Abstract
The repair of unilateral cleft lip nose deformity remains a challenging endeavor for reconstructive surgeons for many reasons, one of which is the timing of rhinoplasty, whether to be synchronous or staged with cleft lip repair and the technique for rhinoplasty. Many authors now favor primary rhinoplasty with the cleft lip repair. Various surgical techniques have been used, most commonly the closed and open rhinoplasty techniques. In this randomized controlled prospective study, we compare the closed rhinoplasty technique with open rhinoplasty during primary unilateral cleft lip repair. Thirty-six patients with unilateral complete cleft lip and nose deformity were selected. Out of this 19 patients were assigned randomly and operated with open rhinoplasty and 17 patients with closed rhinoplasty. The cleft lip repair was done using modified, Millard’s rotation-advancement technique in both the groups. Follow-up assessment was done after 6 months. Quantitative and qualitative analysis were done. Statistical analysis of the data was done using SPSS 11.0. Post-operatively, the alar base width difference between the open and closed rhinoplasty techniques was statistically significant. There was no statistically significant difference in other parameters compared.
Keywords: Unilateral complete cleft lip, Nose deformity, Open/closed rhinoplasty
Introduction
Correction of cleft lip nasal deformity is a major challenge in cleft surgery. For many years, the nose was left untouched at the time of primary lip repair. This was because of concern about interfering with nasal growth, damage to nasal cartilage and the introduction of the scar that could make secondary correction more difficult [1, 2]. However, evidence demonstrates no interference in growth or subsequent surgeries [3, 4].
Often a repaired cleft is revealed more by associated nasal deformity than by the lip repair line. The multiplicity of methods described for realignment of the deformed cartilages testifies to the difficulty of first achieving and then sustaining correction of the nasal deformity. The alar cartilages provide the key to the cleft lip nasal problems. Failing to address the alar cartilage at the time of lip repair leaves it locked and tethered in its displaced position by scar and transverse shortage of nostril lining. Moreover, the growth of nasal tip is altered and secondary correction is difficult to achieve.
Correction of nasal deformity can be with or without direct exposure of the alar cartilages. The open and closed rhinoplasty approaches remain a subject for debate. Advances in surgical techniques and improved understanding of rhinoplasty dynamics ensure that this topic remains contemporary. However, literature is lacking in randomized controlled trials comparing these two approaches at the time of primary cleft lip repair. Hence, in this study, the outcomes of primary rhinoplasty by open and closed methods at the time of cleft lip repair have been compared after 6 months of surgery. The two techniques are compared based on evaluation of nasal asymmetry.
Patients and Methods
A randomized controlled prospective study was done between 1st January 2007 to 31st January 2008 at Bhagwan Mahaveer Jain Hospital, Smile Train Unit. Thirty-six patients between the age of 2–45 years undergoing cheilorhinoplasty for unilateral complete cleft lip and nose deformity were included. The patients were assigned into two groups randomly. Sealed envelops numbered from 1–50 were used for randomization. One envelop was picked randomly when patient was planned for cleftlip–nose surgery. Even numbers were assigned to open rhinoplasty with primary cleft lip repair group and odd numbers to the closed rhinoplasty group with primary cleft lip repair. The technique of lip repair was the same for both the groups, i.e., modified Millard’s approach and was performed by two surgeons. However the cleft nose deformity was addressed with an open approach in 19 cases and a closed approach in 17 cases.
