Abstract
Context
Major cardiovascular diseases (CVDs) are leading causes of mortality among US Hispanic and Latino individuals. Comprehensive data are limited regarding the prevalence of CVD risk factors in this population and relations of these traits to socioeconomic status (SES) and acculturation.
Objectives
To describe prevalence of major CVD risk factors and CVD (coronary heart disease [CHD] and stroke) among US Hispanic/Latino individuals of different backgrounds, examine relationships of SES and acculturation with CVD risk profiles and CVD, and assess cross-sectional associations of CVD risk factors with CVD.
Design, Setting, and Participants
Multicenter, prospective, population-based Hispanic Community Health Study/Study of Latinos including individuals of Cuban (n =2201), Dominican (n = 1400), Mexican (n=6232), Puerto Rican (n=2590), Central American (n=1634), and South American backgrounds (n = 1022) aged 18 to 74 years. Analyses involved 15 079 participants with complete data enrolled between March 2008 and June 2011.
Main Outcome Measures
Adverse CVD risk factors defined using national guidelines for hypercholesterolemia, hypertension, obesity, diabetes, and smoking. Prevalence of CHD and stroke were ascertained from self-reported data.
Results
Age-standardized prevalence of CVD risk factors varied by Hispanic/Latino background; obesity and current smoking rates were highest among Puerto Rican participants (for men, 40.9% and 34.7%; for women, 51.4% and 31.7%, respectively); hypercholesterolemia prevalence was highest among Central American men (54.9%) and Puerto Rican women (41.0%). Large proportions of participants (80% of men, 71% of women) had at least 1 risk factor. Age- and sex-adjusted prevalence of 3 or more risk factors was highest in Puerto Rican participants (25.0%) and significantly higher (P<.001) among participants with less education (16.1%), those who were US-born (18.5%), those who had lived in the United States 10 years or longer (15.7%), and those who preferred English (17.9%). Overall, self-reported CHD and stroke prevalence were low (4.2% and 2.0% in men; 2.4% and 1.2% in women, respectively). In multivariate-adjusted models, hypertension and smoking were directly associated with CHD in both sexes as were hypercholesterolemia and obesity in women and diabetes in men (odds ratios [ORs], 1.5–2.2). For stroke, associations were positive with hypertension in both sexes, diabetes in men, and smoking in women (ORs, 1.7–2.6).
Conclusion
Among US Hispanic/Latino adults of diverse backgrounds, a sizeable proportion of men and women had adverse major risk factors; prevalence of adverse CVD risk profiles was higher among participants with Puerto Rican background, lower SES, and higher levels of acculturation.
In the last decades, the US hispanic and Latino population has increased dramatically, now comprising the nation’s largest minority group.1 Cardiovascular diseases (CVDs) are leading causes of mortality among Hispanic/Latino individuals in the United States,2 and this relatively young ethnic group is at high risk of future CVD morbidity and mortality as it ages. Evidence also suggests that CVD risk factors and disease rates may vary considerably among Hispanic/ Latino groups. Risk for CVDs among Hispanic/Latino individuals has been reported to differ by degree of acculturation and duration of residence in the United States.3–7
Existing research on CVD risk factors among Hispanic/Latino groups in the United States has largely involved Mexican-American individuals.2,8–10 The few studies that have attempted to examine differences in CVD risk factors within this heterogeneous population have been limited to a few Hispanic/Latino groups11,12 or small sample sizes.13,14
This report expands the literature on Hispanic/Latino health by describing the prevalence of 5 major, readily measured biomedical CVD risk factors (high serum cholesterol and blood pressure levels, obesity, hyperglycemia/diabetes, cigarette smoking), adverse CVD risk profiles (combinations of CVD risk factors; ie, any 1 only, any 2 only, or ≥3 risk factors), and CVD (coronary heart disease [CHD] and stroke) among US Hispanic/Latino adults of diverse backgrounds. Relationships of socioeconomic status (SES), acculturation, and lifestyle factors with adverse CVD risk factor profiles and CVD were examined, and cross-sectional associations of CVD risk factors with self-reported CVD were assessed using data from the landmark Hispanic Community Health Study/Study of Latinos (HCHS/SOL).
METHODS
The HCHS/SOL is a population-based cohort study designed to examine risk and protective factors for chronic diseases and to quantify morbidity and mortality prospectively. Details of the sampling methods and design have been published.15,16 Briefly, between March 2008 and June 2011, the HCHS/ SOL examined 16 415 self-identified Hispanic/Latino persons aged 18 to 74 years recruited from randomly selected households in 4 US communities (Bronx, New York; Chicago, Illinois; Miami, Florida; San Diego, California). Households were selected using a stratified 2-stage area probability sample design.15 Census block groups were randomly selected in the defined community areas of each field center, and households were randomly selected in each sampled block group. Households were screened for eligibility, and Hispanic/Latino persons aged 18 to 74 years were selected in each household agreeing to participate. Oversampling occurred at each stage, with block groups in areas of Hispanic/Latino concentration, households associated with a Hispanic/ Latino surname, and persons aged 45 to 74 years selected at higher rates than their counterparts. Sampling weights were generated to reflect the probabilities of selection at each stage. The HCHS/SOL included participants from Cuban, Dominican, Mexican, Puerto Rican, Central American, and South American backgrounds. The study was approved by institutional review boards at each participating institution; written informed consent was obtained from all participants.
Examination Methods
Participants were asked to fast and refrain from smoking for 12 hours prior to the examination and to avoid vigorous physical activity the morning of the visit. Height was measured to the nearest centimeter and body weight to the nearest 0.1 kg. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. After a 5-minute rest period, 3 seated blood pressure measurements were obtained with an automatic sphygmomanometer; the second and third readings were averaged. Blood samples, including plasma glucose (fasting and after a 2-hour oral glucose load) were collected according to standardized protocols. Total serum cholesterol was measured using a cholesterol oxidase enzymatic method and high-density lipoprotein (HDL) cholesterol with a direct magnesium/dextran sulfate method. Plasma glucose was measured using a hexokinase enzymatic method (Roche Diagnostics). Low-density lipoprotein (LDL) cholesterol was calculated using the Friedewald equation.17 Hemoglobin A1c (HbA1c) was measured using a Tosoh G7 Automated HPLC Analyzer (Tosoh Bioscience).
Information was obtained by questionnaires on demographic factors, SES (education and income), acculturation (including years of residence in the United States, generational status, and language preference), cigarette smoking, physical activity (moderate/heavy intensity work and leisure activities in a typical week), and medical history. Participants were instructed to bring all prescription and nonprescription medications taken in the past month. Dietary intake was ascertained by two 24-hour dietary recalls administered 6 weeks apart. A diet score was calculated by assigning participants a score of 1 to 5 according to sex-specific quintile of daily intake of saturated fatty acids, potassium, calcium, and fiber (with 5 the most favorable quintile). The 4 scores were summed and the highest 40 percentile considered a healthier diet.18
Risk Factors, CHD, and Stroke
Major CVD risk factors were defined based on current national guidelines. Hypercholesterolemia and dyslipidemia were defined as total cholesterol 240 mg/dL or greater, LDL cholesterol 160 mg/dL or greater, or HDL cholesterol less than 40 mg/dL (for persons with and without diabetes) or receiving cholesterol-lowering medication.19 Hypertension was a systolic blood pressure 140 mm Hg or greater, diastolic blood pressure 90 mm Hg or greater, or receiving antihypertensive medication.20 Obesity was defined as a BMI of 30.0 or greater.21 Diabetes mellitus was a fasting plasma glucose 126 mg/dL or greater, 2-hour-postload plasma glucose 200 mg/dL or greater, an HbA1c 6.5% or greater, or use of antihyperglycemic medications.22 Smoking was defined as currently smoking cigarettes. (To convert total, LDL, and HDL cholesterol to mmol/L, multiply by 0.0259; to convert glucose to mmol/L, multiply by 0.0555.)
