Abstract
Allergic bronchopulmonary aspergillosis (ABPA), as a complication of asthma, is rare in children. The persistent and poorly-controlled asthma leading to cor pulmonale is not uncommon in adults but rarely described in the pediatric age group. Here, we report a case of asthma and ABPA complicated by pulmonary thrombo-embolism and cor pulmonale. To the best of our knowledge, such association has never been reported in the pediatric age group.
Keywords: Allergic bronchopulmonary aspergillosis, bronchial asthma, cor pulmonale, pulmonary thrombo-embolism
Introduction
ABPA is a rare complication of asthma in children; only a few case reports and small series have been published.[1] Severe asthma is known to cause cor pulmonale in adults,[2] but rarely described in pediatric age group.[3] Further, pulmonary thrombo-embolism (PTE) in children with asthma and cor pulmonale has been described only at autopsy.[3] We describe a child who developed ABPA with pulmonary thrombo-embolism and cor pulmonale as a complication of poorly-controlled asthma.
Case Report
A 9-year-old boy presented with bluish discoloration of the nails and lips since last one year andanasarca (generalized swelling), worsening cough, respiratory distress, and periumbilical pain abdomen since 20 days previously. He had past history suggestive of asthma (recurrent episodes of cough and respiratory distress since the first year of life), for which he had received irregular treatment. He was not receiving any regular inhaled steroids. He had no significant febrile illnesses and loose stools in the past. His sibling had bronchial asthma. There was no history of tuberculosis or sibling death in family. On admission, patient found to have central cyanosis, tachycardia, marked respiratory distress with normal blood pressure. The child had anasarca, grade III clubbing, and raised jugular venous pressure. His weight and height both were below the third percentile. Examination revealed a hyper-resonant chest with generalized crepts and rhonchi. The second heart sound was loud, but no murmur was detected. He had tender hepatomegaly.
Investigations showed hemoglobin of 150 g/L, total leukocyte count 12.8 × 109/L with neutrophils 80%, lymphocytes 18%, monocytes 1%, and eosinophils 1%. Arterial blood gas analysis on 100% oxygen showed pH of 7.36, pCO2 59.5 mm of Hg, pO2 116 mm of Hg, HCO3 32.6 mmol/L, base excess 5.2 and oxygen saturation 98.3%, suggesting chronic respiratory acidosis. Tubercular workup was negative. Sweat chloride level (pilocarpine iontophoresis method) was 42 meq/L (borderline). HIV was non-reactive. Chest x-ray revealed cardiomegaly and bilateral lung infiltrates. Electrocardiography revealed right axis deviation and p-pulmonale. HRCT chest showed central bronchiectasis [Figure 1a], minimal right pleural and pericardial effusion, and gross cardiomegaly. Chest angiography revealed dilated main pulmonary artery and filling defect in right branch of pulmonary artery [Figure 1b]. Echocardiography finding were: Dilated right-sided heart, right ventricular dysfunction, severe pulmonary artery hypertension, and right atrial clot. Lung ventilation-perfusion scan was suggestive of pulmonary thrombo-embolism. Serum IgE levels were 1100 IU/ml (normal 50-100 IU/ml). Immediate skin hypersensitivity to Aspergillus fumigatus was positive. Serum precipitants against aspergillus and candida were negative. Coagulogram revealedPprothrombin time index of 82%, APTT 33 seconds, INR 1.2 and presence of fibrin degradation products.
Figure 1.
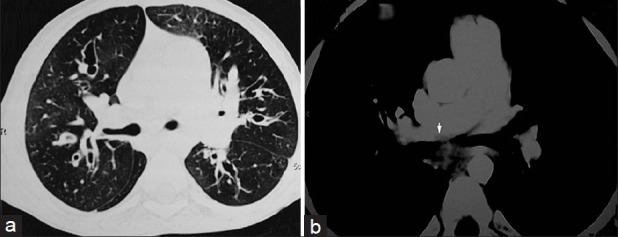
(a) HRCT chest showing central Bronchiectasis; (b) CT angiography showing thrombus in right pulmonary artery (arrow head)
The patient was managed with salbutamol (0.15 mg/kg/dose) and ipratropium bromide (0.5 mg/dose) nebulization and intravenous hydrocortisone (10 mg/kg stat followed by 2 mg/kg every 6 hourly) for exacerbation of asthma. For congestive heart failure, digoxin (3 μg/kg/day) and furosamide (2 mg/kg/day) was given. He received injection ceftriaxone (100 mg/kg/day) for 14 days. Low molecular weight heparin (1.0 mg/kg 12 hourly for 5 days) followed by warfarin (0.1 mg/kg/day) was administered for thrombo-embolism after chest angiography. He improved and was discharged on request on warfarin, home oxygen therapy, oral steroids (prednisolone 2 mg/kg/day), and inhaled steroids (budesonide 400 μg/day) after three weeks of admission. He didn’t return for follow-up, and on enquiry, we came to know that he expired after few days of discharge.
