Abstract
Context
Clinical experience and factor analytic studies suggest that some psychiatric disorders may be more closely related to one another, as indicated by the frequency of their co-occurrence, which may have etiologic and treatment implications.
Objective
To construct a virtual space of common psychiatric disorders, spanned by factors reflecting major psychopathologic dimensions, and locate psychiatric disorders in that space, as well as to examine whether the location of disorders at baseline predicts the prevalence and incidence of disorders at 3-year follow-up.
Design, Setting, and Patients
A total of 34 653 individuals participated in waves 1 and 2 of the National Epidemiologic Survey on Alcohol and Related Conditions.
Main Outcome Measures
The distance between disorders at wave 1, calculated using the loadings of the factors spanning the space of disorders as coordinates. This distance was correlated with the adjusted odds ratios for age, sex, and race/ethnicity of the prevalence and incidence of Axis I disorders in wave 2, with the aim of determining whether smaller distances between disorders at wave 1 predicts higher disorder prevalence and incidence at wave 2.
Results
A model with 3 correlated factors provided an excellent fit (Comparative Fit Index = 0.99, Tucker-Lewis Index=0.98, root mean square error of approximation=0.008) for the structure of common psychiatric disorders and was used to span the space of disorders. Distances ranged from 0.070 (between drug abuse and dysthymia) to 1.032 (between drug abuse and avoidant personality disorder). The correlation of distance between disorders in wave 1 with adjusted odds ratios of prevalence in wave 2 was −0.56. The correlation of distance in wave 1 with adjusted odds ratios of incidence in wave 2 was −0.57.
Conclusions
Mapping psychiatric disorders can be used to quantify the distances among disorders. Proximity in turn can be used to predict prospectively the incidence and prevalence of Axis I disorders.
Preparations for DSM-5 bring to the fore underlying interrelationships among psychiatric disorders.1–4 Examination of these interrelationships should ideally inform the structure of the diagnostic classification system and guide research strategies and treatment approaches for each disorder.5,6 Disorders deemed to be more closely related to one another may share etiologic factors, clinical course, or treatment response.1,3,7,8
Several studies have used latent variable techniques to investigate relationships among psychiatric disorders. In a seminal study, Krueger8 used 10 psychiatric diagnoses available in the National Comorbidity Survey to identify 2 correlated factors, one corresponding to externalizing disorders and the other to internalizing disorders. The latter could further be decomposed into 2 lower-order factors called anxious-misery or distress and fear. Other studies have confirmed this model, with small variations (such as whether the internalizing factor can be decomposed), and extended it to document its structural stability over time9,10 and cross-cultural validity in Western and non-Western countries.11 Indeed, the underlying structure of genetic risk for these disorders closely resembles the observed, phenotypic structure of their co-occurrence patterns.12 Using cross-sectional data from the World Health Organization World Mental Health Survey Initiative, Kessler and colleagues13 showed that 2 factors (one representing internalizing and the other externalizing disorders) identified through exploratory factor analyses accounted for most of the comorbidity among 18 psychiatric disorders. Moreover, their temporal sequencing could be parsimoniously modeled as a function of those 2 factors. More recently, using data from a large outpatient clinic, Kotov et al14 confirmed the existence of the internalizing, externalizing, and thought disorder dimensions, and they suggested the existence of somatoform and antagonism dimensions. Taken together, these findings suggest that there are a limited number of common causal pathways for the common disorders. An implicit assumption of research in this area, which is reflected in the structure of psychiatric classifications15,16 and reflects clinicians’ experience, is that some disorders are more similar to one another than others; therefore, they can be considered more closely related regarding their clinical manifestations, likelihood of co-occurrence, etiology, or treatment response. For example, major depressive disorder (MDD) might be considered closer to dysthymia or generalized anxiety disorder (GAD) than to substance use disorders (SUDs), based on the tendencies for these disorders and their symptoms to co-occur and respond to similar treatment strategies.17,18
We sought to build on prior work by developing a formal measure of similarity among common disorders. One means of operationalizing the similarity of disorders to one another is to conceive of them as existing along 1 or more dimensions in space with values (represented as coordinates) on each dimension corresponding to the role each dimension plays in the occurrence of the disorder. Comparing the location of disorders to one another along these dimensions then provides a formal measure of their proximity.19,20 We sought to examine the proximity among disorders using data from a large nationally representative sample of US adults who were followed up 3 years later and assessed for a broad range of Axis I and Axis II disorders. Based on the prior literature, we expected that disorders included within the same DSM chapters (eg, mood disorders) would tend to be closer to each other than to disorders from other chapters.
The pattern of disorder development over time provides a means of evaluating the validity of the disorder map. For example, if GAD was closer to MDD than to SUDs at baseline, we would expect that the correlation between having GAD at baseline and MDD at follow-up would be higher than the correlation between GAD and SUDs at follow-up. After assigning each disorder to a position on the dimensions, we tested the validity of these positions by evaluating correlations with prevalent and incident disorders at follow-up. The results provide an empirical map of common mental disorders that may help guide etiologic research and clinically focus the differential diagnosis assessment on neighboring disorders.
METHODS
SAMPLE
The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC)21,22 was the source of data. At wave 1, NESARC targeted the civilian noninstitutionalized population 18 years and older residing in households and group quarters. Black and Hispanic individuals, as well as adults aged 18 to 24 years, were oversampled, with data adjusted for over-sampling and household-level and person-level nonresponse. Interviews were conducted with 43 093 participants by experienced lay interviewers with extensive training and supervision.22,23 All procedures, including informed consent, received full human subjects review and approval from the US Census Bureau and US Office of Management and Budget. The wave 2 interview was conducted approximately 3 years later (mean interval, 36.6 months). Excluding ineligible respondents (eg, deceased), the wave 2 response rate was 86.7% (n=34 653).22 Wave 2 NESARC weights include a component that adjusts for nonresponse, demographic factors, and psychiatric diagnoses to ensure that the wave 2 sample approximated the target population, that is, the original sample minus attrition between the 2 waves.22
All diagnoses were made according to DSM-IV criteria using the Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM IV waves 1 and 2 version.24 Axis I diagnoses included SUDs (alcohol abuse and dependence, drug abuse and dependence, and nicotine dependence), mood disorders (MDD, dysthymia, and bipolar disorder), and anxiety disorders (panic disorder, social anxiety disorder, specific phobia, and GAD). Personality disorders were assessed on a lifetime basis, required long-term patterns of social and occupational impairment, and excluded substance-induced cases.25 In wave 1, DSM-IV avoidant, dependent, obsessive-compulsive, paranoid, schizoid, histrionic, and antisocial personality disorders were assessed and included in this study. As documented by previous national and international studies, the test-retest reliability of the Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM IV version measures of DSM-IV diagnoses is good for MDD (κ=0.65–0.73) and good to excellent for SUDs (κ>0.74). Reliability is fair to good for other mood and anxiety disorders (κ=0.40–0.60) and personality disorders (κ=0.40–0.67).24,26–28 In the current study, we used 12-month Axis I disorders and lifetime Axis II disorders for our wave 1 analyses. We used incidence between wave 1 and wave 2, as well as 12-month wave 2 disorders, for our analyses of wave 2 data.
STATISTICAL ANALYSES
Identification of Dimensions
Entering all Axis I and Axis II disorders included in wave 1 of the NESARC as indicators, we used exploratory factor analysis (EFA) to identify the potential latent factors (ie, dimensions). Exploratory factor analysis was chosen over confirmatory factor analyses (CFA) to allow for cross-loadings. Factor selection was guided by several considerations including the scree test, fit indices, parallel analyses, and interpretability. Each factor was subsequently interpreted as a latent dimension, which could be represented spatially by an axis. Those axes spanned a vectorial space that was subsequently used to calculate the distance between each disorder and each axis, as well as between all pairs of disorders.
