Abstract
We report a case of lumbar intradural extramedullary lesion in an 11-year-old boy who presented with cauda equina syndrome and acute bladder disturbance. He underwent emergency surgical resection of the lesion, which was proved to be a lymphoma by histopathology and immunohistochemistry. He has improved neurologically and after 1 year, he is leading a normal life with near normal neurological functions. This is the second case of primary spinal intradural extramedullary lymphoma. This is the first such case in the pediatric age group and causing cauda equina syndrome. We describe the characteristics of such tumors along with pathogenesis and management.
Keywords: Cauda equina syndrome, chemoradiation, intradural extramedullary tumors, primary spinal lymphoma
INTRODUCTION
Spinal location of a lymphomatous lesion is commonly seen as a metastasis in patients known to have systemic lymphoma. Many authors have described the entity of primary spinal epidural lymphomas (PSEL), where there is no other evidence of lymphoma in the body other than a solitary lesion in the epidural space.[1] Here we have defined the term “primary spinal intradural extramedullary lymphoma” (PSIEL) and report the second case of PSIEL in the literature.
CASE REPORT
This 11-year-old boy presented with 3 days history of progressively increasing radicular pain over the sacrogluteal region bilaterally; left side more than the right side, along with lower limb weakness and sensory impairment in both lower limbs. He also developed urinary retention and was catheterized elsewhere 1 day prior to his presentation. On examination, his cranial nerves and upper limbs were normal. He had asymmetrical lower limb weakness with the left side worse than the right. His sensory examination also revealed an asymmetrical sensory impairment in the lower limbs with the upper limit being D12 dermatome. Both knee jerk and ankle jerk were absent with plantars not being elicitable. His muscle tone and bulk were normal. He did not have any neurocutaneous markers, palpable lymph nodes or spinal deformity. With this presentation and neurological examination, a diagnosis of spinal cord pathology with clinical localization to cauda equina was made. An emergency magnetic resonance imaging (MRI) of the lumbosacral spine with screening was performed, which showed a well-defined sausage shaped intradural lesion at L2, L3 level, without evidence of any other central nervous system (CNS) lymphomas. The lesion was iso-intense in T1- and T2-weighted images [Figure 1]. He underwent emergency L2, L3 laminectomy and excision of intradural extramedullary lesion. The lesion was removed piecemeal. Intra-operatively the lesion had some attachment to the anterior dura. Total removal was carried out, with coagulation of the anterior dura.
Figure 1.
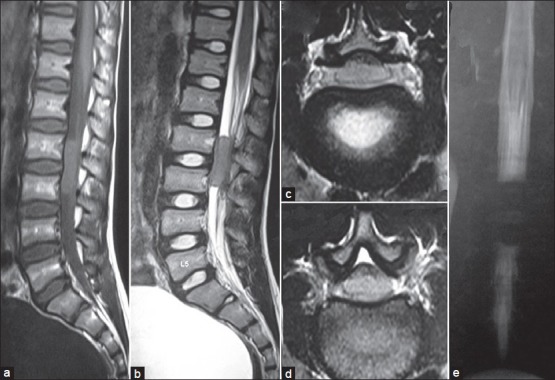
Pre-operative magnetic resonance imaging of the spine showing a sausage shaped intradural extramedullay lesion at L1 and L2 spinal levels. (a) T1-weighted sagittal, (b) T2-weighted sagittal, (c) T1-weighted axial, (d) T2-weighted axial, and (e) MR myelogram
Post-operatively he had total relief of pain and his motor power improved by one Medical Research Council grade and sensations were slowly improving. Histoplathological examination of the tumor revealed a dense infiltration of round cells admixed with cells with a large eosinophilic cytoplasm and vesicular nucleus with prominent nucleolus, which was consistent with non-Hodgkin's lymphoma [Figure 2]. The diagnosis was confirmed by immunohistochemistry showing CD20 positivity. Detailed investigation was carried out to stage the disease, which included complete hematological examination, including bone marrow aspiration and computerized tomography of the chest and abdomen. All the above investigations were normal.
Figure 2.
