Abstract
This study aims to evaluate incidence, patterns and epidemiology of mandibular condylar fractures (MCF) to propose a treatment strategy for managing MCF and analyze the factors which influence the outcome. One hundred and seventy-five MCF’s were evaluated over a four year period and their pattern was recorded in terms of displacement, level of fracture, age of incidence and dental occlusion. Of the 2,718 facial bone fractures, MCF incidence was the third most common at 18.39 %. Of 175 MCF 58.8 % were unilateral and 41.12 % were bilateral. 67 % of bilateral fractures and 43.8 % of unilateral fractures were associated with midline symphysis and contralateral parasymphysis fractures respectively. Most of the MCF was seen in the age group of above 16 years and 50 % of them were at subcondylar level (below the neck of the condyle). Majority of MCF sustained due to inter personal violence were undisplaced (72.7 %) and contrary to this majority of MCF sustained during road traffic accident were displaced. 62.9 % of total fractures required open reduction and rigid fixation and 37.1 % were managed with closed reduction. 80 % of MCF managed with closed reduction were in the age group of below 16 years. From this study it can be concluded that the treatment algorithm proposed for managing MCF is reliable and easy to adopt. We observed that absolute indication for open reduction of MCF is inability to achieve satisfactory occlusion by closed method and absolute contraindication for open reduction is condylar head fracture irrespective of the age of the patient.
Electronic supplementary material
The online version of this article (doi:10.1007/s12663-012-0428-9) contains supplementary material, which is available to authorized users.
Keywords: Mandibular condyle fractures, Temporomandibular joint, Dental occlusion, Age distribution of fractures, Treatment algorithm
Introduction
In the entire spectrum of maxillofacial trauma no other topic has created so much of debate and controversies than that of mandibular condyle fractures (MCF), both among children and adult population. Though a small non weight bearing joint, the significance of its nominal functioning has been best demonstrated in the statement by Ellis III and Gaylord [1] “Complications of trauma to the temporomandibular joint (TMJ) are far-reaching in their effects and not always immediately apparent. Disturbance of occlusal function, deviation of the mandible, internal derangements of the TMJ, and ankylosis of the joint with resultant inability to move the jaw are all sequel of this injury.”Thus, proper assessment and choosing appropriate treatment strategy is of paramount importance.
Injuries to the condylar cartilage as well as gross condylar head dislocation in children can reduce the capacity for complete remodeling and often result in mandibular deviation, but a (genetic) guidance system exists to rebuild the condylar process in children sustaining fractures [2]. In children between the ages of 3 and 11, the dislocated fractured condylar segment tends to be resorbed after successful therapy [3]. Teenagers show condylar remodeling, which is neither complete nor predictable and in adults fractures remodel only functionally [2]. According to Lindhal, complete remodeling can occur in children, which he called as “restitutional” remodeling and with advancing age this becomes less satisfactory though not completely lost, which he termed as “functional” restitution. The ability of condyle to remodel and regenerate is more impaired and unpredictable in adults and thus there is a greater need for open reduction in post pubertal patients [4].
An analysis of the frequency of fractures at different anatomic sites of the mandible revealed that the mandibular condyle sustains a fracture in 10–40 % of cases [5, 6]. Fridrich et al. [7] in their study of 1,967 patients found condylar fractures to be the second most common form of fracture after mandibular angle fractures.
The raging controversy of open (open reduction and internal fixation, ORIF) against closed or functional treatment of condylar fractures (Cranio maxillomandibular fixation, CMMF) are guided by three main factors: (1) the age of fracture incidence, (2) pattern of deviation of fracture and (3) level of fracture. Our paper not only adds to the existing literature on various patterns of MCF and its distribution in a 4 year period (175 fractures) at one of the suburban trauma units of south India but also presents the treatment protocol in choosing appropriate treatment based on the above three factors in comparison to the existing literature.
Patients and Methods
All the recorded data related to trauma between May 2006 and April 2010 (4 years duration) was retrieved and analyzed retrospectively from the medical records wing of our unit which is located in a southern state of India. Information was collected from the clinical and surgical notes of each of the patients in a standardised and systematic pattern to evaluate the epidemiological factors of general, facial and condylar trauma in a generalised population where road traffic accidents are highly rampant in the form of high speed motor vehicle collisions, as the hospital lies very close to one of the busiest express highways of the country connecting two major industrial cities, Hyderabad and Bangalore.
