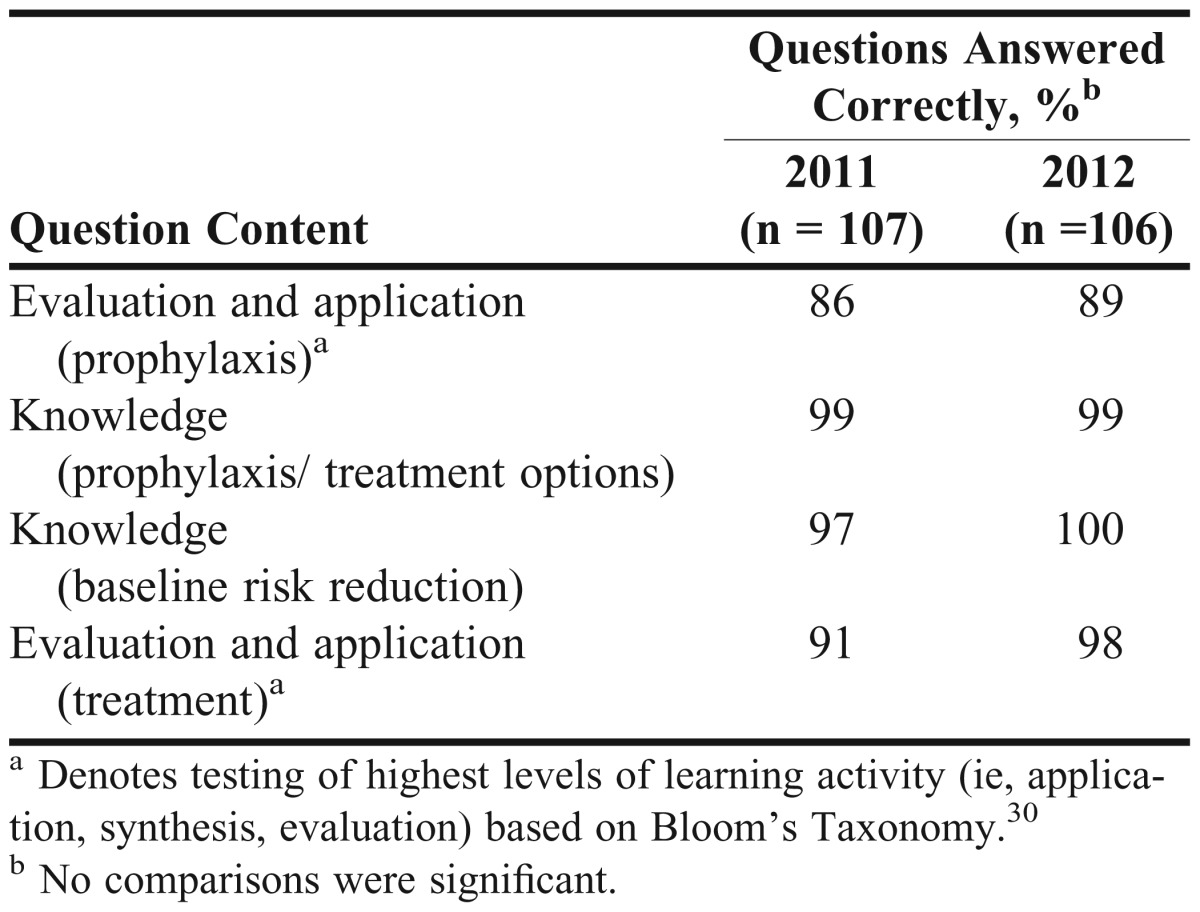
Retention of postoperative nausea and vomiting concepts, captured from final examination scores, was similar in both groups 86% vs 89%, p<0.920) for question 4 and 91% vs 98% (p<0.695) for question 28) (Table 5). No difference was found between academic years 2011 and 2012.
Table 5.
Student Final Examination Scores for Postoperative Nausea and Vomiting Questions in Academic Years 2011 and 2012
DISCUSSION
Instructors of health science curricula are tasked with developing teaching methods that can facilitate learning while instilling a sense of professionalism, critical thinking, and life-long learning consistent with contemporary practitioners and adult learners.4,6 Self-directed learning is a necessity for life-long learners, a vital component to critical-thinking, and an essential for graduates of higher education. While SDL is recognized by many curricula to be imperative for student development,8,9 its principles can be overlooked and assumed rather than enforced.11,17 Consequently, the design and development of strategies for higher education faculty members to teach fundamental knowledge and skills using the tenets of adult learning, such as SDL, are crucial if programs hope to graduate independent professionals with effective problem-analysis skills.