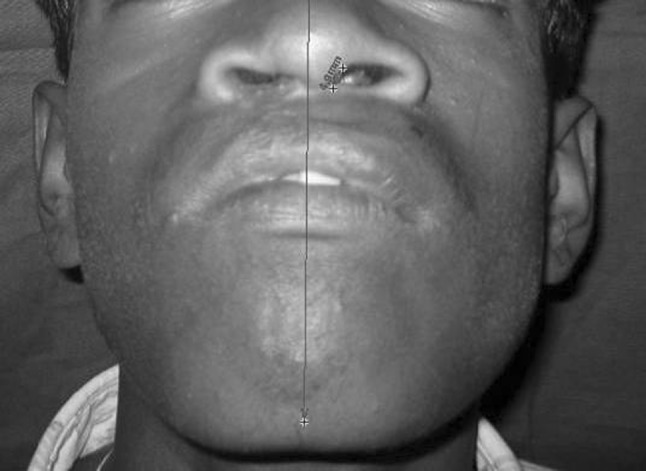
All cases were evaluated for the nasal deformity correction clinically and photographically using Windows Vista Software post-operatively. Comparison of the cleft side was done with the non cleft side in each case. Postoperatively, four points were marked on the patient’s face–the right and left outer canthus of the eye, the glabella and the menton. Measurements were made from glabella to menton and left outer canthus to right outer canthus using a thread and then measuring across a ruler. Photographs were taken pre and post-operatively (case 1 and case 2). The points act as control during our post operative software analysis. By entering these values, the software enables to orient the actual size of the image. Patients were reviewed after a period of 6 months post-operatively.
Case 1: Open rhinoplasty
Case 2: Closed rhinoplasty

Post-operatively the landmarks were measured from the
Mid-point of columella base to the midpoint of the ala base of both non-cleft and cleft side (alar base width) (Fig. 1).
Height of nostril on cleft and non-cleft side (Fig. 2).
Columella length on the cleft and non-cleft side (Fig. 3).
Columella deviation—whether present or absent.
Orientation of nostril—whether horizontal, vertical or intermediate on the cleft and non-cleft side
Fig. 1.

Mid-point of columella base to the midpoint of the ala base of both non-cleft and cleft side (alar base width)
Fig. 2.

Height of nostril on cleft and non-cleft side
Fig. 3.
Columella length on the cleft and non-cleft side
The design of this study was proposed for a sample of 50, with 25 in each arm. However, in the time allotted for the study only 36 could be recruited. Out of them, only 16 were available for complete follow-up assessment, eight each from closed rhinoplasty and eight patients of open rhinoplasty. Due to reasons like poor socio economic status and lack of interest, many of them did not return for follow-up in spite of repeated letters and phone calls.
The data obtained through the available sample size for the study were analyzed with student t test using statistical software SPSS 11.0.
Surgical Technique
The markings for lip (Fig. 4), closed (Fig. 5) and open (Fig. 6) rhinoplasty are shown. The lip was operated with modified Millard’s rotation-advancement technique.
Fig. 4.
Markings for modified Millard’s rotation-advancement technique
Fig. 5.

Marking for closed rhinoplasty
Fig. 6.

Marking for open rhinoplasty
In closed rhinoplasty, sharp pointed scissors are passed up through the columella and the gingivolabial incision on the side of cleft (Fig. 7). Dissection is carried out in a closed fashion to free the skin from the medial crus and dome of the alar cartilage extending till the attachment of lower lateral cartilage to maxilla. Dissection extends from nostril rim below, over nasal tip and up to the medial crus to lateral cartilage.
Fig. 7.

Dissection for closed rhinoplasty passed through the columella and the gingivolabial incision on the side of cleft
The technique by Thomas [5, 6] was followed for open rhinoplasty. Marginal incisions were given following the markings done (Figs. 6, 8) and connected by the transcolumellar incision. Nasal skin overlying the columella and alar were dissected upwards to expose the medial crus of the alar cartilage on the cleft and non-cleft side. Dissection is done below the superficial musculo aponeurotic layer, exposing the lower lateral cartilage. This is continued laterally till the fibrous attachment of the lower lateral cartilage to the anterior wall of maxilla. Dissection is extended till the lateral angle of dome on the cleft side. Care is taken to free the fibrofatty tissue between the domes of the alar cartilage and leave it attached to the overlying skin. The nasal skin is dissected widely to allow redraping over the reconstituted nasal tip. The medial alar cartilages are visualized, lifted upward, aligned symmetrically and sutured in place with three to four 5-0 proline sutures (Fig. 9). Mucosal and skin closures were done with 4-0 vicryl and 5-0 rapide vicryl respectively.
Fig. 8.

Dissection for open rhinoplasty exposing the medial crus of the alar cartilage on the cleft and non cleft side and extending till the lateral angle of dome on the cleft side
Fig. 9.