The data collected included incidence of MCF with respect to generalised/facial trauma, age, gender, diagnosis, location, pattern, level of condylar fractures, dislocation of the fracture, status of dentition and occlusion, treatment methods and duration between trauma and the treatment. The exclusion criteria were, if any of the above mentioned information was missing from the case notes of the patient.
The patients were divided into growing and non-growing groups based on their age at the time of presentation to understand the effect of choice of treatment and its outcome. The diagnosis was made in all the cases with the aid of orthopantomogram and multi detector CT scan (MDCT). The fractures were classified as condylar head, condylar neck (extracapsular), or subcondylar [8]. The degree of condylar displacement was categorized according to MacLennan [9] into four classes: (I) non-displaced, (II) deviation at the fracture line, (III) displacement (condylar fragment not in contact with the distal fragment but condyle still in the glenoid fossa), and (IV) dislocation (condyle dislocated from the glenoid fossa). Treatment of the condylar fractures was divided into non-surgical treatment (arch bars/elastics/physiotherapy) and surgical treatment (ORIF). Other associated fractures were classified based upon their location as symphysis, parasymphysis, body, angle, dentoalveolar, midface or isolated condylar fractures. The condyle fractures were grouped as unilateral or bilateral fractures. General trauma was classified according to the anatomic location of the injury (e.g., cranium, neck, thorax, abdomen, upper limb, lower limb).
Results
A total of 15,345 trauma patients received at the casualty wing of SVS Medical College & Hospital were evaluated between May 2006 and May 2010. 2718 (17.7 %) individuals suffered maxillofacial trauma in isolation or in combination with other body injuries. Of the 2,718 facial trauma, 674 (24.79 %) were fractures of mandible. Of all mandibular fractures the highest percentage of incidence of fractures (Graph 1—supplementary material) were of parasymphysis (32.78 %) followed by angle (20 %) and condyle (18.39 %).
Of the 124 patients with MCF, 73 (58.8 %) were unilateral and 51 (41.12 %) were bilateral totalling to 175 MCF (Table 1). Eighty (64 %) of these fractures resulted from RTA, 22 (17 %) from inter personal violence (IPV), 12 (9.6 %) from sports related injuries and 10 (8.06 %) from falls and various other miscellaneous reasons (Table 2). Among unilateral fractures 38 (52.05 %) were on the left side and 35 (47.9 %) were on the right side (Table 1). Male to female ratio was 1.5:1. We divided the age of the patients based on their growth and puberty into two groups. Majority of MCF were found in subjects above 16 years of age (74.19 %) which was taken as the delineating age between paediatric and adult population in designing our treatment algorithm.
Table 1.
Distribution of condyle fractures
| Total no of patients with condylar fracture | 124 | |
| Total no of condylar fractures | 175 | |
| Unilateral condyle fractures | 73 | |
| Right—35 | Left—38 | |
| Bilateral condyle fractures | 51 | |
Table 2.
Etiology of trauma
| Etiology | n | % |
|---|---|---|
| Road traffic accidents | 80 | 64 |
| Inter-personal violence | 22 | 17 |
| Sports | 12 | 9.6 |
| Falls | 10 | 8.6 |
| Total | 124 | 100 |
Eight-eight fractures (50 %) were subcondylar in nature, 32 fractures (18.54 %) were condylar head fractures and 55 (31.45 %) were condylar neck fractures (Table 3). Of 175 fractures, 41 (23.4 %) belonged to class I, 28 (16 %) to class II, 67 (38.2 %) to class III and 39 (22.2 %) to class IV (Table 4). Of the 22 patients who sustained injury from IPV 16 (72.7 %) showed very minimal displacement, 4 (18 %) presented with lateral displacement and 2 (9 %) with medial dislocation. 67 % of bilateral fractures were associated with midline symphysis fractures and majority of unilateral fractures, 43.8 %, were associated with parasymphysis fractures (Table 5; Graph 2—supplementary material). This data corroborates the fact that when the impact is on the midline of the mandible the force is transmitted equally to the bilateral condyles, fracturing both of them, whereas when the patient turns his or her head to one side as a protective mechanism at the time of impact it results in the energy being transferred to opposite condyle resulting in unilateral fractures.
Table 3.
Distribution of condyle fractures based on their location
| n | |
|---|---|
| Subcondyle | 88 |
| Head | 32 |
| Neck | 55 |
Table 4.