The project goals were achieved in that 3 virtual patient cases were designed, developed, and implemented to promote the principles of SDL and replace lectures, without compromising learning integrity. This teaching method is capable of personalizing learning for students, while offering faculty members an alternate approach to facilitate learning of new knowledge and skills. Our strategy incorporated educational technology with social learning principles in motivating students to practice a degree of autonomy as it related to the learning endeavor. This teaching method substituted lecture with virtual patient cases, cultivating an SDL attitude in students as they took responsibility for what and how they should learn course objectives. In addition, all learning paths within the virtual patient cases introduced and emphasized the principles of SDL so that students could practice the skill. Finally, large group discussion followed each virtual patient case, emphasizing social learning principles and allowing for further refinement of students’ knowledge and skills.
Student satisfaction was high with this teaching method and met the expectations of millennial students who are digital natives and consequently more acclimated to learn in a technology-enhanced environment.35 Similar to previously published virtual patient studies in higher education,23,24,28,36-38 our students found completion of virtual patient cases to be helpful, enjoyable, and challenging. The majority of students (78%) indicated that replacing lecture with virtual patients cases allowed for better use of faculty contact time with them. Most students also agreed (84%) that completing the virtual patient prior to class allowed them to become better self-directed learners.
However, despite positive reviews, students chose lectures over virtual patient technology and PBL when asked to rank their preferred learning methods to acquire new knowledge. This was a surprising yet somewhat expected finding, likely reflecting the view that some individuals are incapable of engaging in SDL because of lack of independence, lack of confidence, and/or lack of resources.39 Not all learners prefer the self-directed option and many educators question its worth.40,41 To compound the issue, our students are likely in a cognitive transition from adolescent to more adult-learning behaviors. Only 44% of first-year pharmacy students at the University of Maryland achieved a “high” SDL readiness score.42 This is comparable to results from our study, as only a third of third-year pharmacy students indicated that they would prefer to develop new knowledge through SDL.
These data are further evidence of the need for faculty members to develop innovative strategies to teach foundational concepts through adult-learning principles. Researchers have theorized that when students’ formal schooling consists of passively receiving information from instructors, their skills at monitoring and managing their own learning may be poorly developed and their commitment to actively manage their own learning will be lacking.43 This is likely the case with the pharmacy students in this study as most preferred listening to a lecture over participating in learning strategies that incorporated SDL for new knowledge and skill acquisition. Self-directed learning is both a set of skills to be developed and an attitude towards learning. While students may be required to practice the skill (eg, recognize knowledge deficits, develop learning goals, etc), a commitment to learning through SDL must be made by the individual.
As mentioned above, our teaching strategy may have subjected students to a learning environment with which many were unaccustomed. Most of the students had been exposed to 16+ years of conventional, lecture-based, passive-learning techniques. Introducing an educational technology to supplant their traditions, perceptions, and expectations of learning was both novel and radical. Despite this, results from pretests, posttests, and final examinations showed student learning and knowledge retention to be equivalent to established techniques. Students improved significantly from pretest to posttest in the group of students who were taught course objectives through lectures and the group of students who were taught the same material through virtual patient cases. Similarly, students did remarkably well on final examination questions related to postoperative nausea and vomiting; even in questions testing higher levels of learning activity and no difference was found when comparing final examinations scores between the 2 groups.
The potential advantages of this innovative approach to students and faculty members should not be overshadowed by the absence of demonstrable benefits from this study. While student expectations were met and learning integrity was preserved, completion of virtual patient cases with large group discussion to promote SDL and replace lecture offers a multitude of other rewards. Faculty members can immerse students in a learning environment that promotes the skills and attitudes of SDL, an androgogic learning behavior central to the adult learner and contemporary healthcare professional. Active learning replaces passive instruction while students are provided on-demand curricular content. Learning can be personalized to the individual as students lead large group discussions and faculty members serve only as facilitators. The strategy enhances the teaching mission of the schools of pharmacy and medicine by promoting life-long learning principles through demonstration and repetition of SDL skills and attitudes.8,9 Finally, using virtual patient and group discussion to promote SDL and replace lecture aligns with the accreditation standards and educational outcomes of the health sciences, which expect curricula to provide opportunities to develop life-long learning skills and enable students to transition from dependent to active, self-directed learners.4-7
Obstacles to implementing any technology in the classroom can be grouped into 3 key areas: cultural, process, and academic.44 Cultural obstacles are those related to the attitudes of the institution towards technology and pedagogy. Process obstacles address workflow assessments to ensure seamless adoption. Academic obstacles deal with the degree to which the technology meets the pedagogical goals of the university or the extent to which the technology enhances the educator’s ability to engage students.