The default estimator for the analysis was mean and variance-adjusted weighted least squares, a robust estimator that does not assume normally distributed variables and provides the best option for modeling categorical data.29 The fit indices used for model evaluation were the Comparative Fit Index (CFI), the Tucker-Lewis Index (TLI), the root mean square error of approximation (RMSEA), and the number of free parameters in the model. Values of CFI and TLI greater than 0.95 and values of RMSEA less than 0.06 are commonly used guidelines for inferring reasonably good model fit.30 A number of options are available for rotating the factor structure extracted in an EFA.20 We used the oblique geomin rotation, which is the recommended approach in Mplus (www.statmodel.com). All analyses were conducted using Mplus, which uses a sandwich estimator to correct standard errors for the nonindependence of the data resulting from the complex design of the NESARC.29
Coordinates of the Disorders
In factor analysis, the loadings are the regression coefficients of the indicators (disorders) on the latent variables.31 They estimate the amount of change on the latent response variables underlying the binary indicators given a unit change on the factor. Higher factor loadings indicate that a particular indicator (ie, disorder) shares larger amounts of variance with the common factor (ie, dimension) that is being defined by the set of indicators included in the model. Thus, the loadings of the disorders on the factors can be used to create a system of coordinates that locates each disorder in the space spanned by the factors. High positive values of the coordinates indicate strong association of a disorder with that dimension and that the dimension is an important component in the occurrence of the disorder. Low values on a dimension would indicate that the dimension plays a smaller role in the disorder’s occurrence, whereas negative values indicate an inverse association with the disorder.
Distance Between Disorders in Wave 1 and Prevalence and Incidence of Axis I Disorders in Wave 2
To estimate the proximity of 2 disorders, we calculated the Euclidian distance between them. The Euclidean distance between 2 points in a space (or hyperplane) is the square root of the sum of squares of its coordinates, applying a generalization for higher dimensional spaces of the well-known Pythagorean theorem19: distance=||a−b||, where a and b are vectors whose elements are the loadings of the disorders on the factors.
To assess the predictive validity of this measure, we first estimated, the adjusted odds ratios (AORs) for age, sex, and race/ethnicity of the 12-month prevalence and incidence of Axis I disorders at wave 2. Pearson correlation coefficient was then used to assess the strength of association between distance among disorders in wave 1 and the AORs of the 12-month prevalence and incidence of disorders at wave 2. Because smaller distances between pairs of disorders at wave 1 would indicate a higher degree of similarity between those 2 disorders, we hypothesized that the closer 2 disorders were at wave 1, the better they would predict the incidence and prevalence of Axis I disorders at wave 2 as measured by the AORs.
Complementary Analyses
To assess the predictive value of alternative approaches, we conducted a CFA for the 3-factor and 4-factor models in which disorders were constrained to load exclusively on the factor on which they had the largest loading in the EFA, as well as a bifactor model with a general psychopathology factor loading on all disorders in addition to disorder-specific factors.32 We then calculated the correlation between the distances derived from those models and the prevalence and incidence of Axis I disorders at wave 2. We also calculated the correlation between the prevalence and incidence of Axis I disorders in wave 2 and the inverse of the odds ratios (ORs) between pairs of disorders in wave 1. The inverse of the ORs was used rather than the OR per se to ensure that the correlation would be negative, thus comparable to our correlation with distance measures (because greater ORs indicate stronger association, whereas larger distances indicate weaker association in the multidimensional space).
RESULTS
IDENTIFICATION OF DIMENSIONS
The eigenvalues for the first 5 factors were 7.97, 2.32, 1.87, 1.58, and 1.03. The 95th percentiles of the eigenvalues for the 5 factors derived from the parallel analyses were 1.04, 1.04, 1.03, 1.03, and 1.02, which supported the extraction of up to 5 factors. Fit indices indicated that a 1-factor model had poor fit (CFI=0.91, TLI=0.89, RMSEA=0.019). A model with 2 factors provided a reasonably good fit (CFI = 0.95, TLI = 0.94, RMSEA = 0.014), whereas models with 3 (CFI=0.99, TLI=0.98, RMSEA=0.008), 4 (CFI=0.99, TLI = 0.99, RMSEA = 0.006), and 5 (CFI = 1.00, TLI=0.99, RMSEA=0.005) factors provided excellent and comparable fit. In the 2-factor model, factor 1 had the highest loadings on SUDs, pathological gambling, and antisocial personality disorders, whereas factor 2 had higher loadings on mood and anxiety disorders and the other 6 personality disorders assessed in wave 1. The correlation between the 2 factors was 0.44 (Table 1).
Table 1.
Factor Analyses of Axis I and Axis II Disorders in Wave 1 of the National Epidemiologic Survey on Alcohol and Related Conditions
| Index
|
Model 2
|
Model 3
|
Model 4
|
Model 5
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CFI | 0.954 | 0.986 | 0.993 | 0.997 | ||||||||||
| TLI | 0.943 | 0.980 | 0.989 | 0.994 | ||||||||||
| RMSEA | 0.014 | 0.008 | 0.006 | 0.005 | ||||||||||
| Disorder | Factor 1 | Factor 2 | Factor 1 | Factor 2 | Factor 3 | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 |
| AA | 0.41 | −0.15 | 0.48 | −0.22 | −0.04 | 0.45 | −0.03 | −0.09 | −0.09 | 0.39 | −0.02 | 0.03 | 0.03 | −0.25 |
| AD | 0.72 | 0.04 | 0.80 | −0.11 | 0.08 | 0.75 | 0.02 | 0.01 | 0.02 | 0.78 | 0.02 | −0.03 | −0.02 | 0.09 |
| DA | 0.74 | −0.02 | 0.81 | −0.16 | 0.03 | 0.77 | −0.01 | −0.01 | −0.03 | 0.77 | −0.01 | 0.00 | −0.07 | 0.04 |
| DD | 0.68 | 0.27 | 0.77 | 0.02 | 0.18 | 0.73 | 0.13 | 0.07 | 0.10 | 0.75 | 0.08 | 0.02 | 0.03 | 0.17 |
| ND | 0.48 | 0.21 | 0.59 | 0.02 | 0.13 | 0.57 | 0.04 | 0.16 | 0.00 | 0.54 | 0.06 | 0.05 | 0.20 | −0.08 |