Medial alar cartilages were visualized, lifted upward, aligned symmetrically and sutured in place with three to four 5-0 proline sutures
Results
Of the eight patients followed-up in open rhinoplasty group, the mean value of alar base width on the cleft side and non-cleft side post-operatively was 17.76 and 15.06 mm respectively. Of the eight patients followed-up in closed rhinoplasty group, the mean value of alar base width on the cleft side and non-cleft side post-operatively was 19.85 and 14.29 mm respectively. Alar base width difference between the cleft and non-cleft side postoperatively in open and closed rhinoplasty is 2.7 and 5.56 mm respectively. P value is 0.046 which is statistically significant. The width of alar base was consistently more on the cleft side than on the non-cleft side in both the groups. However, the alar base width difference between the cleft and non-cleft side is less in open rhinoplasty technique than in the closed rhinoplasty technique (Table 1).
Table 1.
Comparison of alar base width in closed rhinoplasty and open rhinoplasty
| Midpoint of columella to alar base | Open (mm) | Closed (mm) |
|---|---|---|
| Results are presented in mean ± SD | ||
| Post op non-cleft side | 15.06 ± 2.02 | 14.29 ± 2.07 |
| Post op cleft side | 17.76 ± 2.65 | 19.85 ± 3.2 |
| Alar base width difference (non-cleft vs cleft) | 2.7 ± 2.72 | 5.56 ± 2.47 |
| P value | 0.046 (significant) | |
Of the eight patients followed-up in the open rhinoplasty group, the mean value of nostril height on the cleft side and non-cleft side postoperatively was 4.3 and 6.4 mm respectively. Of the eight patients followed-up in the closed rhinoplasty group, the mean value of nostril height on the cleft side and non-cleft side post-operatively was 5.01 and 7.48 mm respectively. Nostril height difference between the cleft and non-cleft side postoperatively in open and closed rhinoplasty is −2.1 and −2.48 mm respectively. P value is 0.593 which is statistically not significant. The nostril height on the cleft side was consistently less than on the non-cleft side in both the groups (Table 2).
Table 2.
Comparison of nostril height between closed rhinoplasty and open rhinoplasty
| Nostril height | Open (mm) | Closed (mm) |
|---|---|---|
| Results are presented in Mean ± SD | ||
| Post op non-cleft side | 6.4 ± 1.53 | 7.48 ± 1.34 |
| Post op cleft side | 4.3 ± 1.03 | 5.01 ± 1.14 |
| Nostril height difference (non-cleft vs cleft) | −2.1 ± 1.53 | −2.48 ± 1.29 |
| P value | 0.593 (not significant) | |
Of the eight patients followed-up in the open rhinoplasty group, the mean value of columella length on the cleft side and non-cleft side postoperatively was 3.23 and 4.71 mm respectively. Of the eight patients followed-up in the closed rhinoplasty group, the mean value of columella length on the cleft side and non-cleft side post-operatively was 4.07 and 6.11 mm respectively. Columella length difference between the cleft and non-cleft side postoperatively in open and closed rhinoplasty is −1.47 and −2.07 mm respectively. P value is 0.271 which is statistically not significant. The columella length on the cleft side was consistently less than on the non-cleft side in both the groups (Table 3).
Table 3.
Comparison of columella length between closed rhinoplasty and open rhinoplasty
| Columella length | Open (mm) | Closed (mm) |
|---|---|---|
| (Results are presented in Mean ± SD) | ||
| Post op non-cleft side | 4.71 ± 1.1 | 6.11 ± 1.47 |
| Post op cleft side | 3.23 ± 0.9 | 4.07 ± 1.23 |
| Columella length difference (non-cleft vs cleft) | −1.47 ± 0.9 | −2.07 ± 1.16 |
| P value | 0.271 (not significant) | |
The nostrils on cleft and non-cleft side were observed for symmetrical orientation (whether horizontal, intermediate, or vertical). In open rhinoplasty 50 % of cases had similar kind of orientation on the cleft and non-cleft side postoperatively, and in 50 % of cases the orientation was not similar on the cleft and non-cleft side post-operatively. In closed rhinoplasty 62.5 % of cases had similar kind of orientation on the cleft and non-cleft side postoperatively, and in 37.5 % of cases the orientation was not similar on the cleft and non-cleft side post-operatively (Table 4).