Prevalent CHD was defined as selfreported history of myocardial infarction, coronary bypass surgery, balloon angioplasty, or stent placement in coronary arteries. Prevalence of stroke was ascertained from self-reported history of stroke.
Statistical Analyses
All reported values (means, prevalence, and odds ratios [ORs]) were weighted to adjust for sampling probability and nonresponse.15,16 Descriptive characteristics, age-standardized to the year 2010 US population, were computed by sex and for all participants by Hispanic/Latino background. Additional analyses age-standardized to the year 2000 US population were also conducted. Mean levels and prevalence of individual risk factors, adverse CVD risk profiles (ie, presence of 0, any 1 only, any 2 only, any ≥3 risk factors), and self-reported CVD were computed by sex and by Hispanic/Latino group. Prevalence was also assessed of various combinations of risk factors, and self-reported CHD and stroke stratified by age and sex. Survey-specific procedures were used to compute 95% confidence intervals to account for the 2-stage sampling design, stratification, and clustering. Comparisons across Hispanic/Latino groups were performed using the overall Wald test.
Age- and sex-adjusted prevalence of adverse CVD risk profiles and selfreported CHD and stroke were calculated for the total cohort by age group (sex-adjusted only), sex (age-adjusted only), SES, acculturation, and lifestyle factors. Similar analyses were done for individual risk factors.
Logistic regression analyses were used to examine associations of CVD risk factors with CHD and stroke prevalence for men and women separately. Models were adjusted for age only (model 1); age plus all other major CVD risk factors (model 2); and all variables in model 2 plus education, annual family income, Hispanic/ Latino background, language preference, nativity (US-born), Short Acculturation Scale for Hispanics (SASH) score, physical activity, diet (model 3). Age, years of education, years resided in the United States, and SASH score were continuous variables, and the remaining variables were categorical. Odds ratios with 95% CIs were computed. All statistical tests were 2-sided at a significance level of .05. No adjustments were made for multiple comparisons. All analyses were performed using SAS version 9.2 (SAS Institute) and SUDAAN release 10.0.0 (RTI).
RESULTS
Household-level response rate was 33.5%. Of 39 384 individuals who were screened and selected and who met eligibility criteria, 41.7% were enrolled, representing 16 415 persons from 9872 households.
Of the 16 415 HCHS/SOL participants, 772 were excluded from analyses here because of missing data on total cholesterol (n =16), BMI (n = 48), cigarette smoking (n = 39), self-reported CHD (n =19), stroke (n = 9), or other covariates (n = 641). In addition, 9 participants 75 years and older and 555 participants who did not self-identify as any of the 6 aforementioned Hispanic/Latino groups were excluded. Thus, these analyses are based on data from 15 079 participants (5979 men; 9100 women).
Participant Characteristics
Mean baseline ages standardized to year 2010 US population were similar in all Hispanic/Latino groups (range 43 to ~44 years) (Table 1). About 15% of the sample had a college degree, and 37% had annual family income between $20 000 and $50 000. Approximately 51% were married or living with a partner. Seventy percent had lived in the United States for 10 or more years. Spanish was the preferred language for the majority (78%). These demographic characteristics varied across Hispanic/Latino groups. Sex-specific and other characteristics are described in eTable 1 and eTable 2 (available at http://www.jama.com).
Table 1.
Descriptive Characteristics for All Participants and by Hispanic/Latino Group (Age Standardized)a
| % (95% CI) |
|||||||
|---|---|---|---|---|---|---|---|
| Characteristic | All (N = 15 079) |
Cuban (n = 2201) |
Dominican (n = 1400) |
Mexican (n = 6232) |
Puerto Rican (n = 2590) |
Central American (n = 1634) |
South American (n = 1022) |
| Women, No. | 9100 | 1167 | 920 | 3895 | 1523 | 986 | 609 |
| Age, mean, yb | 43.2 (43.1–43.3) | 43.5 (43.3–43.7) | 43.1 (42.9–43.3) | 43.0 (42.9–43.2) | 43.2 (43.0–43.4) | 43.4 (43.2–43.6) | 43.2 (42.9–43.4) |
| Educationb | |||||||
| <High school | 35.3 (33.8–36.8) | 21.2 (19.2–23.4) | 40.2 (36.9–43.6) | 41.5 (38.9–44.2) | 35.7 (32.8–38.8) | 40.1 (36.9–43.5) | 24.0 (20.4–28.0) |
| High school graduate | 27.4 (26.4–28.5) | 30.9 (28.2–33.7) | 22.3 (19.0–25.9) | 26.9 (25.4–28.5) | 28.0 (25.8–30.4) | 24.4 (21.7–27.2) | 26.8 (23.5–30.4) |
| Some college | 22.0 (20.9–23.1) | 27.7 (25.1–30.5) | 21.9 (19.2–24.9) | 19.2 (17.7–20.9) | 21.7 (19.1–24.5) | 20.6 (17.8–23.8) | 26.8 (23.4–30.4) |
| College degree | 15.3 (14.0–16.6) | 20.2 (17.5–23.2) | 15.6 (13.4–18.1) | 12.4 (10.2–14.9) | 14.5 (12.6–16.7) | 14.8 (12.6–17.4) | 22.4 (19.3–25.9) |
| Annual family income, $b | |||||||
| <20000 | 42.6 (40.9–44.3) | 45.1 (42.3–48.0) | 50.9 (47.0–54.7) | 38.0 (35.2–40.9) | 44.0 (40.6–47.5) | 47.3 (43.4–51.2) | 40.3 (36.1–44.6) |
| 20 000–50 000 | 37.3 (36.1–38.5) | 31.4 (28.6–34.4) | 32.4 (29.2–35.8) | 42.2 (40.4–44.0) | 33.6 (30.4–36.9) | 34.6 (31.2–38.2) | 40.0 (36.3–43.9) |
| > 50 000 | 11.4 (10.1–12.9) | 8.2 (6.3–10.7) | 7.2 (5.3–9.5) | 14.0 (11.7–16.6) | 14.0 (11.9–16.4) | 7.2 (5.6–9.3) | 11.6 (9.3–14.4) |
| Not reported | 8.7 (8.0–9.4) | 15.3 (13.2–17.5) | 9.5 (7.8–11.6) | 5.9 (5.1–6.7) | 8.4 (7.1–9.9) | 10.9 (9.1–12.9) | 8.0 (6.0–10.7) |
| Marital statusb | |||||||
| Single | 31.0 (29.9–32.1) | 30.0 (27.6–32.4) | 41.1 (37.9–44.4) | 23.3 (21.9–24.8) | 45.6 (42.5–48.8) | 34.2 (31.4–37.1) | 29.5 (26.5–32.7) |
| Married or living with a partner | 51.1 (49.6–52.5) | 50.3 (47.3–53.2) | 39.8 (36.2–43.5) | 61.3 (59.2–63.3) | 34.9 (31.9–38.1) | 47.8 (44.6–51.1) | 50.4 (46.5–54.3) |
| Separated, divorced, or widowed | 18.0 (17.0–18.9) | 19.8 (17.9–21.7) | 19.1 (16.5–22.0) | 15.4 (14.1–16.9) | 19.5 (17.2–21.9) | 18.0 (15.8–20.4) | 20.1 (17.4–23.1) |
| US residence >10 yb | 69.5 (67.6–71.4) | 45.1 (41.1–49.1) | 73.6 (70.0–76.9) | 73.2 (71.1–75.3) | 92.7 (90.9–94.2) | 62.6 (58.8–66.3) | 53.9 (49.4–58.3) |
| Immigrant generational statusb | |||||||
| First | 78.5 (77.1–79.8) | 90.9 (88.4–93.0) | 86.9 (83.8–89.5) | 77.8 (75.9–79.6) | 49.6 (47.1–52.2) | 93.4 (91.1–95.1) | 94.1 (91.8–95.8) |
| Second or higher | 21.5 (20.2–22.9) | 9.1 (7.0–11.6) | 13.1 (10.5–16.2) | 22.2 (20.4–24.1) | 50.4 (47.8–52.9) | 6.6 (4.9–8.9) | 5.9 (4.2–8.2) |
| Language preferenceb | |||||||
| Spanish | 77.5 (75.9–79.0) | 91.9 (88.9–92.9) | 80.4 (76.8–83.7) | 81.4 (79.6–83.1) | 42.7 (39.4–46.2) | 89.0 (86.0–91.4) | 89.9 (87.1–92.1) |
| English | 22.5 (21.0–24.1) | 8.9 (7.1–11.1) | 19.6 (16.3–23.2) | 18.6 (16.9–20.4) | 57.3 (53.8–60.6) | 11.0 (8.6–14.0) | 10.1 (7.9–12.9) |
| Health insuranceb | 50.9 (49.2–52.5) | 40.0 (37.1–43.0) | 72.3 (68.4–75.9) | 44.7 (42.4–46.9) | 77.3 (74.5–79.9) | 34.4 (30.8–38.2) | 41.9 (37.6–46.3) |
| Physical activity, higher 40%b,c | 39.1 (37.9–40.2) | 29.7 (27.3–32.3) | 37.1 (33.1–41.2) | 42.1 (40.3–43.8) | 41.1 (38.3–44.0) | 43.2 (40.1–46.2) | 37.0 (33.1–41.1) |
| Diet score, higher 40%b,d | 46.1 (44.2–48.0) | 36.2 (33.6–38.9) | 19.6 (17.0–22.5) | 69.2 (67.3–71.0) | 18.9 (16.6–21.3) | 39.5 (36.2–43.0) | 40.7 (36.8–44.7) |
Values (except No. of women) are weighted for study design and nonresponse and age standardized to Census 2010 US population
P<.001.