| MDD | −0.29 | 0.74 | 0.04 | 0.02 | 0.78 | 0.03 | 0.75 | 0.13 | −0.05 | 0.01 | 0.72 | 0.00 | 0.24 | −0.10 |
| BD | 0.21 | 0.62 | 0.25 | 0.44 | 0.25 | 0.19 | 0.48 | 0.04 | 0.35 | 0.16 | 0.46 | 0.36 | 0.07 | 0.02 |
| Dysthymia | −0.47 | 0.89 | −0.01 | −0.01 | 0.89 | −0.06 | 0.97 | −0.08 | 0.04 | −0.01 | 1.01 | 0.01 | −0.07 | 0.02 |
| Panic disorder | 0.00 | 0.65 | 0.10 | 0.34 | 0.40 | 0.14 | 0.23 | 0.56 | −0.05 | 0.10 | 0.25 | −0.02 | 0.56 | 0.04 |
| SAD | −0.12 | 0.76 | −0.15 | 0.66 | 0.25 | −0.10 | 0.00 | 0.72 | 0.17 | −0.06 | 0.02 | 0.02 | 0.51 | 0.43 |
| Specific phobia | 0.01 | 0.54 | 0.02 | 0.43 | 0.20 | 0.06 | −0.04 | 0.61 | 0.03 | 0.01 | −0.04 | 0.03 | 0.64 | 0.07 |
| GAD | −0.12 | 0.79 | 0.00 | 0.42 | 0.50 | 0.02 | 0.36 | 0.49 | 0.06 | −0.01 | 0.38 | 0.07 | 0.48 | 0.07 |
| PG | 0.43 | 0.14 | 0.41 | 0.23 | −0.16 | 0.37 | −0.17 | 0.03 | 0.28 | 0.25 | −0.15 | 0.40 | 0.20 | −0.24 |
| Avoidant PD | 0.01 | 0.83 | −0.08 | 0.82 | 0.15 | −0.06 | 0.03 | 0.46 | 0.50 | 0.05 | 0.01 | 0.19 | 0.01 | 0.76 |
| Dependent PD | 0.16 | 0.73 | 0.07 | 0.76 | 0.07 | 0.08 | −0.03 | 0.38 | 0.51 | 0.20 | −0.02 | 0.28 | 0.03 | 0.57 |
| OCPD | 0.10 | 0.61 | 0.00 | 0.73 | −0.05 | −0.05 | 0.03 | 0.03 | 0.71 | −0.16 | 0.03 | 0.77 | 0.04 | 0.01 |
| Paranoid PD | 0.19 | 0.73 | 0.12 | 0.79 | 0.00 | 0.06 | 0.06 | 0.05 | 0.78 | 0.01 | −0.06 | 0.74 | 0.01 | 0.16 |
| Schizoid PD | 0.09 | 0.68 | 0.02 | 0.74 | 0.01 | −0.03 | 0.07 | 0.05 | 0.72 | −0.08 | 0.07 | 0.67 | −0.01 | 0.17 |
| Histrionic PD | 0.35 | 0.51 | 0.32 | 0.62 | −0.14 | 0.25 | −0.03 | −0.06 | 0.69 | 0.18 | −0.03 | 0.71 | −0.05 | 0.02 |
| Antisocial PD | 0.52 | 0.27 | 0.54 | 0.25 | −0.03 | 0.49 | 0.01 | −0.06 | 0.37 | 0.43 | 0.01 | 0.42 | −0.02 | −0.04 |
| Factor correlation | ||||||||||||||
| Factor 1 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||
| Factor 2 | 0.44 | 1.00 | 0.49 | 1.00 | 0.28 | 1.00 | 0.23 | 1.00 | ||||||
| Factor 3 | 0.25 | 0.42 | 1.00 | 0.30 | 0.46 | 1.00 | 0.47 | 0.34 | 1.00 | |||||
| Factor 4 | 0.40 | 0.40 | 0.64 | 1.00 | 0.31 | 0.31 | 0.62 | 1.00 | ||||||
| Factor 5 | 0.18 | 0.43 | 0.55 | 0.45 | 1.00 | |||||||||
Abbreviations: AA, alcohol abuse; AD, alcohol dependence; BD, bipolar disorder; CFI, Comparative Fit Index; DA, drug abuse; DD, drug dependence; GAD, generalized anxiety disorder; MDD, major depressive disorder; ND, nicotine dependence; OCPD, obsessive compulsive personality disorder; PD, personality disorder; PG, pathological gambling; RMSEA, root mean square error of approximation; SAD, social anxiety disorder; TLI, Tucker-Lewis Index.
In the models with 3 to 5 factors, the first factor replicated the first factor of the 2-factor model, whereas the remaining factors constituted an expansion of the other factor. In the 3-model factor, factor 2 of the 2-factor model subdivided into a factor that included bipolar disorder, social anxiety disorder, specific phobia, and all personality disorders except antisocial personality disorder, and another factor that included MDD, dysthymia, GAD, and panic disorder. In the 4-factor model, factor 2 of the 2-factor model subdivided into 3 factors: a first factor included MDD, dysthymia, and bipolar disorder; a second factor included panic disorder, social anxiety disorder, GAD, and specific phobia; and a third factor included all the personality disorders except antisocial personality disorder. The 5-factor model was very similar to the 4-factor model but with avoidant and dependent personality disorders splitting into a separate factor (Table 1).
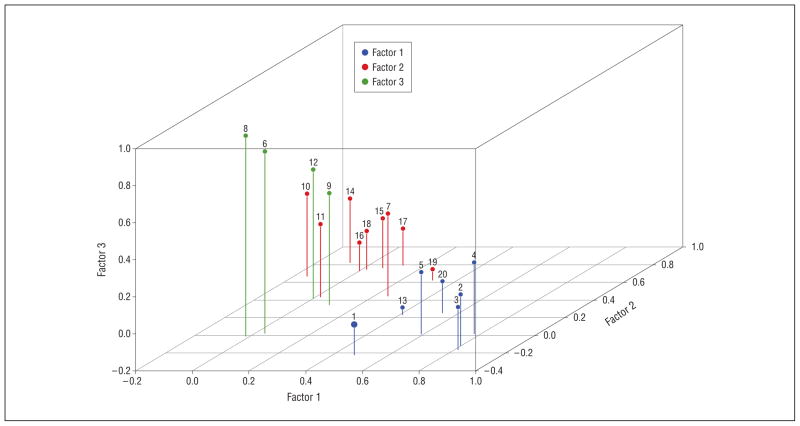
Based on these results, the 3-factor, 4-factor, and 5-factor models were further evaluated. However, because the results for 3 models were very similar (possibly because of the relatively high correlations among factors with higher loadings from internalizing disorders), only the results of the 3-factor model (which is graphically represented in the Figure) are presented. Detailed results of the 4-factor and 5-factor models are presented in eTable 1 and eTable 2 (http://www.jamapsych.com).
Figure.
Three-dimensional representation of the space among psychiatric disorders. Each disorder is represented in the color of the factor for which it has higher loadings. Although the factors are correlated (see Table 1 and the “Results” section), they are represented as orthogonal to facilitate visualization. 1 indicates alcohol abuse; 2, alcohol dependence; 3, drug abuse; 4, drug dependence; 5, nicotine dependence; 6, major depressive disorder; 7, bipolar disorder; 8, dysthymia; 9, panic disorder; 10, social anxiety disorder; 11, specific phobia; 12, generalized anxiety disorder; 13, pathological gambling; 14, avoidant personality disorder; 15, dependent personality disorder; 16, obsessive compulsive personality disorder; 17, paranoid personality disorder; 18, schizoid personality disorder; 19, histrionic personality disorder; 20, antisocial personality disorder.
COORDINATES AND DISTANCE BETWEEN DISORDERS
The coordinates for each disorder can be derived from Table 1. For example, in the 3-factor model, the coordinates for alcohol abuse were 0.476, −0.217, and −0.036, whereas for MDD, they were 0.037, 0.019, and 0.784. There was broad variation in the pattern of coordinates. Some disorders, such as alcohol dependence and avoidant personality disorder, had coordinates with large values in 1 dimension but low in the others. Other disorders, such as bipolar disorder and histrionic personality disorder, had coordinates with moderately large values in 1 dimension and intermediate values in the others.
Table 2 and Table 3 present the Euclidian distances among all pairs of disorders in the 3-factor model. Because Euclidian distances are symmetric, only the cells under the matrix diagonal are presented. Although there was a wide range of distances, with the smallest distance being between drug abuse and alcohol dependence (0.070) and the largest between drug abuse and dysthymia (1.032), the overall pattern indicated that disorders traditionally considered to be more closely related (eg, alcohol dependence and drug dependence) tended to have smaller distances separating them than did disorders considered less similar such as alcohol dependence and MDD.
