Abstract
Hangman's fractures, also known as traumatic spondylolisthesis of axis, can be managed either conservatively with immobilization or by surgery. Surgery is usually indicated in cases with instability or failure of conservative treatment. Different surgical approaches, both anterior and posterior, have been described for treating Hangman's fracture. We report two patients, one with type IIa and another with type III Hangman's fracture treated with C1-C3 lateral mass fusion and discuss the advantages and limitations of this technique when compared to other techniques for fusion in patients with Hangman's fracture.
Keywords: Axis fracture, C1-C3 fusion, cervical spine, Hangman's fracture, pars, pedicle, spinal fusion, traumatic spondylolisthesis of axis
INTRODUCTION
Hangman's fractures constitute 20% of acute axis fractures.[1] Options for the management of Hangman's fracture also known as traumatic spondylolisthesis of axis, include external immobilization or surgery.[2] Surgery is indicated for cases in which orthoses do not maintain stability or in whom the fracture has failed to fuse or for patients in whom immediate fixation is desired.[2] Surgical procedures used to treat Hangman's fracture include anterior, posterior, and anterior-posterior approaches.[3,4,5] The surgical approach should depend upon the translation, angulation, patient's anatomy and the experience and skill of the surgeon.[2] We report two patients with Hangman's fracture treated with C1-C3 lateral mass fusion and discuss the rational for this approach in properly selected patients.
CASE REPORTS
Case 1
A 36-year-old female who was the unrestrained passenger in a vehicle, which was involved in a collision and roll over and she lost consciousness briefly and on regaining consciousness, she complained of neck pain. She was transferred to a nearby medical facility where radiographs revealed Hangman's fracture and the patient was subsequently transferred to our department for surgical management. On admission, she was noted to have no neurological deficits, but had tenderness over the cervical spine. Her cranial computed tomography (CT) examination was normal. Her radiographs of the cervical spine revealed Levine and Edwards type IIa Hangman's fracture [Figure 1]. Magnetic resonance imaging (MRI) of the spine revealed evidence of hematoma extending from clivus to C4 anteriorly and from occiput to C7 posteriorly [Figure 2]. There was also evidence of anterior translation and mild angulation at C2-C3 suggestive of type IIa Levine and Edwards Hangman's fracture. In view of the unstable nature of the fracture and the presence of angulation, it was believed immobilization with external orthosis will not be effective and hence, surgical fixation was opted for. Pre-operative traction was not attempted as the patient was not willing for the same. CT studies of the spine showed that the fracture fragments were displaced [Figure 3] and hence, direct fixation of the pars fracture with pars screws as suggested by Bristol et al. and Dalbayrak et al. was not considered safe or feasible.[2,6] Hence, C1-C3 lateral mass fusion was planned. With the patient kept under skeletal traction in the prone position, proper alignment was achieved under fluoroscopic control and then the region from C1 to C3 was exposed. The C2 root and ganglion were sectioned on either side and the C1 lateral mass was exposed. The C3 lateral masses were exposed on either side or 3.5 mm × 28 mm polyaxial titanium screws were inserted into the C1 lateral masses on either side followed by insertion of 3.5 mm × 14 mm polyaxial screws into the lateral masses of C3. For insertion of C1 lateral mass screw, the entry point was the middle of the lateral mass with 10* medial angulation aiming for the anterior tubercle of atlas and for C 3 lateral mass screw, the entry point was 1mm medial to the center of the lateral mass with 30* lateral and 15* rostral angulation. The exposed posterior surfaces of C1, C2, and C3 were decorticated and autologous grafts obtained from posterior iliac crest was applied as onlay graft and the wound was closed in layers. Post-operative radiographs showed good alignment with proper placement of screws [Figure 4]. Post-operatively, when examined 3 months later, there was no change in the patient's clinical condition except for numbness in the occipital region due to sectioning of C2 root.
Figure 1.

Plain radiograph of the cervical spine in patient 1 revealing a Levine and Edwards type IIa Hangman's fracture
Figure 2.