Higher sex-specific 40% of mean total physical activity.
Diet score was calculated by assigning participants a score of 1–5 according to their sex-specific quintile of daily intake of saturated fatty acids, potassium, calcium, and fiber, with 5 representing the most favorable quintile (ie, lowest quintile of intake for saturated fatty acids and highest quintile of intake for potassium, calcium, and fiber). The 4 scores were summed and the higher 40 percentile considered a healthier diet.
Prevalence of Major CVD Risk Factors
The overall prevalence of hypercholesterolemia was 52% among men and ranged from 48% (Dominican and Puerto Rican men) to 55% (Central American men). In women, prevalence of hypercholesterolemia was 37% and ranged from 31% (South American women) to 41% (Puerto Rican women) (Table 2).
Table 2.
Prevalence of Cardiovascular Disease Risk Factors for All Participants and by Hispanic/Latino Group and Sex (Age Standardized)a
| % (95% CI) |
|||||||
|---|---|---|---|---|---|---|---|
| Characteristicb | All | Cuban | Dominican | Mexican | Puerto Rican | Central American |
South American |
| Men, No. | 5979 | 1034 | 480 | 2337 | 1067 | 648 | 413 |
| Hypertensionc | 25.4 (24.1–26.7) | 28.9 (26.6–31.4) | 32.6 (28.2–37.4) | 21.4 (19.1–24.0) | 27.4 (24.5–30.5) | 25.0 (21.8–28.5) | 19.9 (16.0–24.4) |
| Hypercholesterolemia | 51.7 (50.1–53.3) | 53.7 (50.3–57.1) | 47.6 (42.3–52.9) | 53.9 (51.4–56.3) | 48.2 (43.8–52.6) | 54.9 (50.5–59.1) | 52.2 (45.3–58.9) |
| Obesityc | 36.5 (34.7–38.3) | 33.6 (30.2–37.3) | 38.6 (33.1–44.5) | 36.8 (33.9–39.8) | 40.9 (36.8–45.1) | 32.7 (28.7–36.9) | 26.8 (22.4–31.9) |
| Diabetes mellitusc | 16.7 (15.5–17.9) | 13.2 (11.3–15.3) | 18.2 (15.0–21.9) | 19.3 (17.0–21.8) | 16.2 (14.0–18.7) | 16.3 (13.1–20.1) | 10.1 (7.2–14.1) |
| Smokingc | 25.7 (24.1–27.4) | 31.1 (27.6–34.8) | 11.1 (7.7–15.7) | 23.1 (20.8–25.7) | 34.7 (30.7–38.9) | 19.9 (16.4–24.0) | 15.1 (11.0–20.4) |
| Women, No. | 9100 | 1167 | 920 | 3895 | 1523 | 986 | 609 |
| Hypertensionc | 23.5 (22.4–24.5) | 26.4 (24.5–28.3) | 26.1 (23.2–29.3) | 19.5 (17.8–21.3) | 29.1 (26.4–31.9) | 25.6 (22.9–28.4) | 15.9 (13.2–19.0) |
| Hypercholesterolemiad | 36.9 (35.6–38.3) | 37.5 (33.8–41.4) | 33.1 (29.7–36.6) | 36.2 (30.4–38.4) | 41.0 (36.9–45.1) | 39.4 (35.4–43.5) | 31.4 (27.3–35.8) |
| Obesityc | 42.6 (41.0–44.2) | 38.9 (35.3–42.7) | 42.5 (37.8–47.2) | 41.5 (38.8–44.2) | 51.4 (47.6–55.1) | 41.6 (37.9–45.4) | 30.8 (26.0–36.0) |
| Diabetes mellitusc | 17.2 (16.3–18.3) | 13.9 (12.0–16.0) | 18.0 (15.4–21.0) | 18.5 (16.8–20.2) | 19.4 (17.0–22.1) | 17.9 (15.0–21.3) | 9.8 (7.8–12.3) |
| Smokingc | 15.2 (14.1–16.5) | 21.2 (18.6–24.0) | 11.7 (8.3–16.4) | 10.0 (8.3–11.9) | 31.7 (28.3–35.2) | 8.7 (6.7–11.2) | 11.3 (8.6–14.8) |
Values (except No.) weighted for survey design and nonresponse and age standardized to Census 2010 US population.
Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or receiving treatment. Hypercholesterolemia was defined as total cholesterol ≥240 mg/dL, high-density lipoprotein cholesterol <40 mg/dL, low-density lipoprotein cholesterol ≥160 mg/dL, or receiving treatment. Obesity was defined as a body mass index ≥30, calculated as weight in kilograms divided by height in meters squared. Diabetes mellitus was defined as fasting glucose ≥126 mg/dL, 2-hour-postload plasma glucose ≥200 mg/dL, hemoglobin A1c ≥6.5%, or use of diabetes medications. Smoking was defined as currently smoking cigarettes. (To convert total, LDL, and HDL cholesterol to mmol/L, multiply by 0.0259; to convert glucose to mmol/L, multiply by 0.0555.)
P<.001.
P<.01.
Overall, 25% of men had hypertension; hypertension prevalence was highest among Dominican men. Hypertension prevalence overall among women was 24%. The prevalence of hypertension ranged from 16% (South American women) to 29% (Puerto Rican women) (Table 2).
About 37% of men were obese; prevalence of obesity ranged from 27% (South American men) to 41% (Puerto Rican men). Among women, overall prevalence of obesity was 43%. Prevalence of obesity was highest among Puerto Rican women (Table 2).