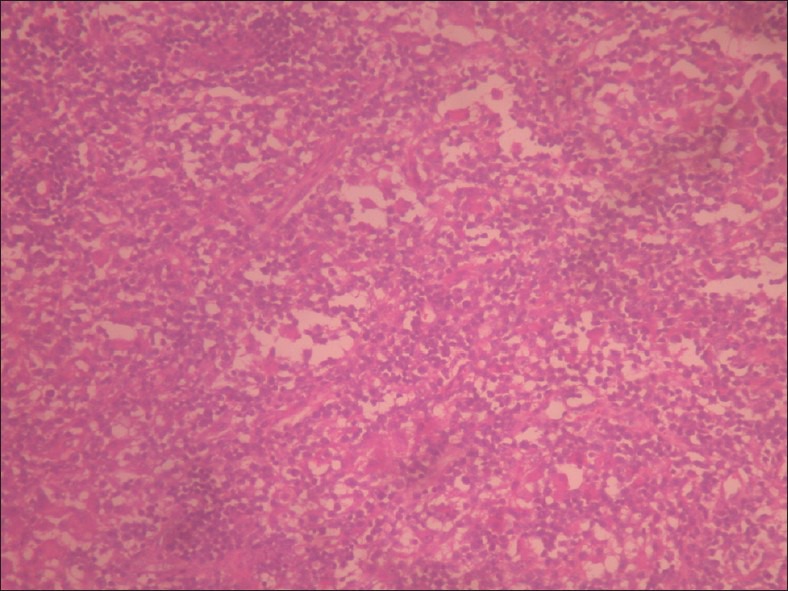
Histopathological examination of the tumor showing a dense infi ltration of round cells admixed with cells with large eosinophilic cytoplasm and vesicular nucleus with prominent nucleolus, consistent with non-hodgkin's lymphoma
On follow-up after 1 month he had received radiotherapy to the local area of 32 Gy in 20 fractions and was on chemotherapy; cyclophosphamide, hydroxydaunomycin, oncovin-vincristine, and prednisone regimen. Post-operative MRI showed total excision of the lesion [Figure 3]. At 1 year follow-up, he was having near normal power, normal sensations, and normal bladder control.
Figure 3.
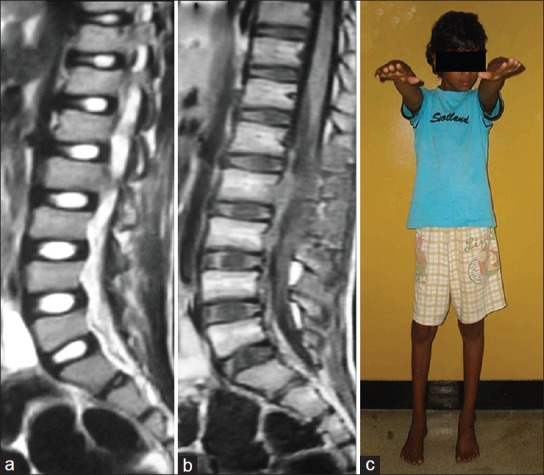
Post-operative magnetic resonance imaging showing total excision of the lesion. (a) T1-weighted sagittal and (b) T2-weighted sagittal, (c) clinical photograph at 1 year
DISCUSSION
Spinal location of a lymphomatous lesion is seen in various conditions. The most common occurrence is a metastatic spinal lymphoma in patients known to have systemic lymphoma. In the literature, there are many cases of primary spinal epidural lymphomas (PSEL) reported, where there is no other evidence of lymphoma in the body other than a solitary lesion in the epidural space.[1] The present case is an unique from these cases reported in literature that it has a purely intradural extramedullay origin. Tumors with a characteristic histopathological picture of a lymphoma that are seen purely in the spinal intradural extramedullay compartment, with an accompanying negative diagnostic work-up for lymphoma at other sites are termed PSIEL. First reported case of presumed PSIEL was by Heran et al. in 2006.[2] They operated on a cervical intradural extramedullary lesion which they thought initially as meningioma. After performing a laminectomy, the biopsy of the lesion was in favor of Hodgkins lymphoma; hence, the surgery was abandoned and the patient subsequently received chemotherapy. On further investigations, mediastinal, and paratracheal lymph nodes were seen. This finding is against the diagnosis being called PSIEL. Later in 2010, Yamashita et al. reported the first “true” PSIEL in a 64-year-old gentleman in the cervical spinal canal.[3] The present case is the second reported case of PSIEL in the literature.
The current patient presented classically like any other tumor in the cauda equina except for the sub-acute onset of symptoms and early bladder involvement. The tumor was intradural extramedullay in location. There was no radiological evidence of extradural infiltration or bony involvement. Keeping in mind the age of the patient and location, a pre-operative diagnosis of ependymoma was made. Other differentials for a tumor in this location include neurofibroma, meningioma, paraganglioma, and rarely hemangioblastoma or an astrocytoma of the filum terminale. There was no evidence of the systemic lymphoma as confirmed by whole body contrast computed tomography evaluation done post-operatively. A negative bone marrow evaluation ruled out involvement of lymphoreticular system. Earlier reports have suggested positron emission tomography to be highly sensitive in picking up lymphoma. The mean SUVmax (mean + standard deviation) for non-Hodgkins lymphoma is 3.2-43.0. Another useful adjunct in diagnosing lymphoma is serum ‘soluble interleukin-2 receptor’ (sIL-2R) levels.[3]
Intraoperatively the lesion was grey in color, firm in consistency, and relatively avascular. After laminectomy, on opening the dura the tumor was filling the dural sac and causing severe pressure on the cauda equina. There was an attachment to the dura anteriorly, which was coagulated. In the previous reported case by Yamashita et al., there was an attachment to a cervical spinal root and the adjoining dura as well. Total removal of the tumor and coagulation of the adherent dura may be necessary.[3]
Pathogenesis of this tumor is thought to be similar to that of primary CNS lymphomas, where a clone of malignant systemic lymphocytes having specific adhesion molecules might have given rise to the tumor. Marcotte et al. have described a case with intradural lymphoid hyperplasia in the cervical region as an immunoreaction to an unidentified antigen.[4] Borovich et al. have described the presence of lymphatic spaces within the dural lakes.[5] The above two reports suggest the possible presence of lymphatics within the dura. Lymphatic cell rests in these lymphatic spaces giving rise to lymphoma might be another probable hypothesis. Intra-operative evidence of the dural attachment might be due to its origin from these lymphatic spaces.[2] Histopathology of the tumor was confirmatory of non-Hodgkin's lymphoma. The diagnosis was also confirmed by immunohistochemistry showing CD20 positivity.