Table 4.
Comparison of nostril orientation between closed rhinoplasty and open rhinoplasty
| Post op | Symmetrical | Asymmetrical |
|---|---|---|
| Open rhinoplasty | 4 (50 %) | 4 (50 %) |
| Closed rhinoplasty | 5 (62.5 %) | 3 (37.5 %) |
In all unilateral cleft lip patients, the columella is usually deviated away from the cleft side. Postoperatively, evaluation was done for all 16 patients. Of the eight patients operated with open rhinoplasty, mild columella deviation was persistent in three cases while five cases had the columella centrally repositioned. Of the eight patients operated with closed rhinoplasty, columella deviation was persistent in five cases while three cases had the columella centrally repositioned (Table 5).
Table 5.
Comparison of columella deviation between closed rhinoplasty and open rhinoplasty
| Post op | Present | Absent |
|---|---|---|
| Open rhinoplasty | 3 (37.5 %) | 5 (62.5 %) |
| Closed rhinoplasty | 5 (62.5 %) | 3 (37.5 %) |
Of the 16 patients, only one patient had wound dehiscence on lip at one week follow-up. The patient was advised to keep the area clean and continue the antibiotic ointment (Neosporin) for another week. After 15 days, wound healing was uneventful. No other complications were encountered.
Discussion
The nasal deformity in unilateral cleft lip is a social stigma and burden to the patient and a challenge to the surgeon. In recent years there has been an interest in addressing this problem primarily at the time of lip repair, using a closed or an open approach rhinoplasty at the time of cleft lip repair. However, literature is lacking in randomized controlled trials comparing these two approaches, to address the problem of cleft nose deformity at the time of cleft lip repair.
In most studies the results have been based on qualitative analysis. Qualitative analysis will vary according to the perception of the observer. However, this has to be taken seriously because ultimately the results have to satisfy everyone and not only the surgeons. Moreover, there is no literature comparing closed and open rhinoplasty technique during primary cleft lip repair. Few authors are in favour of closed rhinoplasty [1, 7] and most others are of the opinion that open rhinoplasty [2–5, 8] gives superior results. However, no comparative study of the two techniques and no quantitative analysis has yet been reported.
McComb [1] and Salyer [7] have reported on their long term experiences using various approaches for mobilizing and reorienting the nasal alar cartilages.
They claimed improved symmetry and a decreased rate of secondary nasal revision surgery using a closed approach that did not require direct exposure of the nasal cartilage at the time of repair.
Trott and Mohan [4] also reported consistently better results with open-tip rhinoplasty than those obtained by primary closed rhinoplasty as described by McComb.
Thomas and Mishra [5] stated that closed rhinoplasty technique does not allow the intercrural soft tissue dissection; hence a better projection of the nasal tip is possible in the open tip rhinoplasty.
Kim et al. [8] studied 412 cases of cleft lip, of which 195 were corrected by the conventional method (only lip repair was done) and 217 cases were corrected by simultaneous open rhinoplasty. The latter showed more symmetry of nostril and nasal dome projection and better correction of buckling and alar flaring were achieved.
La Rossa & Donath [2] have summarized four principles in the primary correction of the cleft nasal deformity. The second principle is to reshape the cartilage which can be done using intranasal splints inserted immediately following primary cleft lip and nasal repair as demonstrated by Matsuo. However, in our study we did not use the nasal conformers. Whether better nostril symmetry could have been achieved by using nasal conformers postoperatively to retain the columella length and nostril height achieved in the immediate postop, in open rhinoplasty cases is yet to be studied by us.
Chang et al. [9] have compared four techniques for obtaining nasal symmetry in unilateral cleft lip cases. They have concluded that nasoalveolar molding plus primary rhinoplasty plus overcorrection gives the best results. In this study, nasoalveolar molding was not performed as the age group did not favour the treatment. Few nasal tip complications have been reported in literature following primary nasoplasty [10]. We had one case of lip dehisence which healed uneventfully with conservative management.