Overall, 17% of men and women had diabetes. Prevalence ranged from 10% in South American men and women to 19% in Mexican men and women and Puerto Rican women (Table 2).
About 26% of men were current smokers, with highest prevalence of smoking among Puerto Rican men. Overall, current smoking prevalence in women was low (15%). However, 32% of Puerto Rican women and 21% of Cuban women were current smokers (Table 2).
Mean levels of individual risk factors varied by Hispanic/Latino group (eTable 3 and eTable 4). For example, among men, those of Central American background had the highest mean level of total cholesterol, and those of Central and South American backgrounds had higher mean levels of LDL cholesterol compared with others. Among women, those of Cuban and Central American background had higher mean total cholesterol levels than other groups; Cuban women also had the highest average level of LDL cholesterol.
About 15% of men and women were currently using an antihypertensive medication. Use of antihypertensive medications was highest among Dominican men; in women, antihypertensive medication use was higher among those of Puerto Rican and Dominican backgrounds. Dominican and Mexican men and Puerto Rican women had the highest rate of antihyperglycemic medication use (eTable 3 and eTable 4).
When analyses were repeated on the whole sample without exclusions other than missing data for the major CVD risk factors, prevalences were almost identical to those in Table 2.
Prevalence rates age-standardized to year 2000 US population were slightly lower (~1 percentage point) than rates reported earlier in this section.
CVD Risk Profiles and Self-reported CVD
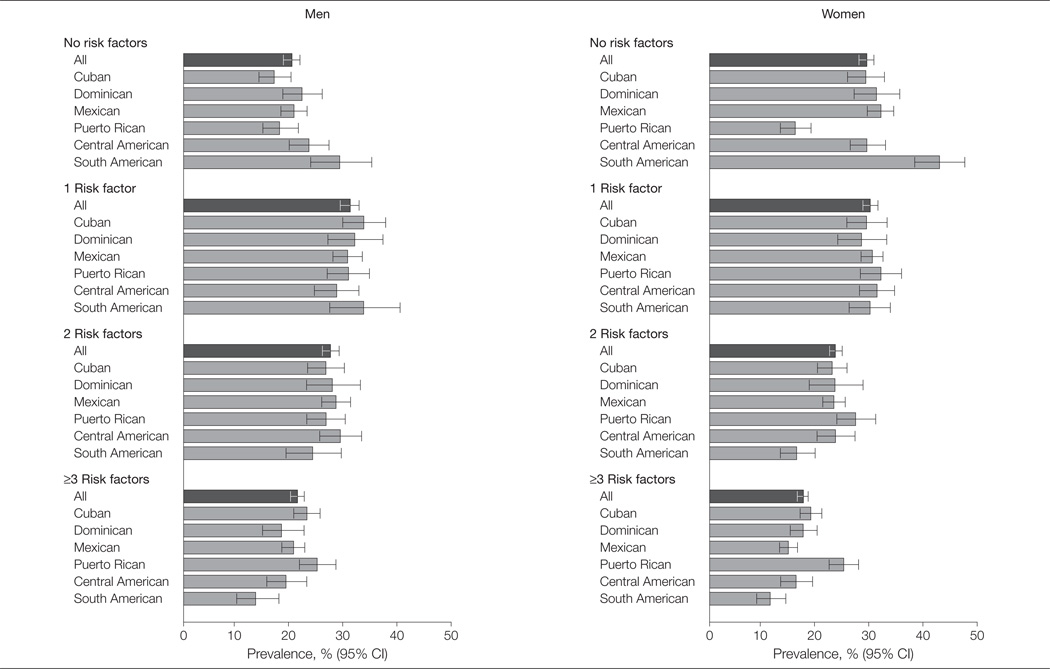
Overall, 31% of men had an adverse level of any 1 major risk factor only (most commonly hypercholesterolemia); 28% and 21% had any 2 only or 3 or more risk factors (Figure 1). Prevalence of 3 or more risk factors was highest among Puerto Rican men and lowest among South American men. Among women, 30% had 1 risk factor only (most commonly obesity); 23% and 17% had any 2 or 3 or more risk factors (Figure 1). Prevalence of 3 or more risk factors was highest among Puerto Rican women and lowest among South American women. Specific combinations of individual risk factors by sex are shown in eTable 5 and eTable 6.
Figure 1. Prevalence of Adverse Cardiovascular Disease Risk Profiles for All Participants and by Hispanic/Latino Group and Sex.
Risk factors were hypercholesterolemia (serum total cholesterol ≥240 mg/dL or taking cholesterol-lowering medication), hypertension (systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg or taking antihypertensive medication), obesity (body mass index ≥30, calculated as weight in kilograms divided by height in meters squared), diabetes mellitus (use of diabetes medication, fasting glucose ≥126 mg/dL, 2-hour-postload plasma glucose ≥200 mg/dL, or hemoglobin A1c ≥6.5%), and smoking (current cigarette smoker). Values were weighted for survey design and nonresponse and adjusted for age. Error bars indicate 95% CI.
The overall prevalence of CHD and stroke was, respectively, 4% and 2% for men and 2% and 1% for women. Prevalence of CHD was highest among Puerto Rican men and women and Cuban and Dominican men (5%); self-reported stroke was highest for Dominican men (4%) and Puerto Rican women (2%) (eTable 7).
A significantly higher proportion of men than women, and those aged 65 to 74 years compared with younger persons had 3 or more risk factors (Table 3). Prevalence of 3 or more risk factors was significantly higher (P< .001) with lower education or income. In general, participants with lower income or education had higher rates of smoking, diabetes, obesity, and hypercholesterolemia (eTable 8). Compared with those who were less acculturated (ie, were foreign-born or firstgeneration immigrants, had lived in the United States <10 years, or for whom Spanish was the preferred language), more acculturated participants had higher prevalence of 3 or more risk factors. In sensitivity analyses excluding Puerto Rican participants (the most acculturated group who also had the highest prevalence of multiple risk factors), the magnitude of difference in prevalence of 3 or more risk factors by acculturation level was slightly lower; findings remained significant although level of significance was diminished. In general, more acculturated participants had markedly higher rates of current smoking and obesity compared with others. Additionally, participants with lower physical activity levels and less healthy diets had higher prevalence of 3 or more CVD risk factors.
Table 3.