Distribution of condyle fractures based on their displacement
| MCF classification | n | % |
|---|---|---|
| Class 1 | 41 | 23.4 |
| Class 2 | 28 | 16 |
| Class 3 | 67 | 38 |
| Class 4 | 39 | 22.2 |
| Total | 175 | 100 |
Table 5.
Other concomitant facial bone fractures along with condyle fractures
| Fractures | Unilateral | Bilateral | Total |
|---|---|---|---|
| Symphysis | 13 | 32 | 45 |
| Parasymphysis | 32 | 1 | 33 |
| Body | 1 | 2 | 3 |
| Angle | 3 | 0 | 3 |
| Mid-face | 1 | 3 | 4 |
| Dental | 0 | 0 | 0 |
| Isolated | 23 | 13 | 36 |
| Total | 73 | 51 | 175 |
Of the 175 cases, 110 (62.9 %) were managed with (ORIF) and 65 (37.1 %) with functional therapy and elastic traction. It must be emphasised that 80 % of MCF managed with functional therapy were below 16 years of age. The most commonly used approach for ORIF was retromandibular approach (transparotid). In our experience as most of the MCF were sub condylar, it was found that retro mandibular approach gave the best access and visibility compared to pre auricular approach. On the other hand, pre auricular approach was found to be extremely useful in grossly anteromedially dislocated MCF as it improved the accessibility and visibility to locate the dislocated condylar fragment. However out of 65 cases of retromandibular approach, facial nerve was encountered in 7 cases (10.7 %) and transient facial palsy was noticed in 16 (24 %). Average duration of recovery of transient facial palsy was 3 months with the shortest being 12 days postoperative and the longest 5 months. Pre auricular approach was found to be extremely useful in grossly anteromedially dislocated MCF as it improved the accessibility and visibility to locate the dislocated condylar fragment. Facial nerve was never encountered during dissection, yet transient facial palsy was noticed among 3 patients (6.6 %). Average duration of facial palsy was 2 weeks post operative. There were few (15) cases where sub mandibular approach was used in fractures which were low-lying.
There was evidence of screw loosening and pus discharge in 5(4.5 %) patients of ORIF group. Four belonged to pre auricular approach and 1 to retro mandibular approach. There was no incidence of plate fracture or extrusion in any of the cases. These patients were subsequently managed with plate removal under antibiotic coverage and CMMF for further 3 weeks
There were no statistically significant differences in the outcome of results between the CMMF group and the ORIF group with two cases in ORIF group and 3 cases in CMMF group resulting in deranged occlusion (Table 6). We presume that this low incidence of complications was a result of the methodology we adopted in the choice of treatment which was evidence based and this was arrived at after thorough review of literature (Fig. 1).
Table 6.
Complications and consequences of the treatment modalities chosen
| Complication | ORIF | CMMF |
|---|---|---|
| Sialoceole | 2 | |
| Ear discharge | 1 | |
| Transient facial palsy | 19 | |
| Occlusion | 2 | 3 |
| Stitch abscess | 1 | |
| Trismus | 2 | 4 |
| Periodontitis | 4 | 10 |
Fig. 1.
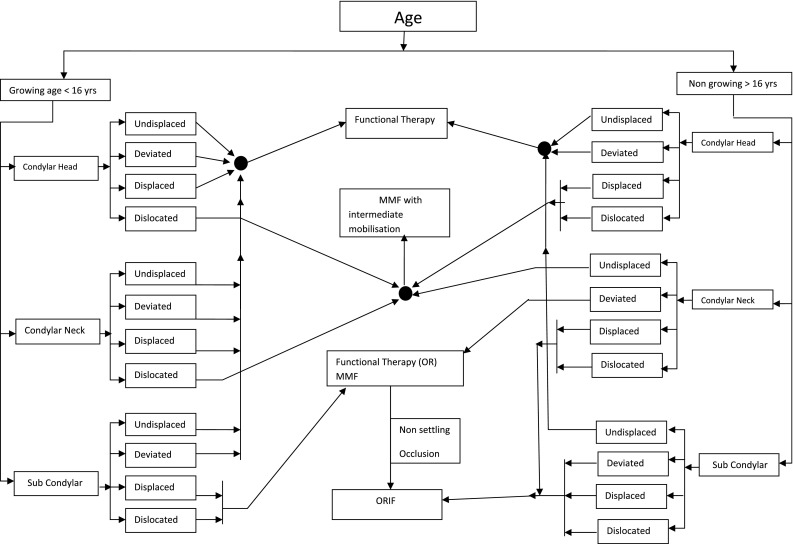
Treatment algorithm
Discussion
Epidemiologic surveys will vary with geographic region, population density, socioeconomic status, regional government policies, era in time, and type of facility in which the study was conducted. Comparison of surveys requires consideration of these factors [10]. This retrospective study which analyzed 15,345 trauma patients over a period of 6 years reiterates the fact that maxillofacial injuries are highly frequent, with 17 % incidence and thus stresses on importance of having a maxillofacial surgeon as part of the trauma team. This is in agreement with 15 % incidence of facial fractures in a sample of 1,088 in a study conducted at Liverpool, UK [11].