This study has a wide age variation which may arise the question of comparison between the groups as the growth of nasal cartilage varies in children and adults. The nasal cartilage dorsal length increased after birth until twenties (27.6 ± 4.6) and does not show significant changes later in adults [11]. But, since the objective of this study was to compare the results of two different surgical techniques and as there were almost an equal distribution of age population in both the groups, we made the conclusion taking into account only the surgical techniques and not the age factor.
In our study we have made a quantitative analysis of the results achieved by comparing open versus closed rhinoplasty during primary cheiloplasty. Both techniques seemed to give similar results.
Conclusion
It is an argument often heard that results obtained by open rhinoplasty appear to be superior to those by closed rhinoplasty techniques, at the time of primary cleft lip repair [6]. It was this hypothesis we set out to test so that the practice could be adopted eventually to infant repairs as well, if it turned out to be true. Notwithstanding the fact that the sample size is small and the age group discrepancy, this is an important finding that there seemed to be no difference between the two groups.
Larger sample sizes as well as different parameters to assess the quality of nose repair might come up with totally different conclusions. However, we have to make do with the result of this prospective randomized trial till such time we have contrary results.
Acknowledgments
The Smile Train Unit, Bhagwan Mahaveer Jain Hospital, Bangalore and Dr. Swaminath, MBBS, DNB (Ortho).
References
- 1.McComb H (1985) Primary correction of unilateral cleft lip nasal deformity: a 10 year review. Plast Reconstr Surg 75:791–797 [DOI] [PubMed]
- 2.LaRossa Don, Donath Gary. Primary nasoplasty in unilateral and bilateral cleft nasal deformity. Clin Plast Surg. 1993;20(4):781–791. [PubMed] [Google Scholar]
- 3.Bhoo-Chai K. Primary repair of the unilateral cleft lip nose in the oriental: a 20 year follow up. Plast Reconstr Surg. 1987;80:185–194. doi: 10.1097/00006534-198708000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Trott JA, Mohan N. A preliminary report on open tip rhinoplasty at the time of lip repair in unilateral cleft lip and palate: the alor setar experience. Br J Plast Surg. 1993;46:363–370. doi: 10.1016/0007-1226(93)90040-I. [DOI] [PubMed] [Google Scholar]
- 5.Thomas C, Mishra P. Open tip rhinoplasty along with the repair of cleft lip and palate cases. Br J Plast Surg. 2000;53(1):1–6. doi: 10.1054/bjps.1999.3248. [DOI] [PubMed] [Google Scholar]
- 6.Thomas C. Primary rhinoplasty by open approach with repair of unilateral complete cleft lip. J Craniofac Surg. 2009;20(Supplement):2. doi: 10.1097/SCS.0b013e3181b3eee4. [DOI] [PubMed] [Google Scholar]
- 7.Salyer Kenneth E. Primary correction of the unilateral cleft lip nose: a 15 year experience. Plast Reconstr Surg. 1986;77:558–566. doi: 10.1097/00006534-198604000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Kim S-K, Cha B-H, Lee K-C, Park J-M (2004) Primary correction of unilateral cleft lip nasal deformity in asian patients: anthropometric evaluation. Plast Reconstr Surg 114:1373–1381 [DOI] [PubMed]
- 9.Chang C-S, Por YC, Liou EJ-W, Chang C-J, Chen PK-T, Noordhoff MS. Long-term comparison of four techniques for obtaining nasal symmetry in unilateral complete cleft lip patients: a single surgeon’s experience. Plast Reconstr Surg. 2010;126:1276–1284. doi: 10.1097/PRS.0b013e3181ec21e4. [DOI] [PubMed] [Google Scholar]
- 10.Alef M (2009) Nasal tip complications of primary cleft lip nasoplasty. J Craniofac Surg 20:1327–1333 [DOI] [PubMed]
- 11.Kim I-S, Lee M-Y, Lee K-I, Kim H-Y, Chung Y-J. Analysis of the development of nasal septum accorrding to age and gender using MRI. Clin Exp Otorhinolaryngol. 2008;1:29–34. doi: 10.3342/ceo.2008.1.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]