Number of Adverse CVD Risk Factors and Prevalence of Self-reported CVD (CHD and Stroke) by Age, Education, Income, Acculturation, and Lifestyle Factors Among Hispanic/Latino Participants (Age and Sex Adjusted)a
| % (95%CI) |
||||||
|---|---|---|---|---|---|---|
| Characteristic | No Risk Factorsb | 1 Risk Factorb | 2 Risk Factorsb | ≥3 Risk Factorsb | CHD | Stroke |
| Age groupa | ||||||
| 18–44 | 35.8 (34.0–37.7)c | 33.8 (32.2–35.5) | 21.5 (20.1–22.9)c | 8.9 (8.0–9.8)c | 0.7 (0.5–1.2)c | 0.6 (0.4–0.9)d |
| 45–64 | 14.0 (12.9–15.3) | 30.1 (28.6–31.7) | 29.0 (27.5–30.6) | 26.8 (25.2–28.5) | 4.5 (3.9–5.2) | 2.0 (1.6–2.5) |
| 65–74 | 6.5 (4.7–8.8) | 18.0 (15.2–21.1) | 32.5 (28.7–36.5) | 43.1 (39.4–46.8) | 9.0 (7.2–11.3) | 4.3 (3.2–5.8) |
| Sexa | ||||||
| Male | 19.4 (17.8–21.1)c | 34.1 (32.3–36.0) | 29.2 (27.5–31.0)c | 17.2 (15.8–18.8)c | 2.0 (1.5–2.6)c | 1.2 (0.8–1.7)d |
| Female | 30.4 (28.9–32.0) | 33.5 (31.9–35.1) | 23.7 (22.3–25.2) | 12.4 (11.5–13.4) | 1.1 (0.8–1.5) | 0.7 (0.5–1.0) |
| Education | ||||||
| <High school | 21.2 (19.3–23.2)c | 34.8 (32.9–36.7) | 27.1 (25.5–28.9)d | 16.9 (15.5–18.4)c | 1.6 (1.1–2.4) | 0.9 (0.6–1.2) |
| High school graduate | 23.6 (21.8–25.5) | 32.9 (30.7–35.1) | 28.7 (26.5–31.1) | 14.8 (13.3–16.4) | 1.3 (1.0–1.7) | 1.0 (0.6–1.5) |
| Some college | 26.0 (23.9–28.3) | 34.8 (32.2–37.6) | 25.9 (23.6–28.3) | 13.3 (11.8–14.9) | 1.5 (1.0–2.1) | 1.0 (0.6–1.5) |
| College degree | 32.5 (29.0–36.3) | 33.9 (30.8–37.2) | 21.7 (19.4–24.2) | 11.8 (9.9–14.1) | 1.4 (0.9–2.0) | 0.8 (0.4–1.3) |
| Annual family income, $ | ||||||
| <20000 | 21.1 (19.6–22.7)c | 34.9 (32.9–36.8) | 27.9 (26.2–29.7) | 16.2 (14.8–17.6)d | 1.8 (1.3–2.5) | 1.3 (1.0–1.7)d |
| 20 000–50 000 | 26.4 (24.5–28.3) | 33.4 (31.5–35.3) | 25.7 (24.1–27.3) | 14.6 (13.3–15.9) | 1.2 (1.0–1.6) | 0.7 (0.5–1.1) |
| ≥ 50 000 | 31.7 (27.0–36.7) | 35.0 (31.5–38.7) | 23.1 (20.0–26.4) | 10.3 (8.2–12.8) | 1.2 (0.7–2.0) | 0.3 (0.1–1.1) |
| Not reported | 26.0 (22.6–29.8) | 32.3 (28.8–36.0) | 27.6 (24.2–31.3) | 14.1 (12.0–16.5) | 1.4 (0.9–2.2) | 1.0 (0.5–1.8) |
| Country of birth | ||||||
| Foreign | 26.4 (25.1–27.8)c | 34.7 (33.3–36.0) | 25.4 (24.2–26.7)d | 13.5 (12.5–14.4)c | 1.3 (1.0–1.8)e | 0.7 (0.5–0.9)c |
| US | 18.5 (16.2–21.0) | 32.1 (29.4–34.9) | 30.1 (27.4–33.0) | 19.3 (17.0–21.8) | 2.1 (1.4–3.1) | 1.8 (1.2–2.8) |
| US residence >10 y | ||||||
| No | 29.2 (27.1–31.4)c | 34.7 (32.7–36.8) | 24.8 (23.1–26.6) | 11.2 (9.9–12.7)c | 0.8 (0.5–1.1)c | 0.7 (0.4–1.1) |
| Yes | 22.7 (21.3–24.1) | 33.8 (32.3–35.3) | 27.2 (25.9–28.6) | 16.3 (15.2–17.5) | 1.8 (1.3–2.4) | 1.0 (0.8–1.4) |
| Language preference | ||||||
| Spanish | 26.3 (24.8–27.9)c | 34.4 (32.9–35.8) | 25.8 (24.6–27.1) | 13.5 (12.6–14.5)c | 1.3 (1.0–1.8)e | 0.8 (0.6–1.1)d |
| English | 19.6 (17.5–21.8) | 33.2 (30.7–35.9) | 28.5 (26.1–31.1) | 18.7 (16.6–20.9) | 2.0 (1.4–2.8) | 1.4 (1.0–2.0) |
| Immigrant generational status | ||||||
| First | 26.5 (25.1–27.9)c | 34.6 (33.3–36.1) | 25.5 (24.3–26.8)e | 13.3 (12.4–14.3)c | 1.3 (0.9–1.8)e | 0.7 (0.5–1.0)c |
| Second or higher | 18.8 (16.6–21.2) | 32.2 (29.6–34.8) | 29.6 (27.0–32.3) | 19.4 (17.2–21.8) | 2.1 (1.5–3.1) | 1.7 (1.1–2.5) |
| Age at immigration | ||||||
| US born | 17.6 (15.4–20.0)c | 32.6 (29.9–35.4) | 30.4 (27.6–33.2)e | 19.5 (17.2–22.0)c | 2.1 (1.4–3.1)c | 1.8 (1.2–2.8)c |
| ≤10 y | 21.5 (18.2–25.2) | 36.2 (31.4–41.3) | 25.1 (21.0–29.7) | 17.3 (13.6–21.7) | 1.5 (1.0–2.3) | 1.2 (0.6–2.3) |
| 11–24 y | 24.5 (22.7–26.4) | 35.5 (33.6–37.5) | 25.9 (24.1–27.9) | 14.0 (12.7–15.4) | 1.7 (1.1–2.5) | 0.5 (0.3–0.8) |
| ≥25 y | 29.4 (27.2–31.7) | 33.3 (31.4–35.3) | 25.0 (23.3–26.7) | 12.3 (11.2–13.6) | 1.0 (0.8–1.3) | 0.7 (0.5–1.0) |
| Acculturation, SASH scoref | ||||||
| Low, 1–<3 | 25.8 (24.4–27.2)c | 34.6 (33.2–36.0) | 25.9 (24.7–27.2) | 13.8 (12.8–14.8)c | 1.3 (1.0–1.8) | 0.7 (0.5–1.0)c |
| High, ≥3 | 20.7 (18.3–23.2) | 32.2 (29.6–35.0) | 28.7 (26.0–31.5) | 18.4 (16.1–20.9) | 2.0 (1.3–2.9) | 1.7 (1.2–2.5) |
| Physical activity, higher 40%g | ||||||
| Yes | 25.9 (24.1–27.8) | 35.3 (33.5–37.1) | 26.4 (24.7–28.2) | 12.5 (11.4–13.6)c | 1.4 (1.0–2.0) | 0.9 (0.6–1.4) |
| No | 24.0 (22.4–25.6) | 33.3 (31.8–34.8) | 26.5 (25.1–28.0) | 16.2 (15.0–17.5) | 1.5 (1.1–1.9) | 0.9 (0.7–1.2) |
| Diet score, higher 40%h | ||||||
| Yes | 28.1 (26.0–30.2)c | 33.9 (32.1–35.7) | 25.1 (23.5–26.7) | 12.9 (11.7–14.2)c | 1.1 (0.8–1.4)c | 0.7 (0.5–0.9)d |
| No | 21.9 (20.5–23.3) | 34.3 (32.6–35.9) | 27.6 (26.2–29.1) | 16.2 (15.1–17.4) | 1.8 (1.3–2.4) | 1.1 (0.8–1.5) |
Abbreviations: CHD, coronary heart disease; CVD, cardiovascular disease; SASH, Short Acculturation Scale for Hispanics.
Prevalence by age group was adjusted for sex. Prevalence by sex was adjusted for age. The average age used for the computation was 41.02 years (overall weighted mean age). Values (except No.) were weighted for survey design and nonresponse. Model-adjusted prevalence was obtained based on multinomial logistic regression for risk factor profiles and logistic regression for CHD and stroke.