While any one of these obstacles is sufficient to derail the implementation of well-intentioned educational technology, we found process obstacles to be the most challenging. The faculty time commitment required to design, develop, and implement such a teaching strategy is extensive. The virtual patient teaching template alone took over 50 hours to create; however, now that the template has been developed, subsequent lectures can be readily converted into virtual patient teaching cases. Also, even though the students were encouraged to lead the large group discussion, careful preparation was required by faculty members in order to effectively facilitate the learning experience.
A second obstacle, and one that is more cultural in nature, involves student learning with our strategy. Not all students learn as effectively through virtual patient cases designed to promote SDL. Therefore, using multiple teaching methods in a course is necessary to ensure all learners are supported.
There were several limitations to this study. In the 2011 control group, students did well on posttests following the lecture which may be attributable to (1) the close proximity in time of delivery of the posttest questions and the learning technique, and (2) “cuing” from pretest questions taken only an hour before the posttest. Cuing was less of an issue for students in the virtual patient group as posttests were taken prior to the group discussion, which was typically days after completion of the virtual patient case.
An unexpected finding from the study was that students in the lecture group retained course content to the same degree as students in the virtual patient case group. While this may certainly be the case, it may also reflect a poor measure used to assess knowledge retention. From a qualitative perspective, the final examination may not truly measure “retention” as, among other confounders, most students review and relearn course content immediately before a final examination. Quantitatively, our analysis consisted of only 4 questions on the final examination. Hence, it is difficult to relate performance with method of instruction using final examination questions as the assessment. In the future, a better measure of knowledge retention might include an unscheduled test with 10 or more questions administered prior to the final examination, or some type of assessment administered after the course has concluded (ie, in the fourth year).
SUMMARY
Self-directed learning personalizes education to the learning needs of the individual, while motivating students to develop autonomy related to the learning endeavor. Self-directed learning skills are a necessity for life-long learners, a vital component to critical-thinking, an essential for graduates of higher education, and a characteristic that should be thought to exist in every person. Educational technologies may provide educators a means of implementing teaching methods that facilitate learning, while instilling a sense of professionalism, critical thinking, and self-directedness consistent with contemporary practitioners and adult learners. Through virtual patient cases and large group discussion, this project met the expectations of the millennial student, facilitated learning and knowledge retention, successfully replaced passive instruction with active learning, provided on-demand curricular content to students, enhanced the teaching mission of the schools, and aligned with accreditation standards and educational outcomes established for the health sciences.
ACKNOWLEDGEMENT
This project was funded by an Innovation in Education Award received in 2011 from the University of Pittsburgh Office of the Provost’s Advisory Council on Instructional Excellence. The authors thank Susan Meyer, PhD, Associate Dean of Education at the University of Pittsburgh School of Pharmacy, for her vision, guidance, and inspiration throughout this project. Authors gratefully acknowledge the support of the Laboratory for Educational Technology at the University of Pittsburgh.
