Abstract
Objective
To examine racial/ethnic disparities in medication adherence between Asian and Pacific Islander Americans and Whites.
Methods
This retrospective data analysis included diabetes patients enrolled in a Hawaiian health plan (N = 43,445). For anti-diabetic, lipid-lowering, and anti-hypertensive medications, quantile regression was estimated at 25th, 50th, and 75th quantiles to examine the association with race and ethnicity, controlling for other patient characteristics.
Results
Consistently, Filipinos, Native Hawaiians, and other Pacific Islanders were significantly less adherent than Whites. The greatest disparities were found for other Pacific Islanders using lipid-lowering medications, with adjusted differences in medication adherence, with reductions relative to Whites of as much as 19% for lipid-lowering medications for the 25th quantile of adherence.
Conclusion
Whereas the large sample size undoubtedly contributed to the statistical significance, the large magnitude of the disparities, particularly for Filipinos, Native Hawaiians, and other Pacific Islanders, suggests that these are meaningful differences that need to be addressed. The largest disparities were found at the lowest quantile suggests that they may be occurring among the most vulnerable populations with potentially poor access to care.
A World Health Organization report called poor medication adherence a “worldwide problem of striking magnitude.”1 Although it is well known that anti-diabetic, anti-hypertensive, and lipid-lowering therapies significantly reduce the risk of adverse cardiac events in patients with diabetes, adherence to recommended medication treatment regimens is known to be low,2-5 particularly in certain racial or ethnic subgroups. Consistent results in prior studies show that African Americans and Latinos are less likely than Whites to adhere to medication regimens, regardless of medical condition, type of health insurance coverage, and way in which adherence is measured.6-38
Despite the fact that Asian and Pacific Islander populations in the US are growing more rapidly than most other groups, few studies have examined the relationship between Asian and Pacific Islander ethnicity and medication adherence. The studies that do exist provide conflicting findings.39,40 Our prior work has found significant disparities in medication adherence between Asian American and Pacific Islander subgroups and Whites.41-44 In particular, Native Hawaiians and Filipinos tend to be less adherent to medications than Whites, Japanese, and Chinese. Existing disparities among subgroups highlight the importance of analyzing disparities in specific ethnic subgroups rather than combining all Asian and Pacific Islander groups into one category due to large variation in health-related behavior, quality of care, and health status among these ethnic subgroups.45,46
Most of these studies, as well as other medication adherence studies, however, define adherence as a possession ratio or percent of covered days greater than 80% and use logistic regression models to examine the relationship of predictor variables, including race and ethnicity, and the likelihood that a patient reaches that 80% threshold. This paper takes a different approach, using quantile regression to obtain a more comprehensive view of ethnic disparities in medication adherence. Quantile regression models the relationship between a set of predictor variables and specific quantiles (or quantiles) of the response variable.15,47,48
In our study, quantile regression is useful in that it provides a comprehensive view of the relationships between ethnicity and medication adherence and can bring to light differences in the tails as well as the center of the adherence distribution. For example, a 50th quantile regression of medication adherence specifies the differences in the median adherence related to ethnicity. However, ethnic disparities may vary substantially between quantiles and may only be statistically significant in specific quantiles of the adherence distribution. Hence, quantile regression might find that Native Hawaiians have lower adherence at the 25th quantile but have similar adherence at the 50th quantile, suggesting that special attention should be focused on those within that quantile. By focusing on mean adherence or dichotomous criteria (such as an 80% adherence rate), traditional linear and logistic regression models might miss these disparities. The objective of this study was to examine heterogeneous impacts of race and ethnicity at different quantiles of the adherence distribution as defined by percent of covered days.
When examining ethnic or racial disparities, issues of potential confounding need to be addressed. In our study, we control for age, sex, history of cardiovascular disease, and overall morbidity level; however, one limitation of the study is potential confounding by factors for which we were unable to adjust due to lack of data, including socioeconomic status and access to care.
METHODS
Study Sample
This retrospective claims analysis identified patients with diabetes enrolled in a large health plan in Hawaii from 1/1/2007 through 12/31/2010 (N = 116,726 observations for 45,047 patients).
Diabetes was identified using a disease management algorithm as either having 2 or more claims for type 2 diabetes in medical claims ([ICD-9-CM] codes 250.xx) or had at least one prescription for an oral hypoglycemic agent and/or insulin.
Measures
Patient information including age, sex, history of cardiovascular disease, morbidity level, and year was obtained from administrative data. Patient morbidity level was determined by using ICD-9-CM codes according to the Johns Hopkins Adjusted Clinical Group methodology; levels of 4 or 5 on the 5-point scale were considered high morbidity.49 The year variable was dichotomous and controlled for the year in which adherence was measured (2007–2010).