Adverse CVD risk factors were defined as follows. Hypercholesterolemia was total cholesterol ≥240 mg/dL, high-density lipoprotein cholesterol <40 mg/dL, low-density lipoprotein cholesterol ≥160 mg/dL, or receiving treatment. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or receiving treatment. Obesity was defined as a body mass index ≥30, calculated as weight in kilograms divided by height in meters squared. Diabetes mellitus was defined as use of diabetes medications, fasting glucose ≥126 mg/dL, 2-hour-postload plasma glucose ≥200 mg/dL, or hemoglobin A1c ≥6.5%. Smoking was defined as currently smoking cigarettes. (To convert total, LDL, and HDL cholesterol to mmol/L, multiply by 0.0259; to convert glucose to mmol/L, multiply by 0.0555.)
P<.001.
P<.01.
P<.05.
An abbreviated 10-question SASH was used; the range of scores was 1–5. Average scores <3 indicate lower acculturation and scores ≥3 indicate higher acculturation.
Higher sex-specific 40% of mean total physical activity.
Diet score was calculated by assigning participants a score of 1–5 according to their sex-specific quintile of daily intake of saturated fatty acids, potassium, calcium, and fiber, with 5 representing the most favorable quintile (ie, lowest quintile of intake for saturated fatty acids and highest quintile of intake for potassium, calcium, and fiber). The 4 scores were summed and the higher 40 percentile considered a healthy diet.
Age- and sex-adjusted prevalence of CHD and stroke were significantly higher among men, older participants (aged 65–74 years compared with younger), those who were second- or third-generation immigrants, and those who preferred English (Table 3). Additionally, CHD prevalence was significantly higher among participants who had resided in the United States 10 or more years, and stroke prevalence was significantly higher among participants with lower family income and those born in the United States. Unweighted cell counts corresponding to weighted prevalences in eTables 1– 8 are presented in eTables 9–16.
Association of CVD Risk Factors With CHD and Stroke
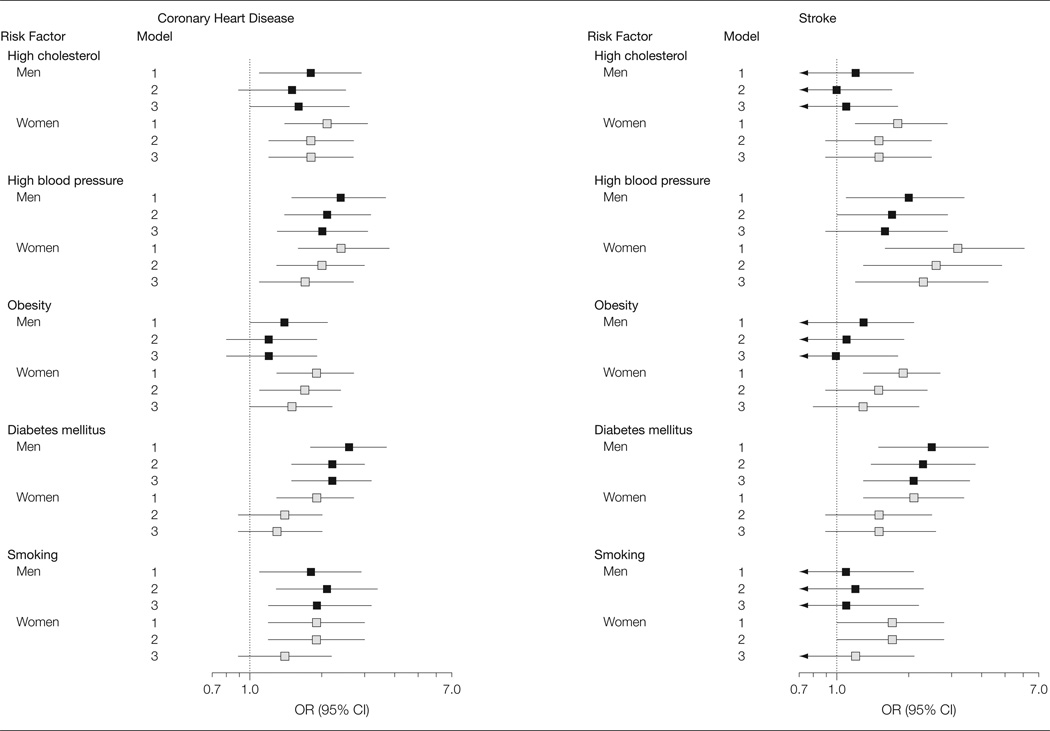
In age-adjusted analyses (model 1), all individual CVD risk factors were associated with higher odds of prevalent CHD (Figure 2); associations were especially strong for hypertension and diabetes. Associations of CVD risk factors with self-reported CHD were attenuated and in some cases lost statistical significance, with additional adjustment for other CVD risk factors (model 2) or for variables in model 3.
Figure 2. Association of Cardiovascular Disease Risk Factors With Cardiovascular Disease Prevalence Among Hispanic/Latino Participants by Sex.
High cholesterol was defined as serum total cholesterol level ≥240 mg/dL or taking cholesterol-lowering medication. High blood pressure was defined as systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg or taking antihypertensive medication. Obesity was defined as a body mass index ≥30 (calculated as weight in kilograms divided by height in meters squared). Diabetes mellitus was defined as use of diabetes medication, fasting glucose ≥126 mg/dL, 2-hour-postload plasma glucose ≥200 mg/dL, or hemoglobin A1c ≥6.5%. Smoking was defined as current cigarette smoker. Model 1 was adjusted for age. Model 2 was adjusted for age and all other major biomedical cardiovascular disease risk factors. Model 3 was adjusted for all variables in model 2 plus education, annual family income, Hispanic/ Latino background, language preference, nativity (US born), Short Acculturation Scale for Hispanics score, physical activity, and diet. Error bars indicate 95% CI.
Associations of risk factors with prevalent stroke were less consistent (Figure 2). In age-adjusted analyses (model 1), hypertension and diabetes mellitus were strongly associated with prevalent stroke in both sexes; high cholesterol and obesity were significantly associated and cigarette smoking was borderline significantly associated with prevalent stroke among women only. With further adjustment for other CVD risk factors (model 2), the association of hypertension with prevalent stroke was attenuated but remained significant in women and borderline significant in men, diabetes remained significantly associated with stroke in men, and smoking was borderline significantly associated with stroke in women only. With additional adjustment for variables in model 3, diabetes and hypertension remained positively associated with stroke among men and women, respectively.
COMMENT
The HCHS/SOL baseline examination has yielded several insights about CVD risk factors among adult Hispanic/ Latino men and women living in the United States. Prevalence of individual major CVD risk factors varied markedly across Hispanic background groups. Moreover, as compared with first-generation participants (born outside of the United States), participants who were US-born were more likely to report a history of CHD and stroke and to have multiple CVD risk factors. Additionally, higher prevalence of CVD was associated with longer duration of residence in the United States and greater acculturation. Thus, although numerous US studies have demonstrated racial/ethnic variations in CVD and its risk factors, our findings demonstrate a great deal of diversity within a population that would typically be classified as a single “Hispanic/Latino” group in biomedical research.