Twenty-four per cent incidence of mandibular fractures among 2,718 facial fractures establishes the fact that mandible is one of the most frequently injured bones as stated by other authors in their reports [12, 13]. In our study MCF (18 %) is next only to angle fracture in frequency. In a study conducted by Marker et al. [14] condyle comprised of 41 % of all mandibular fractures. In contrast Ellis et al. [12] found only 29 % incidence of condyle fracture in a sample of 2,137 mandibular fractures. Marker et al. attributed this to the larger number of young and unemployed people with more propensities for interpersonal violence and increased edentulism in their study population. In our experience, the pattern of displacement and dislocation of condylar fracture is also dictated by the status of dentition and position of the mandible at the time of impact. It was noted that significantly displaced condylar fractures were noted in road traffic accidents and no or minimal displaced fractures resulting from IPV. This is similar to observations made by Silvennoinen et al. [8] where they noticed 26 % of condylar dislocation due to RTA and only 8 % from IPV.
We hypothesize that the status of lateral pterygoid (LP) muscle contraction at the time of impact and kinematics of condylar movement plays an important role in the dislocation of MCF. LP muscle is one of the chief depressors of the mandible and causes translation of the condylar head anteriorly in the glenoid fossa. At the time of impact to the mandible when the subject is in the process of opening the mouth as in yelling out or shouting, the LP is in the process of continued contraction. If a fracture condyle occurs at this situation below the level of muscle insertion, the muscle fibers snap like in stretched elastic fibers and thus result in severely dislocated proximal fragment. This situation is akin to what happens in high speed collisions where the subject tends to open the mouth wide in shock. In IPV, subjects generally tend to keep their mandible tightly closed with teeth in firm occlusion like clenching. This act will keep the condyle firmly seated at the centre of glenoid fossa and thus results in laterally deviated fracture or a compression type of fracture with minimal displacement. In the kinematics of mandibular movements, rotation of condyle head is followed by translation. If the impact on mandible occurs when the mouth is partially open, which is when the head is still in rotation, the degree of displacement is much less than when the mouth is wide open, (>15 mm) as the condyle shifts to translatory motion. This is because of continuity of movements of condyle in its anterior direction even after the fracture due to inertia which is coupled with LP pull.
Another significant finding was association of bilateral condyle fractures with symphysis fractures and unilateral fractures with opposite parasymphysis fractures. Lindahl and Hollender (1977) [2] have also found that concomitant fractures of the mandibular body are more frequent in bilateral than in unilateral condylar fractures. Zachariades [15] recorded 52 %, 19 % and 11 % of symphysis, parasymphysis, body and angle fractures respectively as other associated fractures. They concluded that condylar fractures result from an indirect force applied to the mandible, associated with at least one other mandibular fracture, mostly symphyseal or parasymphyseal. This suggests that condylar fractures may be the result of the transmission of force which is not fully absorbed in the majority of cases in the area of its primary application, i.e. the mental region [15].
There is no other single concept in the entire spectrum of maxillofacial trauma which has created so much furore as that of MCF treatment [16–19]. Lindahl and Hollender [2] had stressed on the importance of age and growth on the treatment outcome of MCF. In our view age plays a very significant role in the choice of treatment and this forms the baseline for our treatment algorithm. Assael [20] in his review paper of 2,033 patients, proposed 26 variables influencing MCF treatment selection and outcome, starting from age to institutional resources and willing prayers. This data though elaborately covers all the aspects of MCF treatment is too laborious and impractical to apply in every situation. Zide and Kent’s [3] landmark publication of 1983 on absolute and relative indications has undergone considerable modifications with time by various authors and also same authors [21, 22]. Haug and Assael [18] in 2001 made an attempt at refining the absolute and relative indications and contraindications.