Table 2.
Euclidian Distances Among Axis I and Axis II Disorders in Wave 1 of the NESARC in the 3-Factor Model
| Alcohol Abuse | Alcohol Dependence | Drug Abuse | Drug Dependence | Nicotine Dependence | MDD | Bipolar Disorder | Dysthymia | Panic Disorder | SAD | |
|---|---|---|---|---|---|---|---|---|---|---|
| Alcohol abuse | 0.00 | |||||||||
| Alcohol dependence | 0.43 | 0.00 | ||||||||
| Drug abuse | 0.39 | 0.07 | 0.00 | |||||||
| Drug dependence | 0.58 | 0.20 | 0.27 | 0.00 | ||||||
| Nicotine dependence | 0.41 | 0.19 | 0.24 | 0.21 | 0.00 | |||||
| MDD | 0.90 | 0.90 | 0.94 | 0.83 | 0.74 | 0.00 | ||||
| Bipolar disorder | 0.74 | 0.61 | 0.66 | 0.49 | 0.43 | 0.59 | 0.00 | |||
| Dysthymia | 0.98 | 0.99 | 1.03 | 0.92 | 0.84 | 0.10 | 0.69 | 0.00 | ||
| Panic disorder | 0.75 | 0.71 | 0.76 | 0.62 | 0.52 | 0.40 | 0.22 | 0.49 | 0.00 | |
| SAD | 0.91 | 0.91 | 0.96 | 0.83 | 0.73 | 0.61 | 0.35 | 0.69 | 0.30 | 0.00 |
| Specific phobia | 0.68 | 0.71 | 0.75 | 0.66 | 0.52 | 0.56 | 0.26 | 0.65 | 0.21 | 0.23 |
| GAD | 0.88 | 0.83 | 0.89 | 0.73 | 0.65 | 0.37 | 0.31 | 0.44 | 0.13 | 0.28 |
| PG | 0.39 | 0.41 | 0.41 | 0.47 | 0.32 | 0.90 | 0.49 | 1.00 | 0.60 | 0.68 |
| Avoidant PD | 0.98 | 0.93 | 0.97 | 0.83 | 0.75 | 0.76 | 0.35 | 0.83 | 0.40 | 0.18 |
| Dependent PD | 0.90 | 0.81 | 0.86 | 0.72 | 0.65 | 0.79 | 0.28 | 0.88 | 0.40 | 0.28 |
| OCPD | 0.82 | 0.81 | 0.84 | 0.75 | 0.64 | 0.83 | 0.36 | 0.91 | 0.45 | 0.29 |
| Paranoid PD | 0.90 | 0.80 | 0.85 | 0.70 | 0.65 | 0.86 | 0.31 | 0.95 | 0.47 | 0.35 |
| Schizoid PD | 0.85 | 0.81 | 0.85 | 0.74 | 0.65 | 0.80 | 0.32 | 0.89 | 0.42 | 0.26 |
| Histrionic PD | 0.73 | 0.62 | 0.66 | 0.56 | 0.50 | 0.93 | 0.36 | 1.02 | 0.54 | 0.52 |
| Antisocial PD | 0.51 | 0.32 | 0.35 | 0.29 | 0.21 | 0.85 | 0.38 | 0.95 | 0.54 | 0.67 |
Abbreviations: GAD, generalized anxiety disorder; MDD, major depressive disorder; NESARC, National Epidemiologic Survey on Alcohol and Related Conditions; OCPD, obsessive compulsive personality disorder; PD, personality disorder; PG, pathological gambling; SAD, social anxiety disorder.
Table 3.
Additional Euclidian Distances Among Axis I and Axis II Disorders in Wave 1 of the NESARC in the 3-Factor Model
| Specific Phobia | GAD | PG | Avoidant PD | Dependent PD | OCPD | Paranoid PD | Schizoid PD | Histrionic PD | Antisocial PD | |
|---|---|---|---|---|---|---|---|---|---|---|
| Specific phobia | 0.00 | |||||||||
| GAD | 0.29 | 0.00 | ||||||||
| PG | 0.48 | 0.73 | 0.00 | |||||||
| Avoidant PD | 0.33 | 0.39 | 0.69 | 0.00 | ||||||
| Dependent PD | 0.32 | 0.44 | 0.58 | 0.14 | 0.00 | |||||
| OCPD | 0.29 | 0.50 | 0.50 | 0.23 | 0.17 | 0.00 | ||||
| Paranoid PD | 0.38 | 0.51 | 0.56 | 0.22 | 0.08 | 0.18 | 0.00 | |||
| Schizoid PD | 0.29 | 0.46 | 0.53 | 0.17 | 0.10 | 0.07 | 0.13 | 0.00 | ||
| Histrionic PD | 0.43 | 0.63 | 0.36 | 0.44 | 0.30 | 0.28 | 0.24 | 0.29 | 0.00 | |
| Antisocial PD | 0.49 | 0.66 | 0.22 | 0.65 | 0.52 | 0.51 | 0.50 | 0.52 | 0.31 | 0.00 |
Abbreviations: GAD, generalized anxiety disorder; MDD, major depressive disorder; NESARC, National Epidemiologic Survey on Alcohol and Related Conditions; OCPD, obsessive compulsive personality disorder; PD, personality disorder; PG, pathological gambling; SAD, social anxiety disorder.
CORRELATION BETWEEN DISTANCE IN WAVE 1 AND PREVALENCE AND INCIDENCE IN WAVE 2
In wave 2, the largest AORs for prevalence were for the disorders with themselves, followed by disorders that were at short distances in wave 1 (Table 4). The correlation coefficient between the distance between pairs of disorders in wave 1 and AORs of prevalence in wave 2 was −0.56 (P<.001), indicating that larger distances in wave 1 were related to weaker associations in wave 2. A similar pattern was found for incidence; although in the case of incidence, by definition, the AOR of the disorder with itself was not computed because the disorder was already present in wave 1 (Table 5). The correlation between distance in wave 1 and the AORs of incidence in wave 2 was −0.57 (P < .001), indicating a strong inverse relationship between distance and incidence. The correlation coefficients for prevalence and incidence were also −0.56 and −0.57, respectively, using the 4-factor model, whereas they were −0.54 and −0.55, respectively, for the 5-factor model. Overall, the results indicate that the closer 2 disorders were in wave 1, the better predictors they were of the prevalence and incidence of each other in wave 2.
Table 4.