Previous studies of US Hispanic/ Latino individuals have primarily involved Mexican American participants or have considered Hispanics/Latinos as a single group.2,8–10,23–26 The limited available data on Hispanic/Latino people from diverse ethnic, geographic, cultural, and socioeconomic backgrounds suggest that CVD risk factor burden may vary by Hispanic/Latino origin and sociocultural characteristics. However, findings on intergroup variation in individual CVD risk factor prevalence have been inconsistent.11–14,27
The HCHS/SOL aimed to address the gap in current knowledge on prevalence of CVD risk factors and adverse CVD risk profiles within the diverse Hispanic/Latino population and relationships of sociocultural factors and acculturation to risk factors. Baseline HCHS/SOL findings demonstrate the sizeable burden of CVD risk factors among all Hispanic/Latino groups with prevalence of risk factors comparable or higher than those reported for non-Hispanic white individuals.28,29 The HCHS/SOL data show marked variation in CVD risk factor prevalence within the Hispanic/Latino population with some groups, particularly those of Puerto Rican background, experiencing strikingly high rates of individual adverse CVD risk factors or overall risk factor burden compared with others. For example, women of Puerto Rican background had the highest prevalence of each of the major CVD risk factors, and Mexican men and women both had high rates of diabetes. Thus, results from the HCHS/SOL suggest that previous prevalence estimates based on data primarily from Mexican American participants may have underestimated the CVD risk factor burden and diversity among US Hispanics/Latinos.
Studies in diverse Latin American countries have demonstrated similar variations in prevalence of CVD risk factors. The cross-sectional population-based Cardiovascular Risk Factor Multiple Evaluation in Latin America (CARMELA) study30 examined participants from Mexico and 6 South American countries; Mexican participants had higher prevalence of obesity and diabetes compared with South American participants, consistent with findings reported here. Rates of hypertension and cigarette smoking were higher in CARMELA participants from some South American countries, in contrast to generally lower risk factor burden among South American participants in the HCHS/ SOL; these differences are likely due to differential patterns of immigration to the United States.
Among HCHS/SOL participants, major CVD risk factors were strongly associated with prevalent self-reported CVD. These findings are consistent with those reported by studies in Latin American populations such as the INTERHEART Study, ie, strong associations of CVD risk factors with risk of acute myocardial infarction.31,32
In other racial/ethnic groups with little or no CVD originally, migration and adoption of Western lifestyles have been associated with development of unfavorable risk factor profiles and CVD.33–35 In the HCHS/SOL, higher degrees of acculturation by multiple proxy measures were associated with higher prevalence of multiple adverse CVD risk factors. Moreover, more acculturated participants—particularly those born in the United States—were significantly more likely to have prevalent CHD and stroke. Mexican background participants from the HCHS/SOL had higher rates of hypertension and obesity compared with those from the CARMELA study (based on similar definitions for these risk factors).30 Thus, findings from the HCHS/SOL suggest that CVD risk status of Hispanic/Latino individuals is likely to worsen over time with increasing adoption of US lifestyles.
Findings here are limited to selfreported information on prevalent CHD and stroke (possibly biased by access to health care) and the cross-sectional nature of the data. However, the planned long-term follow-up of HCHS/ SOL participants will produce objective information on incident CVD and non-CVD outcomes. A further limitation is that the HCHS/SOL did not include any other US racial/ethnic groups for comparison. However, the data were age-standardized to the year 2000 US population to allow for comparisons with observations from national surveys, and protocols used were similar to those of other epidemiological studies.
In conclusion, findings from the HCHS/SOL demonstrate the pervasive burden of CVD risk factors in all Hispanic/Latino groups in the United States and identify specific groups by origin, sociodemographic characteristics, and sociocultural backgrounds at particularly high risk of CVD. These data may enhance the impetus to implement interventions to lower the burden of CVD risk factors among Hispanic/Latino people overall and targeted at-risk groups, as well as develop strategies to prevent future development of adverse CVD risk factors starting at the youngest ages.
Acknowledgments
Funding/Support: The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237). The following institutes, centers, or offices contribute to the HCHS/SOL through a transfer of funds to the NHLBI: National Center on Minority Health and Health Disparities, the National Institute on Deafness and Other Communications Disorders, the National Institute of Dental and Craniofacial Research, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the Office of Dietary Supplements.
Role of the Sponsor: The funding agency had a role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; and in the review and approval of the manuscript.
Appendix
The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Investigators: Program Office: National Heart, Lung, and Blood Institute, Bethesda, Maryland: Larissa Avilé s-Santa, Paul Sorlie, Lorraine Silsbee. Field Centers: Bronx Field Center, Albert Einstein School of Medicine, Bronx, New York: Robert Kaplan, Sylvia Wassertheil-Smoller. Chicago Field Center, Northwestern University Feinberg School of Medicine and University of Illinois at Chicago: Martha L. Daviglus, Aida L. Giachello, Kiang Liu. Miami Field Center, University of Miami, Miami, Florida: Neil Schneiderman, David Lee, Leopoldo Raij. San Diego Field Center, San Diego State University and University of California, San Diego: Greg Talavera, John Elder, Matthew Allison, Michael Criqui. Coordinating Center: University of North Carolina, Chapel Hill: Jianwen Cai, Gerardo Heiss, Lisa LaVange, Marston Youngblood. Central Laboratory: University of Minnesota, Minneapolis: Bharat Thyagarajan, John H. Eckfeldt. Central Reading Centers: Audiometry Center: University of Wisconsin: Karen J. Cruickshanks. ECG Reading Center: Wake Forest University: Elsayed Soliman. Neurocognitive Reading Center: University of Mississippi Medical Center: Hector Gonza´ les, Thomas Mosley. Nutrition Reading Center. University of Minnesota: John H. Himes. Pulmonary Reading Center: Columbia University: R. Graham Barr, Paul Enright. Sleep Center: Case Western Reserve University: Susan Redline.
Footnotes
Author Contributions: Drs Daviglus and Talavera had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Drs Daviglus and Talavera, as co–first authors, contributed equally to this article.
Study concept and design: Daviglus, Talavera, Gellman, Kaplan, LaVange, Penedo, Perreira, Schneiderman, Wassertheil-Smoller, Sorlie.
Acquisition of data: Daviglus, Talavera, Avilé s-Santa, Allison, Criqui, Gellman, Kaplan, Penedo, Perreira, Schneiderman, Wassertheil-Smoller, Stamler.
Analysis and interpretation of data: Daviglus, Talavera, Avilé s-Santa, Cai, Criqui, Giachello, Gouskova, Kaplan, LaVange, Penedo, Pirzada, Schneiderman, Wassertheil-Smoller, Sorlie, Stamler.
Drafting of the manuscript: Daviglus, Talavera, Cai, Kaplan, Pirzada.
Critical revision of the manuscript for important intellectual content: Daviglus, Talavera, Avilé s-Santa, Allison, Cai, Criqui, Gouskova, Kaplan, LaVange, Penedo, Perreira, Pirzada, Schneiderman, Wassertheil-Smoller, Sorlie, Stamler.
Statistical analysis: Cai, Gouskova, LaVange, Perreira.
Obtained funding: Daviglus, Talavera, Avilé s-Santa, Criqui, Kaplan, Penedo, Perreira, Schneiderman, Wassertheil-Smoller, Sorlie, Stamler.
Administrative, technical, or material support: Daviglus, Talavera, Cai, Gellman, Kaplan, Perreira, Pirzada, Schneiderman, Wassertheil-Smoller.
Study supervision: Daviglus, Talavera, Allison, Cai, Criqui, Gellman, Kaplan, Schneiderman, Stamler.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Cai reported having consulted for Outcomes Research Solutions. Dr Gellman reported receiving book royalties from Springer. No other disclosures were reported.
Online-Only Material: The eTables are available at http://www.jama.com.
Additional Contributions: We thank the staff and participants of HCHS/SOL for their important contributions. A complete list of staff and investigators was published in Ann Epidemiol. 2010;20:642–649 and is also available on the study website, http://www.cscc.unc.edu/hchs/.
REFERENCES
- 1.Ennis S, Rios-Vargas M, Albert N. Census Briefs: The Hispanic Population: 2010. [Accessed October 11, 2012];US Census Bureau. 2010 http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf.