Data on ethnicity were available for 44% of patients from annual membership surveys. Members were asked to check all ethnicities that applied. Those who selected more than one ethnicity were classified as “mixed race” and excluded from the analyses (N = 1456). The exception was Native Hawaiians. In keeping with the approach used by the Hawai’i State Department of Health, we categorized as Hawaiian anyone who checked Hawaiian even if they checked more than one other ethnicity.50 Ethnic categories for this study included the 6 largest groups: White, Filipino, Japanese, Chinese, Native Hawaiian, and other Pacific Islander. All other racial or ethnic groups were combined into an “other race” category.
Medication fill data including medication names, fill dates, and days of supply were obtained from pharmacy claims databases. Medication adherence was assessed for 3 types of medications: (1) anti-diabetic, (2) lipid-lowering, and (3) anti-hypertensive. To estimate medication adherence, we used the proportion of days covered (PDC), calculated as:
PDC is a well-validated and widely-used measure of medication adherence.51,52 We determined the patient’s measurement period as the index prescription date to the end of the calendar year or to the date of disenrollment. Within the measurement period, we counted the days the patient was covered by at least one drug for each type of medication based on the prescription fill date and days of supply. The number of covered days was divided by the number of days of drug coverage and multiplied this number by 100 to obtain the PDC (as a percentage) for each patient.
Analysis Plan
Initially, we tabulated frequencies of the patient characteristics in year 2007 according to racial and ethnic groups and tested for statistical significance using analysis of variance for age and Pearson’s chi-square test for categorical variables. To examine the relationship among race and ethnicity and medication adherence, quantile regression was estimated at 25th, 50th, and 75th quantiles.48 Control variables included age, sex, region (Honolulu vs other), comorbidity level, history of coronary artery disease or congestive heart failure, and year. All analyses were conducted using Stata statistical software, Version 11.53
RESULTS
Patient Characteristics
All patient characteristics differed significantly by race and ethnicity (Table 1). Mean age ranged from 55 years old for other Pacific Islanders to 67 years old for Japanese and Chinese; percent female ranged from 45% for Whites to 57% for Filipinos. The percentage living in Honolulu varied significantly from 21% of Native Hawaiians to 66% of Chinese. High morbidity ranged from 47% for Whites to 30% for other Pacific Islanders. For coronary artery disease, percentages ranged from 21% for Pacific Islanders to 33% for Chinese; for congestive heart failure, percentages ranged from 12% for Japanese, Chinese, and Filipinos to 18% for Native Hawaiians.
Table 1. Patient Characteristics at Baseline According to Race and Ethnicity (N =43,445).
| White (N = 1705) |
Japanese (N = 7800) |
Chinese (N = 1293) |
Filipino (N = 2970) |
Native Hawaiian (N = 3378) |
Other Pacific Islander (N = 210) |
Other race (N = 1206) |
Race missing (N = 24,883) |
p-valuea | |
|---|---|---|---|---|---|---|---|---|---|
|
Age
(mean, SD) |
63.3 (11.3) | 67.4 (11.6) | 67.5 (12.0) | 62.6 (12.3) | 61.0 (12.3) | 54.8 (12.4) | 65.1 (12.1) | 56.7 (13.9) |
< .001 |
| Female (%) | 44.8% | 53.6% | 51.3% | 57.1% | 55.5% | 48.1% | 51.6% | 44.6% | < .001 |
| Honolulu (%) | 27.3% | 38.5% | 66.0% | 21.9% | 21.0% | 27.6% | 33.1% | 29.6% | < .001 |
|
High
Morbidity (%) |
46.9% | 42.0% | 40.7% | 34.6% | 40.2% | 30.0% | 44.9% | 25.4% | < .001 |
|
Coronary
Artery Disease (%) |
29.0% | 27.7% | 32.6% | 24.4% | 29.7% | 21.0% | 32.6% | 17.7% | < .001 |
|
Congestive
Heart Failure (%) |
14.0% | 11.5% | 12.1% | 12.0% | 18.2% | 12.9% | 15.6% | 8.5% | < .001 |
Note.
Analysis of variance was used to examine differences in age; Pearson’s chi-squared test was used for categorical variables.