Our treatment protocol agrees with some of the aspects of their proposals like absolute contraindication for ORIF would be condyle head fractures irrespective of the age and absolute indication would be inability to achieve desirable occlusion for condylar neck and subcondylar level fractures with CMMF. We believe that the indication/contraindication method of proposals are highly subjective and does not draw any definitive conclusion on treatment choice. The protocol we suggest here is highly objective and self derivative when we come across a MCF, more or less it works like a mathematical formula and it is based on the radiographic findings except for status of occlusion and age of the patient. In case of bicondyle fractures the algorithm was applied to both the condyles separately and if at least one condyle comes into open reduction category, it needs to be treated accordingly.
Retromandibular approach [23, 24] gives an advantage of shorter working distance from the skin, greater access to the posterior border of the mandible, sigmoid notch and thus subcondylar fractures [25]. Fifty per cent of MCF in our study were subcondylar and we used retromandibular approach in 61.2 % of these cases. The greatest advantage with this approach apart from the above mentioned was greater accessibility to the fracture site and convenience in fixing a mini plate in low lying condylar fractures. The greatest disadvantage with this approach is difficulty in locating the medially dislocated condylar head in which case pre auricular approach would be the better option. Also 2 patients presented with post-operative sialoceol which was managed conservatively with pressure dressing. Preauricular approach was used in 21(26.9 %) cases and the major disadvantage was in accessing the distal mandibular portion while fixing the plate. This could be achieved by slightly lengthening the incision or retraction but both at the risk of facial nerve. Apart from these indications and contraindications for each approach we did not find any other significant morbidity related to facial nerve in any of the approaches when the surgical dissection planes were well maintained and respected.
With its rapidly growing economy, India is an epitome of changing disease patterns of developing nation to developed nation and thus serves as the best feeding ground for researchers to analyze and test various disease patterns and treatment concepts. Our treatment protocol for condylar fractures resulted in a logical choice of treatment in varying patterns of fracture with fewer complications and satisfactory outcome. Yet it needs to be analyzed further as this is partly a retrospective study, and the nature of a retrospective study inherently results in flaws. These problems were manifested by the gaps in information and incomplete records. Furthermore, all data rely on the accuracy of the original examination and documentation. Items may have been excluded in initial examination or not recorded in the medical chart.
Electronic supplementary material
References
- 1.Ellis III E, Gaylord S. Throckmorton: treatment of mandibular condylar process fractures: biological considerations. J Oral Maxillofac Surg. 2005;63:115–134. doi: 10.1016/j.joms.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 2.Lindahl L, Hollender L. Condylar fractures of the mandible II. Radiographic study of remodeling processes in the temporomandibular joint. Int J Oral Surg. 1977;6:157–165. doi: 10.1016/s0300-9785(77)80048-3. [DOI] [PubMed] [Google Scholar]
- 3.Zide MF, Kent JN. Indications for open reduction of mandibular condyle fractures. J Oral Maxillofac Surg. 1983;41:89–98. doi: 10.1016/0278-2391(83)90214-8. [DOI] [PubMed] [Google Scholar]
- 4.Takenoshita Y, Oka M, Tashiro H. Surgical treatment of the mandibular condylar neck. J Cranio-Maxillofac Surg. 1989;17:119–124. doi: 10.1016/S1010-5182(89)80083-6. [DOI] [PubMed] [Google Scholar]
- 5.Brasileiro BF, Passeri LA. Epidemiological analysis of maxillofacial fractures in Brazil: a five-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:28. doi: 10.1016/j.tripleo.2005.07.023. [DOI] [PubMed] [Google Scholar]
- 6.Bataineh A. Etiology and incidence of maxillofacial fractures in the north of Jordan. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:31. doi: 10.1016/S1079-2104(98)90146-9. [DOI] [PubMed] [Google Scholar]