- 2.Roger VL, Go AS, Lloyd-Jones DM, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics: 2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diez Roux AV, Detrano R, Jackson S, et al. Acculturation and socioeconomic position as predictors of coronary calcification in a multiethnic sample. Circulation. 2005;112(11):1557–1565. doi: 10.1161/CIRCULATIONAHA.104.530147. [DOI] [PubMed] [Google Scholar]
- 4.Kandula NR, Diez-Roux AV, Chan C, et al. Association of acculturation levels and prevalence of diabetes in the multi-ethnic study of atherosclerosis (MESA) Diabetes Care. 2008;31(8):1621–1628. doi: 10.2337/dc07-2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morales LS, Leng M, Escarce JJ. Risk of cardiovascular disease in first and second generation Mexican-Americans. J Immigr Minor Health. 2011;13(1):61–68. doi: 10.1007/s10903-009-9262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mainous AG, III, Majeed A, Koopman RJ, et al. Acculturation and diabetes among Hispanics: evidence from the 1999–2002 National Health and Nutrition Examination Survey. Public Health Rep. 2006;121(1):60–66. doi: 10.1177/003335490612100112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bethel JW, Schenker MB. Acculturation and smoking patterns among Hispanics: a review. Am J Prev Med. 2005;29(2):143–148. doi: 10.1016/j.amepre.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 8.Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97(7):1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitchell BD, Stern MP, Haffner SM, Hazuda HP, Patterson JK. Risk factors for cardiovascular mortality in Mexican Americans and non-Hispanic whites: San Antonio Heart Study. Am J Epidemiol. 1990;131(3):423–433. doi: 10.1093/oxfordjournals.aje.a115517. [DOI] [PubMed] [Google Scholar]
- 10.Sundquist J, Winkleby MA. Cardiovascular risk factors in Mexican American adults: a transcultural analysis of NHANES III, 1988–1994. Am J Public Health. 1999;89(5):723–730. doi: 10.2105/ajph.89.5.723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flegal KM, Ezzati TM, Harris MI, et al. Prevalence of diabetes in Mexican Americans, Cubans, and Puerto Ricans from the Hispanic Health and Nutrition Examination Survey, 1982–1984. Diabetes Care. 1991;14(7):628–638. doi: 10.2337/diacare.14.7.628. [DOI] [PubMed] [Google Scholar]
- 12.Crespo CJ, Loria CM, Burt VL. Hypertension and other cardiovascular disease risk factors among Mexican Americans, Cuban Americans, and Puerto Ricans from the Hispanic Health and Nutrition Examination Survey. Public Health Rep. 1996;111(suppl 2):7–10. [PMC free article] [PubMed] [Google Scholar]
- 13.Allison MA, Budoff MJ, Wong ND, Blumenthal RS, Schreiner PJ, Criqui MH The Multi-Ethnic Study of Atherosclerosis. Prevalence of and risk factors for subclinical cardiovascular disease in selected US Hispanic ethnic groups: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167(8):962–969. doi: 10.1093/aje/kwm402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Derby CA, Wildman RP, McGinn AP, et al. Cardiovascular risk factor variation within a Hispanic cohort: SWAN, the Study of Women’s Health Across the Nation. Ethn Dis. 2010;20(4):396–402. [PMC free article] [PubMed] [Google Scholar]
- 15.Lavange LM, Kalsbeek WD, Sorlie PD, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20(8):642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sorlie PD, Avilé s-Santa LM, Wassertheil-Smoller S, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010;20(8):629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 18.Liu K, Daviglus ML, Loria CM, et al. Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: the Coronary Artery Risk Development in (Young) Adults (CARDIA) study. Circulation. 2012;125(8):996–1004. doi: 10.1161/CIRCULATIONAHA.111.060681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 20.Chobanian AV, Bakris GL, Black HR, et al. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 21.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report [NIH Publication No. 98–4083] National Heart, Lung, and Blood Institute; [Accessed October 11, 2012]. http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf. [Google Scholar]
- 22.AmericanDiabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rewers M, Shetterly SM, Hoag S, Baxter J, Marshall J, Hamman RF. Is the risk of coronary heart disease lower in Hispanics than in non-Hispanic whites? the San Luis Valley Diabetes Study. Ethn Dis. 1993;3(1):44–54. [PubMed] [Google Scholar]
- 24.Swenson CJ, Trepka MJ, Rewers MJ, Scarbro S, Hiatt WR, Hamman RF. Cardiovascular disease mortality in Hispanics and non-Hispanic whites. Am J Epidemiol. 2002;156(10):919–928. doi: 10.1093/aje/kwf140. [DOI] [PubMed] [Google Scholar]
- 25.Hunt KJ, Resendez RG, Williams K, Haffner SM, Stern MP, Hazuda HP. All-cause and cardiovascular mortality among Mexican-American and non-Hispanic White older participants in the San Antonio Heart Study: evidence against the “Hispanic paradox”. Am J Epidemiol. 2003;158(11):1048–1057. doi: 10.1093/aje/kwg249. [DOI] [PubMed] [Google Scholar]
- 26.Stern MP, Rosenthal M, Haffner SM, Hazuda HP, Franco LJ. Sex difference in the effects of sociocultural status on diabetes and cardiovascular risk factors in Mexican Americans: the San Antonio Heart Study. Am J Epidemiol. 1984;120(6):834–851. doi: 10.1093/oxfordjournals.aje.a113956. [DOI] [PubMed] [Google Scholar]
- 27.Pabon-Nau LP, Cohen A, Meigs JB, Grant RW. Hypertension and diabetes prevalence among US Hispanics by country of origin: the National Health Interview Survey 2000–2005. J Gen Intern Med. 2010;25(8):847–852. doi: 10.1007/s11606-010-1335-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keenan NL, Rosendorf KA Centers for Disease Control and Prevention (CDC) Prevalence of hypertension and controlled hypertension: United States, 2005–2008. MMWR Surveill Summ. 2011;60(suppl):94–97. [PubMed] [Google Scholar]
- 29.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 30.Schargrodsky H, Herna´ndez-Herna´ndez R, Champagne BM, et al. CARMELA Study Investigators. CARMELA: assessment of cardiovascular risk in seven Latin American cities. Am J Med. 2008;121(1):58–65. doi: 10.1016/j.amjmed.2007.08.038. [DOI] [PubMed] [Google Scholar]
- 31.Yusuf S, Hawken S, Ôunpuu S, et al. INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 32.Lanas F, Avezum A, Bautista LE, et al. INTERHEART Investigators in Latin America. Risk factors for acute myocardial infarction in Latin America: the INTERHEART Latin American study. Circulation. 2007;115(9):1067–1074. doi: 10.1161/CIRCULATIONAHA.106.633552. [DOI] [PubMed] [Google Scholar]
- 33.Marmot MG, Syme SL. Acculturation and coronary heart disease in Japanese-Americans. Am J Epidemiol. 1976;104(3):225–247. doi: 10.1093/oxfordjournals.aje.a112296. [DOI] [PubMed] [Google Scholar]
- 34.Mooteri SN, Petersen F, Dagubati R, Pai RG. Duration of residence in the United States as a new risk factor for coronary artery disease (The Konkani Heart Study) Am J Cardiol. 2004;93(3):359–361. doi: 10.1016/j.amjcard.2003.09.044. [DOI] [PubMed] [Google Scholar]
- 35.Reed D, McGee D, Cohen J, Yano K, Syme SL, Feinleib M. Acculturation and coronary heart disease among Japanese men in Hawaii. Am J Epidemiol. 1982;115(6):894–905. doi: 10.1093/oxfordjournals.aje.a113377. [DOI] [PubMed] [Google Scholar]