Adjusted Odds Ratios of the Prevalence of Axis I and Axis II Disorders in Wave 1 With Prevalence of Axis I in Wave 2
| Wave 1 | Wave 2, Adjusted Odds Ratio
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alcohol Abuse | Alcohol Dependence | Drug Abuse | Drug Dependence | Nicotine Dependence | MDD | Bipolar Disorder | Dysthymia | Panic Disorder | SAD | Specific Phobia | GAD | |
| Alcohol abuse | 6.56 a | 2.73 a | 2.53 a | 1.89 a | 1.71 a | 0.91 | 1.07 | 0.70 | 0.86 | 0.74 | 1.03 | 1.09 |
| Alcohol dependence | 2.23 a | 10.91 a | 3.48 a | 4.32 a | 3.01 a | 1.77 a | 2.63 a | 1.43 | 2.76 a | 2.31 a | 1.35 a | 2.21 a |
| Drug abuse | 2.47 a | 4.46 a | 15.33 a | 7.62 a | 3.23 a | 1.23 | 2.26 a | 0.46 | 2.78 a | 3.02 a | 1.63 a | 1.77 a |
| Drug dependence | 1.51 | 7.18 a | 6.45 a | 22.22 a | 6.52 a | 1.71 | 6.95 a | 1.85 | 4.69 a | 4.05 a | 2.19 a | 4.74 a |
| Nicotine dependence | 1.49 a | 3.13 a | 2.69 a | 4.51 a | 19.72 a | 1.66 a | 2.81 a | 2.50 a | 2.99 a | 2.37 a | 1.96 a | 2.10 a |
| MDD | 1.04 | 1.78 a | 1.83 a | 2.84 a | 1.71 a | 5.16 a | 2.45 a | 8.22 a | 2.90 a | 4.03 a | 2.04 a | 3.92 a |
| Bipolar disorder | 0.96 | 3.12 a | 2.18 a | 2.92 a | 2.49 a | 19.26 a | 5.33 a | 5.14 a | 3.09 a | 4.61 a | ||
| Dysthymia | 0.86 | 1.76 a | 2.84 a | 3.94 a | 2.34 a | 5.07 a | 3.07 a | 15.53 a | 3.60 a | 5.75 a | 2.86 a | 6.44 a |
| Panic disorder | 0.91 | 2.86 a | 2.70 a | 5.12 a | 3.01 a | 2.52 a | 6.11 a | 1.98 a | 10.09 a | 6.54 a | 3.94 a | 4.44 a |
| SAD | 0.76 | 1.73 a | 1.38 | 4.13 a | 1.79 a | 2.33 a | 5.22 a | 2.71 a | 4.53 a | 12.78 a | 3.54 a | 4.46 a |
| Specific phobia | 0.87 | 1.74 a | 1.90 a | 1.75 | 1.88 a | 1.94 a | 2.80 a | 2.01 a | 3.11 a | 3.85 a | 4.58 a | 2.53 a |
| GAD | 1.07 | 2.10 a | 2.21 a | 4.43 a | 2.78 a | 3.00 a | 8.73 a | 6.73 a | 7.28 a | 6.48 a | 2.96 a | 7.72 a |
| PG | 0.50 | 6.66 a | 1.99 | 2.29 | 3.93 a | 2.45 a | 5.82 a | 4.64 a | 1.98 | 0.86 | 2.59 a | 2.26 |
| Avoidant PD | 0.66 | 2.35 a | 1.31 | 5.76 a | 2.05 a | 2.43 a | 8.53 a | 4.22 a | 4.75 a | 13.05 a | 3.19 a | 5.41 a |
| Dependent PD | 0.36 | 3.35 a | 1.61 | 14.82 a | 4.48 a | 2.07 a | 10.73 a | 4.27 a | 7.99 a | 13.07 a | 3.68 a | 11.28 a |
| OCPD | 1.09 | 1.79 a | 1.55 a | 2.23 a | 1.64 a | 1.57 a | 4.06 a | 2.23 a | 2.97 a | 3.15 a | 2.00 a | 3.08 a |
| Paranoid PD | 0.95 | 2.58 a | 1.90 a | 3.96 a | 2.62 a | 1.85 a | 7.01 a | 2.82 a | 4.44 a | 5.27 a | 2.78 a | 4.44 a |
| Schizoid PD | 0.78 | 2.07 a | 2.13 a | 5.36 a | 2.56 a | 2.36 a | 5.20 a | 5.06 a | 3.38 a | 5.45 a | 2.47 a | 4.04 a |
| Histrionic PD | 1.26 | 3.67 a | 3.04 a | 4.29 a | 2.91 a | 1.36 | 6.45 a | 1.90 | 4.24 a | 4.27 a | 2.53 a | 3.85 a |
| Antisocial PD | 1.15 | 2.69 a | 3.14 a | 6.10 a | 3.19 a | 1.27 | 4.20 a | 1.23 | 3.46 a | 2.40 a | 2.12 a | 2.69 a |
Abbreviations: GAD, generalized anxiety disorder; MDD, major depressive disorder; OCPD, obsessive compulsive personality disorder; PD, personality disorder; PG, pathological gambling; SAD, social anxiety disorder.
Significant result.
Table 5.
Adjusted Odds Ratios of the Incidence of Axis I and Axis II Disorders in Wave 1 With Incidence of Axis I in Wave 2
| Wave 1 | Wave 2, Adjusted Odds Ratio
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alcohol Abuse | Alcohol Dependence | Drug Abuse | Drug Dependence | Nicotine Dependence | MDD | Bipolar Disorder | Dysthymia | Panic Disorder | SAD | Specific Phobia | GAD | |
| Alcohol abuse | 3.69 a | 2.51 a | 1.48 | 1.51 a | 1.01 | 1.30 | 0.60 | 0.92 | 0.76 | 0.97 | 1.13 | |
| Alcohol dependence | 2.85 a | 3.57 a | 4.69 a | 1.56 a | 1.54 a | 1.95 a | 1.75 | 1.71 a | 1.74 a | 1.20 | 1.98 a | |
| Drug abuse | 1.86 a | 3.21 a | 9.81 a | 1.65 | 1.10 | 2.19 a | 0.57 | 2.00 a | 2.34 a | 0.93 | 1.68 a | |
| Drug dependence | 1.85 a | 2.86 a | 8.05 a | 2.39 | 0.64 | 6.32 a | 3.15 | 1.62 | 3.39 a | 2.10 a | 2.42 a | |
| Nicotine dependence | 1.65 a | 2.44 a | 2.90 a | 3.87 a | 1.25 a | 2.45 a | 2.12 a | 2.16 a | 2.28 a | 1.81 a | 1.82 a | |
| MDD | 1.10 | 1.63 a | 2.74 a | 2.58 a | 0.96 | 4.11 a | 5.56 a | 2.68 a | 3.08 a | 1.92 a | 3.71 a | |
| Bipolar disorder | 0.75 | 1.72 a | 1.74 a | 2.70 a | 1.01 | 3.08 a | 3.85 a | 2.45 a | 3.74 a | |||
| Dysthymia | 0.64 | 1.38 | 3.38 a | 2.76 a | 1.52 | 2.57 a | 4.96 a | 2.98 a | 3.06 a | 2.93 a | 5.69 a | |
| Panic disorder | 0.95 | 1.81 a | 2.97 a | 3.68 a | 1.92 a | 1.28 | 3.63 a | 1.53 | 4.85 a | 3.18 a | 3.56 a | |
| SAD | 0.91 | 1.26 | 0.98 | 3.73 a | 0.69 | 1.40 | 3.59 a | 1.94 a | 2.72 a | 3.05 a | 2.93 a | |
| Specific phobia | 1.14 | 1.06 | 1.64 a | 1.64 | 0.99 | 1.49 a | 2.04 a | 1.66 | 1.74 a | 2.38 a | 2.07 a | |
| GAD | 1.11 | 1.17 | 2.49 a | 2.89 a | 1.47 | 1.12 | 5.79 a | 4.93 a | 6.27 a | 4.39 a | 2.39 a | |
| PG | 0.46 | 8.49 a | 0.67 | 2.09 | 0.80 | 1.26 | 0.85 | 5.93 a | 2.10 | 0.47 | 3.13 | 3.67 a |
| Avoidant PD | 0.92 | 1.52 | 1.30 | 5.17 a | 0.88 | 1.32 | 5.39 a | 3.55 a | 3.23 a | 6.78 a | 2.59 a | 3.89 a |
| Dependent PD | 0.10 a | 0.95 | 2.95 a | 12.87 a | 1.73 | 1.35 | 7.41 a | 2.56 | 3.47 a | 7.67 a | 1.82 | 7.59 a |
| OCPD | 1.14 | 1.25 | 1.40 | 1.67 a | 0.75 a | 1.10 | 2.81 a | 2.07 a | 2.04 a | 1.65 a | 1.59 a | 2.22 a |
| Paranoid PD | 1.02 | 1.76 a | 1.73 a | 2.88 a | 1.43 a | 1.03 | 4.57 a | 2.29 a | 2.89 a | 2.90 a | 2.08 a | 3.47 a |
| Schizoid PD | 0.76 | 1.60 a | 1.63 | 5.25 a | 1.26 | 1.20 | 3.88 a | 3.94 a | 2.75 a | 3.35 a | 2.30 a | 2.99 a |
| Histrionic PD | 1.36 | 1.78 a | 3.09 | 3.54 a | 1.46 | 0.63 | 5.05 a | 1.72 a | 2.47 a | 3.17 a | 1.49 | 2.31 a |
| Antisocial PD | 1.41 a | 1.67 a | 2.92 a | 5.26 a | 1.45 a | 0.98 | 3.55 a | 0.89 | 2.64 a | 1.90 a | 1.84 a | 2.28 a |
Abbreviations: GAD, generalized anxiety disorder; MDD, major depressive disorder; OCPD, obsessive compulsive personality disorder; PD, personality disorder; PG, pathological gambling; SAD, social anxiety disorder.