- 7.Fridrich KL, Pena-Velasca G, Olson RAJ. Changing trends with mandibular fractures: a review of 1067 cases. J Oral Maxillofac Surg. 1992;50:586–589. doi: 10.1016/0278-2391(92)90438-6. [DOI] [PubMed] [Google Scholar]
- 8.Silvennoinen U, Iizuka T, Lindqvist C, Oikarinen K. Different patterns of condylar fractures: an analysis of 382 patients in a 3 year period. J Oral Maxillofac Surg. 1992;50:1032–1037. doi: 10.1016/0278-2391(92)90484-H. [DOI] [PubMed] [Google Scholar]
- 9.MacLennan WD. Consideration of 180 cases of typical fractures of the mandibular condylar process. Br J Plast Surg. 1952;5:122. doi: 10.1016/S0007-1226(49)80020-8. [DOI] [PubMed] [Google Scholar]
- 10.Haug RH, Prather J, Indresano AT. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990;48:926–932. doi: 10.1016/0278-2391(90)90004-L. [DOI] [PubMed] [Google Scholar]
- 11.Down KE, Boot DA, Gorman DF. Maxillofacial and associated injuries in severely traumatized patients: implications of a regional survey. Int J Oral Maxillofac Surg. 1995;24:409–412. doi: 10.1016/S0901-5027(05)80469-2. [DOI] [PubMed] [Google Scholar]
- 12.Ellis E, 3rd, Moos KF, El-Attar A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol. 1985;59:120–129. doi: 10.1016/0030-4220(85)90002-7. [DOI] [PubMed] [Google Scholar]
- 13.Fasola AO, Nyako EA, Obiechina AE, Arotiba JT. Trends in the characteristics of maxillofacial fractures in Nigeria. J Oral Maxillofac Surg. 2003;61:1140–1143. doi: 10.1016/S0278-2391(03)00671-2. [DOI] [PubMed] [Google Scholar]
- 14.Marker P, Nielsen A, Lehmann Bastian H. Fractures of the mandibular condyle. Part 1: patterns of distribution of types and causes of fractures in 348 patients. Br J Oral Maxillofac Surg. 2000;38:417–421. doi: 10.1054/bjom.2000.0317. [DOI] [PubMed] [Google Scholar]
- 15.Zachariades N, Mezitis M, Mourouzis C, Papadakis D, Spanou A. Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections on treatment and proposals. J CranioMaxillofac Surg. 2006;34:421–432. doi: 10.1016/j.jcms.2006.07.854. [DOI] [PubMed] [Google Scholar]
- 16.Konstantinovic V, Dimitrijevic B. Surgical versus conservative treatment of unilateral condylar process fractures: clinical and radiological evaluation of 80 patients. J Oral Maxillofacial Surg. 1992;50:349. doi: 10.1016/0278-2391(92)90395-G. [DOI] [PubMed] [Google Scholar]
- 17.Raveh J, Vuillemin T, Ladrach K. Open reduction of the dislocated, fractured condylar process: indications and surgical procedures. J Oral Maxillofacial Surg. 1989;47:120. doi: 10.1016/S0278-2391(89)80100-4. [DOI] [PubMed] [Google Scholar]
- 18.Haug RH, Assael LA. Outcome of open versus closed treatment of mandibular subcondylar fractures. J Oral Maxillofacial Surg. 2001;59:370. doi: 10.1053/joms.2001.21868. [DOI] [PubMed] [Google Scholar]
- 19.Hidding J, Wolf R, Pingel D. Surgical versus non-surgical treatment of fractures of the articular process of the mandible. J Craniomaxillofac Surg. 1999;20:345. doi: 10.1016/S1010-5182(05)80363-4. [DOI] [PubMed] [Google Scholar]
- 20.Assael LA. Open versus closed reduction of adult mandibular condyle fractures: an alternative interpretation of the evidence. J Oral Maxillofacial Surg. 2003;61:1333–1339. doi: 10.1016/S0278-2391(03)00736-5. [DOI] [PubMed] [Google Scholar]
- 21.Zide MF. Open reduction of mandibular condyle fractures. Clin Plast Surg. 1989;16:69. [PubMed] [Google Scholar]
- 22.Kent JN, Neary JP, Silvia C. Open reduction of mandibular condyle fractures. Oral Maxillofac Clin North Am. 1990;2:69. [Google Scholar]
- 23.Koberg WG, Momma W. Treatment of fractures of the mandibular process by functional stable osteosynthesis using miniaturized dynamic compression plates. Int J Oral Surg. 1978;7:256–262. doi: 10.1016/S0300-9785(78)80091-X. [DOI] [PubMed] [Google Scholar]
- 24.Manisali M, Amin M, Aghabeigi B, Newman L. Retromandibular approach to the mandibular condyle and cadaveric study. Int J Oral Maxillofacial Surg. 2003;32:253–256. doi: 10.1054/ijom.2002.0270. [DOI] [PubMed] [Google Scholar]
- 25.Narayanan V, Kannan R, Sreekumar K. Retromandibular approach for reduction and fixation of mandibular condyle fractures: a clinical experience. Int J Oral Maxillofacial Surg. 2009;38:835–839. doi: 10.1016/j.ijom.2009.04.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