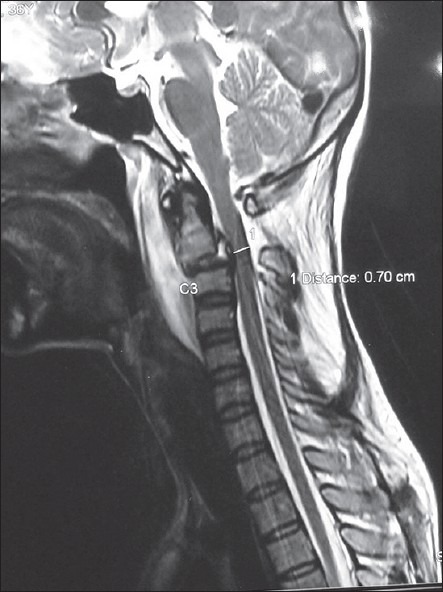
Sagittal T2-weighted magnetic resonance imaging sequences in patient 1 with type IIa Hangman's fracture showing hematoma extending from clivus to C4 along with anterior translation and angulation of C2 over C3
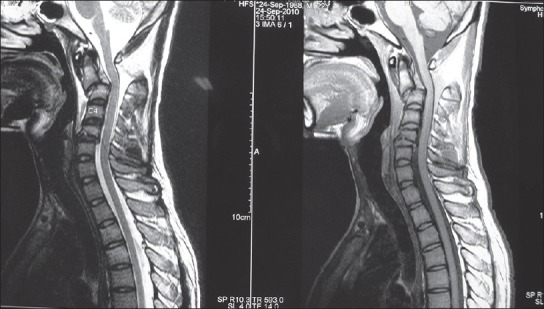
Figure 3.
Axial computed tomography of the spine at C2 level revealing the bilateral pars fractures with displacement of the fragments
Figure 4.

Post-operative radiograph of the cervical spine showing C1 lateral mass and C3 lateral mass screws with good reduction and alignment of the C2-C3
Case 2
A 22-year-old male was the unrestrained passenger in a vehicle involved in road traffic accident. Shortly, after the accident, he complained of severe neck pain. When examined in the hospital, he had no neurological deficits, but had severe pain and tenderness in the neck. His radiographs showed a type III Levine and Edwards Hangman's fracture [Figure 5]. His MRI of the spine showed hematoma extending from the clivus to C4 along with anterior translation and angulation of C2 over C3 along with disruption of the C2-C3 disc [Figure 6]. CT of the spine showed bilateral pars fracture of C2 with significant displacement [Figure 7]. In view of these findings, anterior approach with C2-C3 discectomy and plating was planned. With the patient under traction, the C2-C3 region was exposed through the anterolateral approach and discectomy and grafting of C2-C3 was carried out. However, attempt to plate C2 and C3 was not successful as the diameter of the available plate was greater than the diameter of the base of C2 body as was cautioned by Traynelis and Fontes.[7] Hence, grafting alone was carried out. However, post-operative radiographs on day 2 revealed dislodgment of the graft with recurrence of subluxation. Hence, patient was taken up for posterior C1-C3 lateral mass fusion. The same approach as mentioned for case 1 was carried out uneventfully [Figure 8]. Post-operative radiographs showed good alignment with appropriate position of the screws [Figure 9]. Three months later, patient had no neurological deficits, but had a small trophic ulcer in the occipital region owing to numbness in the area and wearing of Philadelphia collar.
Figure 5.

Plain radiograph of the cervical spine in patient 2 revealing a Levine and Edwards type III Hangman's fracture
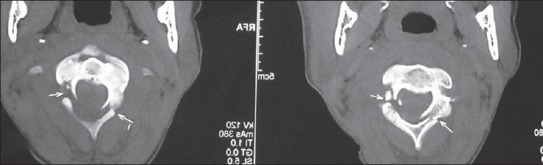
Figure 6.
Magnetic resonance imaging sagittal T2-weighted (left panel) and T1-weighted (right panel) of patient 2, showing signifi cant anterior translation, angulation of C2 over C3 along with disruption of C2-C3 disc space and hematoma extending from the clivus to C4 anteriorly
Figure 7.
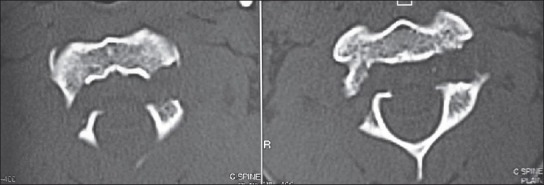
Computed tomography spine - axial slices - revealing bilateral pars fractures in patient 2
Figure 8.