Significant result.
COMPLEMENTARY ANALYSES
The fit indices for the bifactor model with a general factor and 3 disorder-specific factors were 0.982 for CFI, 0.977 for TLI, and 0.009 for RSMEA (eTable 3), and the correlation of distance with the prevalence and incidence of Axis I disorders in wave 2 were −0.56 and −0.57, respectively, whereas a bifactor model with 4 disorder-specific factors produced implausible parameter estimates (eg, standard errors considerably larger than parameter estimates on some of the disorder-specific factors). The fit indices for the 3-factor CFA model were 0.959 for CFI, 0.953 for TLI, and 0.0013 for RSMEA, whereas for the 4-factor CFA model, they were 0.973 for CFI, 0.969 for TLI, and 0.010 for RSMEA. Although the fit of these CFA models was slightly worse than for the corresponding EFA models, it was still good for both the 3-factor and 4-factor CFA models. However, for the 3-factor model, the correlation of distance with prevalence of Axis I disorders in wave 2 was only −0.42, whereas the correlation with incidence was −0.38. For the 4-factor model, the corresponding correlations were −0.31 and −0.26. Furthermore, the correlation of the inverse of the AORs in wave 1 with the AORs of the prevalence and incidence in wave 2 were −0.33 and −0.35, respectively.
COMMENT
In a large nationally representative sample, interrelationships among disorders were well described by 3 correlated dimensions, 2 of which included Axis I and Axis II disorders. When the factors were used to span a space and their loadings used as the coordinates in that space, disorders included in the same DSM-IV diagnostic groups tended to have smaller distances among themselves than from disorders in other diagnostic groups. Furthermore, proximity across disorders significantly predicted prevalence and incidence in wave 2.
We found that the patterns of associations of psychiatric disorders could be described by a relatively small number of underlying dimensions. Our findings are consistent with previous studies, which have documented that 2 to 3 correlated factors (ie, dimensions) capture the patterns of comorbidity among the most common psychiatric disorders.8,10,12,33 The dimensions identified in our study are similar to those identified in previous investigations (which include an externalizing dimension and a variable number of internalizing dimensions), supporting the robustness of these findings across different samples and extending them by including 7 personality disorders. By using the loadings to align the disorders along those dimensions, it was possible to obtain an estimate of the relative importance of each dimension for each disorder and create a space in which psychiatric disorders could be placed.
Disorders considered nosologically related (eg, those grouped in the same DSM-IV chapters) had generally smaller distances among themselves than did those grouped in different categories. Furthermore, proximity at baseline, as measured by the distances obtained from the EFA, was highly correlated with the incidence and prevalence of disorders 3 years later, and it provided a stronger measure of association than alternative approaches such as using CFA to estimate distances or using the ORs at baseline to predict the prevalence and incidence of disorders at follow-up. Our findings are generally consistent with the existing DSM-IV chapter headings and suggest that, in addition to having face validity, these categories provide information about the underlying similarities across disorders and have prognostic validity. These patterns are also consistent with findings by Krueger et al9 and Vollebergh et al,10 who found substantial within-subject stability (also called rank or differential stability) on the scores in the latent factors. By using the concept of proximity in the space of psychiatric disorders and a prospective design, our results extend and generalize recent findings from the World Mental Health Survey Initiative.13 Using a retrospective design, that study found that 2 latent variables, one representing an internalizing dimension and the other representing an externalizing dimension, predicted the onset of psychiatric disorders during the life course. Taken together, these findings may help inform development of the DSM-5 and other future classifications of psychiatric disorders.1,3
To our knowledge, our study is only the third to include a substantial number of Axis I and Axis II disorders,14,34 and the first to use a nationally representative sample. In the 3-factor model, the dimensions identified by our analyses did not neatly correspond with Axis I and Axis II disorders but rather corresponded to the more general processes identified in prior structural psychiatric nosologic studies. In accord with results from clinical samples,32 disorders considered nosologically related, such as social anxiety disorder and avoidant personality disorder, had similar loadings across the dimensions and were therefore close to one another.35 The same was true of antisocial personality disorder and Axis I disorders characterized by high impulsivity such as pathological gambling and SUDs. These findings are consistent with current conceptualizations that question the categorical distinction between Axis I and Axis II disorders36–38 and that relate psychiatric disorders with personality traits described in the broader psychologic literature.39,40
By contrast, our 4-factor model revealed a dimension that loaded on all personality disorders assessed in wave 1 except antisocial personality disorder. This model may be more in line with recent findings from the Norwegian Twin Panel Study,34 which found that 4 factors (2 of which loaded mainly on personality disorders) provided a good fit for 25 Axis I and Axis II disorders. However, even in that study, the pattern of intercorrelations among factors, as well as the loadings of antisocial personality disorder, borderline personality disorder, and dysthymia, suggested some overlap rather than clear separation between Axis I and Axis II disorders. Furthermore, our 4-factor model did not substantially improve the fit of the model, change the distances among disorders, or modify the strength of association between the distance among disorders and the prevalence and incidence of wave 2 disorders. The 5-factor model was very similar to the 4-factor model and, although it had a slightly better fit, it also had slightly lower correlations with the incidence and prevalence of Axis I disorders in wave 2. The bifactor model also provided a good fit to the data, consistent with promising results in a recent twin study of adolescent psychopathology.41 As our understanding of the structure of mental disorders continues to advance, it is possible that for certain applications, the 4-factor or 5-factor models or the bifactor model may present advantages over the 3-factor model.