REFERENCES
- 1.Knowles M. Self-Directed Learning: A Guide for Learners and Teachers. New York: Association Press; 1975. [Google Scholar]
- 2.Gibbons M. The Self-Directed Learning Handbook: Challenging Adolescent Student to Excel. San Francisco: Jossey-Bass Publishers; 2002. [Google Scholar]
- 3.Hiemestra R. Self-directed learning. In: Husen T, Postlethwaite TN, editors. The International Encyclopedia of Education, 2nd ed. Oxford: Pergamon Press; 1994. [Google Scholar]
- 4.Function and Structure of a Medical School. Standards for Accreditation of Medical Education Programs Leading to the MD Degree. http://www.lcme.org/functions.pdf. Accessed July 25, 2012. [Google Scholar]
- 5.Accreditation Council for Graduate Medical Education. ACGME program requirements. http://www.acgme-2010standards.org/pdf/Common_Program_Requirements_07012011.pdf Accessed June 3, 2012. [Google Scholar]
- 6.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed July 3, 2012. [Google Scholar]
- 7.Center for the Advancement of Pharmaceutical Education (CAPE) Educational outcomes 2004. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf. Accessed July 5, 2012. [Google Scholar]
- 8.University of Pittsburgh School of Medicine. Learning objectives of the MD curriculum. http://www.omed.pitt.edu/curriculum-committee/learning-objectives.php. Accessed January 26, 2012. [Google Scholar]
- 9.University of Pittsburgh School of Pharmacy. Curricular outcomes. http://wikis.pharmacy.pitt.edu/groups/PharmDHandbook/wiki/3db92/Curricular_Outcomes.html. Accessed January 28, 2011. [Google Scholar]
- 10.Murad MH, Varkey P. Self-directed learning in health professions education. Ann Acad Med Singapore. 2008;37(7):580–590. [PubMed] [Google Scholar]
- 11.Nothnagle M, Goldman R, Quirk M, Reis S. Promoting Self-directed learning skills in residency: a case study in program development. Acad Med. 2010;85(12):1874–1879. doi: 10.1097/ACM.0b013e3181fa02a4. [DOI] [PubMed] [Google Scholar]
- 12.Toumas M, Basheti I, Bosnic-Anticevich S. Comparison of small-group training with self-directed internet-based training in inhaler techniques. Am J Pharm Educ. 2009;73(5):Article 85. doi: 10.5688/aj730585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hastings J, West D. Comparison of outcomes between two laboratory techniques in a pharmacy communications course. Am J Pharm Educ. 2003;67(4):Article 101. [Google Scholar]
- 14.Conway S, Johnson J, Ripley T. Integration of team-based learning strategies into a cardiovascular module. Am J Pharm Educ. 2010;74(2):Article 35. doi: 10.5688/aj740235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strohfeldt K, Grant D. A model for self-directed problem-based learning for renal therapeutics. Am J Pharm Educ. 2010;74(9):Article 173. doi: 10.5688/aj7409173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sibbald D. A student assessment of the Virtual Interactive Case Tool For Asynchronous Learning (VITAL) and other self-directed learning formats. Am J Pharm Educ. 2004;68(1):Article 11. [Google Scholar]
- 17.Westberg J, Jason H. Fostering learners’reflection and self-assessment. Fam Med. 1994;26(5):278–282. [PubMed] [Google Scholar]
- 18.Conrad E, Kavia S, Burden D, et al. Virtual Patients in a virtual world: Training paramedic students for practice. Med. Teach. 2009;31(8):713–720. doi: 10.1080/01421590903134160. [DOI] [PubMed] [Google Scholar]
- 19.Jasinevicius R, Landers M, Nelson S, Urbankova A. An evaluation of two dental simulation systems: virtual reality versus contemporary non-computer-assisted. J Dent Educ. 2004;68(11):1151–1162. [PubMed] [Google Scholar]
- 20.Kandasamy T, Fung K. Interactive Internet-based cases for undergraduate otolaryngology education. Otolaryngol Head Neck Surg. 2009;140(3):398–402. doi: 10.1016/j.otohns.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 21.Huang G, Reynolds R, Candler C. Virtual patient simulation at US and Canadian medical schools. Acad Med. 2007;82(5):446–451. doi: 10.1097/ACM.0b013e31803e8a0a. [DOI] [PubMed] [Google Scholar]
- 22.Tworek J, Coderre S, Wright B, McLaughlin K. Virtual patients: ED-2 band-aid or valuable asset in the learning portfolio? Acad Med. 2010;85(1):155–158. doi: 10.1097/ACM.0b013e3181c4f8bf. [DOI] [PubMed] [Google Scholar]