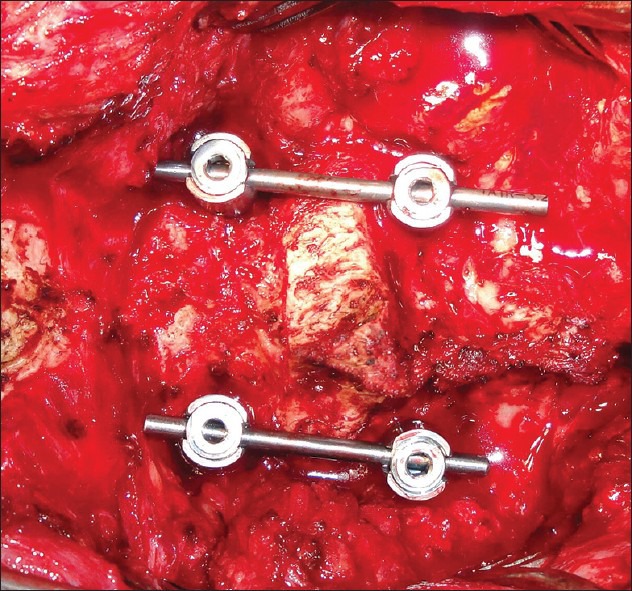
Intra-operative photograph showing the screw-rod construct at C1-C3 levels
Figure 9.

Post-operative radiograph showing the lateral mass screws in C1 and C3 with good restoration of cervical alignment
DISCUSSION
Hangman's fractures constitute 4% of all cervical fractures.[8] Among the different types of axis fractures, Hangman's fractures constitute 20%.[1] Among the different types of Hangman's fractures, type I constitutes 65%, type II 28%, and type III 7%.[9]
Role of conservative management in Hangman's fracture
Immobilization with external orthosis is the first line of treatment for most Hangman's fractures.[10] A recent systematic review of Hangman's fracture by Li et al. has shown that most Hangman's fractures can be treated by rigid external immobilization.[3] These authors recommended rigid external immobilization for Levine-Edwards type I and type II fractures but favored surgical intervention when there was evidence of instability as in type IIa and type III fractures. However, the reported failure rates of rigid orthosis eventually requiring surgical fusion varies from 9% to 32%.[8,9]
Surgical approaches for Hangman's fractures
In choosing a surgical procedure, the goals of surgery are to reduce the fracture, maintain alignment of the spine, confer stability, achieve fusion, preserve mobility, and protect the neural structures. It can be quite difficult to balance these factors equally when determining the most effective operation to perform.[11]
Surgical approaches to traumatic spondylolisthesis of axis include: (1) Anterior discectomy and fusion; (2) posterior approaches, which include (a) occipitocervical fusion, (b) C1-C3 fusion, and (c) direct screw fixation of the fractured pars. Each approach has advantages and limitations and the choice of approach depends upon the degree of translation, angulation, morphology of the fracture, patient's anatomy, and surgeon's experience and skill.[2]
Anterior discectomy and screw plate fixation is an effective, but not very popular technique the limitations of which include: Difficulty in exposing the C2-C3 region, difficulties associated with anterior screw placement in the axis as highlighted by Traynelis and Fontes,[7] and the elimination of C2-C3 rotation.[2] A high anterior approach also places at risk vital structures such as the facial and hypoglossal nerves, contents of the carotid sheath and the superior laryngeal nerve.[12] In our patient 2, our first choice was anterior cervical discectomy and fusion in view of the angulation, translation and disruption of the C2-C3 disc. However, as pointed out by Traynelis and Fontes, anterior fixation of the axis is associated with certain unique problems.[7] Placement of screws in the body of axis and contouring the plate are occasionally difficult[7] as we found out in our case 2.
Posterior approaches include: (1) Occipitocervical fusion, (2) direct fixation of the fracture with pars screw, and (3) C1-C3 lateral mass fusion.
Occipitocervical fusion eliminates occipitocervical movements as well as atlantoaxial rotation and hence should be used as a last resort or as a salvage procedure.