Our findings have nosologic, etiologic, and clinical implications. From the nosologic perspective, our approach generalizes the concept of spectrum disorders to multiple dimensions by creating a space where disorders can be located and to quantify the relative importance of each dimension for each disorder. Our results indicate that no disorder is perfectly aligned along 1 dimension, but rather all disorders include components of several dimensions, albeit in different proportions. Our findings are in accord with previous studies that have suggested that SUDs42 and borderline personality disorder are best conceptualized as multidimensional, having facets of both internalizing and externalizing disorders.36,43 Prior epidemiologic13,44 and twin studies12,33 have also shown substantial cross-loadings among factors. By delineating a space, our study is consistent with recent conceptualizations of psychiatric disorders as continuous rather than discrete entities.8,10,45 Our approach helps support and provides a way to visualize the conceptualization that internalization and externalization are not opposite poles in a spectrum of disorders but rather positively correlated dimensions.8,10,12 When variables are positively correlated, increases in one variable are associated with increases in the other. Therefore, a disorder such as drug dependence that loads predominantly on 1 dimension (externalizing disorders) does not decrease but rather increases the risk for disorders, such as social anxiety disorder or GAD, that load predominantly on other dimensions. Our findings are consistent with previous studies that have documented that the presence of 1 psychiatric disorder increases the risk for most other psychiatric disorders.22,46,47
From the etiologic point of view, our analyses converge with findings from genetic epidemiology12,33 and molecular genetics48 research, suggesting that disorders that are closer to each other are more likely to share liabilities than those located further apart. Furthermore, because each disorder loads on several dimensions (ie, liabilities), our findings suggest that disorders can develop through multiple etiologic paths, although those dimensions with higher loadings may be more common pathways.5 For example, the risk for nicotine dependence may be particularly high in individuals with a propensity toward externalization, but it may also be increased in individuals with some internalizing disorders such as depression.49 Alternatively, it is also possible that several dimensions may have to be affected before a full-blown disorder manifests itself. For example, bipolar disorder may involve abnormalities in facets related to both internalizing and externalizing dimensions. Also converging with the current findings, recent research has started to investigate whether proximity among disorders is the same when examining the structure of their shared genetic vs environmental variance. For example, the Norwegian Twin Panel Study34 found that from a genetic perspective, dysthymia is closely related to personality disorders (ie, close in the genetic space), whereas its environmental risk factors place it much closer to major depression. By contrast, alcohol abuse or dependence were environmentally closer to internalizing disorders, but they shared genetic risk factors with Axis I externalizing disorders. Continuing to uncover the sources of proximities among disorders could help identify common and specific etiologic pathways for those disorders, suggest which neurobiological mechanisms and brain structures or circuits may be shared across disorders, and help guide treatment research. Alternatively, treatments that have efficacy for different disorders may suggest previously undetected etiologic links among disorders. The convergence of multimodal maps50 that integrate data from genetics, neuroimaging, treatment response, and possibly other domains should lead to a more empirically based classification of psychiatric disorders.51
From the clinical perspective, knowledge of the proximity among disorders may help narrow the differential diagnoses as more closely related disorders are more likely to co-occur. Because disorder proximity also provides information about which disorders are most likely to co-occur in the future, spatial mapping may help guide preventive interventions. Proximity among disorders can also inform treatment development. Disorders that are close to each other may have aspects similar to the one being treated, thus they may need to be targeted or prevented. Alternatively, the location of each disorder may suggest how treatments that work for one disorder may need to be modified to address other facets of a neighboring disorder. For example, the efficacy of selective serotonin reuptake inhibitors in the treatment of social anxiety disorder may suggest their efficacy for the treatment of avoidant personality disorder.
Our study should be understood in the context of several limitations. First, although the study included a broad range of disorders, some disorders, such as obsessive compulsive disorder or eating disorders, were not assessed in the NESARC. Inclusion of these disorders might have resulted in identification of additional dimensions. Second, the NESARC did not collect information on individuals younger than age 18 years. It is possible that the space of common psychiatric disorders differs between adults and young people. Data from the National Comorbidity Survey–Adolescent Supplement may be helpful in examining this hypothesis. Third, our study used factor analysis and Euclidian distances to create a space of disorders and calculate the distances among disorders. An important avenue for future research would be the use of other distances or statistical techniques, such as multidimensional scaling,20 exploratory structural equation modeling,52 or self-organizing maps,53 to examine whether alternative approaches can yield additional insights into the structure or etiology of psychiatric disorders.
Despite these limitations, this study helps to advance our understanding of the structure of several DSM-IV Axis I and Axis II disorders. Psychiatric disorders can be conceptualized as existing in a space with a limited number of fundamental dimensions. Proximity in that space can be used to assess nosologic similarity, provide a measure of the likelihood of current and future co-occurrence across disorders, and may yield clues about shared etiology and treatment response. We hope this information can be useful in the development of new classification systems and guide research on etiology and treatment.
Supplementary Material
Acknowledgments
Funding/Support: The National Epidemiologic Survey on Alcohol and Related Conditions was sponsored by the National Institute on Alcohol Abuse and Alcoholism, with supplemental support from the National Institute on Drug Abuse. Work on this article was supported by grants DA019606, DA020783, DA023200, DA023973, CA133050, and MH082773 to Dr Blanco, AA014223 and AA018111 to Dr Hasin, and F31DA025377 to Mr Kerridge from the National Institutes of Health, and the New York State Psychiatric Institute (Drs Blanco, Hasin, and Olfson).
Footnotes
Author Contributions: Dr Blanco had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of Interest Disclosures: Dr Olfson has worked on grants from Eli Lilly and Company and Bristol-Myers Squibb to Columbia University.
Online-Only Material: The eTables are available at http://www.jamapsych.com.
References
- 1.Andrews G, Goldberg DP, Krueger RF, Carpenter WT, Jr, Hyman SE, Sachdev P, Pine DS. Exploring the feasibility of a meta-structure for DSM-V and ICD-11: could it improve utility and validity? Psychol Med. 2009;39(12):1993–2000. doi: 10.1017/S0033291709990250. [DOI] [PubMed] [Google Scholar]
- 2.First MB. Reorganizing the diagnostic groupings in DSM-V and ICD-11: a cost/benefit analysis. Psychol Med. 2009;39(12):2091–2097. doi: 10.1017/S0033291709991152. [DOI] [PubMed] [Google Scholar]
- 3.Hyman SE. Can neuroscience be integrated into the DSM-V? Nat Rev Neurosci. 2007;8(9):725–732. doi: 10.1038/nrn2218. [DOI] [PubMed] [Google Scholar]
- 4.Regier DA, Narrow WE, Kuhl EA, Kupfer DJ. The conceptual development of DSM-V. Am J Psychiatry. 2009;166(6):645–650. doi: 10.1176/appi.ajp.2009.09020279. [DOI] [PubMed] [Google Scholar]
- 5.Krueger RF, South SC. Externalizing disorders: cluster 5 of the proposed meta-structure for DSM-V and ICD-11. Psychol Med. 2009;39(12):2061–2070. doi: 10.1017/S0033291709990328. [DOI] [PubMed] [Google Scholar]
- 6.Krueger RF, Markon KE, Patrick CJ, Iacono WG. Externalizing psychopathology in adulthood: a dimensional-spectrum conceptualization and its implications for DSM-V. J Abnorm Psychol. 2005;114(4):537–550. doi: 10.1037/0021-843X.114.4.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blanco C, Moreyra P, Nunes EV, Sáiz-Ruiz J, Ibáñez A. Pathological gambling: addiction or compulsion? Semin Clin Neuropsychiatry. 2001;6(3):167–176. doi: 10.1053/scnp.2001.22921. [DOI] [PubMed] [Google Scholar]