This being the second case of primary spinal intradural extramedullay lymphoma, there are no guidelines available in literature for optimal management. This entity can be presumed to have a similar pathogenesis and clinical profile like PSEL. Hence, the recommendation of management for PSEL can be adopted for managing PSIEL. Most authors prefer to administer chemotherapy in conjunction to radiotherapy (RT) and not alone.[1,6,7,8] Chemotherapy has been given before RT, after RT, sandwiched between, or administered concomitantly with RT. Various combinations of chemotherapeutic agents have been recommended, cyclophosphamide, vincristine, and prednisone being an integral part of all the combinations. Combined modality treatment, including RT and chemotherapy, is the most efficient treatment and has a better outcome in terms of systemic control, local control, and 5-year and long-term survival. A minimum of 36 Gy is recommended.
Chemotherapy in the management of systemic and primary CNS lymphomas is an established treatment modality. PSIEL being a rare entity, a pre-operative diagnosis is almost never thought off. This makes surgical intervention inevitable. If PSIEL is suspected pre-operatively, a limited laminectomy with biopsy and frozen section is to be carried out to diagnose lymphoma. If frozen section is in favor of lymphoma, surgery can be abandoned and chemoradiation would be more appropriate. If a patient presents with a cauda equina syndrome or acute bladder involvement, like in the current case, then early surgical resection should be preferred followed by chemoradiation.
CONCLUSIONS
Primary spinal intradural lymphomas form the rare differential diagnosis for spinal intradural extramedullary lesions and for cauda equina syndrome. Detailed evaluation is required to identify evidence of systemic or other CNS lymphomas. Early intervention either surgical or chemoradiation will be necessary to prevent the neurological damage.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Monnard V, Sun A, Epelbaum R, Poortmans P, Miller RC, Verschueren T, et al. Primary spinal epidural lymphoma: Patients’ profile, outcome, and prognostic factors: A multicenter Rare Cancer Network study. Int J Radiat Oncol Biol Phys. 2006;65:817–23. doi: 10.1016/j.ijrobp.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Heran NS, Yong RL, Heran MS, Yip S, Fairholm D. Primary intradural extraarachnoid hodgkin lymphoma of the cervical spine. Case report. J Neurosurg Spine. 2006;5:61–4. doi: 10.3171/spi.2006.5.1.61. [DOI] [PubMed] [Google Scholar]
- 3.Yamashita T, Sakaura H, Oshima K, Iwasaki M, Yoshikawa H. Solitary intradural extramedullary lymphoma of the cervical spine. J Neurosurg Spine. 2010;12:436–9. doi: 10.3171/2009.11.SPINE08735. [DOI] [PubMed] [Google Scholar]
- 4.Marcotte P, Montpetit V, Burns B, Dennecy JM. Intradural spinal lymphoid hyperplasia. J Neuropathol Exp Neurol. 1990;49:261. [Google Scholar]
- 5.Borovich B, Keret D, Ben-Arie J, Grushkiewicz I, Peyser E. Spinal intradural metastases of extraneural origin. Acta Neurochir (Wien) 1981;56:99–105. doi: 10.1007/BF01400977. [DOI] [PubMed] [Google Scholar]
- 6.Kahl C, Hirt C, Decker S, Gläser D, Rohde S, Jost K, et al. Multimodal therapy for localized spinal epidural follicular lymphoma. Onkologie. 2010;33:381–4. doi: 10.1159/000315769. [DOI] [PubMed] [Google Scholar]
- 7.Epelbaum R, Haim N, Ben-Shahar M, Ben-Arie Y, Feinsod M, Cohen Y. Non-Hodgkin's lymphoma presenting with spinal epidural involvement. Cancer. 1986;58:2120–4. doi: 10.1002/1097-0142(19861101)58:9<2120::aid-cncr2820580926>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 8.Cugati G, Singh M, Pande A, Ramamurthi R, Balasubramanyam M, Sethi SK, et al. J Craniovertebr Junction Spine. 2011;2:3–11. doi: 10.4103/0974-8237.85307. [DOI] [PMC free article] [PubMed] [Google Scholar]