Direct screw fixation of C2 pars fixes the fracture without compromising movement.[2] However, as pointed out by Bristol et al., this technique cannot be applied routinely to all patients with Hangman's fractures.[2] Direct screw fixation of C2 pars is feasible only in patients where the fracture is posteriorly located and the screw can be placed safely without risking injury to the vertebral artery,[2] and is therefore not indicated for anteriorly placed pars fractures. Another disadvantage of direct pars screw fixation is the need for complete manual reduction of the fracture intraoperatively before placement of lag screws in the fractured pars.[2,12] Moreover, as pointed out by ElMiligui et al., the screw passes through the narrowest part of the vertebra, which is bounded medially by the spinal cord and laterally by the vertebral artery and the diameter of the screw is 3.5 mm and the space available for the screw varies between 5 mm and 7 mm.[12] The rate of vertebral artery injury varies between 11% and 66%.[13,14] As pointed out by Dalbayrak et al. and Verheggen and Jensen,[6,15] direct pars screw fixation is not ideal for type III Hangman's fracture with associated disruption of C2-C3 disc because as shown by Duggal et al., direct pars screw fixation is not effective in limiting flexion and extension if there is disc disruption.[16] In our patient 1, the fractured fragments were displaced and hence this patient was not considered for direct C2 pars screw fixation. In case 2, the fractures were more anteriorly located and there was considerable risk of vertebral artery injury by using this technique and hence was avoided. Moreover, as there was associated disc disruption in case 2, as suggested by Dalbayrak et al. and Verheggen and Jensen,[6,15] it was not considered ideal for direct pars screw fixation.
Fusion of lateral masses of C1 and C3 for Hangman's fractures has the following advantages: (1) Risk of vertebral artery injury is minimized, (2) risk of displacement of the fractured fragments into the spinal canal is eliminated, and (3) conventional lateral mass screws can be used unlike direct pars screw fixation technique, which requires the use of appropriate sized lag screws. However, the disadvantages include: Elimination of atlantoaxial rotation. To the best of the author's knowledge, this technique of C1-C3 lateral mass fixation for Hangman's fracture has been used only once before.[17] Horn et al. reported nine patients with C1-C3 lateral mass fixation one of whom underwent C1-C3 fixation for Hangman's fracture.[17] A recent biomechanical study by Brasiliense et al. has shown that fusion of C1 and C3 lateral masses with C2 sparing provides sufficient stability.[18] The efficacy of posterior C1-C3 fusion technique was confirmed by a recent biomechanical study by Chittiboina et al. who showed that both anterior C2-C3 discectomy and fusion as well as posterior C1-C3 fusion were equally effective biomechanically.[19] Our technique of C1-C3 fusion is based on the cervicocranial concept of Hangman's fracture initially elucidated by Effendi and later elaborated by Chittiboina et al.[9,19] In this concept, Hangman's fracture consists of two parts, the ventrocranial part consisting of the atlas, dens and the body of axis and the dorsocaudal part consisting of the posterior elements of axis and C3.[19] Accordingly, fusion of C1 and C3 lateral masses effectively fixes the ventrocranial and the dorsocaudal components. Moreover, as suggested by Guiot and Fessler, type II and type III fractures with disruption of the C2-C3 disc space and posterior longitudinal ligament are best treated by posterior stabilization as these injuries are more likely to fail in flexion.[11] This technique is easy to use and avoids the above mentioned risks of anterior discectomy and plating as well as the risks associated with direct pars screws.