- 23.Benedict N, Schonder K. Patient simulation software to augment an advanced pharmaceutics course. Am J Pharm Educ. 2011;75(2):Article 21. doi: 10.5688/ajpe75221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Orr KK. Integrating virtual patients into a self-care course. Am J Pharm Educ. 2007;71(2):Article 30. doi: 10.5688/aj710230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zary N, Johnson G, Boberg J, Fors U. Development, implementation and pilot evaluation of a web-based virtual patient case simulation environment-Web-SP. Med Educ. 2006;6:10. doi: 10.1186/1472-6920-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davids M, Chikte U, Halperin M. Development and evaluation of a multimedia e-learning resource for electrolyte and acid-base disorders. Adv Physiol Educ. 2011;35(3):295–306. doi: 10.1152/advan.00127.2010. [DOI] [PubMed] [Google Scholar]
- 27.Guise V, Chambers M, Välimäki M. What can virtual patient simulation offer mental health nursing education? J Psychiatr Ment Health Nurs. 2012;19(5):410–418. doi: 10.1111/j.1365-2850.2011.01797.x. [DOI] [PubMed] [Google Scholar]
- 28.Stevens A, Hernandez J, Johnsen K, et al. The use of virtual patients to teach medical students history taking and communication skills. Am J Surg. 2006;191(6):806–811. doi: 10.1016/j.amjsurg.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 29.Courteille O, Bergin R, Stockeld D, Ponzer S, Fors U. The use of a virtual patient case in an OSCE-based exam–a pilot study. Med. Teach. 2008;30(3):e66–e76. doi: 10.1080/01421590801910216. [DOI] [PubMed] [Google Scholar]
- 30.Cook D, Triola M. Virtual patients: a critical literature review and proposed next steps. Med Educ. 2009;43:303–311. doi: 10.1111/j.1365-2923.2008.03286.x. [DOI] [PubMed] [Google Scholar]
- 31.Benedict N. Virtual patient and problem-based learning in advanced therapeutics. Am J Pharm Educ. 2010;74(8):Article 143. doi: 10.5688/aj7408143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 33.Grusec J. Social Learning Theory and Developmental Psychology: The Legacies of Robert Sears and Albert Bandura. Dev Psychol. 1992;28(5):776–786. [Google Scholar]
- 34.Bloom BS. Taxonomy of Educational Objectives. Boston, MA: Allyn and Bacon; 1984. [Google Scholar]
- 35.Association of American Medical Colleges Institute for Improving Medical Education. Effective use of educational technology in medical education. Colloquium on educational technology: recommendations and guidelines for medical educators. March 2007. [Google Scholar]
- 36.Berman N, Fall L, Smith S, et al. Integration strategies for using virtual patients in clinical clerkships. Acad Med. 2009;84(7):942–949. doi: 10.1097/ACM.0b013e3181a8c668. [DOI] [PubMed] [Google Scholar]
- 37.Gesundheit N, Brutlag P, Youngblood P, Gunning WT, Zary N, Fors U. The use of virtual patients to assess the clinical skills and reasoning of medical students: initial insights on student acceptance. Med. Teach. 2009;31(8):739–742. doi: 10.1080/01421590903126489. [DOI] [PubMed] [Google Scholar]
- 38.Jabbur-Lopes MO, Mesquita AR, Silva LM, de Almeida Neto A, Lyra DP. Virtual patients in pharmacy education. Am J Pharm Educ. 2012;76(5):Article 92. doi: 10.5688/ajpe76592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brookfield S. Self-Directed Learning: From Theory to Practice New Directions for Continuing Education No. 25. San Francisco: Jossey-Bass; 1985. The continuing educator and self-directed learning in the community. [Google Scholar]
- 40.Hewitt-Taylor J. Teachers’ and students’ views on self-directed learning. Nurs Stand. 2002;17(1):33–38. doi: 10.7748/ns2002.09.17.1.33.c3267. [DOI] [PubMed] [Google Scholar]
- 41.Fry H, Jones A. Self-directed learning in the undergraduate dental curriculum. Br Dent J. 1995;179(10):373–376. doi: 10.1038/sj.bdj.4808930. [DOI] [PubMed] [Google Scholar]
- 42.Deyo A, Huynh D, Rochester C, Sturpe D, Kiser K. Readiness for self-directed learning and academic performance in an abilities laboratory course. Am J Pharm Educ. 2011;75(2):Article 25. doi: 10.5688/ajpe75225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Allison A. Preparing our graduates for a lifetime of learning. Am J Pharm Educ. 2006;70(1):Article 15. doi: 10.5688/aj700115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Greenberg A. Wainhouse research white paper: blended learning technology: navigating the challenges of large scale adoption. Wainhouse Research. 2012 [Google Scholar]