Discussion
In the pediatric age group, ABPA in asthma is rare. The criteria for diagnosis of ABPA were fulfilled by standard criteria (asthma, central bronchiectesis, raised serum IgE, immediate cutaneous hypersenstivity to A. fumigatus), and by severity, the ABPA was of the fifth stage (cyanosis, severe dyspnea, raised IgE, central bronchiectesis).[4]
Further work-up of the case revealed features of cor pulmonale and pulmonary thrombo-embolism (PTE). In adults, cor pulmonale is well-known in poorly-controlled asthma. In a study from Ethopia, 36% cases of cor pulmonale in adults had asthma.[2] Its rarity in developed countries might be because of better asthma management as compared to resource-poor countries. In children, we could find only three cases, reported by Griffin et al., of cor pulmonale in poorly-controlled asthma.[3] Better management of asthma in children with time might have decreased cases of cor pulmonale in asthma. Although cor pulmonale is rare in children with asthma, the tissue Doppler echocardiography has shown subclinical right ventricular dysfunction positively correlating with the severity of asthma in children.[5] Cor pulmonale as a presenting feature of ABPA without asthma had also been reported in adult.[6] As both poorly-controlled asthma and ABPA have been associated with cor pulmonale independently, the presence of both in our case may have resulted in cor pulmonale at an early age.
To the best of our knowledge, PTE had never been reported ante-mortem in asthmatic children with ABPA and cor pulmonale. Griffin et al. reported PTE at autopsy in a child with asthma and cor pulmonale.[3] Possible underlying mechanism of PTE in such cases may be chamber hypokinesia (due to cor pulmonale) and polycythemia (due to chronic hypoxia). The hemoglobin was 15 gm% in our case, and echo showed poor right ventricular function. Although the diagnosis of asthma is not in doubt (recurrent cough and respiratory distress, history of asthma in sibling and good response to bronchodilators and steroids), we could not rule out cystic fibrosis completely (second sweat chloride, delta 508 mutation, and cystic fibrosis transmembrane conductance regulator (CFTR) genes could not be performed). Both cystic fibrosis and asthma may co-exist in same patient.[7] Such combination of complications rarely occurs, even if both cystic fibrosis and asthma co-exist.
To conclude, in a poorly-controlled asthma, ABPA should be excluded even in children and if present, should be treated aggressively to prevent complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Gaur SN, Khan ZU, Kumar R. Youngest patient of ABPA in Indian Subcontinent: A case report. Indian J of Allergy Asthma Immunol. 2006;20:37–40. [Google Scholar]
- 2.Aderaye G. Causes and clinical characteristics of chronic cor-pulmonale in Ethiopia. East Afr Med J. 2004;81:202–6. doi: 10.4314/eamj.v81i4.9156. [DOI] [PubMed] [Google Scholar]
- 3.Griffin JT, Kass I, Hoffman MS. Cor pulmonale associated with symptoms and signs of asthma in children. Pediatrics. 1959;24:54–64. [PubMed] [Google Scholar]
- 4.Tillie-Leblond I, Tonnel AB. Allergic bronchopulmonary Aspergillosis. Allergy. 2005;60:1004–13. doi: 10.1111/j.1398-9995.2005.00887.x. [DOI] [PubMed] [Google Scholar]
- 5.Shedeed SA. Right ventricular function in children with bronchial asthma: A tissue Doppler echocardiographic study. Pediatr Cardiol. 2010;31:1008–15. doi: 10.1007/s00246-010-9753-2. [DOI] [PubMed] [Google Scholar]
- 6.Agarwal R, Singh N, Gupta D. Pulmonary hypertension as a presenting manifestation of allergic bronchopulmonary aspergillosis. Indian J Chest Dis Allied Sci. 2009;51:37–40. [PubMed] [Google Scholar]
- 7.Antunes J, Fernandes A, Miguel Borrego L, Leiria-Pinto P, Cavaco J. Cystic fibrosis, atopy, asthma and ABPA. Allergol Immunopathol (Madr) 2010;38:278–84. doi: 10.1016/j.aller.2010.06.002. [DOI] [PubMed] [Google Scholar]