CONCLUSIONS
C1 and C3 lateral mass fusion using polyaxial screw-rod system is an effective and biomechanically sound way of treating properly selected cases of type IIa and type III Hangman's fracture.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hadley MN, Dickman CA, Browner CM, Sonntag VK. Acute axis fractures: A review of 229 cases. J Neurosurg. 1989;71:642–7. doi: 10.3171/jns.1989.71.5.0642. [DOI] [PubMed] [Google Scholar]
- 2.Bristol R, Henn JS, Dickman CA. Pars screw fixation of a Hangman's fracture: Technical case report. Neurosurgery. 2005;56:E204. doi: 10.1227/01.neu.0000144172.84111.a6. [DOI] [PubMed] [Google Scholar]
- 3.Li XF, Dai LY, Lu H, Chen XD. A systematic review of the management of Hangman's fractures. Eur Spine J. 2006;15:257–69. doi: 10.1007/s00586-005-0918-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goel A, Laheri VK. Plate and screw fixation for atlanto-axial dislocation. (Technical report) Acta Neurochir (Wien) 1994;129:47–53. doi: 10.1007/BF01400872. [DOI] [PubMed] [Google Scholar]
- 5.Goel A, Desai K, Muzumdar D. Atlantoaxial fixation using plate and screw method: A report of 160 treated patients. Neurosurgery. 2002;51:1351–1357. [PubMed] [Google Scholar]
- 6.Dalbayrak S, Yilmaz M, Firidin M, Naderi S. Traumatic spondylolisthesis of the axis treated with direct C2 pars screw. Turk Neurosurg. 2009;19:163–7. [PubMed] [Google Scholar]
- 7.Traynelis VC, Fontes RB. Anterior fixation of the axis. Neurosurgery. 2010;67:ons229–36. doi: 10.1227/01.NEU.0000381666.38707.65. [DOI] [PubMed] [Google Scholar]
- 8.Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, Sonntag VK. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine (Phila Pa 1976) 1997;22:1843–52. doi: 10.1097/00007632-199708150-00009. [DOI] [PubMed] [Google Scholar]
- 9.Effendi B, Roy D, Cornish B, Dussault RG, Laurin CA. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Joint Surg Br. 1981;63-B:319–27. doi: 10.1302/0301-620X.63B3.7263741. [DOI] [PubMed] [Google Scholar]
- 10.Pryputniewicz DM, Hadley MN. Axis fractures. Neurosurgery. 2010;66:68–82. doi: 10.1227/01.NEU.0000366118.21964.A8. [DOI] [PubMed] [Google Scholar]
- 11.Guiot B, Fessler RG. Complex atlantoaxial fractures. J Neurosurg. 1999;91:139–43. doi: 10.3171/spi.1999.91.2.0139. [DOI] [PubMed] [Google Scholar]
- 12.El Miligui Y, Koptan W, Emran I. Transpedicular screw fixation for type II Hangman's fracture: A motion preserving procedure. Eur Spine J. 2010;19:1299–305. doi: 10.1007/s00586-010-1401-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ludwig SC, Kramer DL, Vaccaro AR, Albert TJ. Transpedicle screw fixation of the cervical spine. Clin Orthop Relat Res. 1999;359:77–88. doi: 10.1097/00003086-199902000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Ludwig SC, Kowalski JM, Edwards CC, 2nd, Heller JG. Cervical pedicle screws: Comparative accuracy of two insertion techniques. Spine (Phila Pa 1976) 2000;25:2675–81. doi: 10.1097/00007632-200010150-00022. [DOI] [PubMed] [Google Scholar]
- 15.Verheggen R, Jansen J. Hangman's fracture: Arguments in favor of surgical therapy for type II and III according to Edwards and Levine. Surg Neurol. 1998;49:253–61. doi: 10.1016/s0090-3019(97)00300-5. [DOI] [PubMed] [Google Scholar]
- 16.Duggal N, Chamberlain RH, Perez-Garza LE, Espinoza-Larios A, Sonntag VK, Crawford NR. Hangman's fracture: A biomechanical comparison of stabilization techniques. Spine (Phila Pa 1976) 2007;32:182–7. doi: 10.1097/01.brs.0000251917.83529.0b. [DOI] [PubMed] [Google Scholar]
- 17.Horn EM, Hott JS, Porter RW, Theodore N, Papadopoulos SM, Sonntag VK. Atlantoaxial stabilization with the use of C1-3 lateral mass screw fixation. Technical note. J Neurosurg Spine. 2006;5:172–7. doi: 10.3171/spi.2006.5.2.172. [DOI] [PubMed] [Google Scholar]
- 18.Brasiliense LB, Lazaro BC, Reyes PM, Fox D, Sonntag VK, Crawford NR. Stabilization of the atlantoaxial joint with C1-C3 lateral mass screw constructs: Biomechanical comparison with standard technique. Neurosurgery. 2010;67:422–8. doi: 10.1227/NEU.0b013e3181fb414c. [DOI] [PubMed] [Google Scholar]
- 19.Chittiboina P, Wylen E, Ogden A, Mukherjee DP, Vannemreddy P, Nanda A. Traumatic spondylolisthesis of the axis: A biomechanical comparison of clinically relevant anterior and posterior fusion techniques. J Neurosurg Spine. 2009;11:379–87. doi: 10.3171/2009.4.SPINE08516. [DOI] [PubMed] [Google Scholar]