- 8.Krueger RF. The structure of common mental disorders. Arch Gen Psychiatry. 1999;56(10):921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 9.Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. J Abnorm Psychol. 1998;107(2):216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 10.Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: the NEMESIS study. Arch Gen Psychiatry. 2001;58(6):597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- 11.Krueger RF, Chentsova-Dutton YE, Markon KE, Goldberg D, Ormel J. A cross-cultural study of the structure of comorbidity among common psychopathological syndromes in the general health care setting. J Abnorm Psychol. 2003;112(3):437–447. doi: 10.1037/0021-843x.112.3.437. [DOI] [PubMed] [Google Scholar]
- 12.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60(9):929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 13.Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, Stein DJ, Zaslavsky AM, Aguilar-Gaxiola S, Alonso J, Andrade L, Benjet C, de Girolamo G, de Graaf R, Demyttenaere K, Fayyad J, Haro JM, Hu Cy, Karam A, Lee S, Lepine JP, Matchsinger H, Mihaescu-Pintia C, Posada-Villa J, Sagar R, Ustün TB. Development of lifetime comorbidity in the World Health Organization World Mental Health Surveys. Arch Gen Psychiatry. 2011;68(1):90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Arch Gen Psychiatry. 2011;68(10):1003–1011. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- 15.American Psychiatric Association. The Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 16.World Health Organization. The International Classification of Diseases. 10. Geneva, Switzerland: World Health Organization; 1990. [Google Scholar]
- 17.Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behav Ther. 2004;35(2):205–230. doi: 10.1016/S0005-7894(04)80036-4. [DOI] [PubMed] [Google Scholar]
- 18.Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, Ehrenreich-May J, editors. The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders: Therapist Guide. New York, NY: Oxford University Press; 2011. [Google Scholar]
- 19.Leon S, editor. Linear Algebra With Applications. Upper Saddle River, NJ: Prentice Hall; 2004. [Google Scholar]
- 20.Johnson RA, Wichern DW. Applied Multivariate Statistical Analysis. 5. Upper Saddle River, NJ: Prentice Hall; 2002. [Google Scholar]
- 21.Grant BF, Moore T, Shepard J, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- 22.Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP, Ruan WJ, Compton WM. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2009;14(11):1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(4):361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- 24.Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39(1):37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- 25.Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92(1–3):27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Canino G, Bravo M, Ramírez R, Febo VE, Rubio-Stipec M, Fernández RL, Hasin D. The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. J Stud Alcohol. 1999;60(6):790–799. doi: 10.15288/jsa.1999.60.790. [DOI] [PubMed] [Google Scholar]
- 27.Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D. Reliability of the alcohol and drug modules of the Alcohol Use Disorder and Associated Disabilities Interview Schedule–Alcohol/Drug-Revised (AUDADIS-ADR): an international comparison. Drug Alcohol Depend. 1997;47(3):171–185. doi: 10.1016/s0376-8716(97)00088-4. [DOI] [PubMed] [Google Scholar]
- 28.Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend. 1997;44 (2–3):133–141. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- 29.Muthen L, Muthen BO, editors. Mplus User’s Guide. 5. Los Angeles, CA: Muthen and Muthen; 2010. [Google Scholar]
- 30.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6 (1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 31.Bollen K, editor. Structural Equation With Latent Variables. New York, NY: John Wiley and Sons; 1989. [Google Scholar]
- 32.Reise SP, Morizot J, Hays RD. The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Qual Life Res. 2007;16(suppl 1):19–31. doi: 10.1007/s11136-007-9183-7. [DOI] [PubMed] [Google Scholar]
- 33.Kendler KS, Aggen SH, Knudsen GP, Røysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV Axis I and all Axis II disorders. Am J Psychiatry. 2011;168(1):29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Røysamb E, Kendler KS, Tambs K, Orstavik RE, Neale MC, Aggen SH, Torgersen S, Reichborn-Kjennerud T. The joint structure of DSM-IV Axis I and Axis II disorders. J Abnorm Psychol. 2011;120(1):198–209. doi: 10.1037/a0021660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huppert JD, Strunk DR, Ledley DR, Davidson JRT, Foa EB. Generalized social anxiety disorder and avoidant personality disorder: structural analysis and treatment outcome. Depress Anxiety. 2008;25(5):441–448. doi: 10.1002/da.20349. [DOI] [PubMed] [Google Scholar]
- 36.James LM, Taylor J. Revisiting the structure of mental disorders: borderline personality disorder and the internalizing/externalizing spectra. Br J Clin Psychol. 2008;47(pt 4):361–380. doi: 10.1348/014466508X299691. [DOI] [PubMed] [Google Scholar]
- 37.Krueger RF. Continuity of Axes I and II: toward a unified model of personality, personality disorders, and clinical disorders. J Pers Disord. 2005;19(3):233–261. doi: 10.1521/pedi.2005.19.3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schmidt N, Kotov R, Joiner T, editors. Towards a New Diagnostic Scheme for Psychopathology. Washington, DC: American Psychiatric Association; 2004. [Google Scholar]
- 39.Khan AA, Jacobson KC, Gardner CO, Prescott CA, Kendler KS. Personality and comorbidity of common psychiatric disorders. Br J Psychiatry. 2005;186(3):190–196. doi: 10.1192/bjp.186.3.190. [DOI] [PubMed] [Google Scholar]
- 40.Krueger RF, Markon KE. Reinterpreting comorbidity: a model-based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol. 2006;2(2):111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lahey BB, Van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Arch Gen Psychiatry. 2011;68(2):181–189. doi: 10.1001/archgenpsychiatry.2010.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wittchen HU, Fröhlich C, Behrendt S, Günther A, Rehm J, Zimmermann P, Lieb R, Perkonigg A. Cannabis use and cannabis use disorders and their relationship to mental disorders: a 10-year prospective-longitudinal community study in adolescents. Drug Alcohol Depend. 2007;88(suppl 1):S60–S70. doi: 10.1016/j.drugalcdep.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 43.Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, Hasin DS. Borderline personality disorder comorbidity: relationship to the internalizing-externalizing structure of common mental disorders. Psychol Med. 2011;41 (5):1041–1050. doi: 10.1017/S0033291710001662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication [published correction appears in Arch Gen Psychiatry. 2005;62(7):709] Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Clark LA, Watson D, Reynolds S. Diagnosis and classification of psychopathology: challenges to the current system and future directions. Annu Rev Psychol. 1995;46(1):121–153. doi: 10.1146/annurev.ps.46.020195.001005. [DOI] [PubMed] [Google Scholar]
- 46.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication [published correction appears in Arch Gen Psychiatry. 2005;62(7):768] Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 47.Morcillo C, Duarte CS, Sala R, Wang S, Lejuez CW, Kerridge BT, Blanco C. Conduct disorder and adult psychiatric diagnoses: associations and gender differences in the US adult population. J Psychiatr Res. 2012;46(3):323–330. doi: 10.1016/j.jpsychires.2011.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dick DM, Aliev F, Wang JC, Grucza RA, Schuckit M, Kuperman S, Kramer J, Hinrichs A, Bertelsen S, Budde JP, Hesselbrock V, Porjesz B, Edenberg HJ, Bierut LJ, Goate A. Using dimensional models of externalizing psychopathology to aid in gene identification. Arch Gen Psychiatry. 2008;65(3):310–318. doi: 10.1001/archpsyc.65.3.310. [DOI] [PubMed] [Google Scholar]
- 49.Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(11):1107–1115. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- 50.Toga AW, Thompson PM, Mori S, Amunts K, Zilles K. Towards multimodal atlases of the human brain. Nat Rev Neurosci. 2006;7(12):952–966. doi: 10.1038/nrn2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167(7):748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 52.Marsh HW, Muthen B, Asparouhov T, Lüdtke O, Robitzsch A, Morin AJS, Trautwein U. Exploratory structural equation modeling, integrating CFA and EFA: application to students’ evaluations of university teaching. Struct Equ Modeling. 2009;16(3):439–476. doi: 10.1080/10705510903008220. [DOI] [Google Scholar]
- 53.Kohonen T. Self-Organizing Maps. Berlin, Germany: Springer; 2001. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.