Medication Adherence Related to Race and Ethnicity
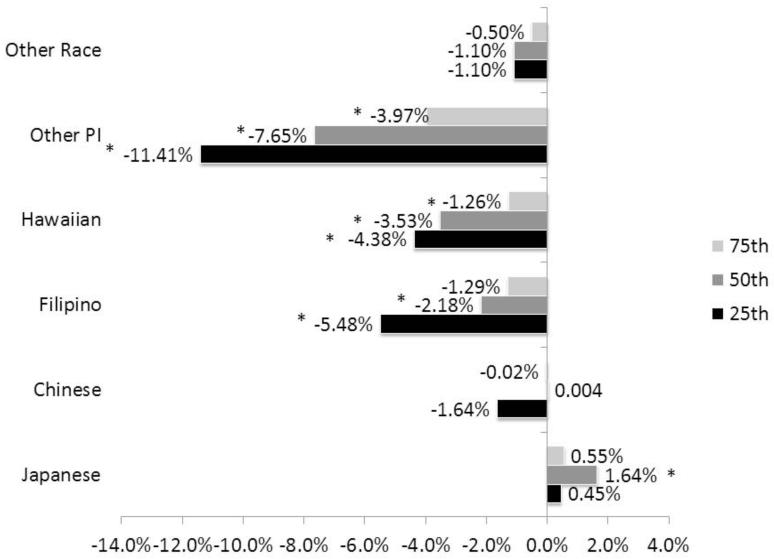
The 3 figures display differences in medication adherence for each racial and ethnic group compared to Whites for the 3 types of medications: anti-diabetic, lipid-lowering, and anti-hypertensive. For anti-diabetic medications, the adherence of Chinese and Japanese did not differ significantly from Whites, except that Japanese had significantly higher adherence at the 75th quantile (Figure 1, Table 2). Filipinos, Native Hawaiians, and other Pacific Islanders were significantly less adherent than Whites for anti-diabetic medications at every quantile level examined. The greatest disparities were found for other Pacific Islanders at all 3 quantiles, with a difference relative to Whites of −11.4% at the 25th, −7.6% at 50th, and −4.0% for 75th quantiles. We found a similar trend, with larger disparities at lower quantile levels for Filipinos (−5.5% at 25th, −2.2% at the 50th, −1.3% at 75th quantile) and Native Hawaiians (−4.4% at the 25th, −3.5% at the 50th, −1.3% at the 75th).
Figure 1. Differences in Adherence to Anti-diabetes Medications Relative to Whites for each Ethnic Group by Quantile (Adjusted).
* = p < .05
Note.
Specific p-values can be found in Table 2. Adjusted for age, sex, living in Honolulu, high morbidity, history of coronary artery disease or congestive heart failure, and year.
Table 2. Medication Adherence Estimates from Quantile Regression Models (Adjusted)*.
| 25th | 50th | 75th | |||||
|---|---|---|---|---|---|---|---|
| Adjusted | p-value | Adjusted | p-value | Adjusted | p-value | ||
|
Adherence to Anti-diabetic Medications (N = 112,897 observations for
43,445 patients) |
Age <35 | 22.9% | < .001 | 47.3% | < .001 | 75.3% | < .001 |
| Age 35-49 | 36.6% | < .001 | 65.6% | < .001 | 86.9% | < .001 | |
| Age 50-64 | 52.6% | Ref | 77.6% | Ref | 91.6% | Ref | |
| Age 65+ | 55.5% | < .001 | 79.3% | < .001 | 92.3% | < .001 | |
| Female | 49.0% | < .001 | 73.9% | < .001 | 89.8% | < .001 | |
| Male | 51.0% | Ref | 76.1% | Ref | 91.0% | Ref | |
| Honolulu | 51.8% | < .001 | 76.8% | < .001 | 91.0% | .02 | |
| Other regions | 48.9% | Ref | 74.3% | Ref | 90.1% | Ref | |
| High morbidity | 50.6% | < .001 | 75.7% | < .001 | 90.7% | < .001 | |
| Low morbidity | 49.5% | Ref | 74.8% | Ref | 90.3% | Ref | |
| Coronary artery disease | 53.1% | .4 | 77.3% | 1.0 | 91.5% | .4 | |
| Congestive heart failure | 50.4% | < .001 | 74.9% | < .001 | 90.6% | < .001 | |
| White | 56.9% | Ref | 79.6% | Ref | 92.4% | Ref | |
| Japanese | 57.6% | .5 | 81.2% | < .001 | 92.9% | .07 | |
| Chinese | 56.0% | .2 | 80.0% | 1.0 | 92.4% | 1.0 | |
| Filipino | 50.7% | < .001 | 76.9% | < .001 | 90.8% | .002 | |
| Native Hawaiian | 50.4% | < .001 | 74.1% | < .001 | 90.2% | < .001 | |
| Other Pacific Islander | 42.0% | < .001 | 69.2% | < .001 | 90.2% | .001 | |
| Other race | 55.7% | .2 | 78.3% | .1 | 91.8% | .2 | |
|
| |||||||
|
Adherence to Lipid-Lowering Medications (N = 82,477 observations
for 30,801 patients) |
Age <35 | 18.1% | < .001 | 38.8% | < .001 | 69.4% | < .001 |
| Age 35-49 | 31.5% | < .001 | 60.1% | < .001 | 83.4% | < .001 | |
| Age 50-64 | 46.5% | Ref | 72.9% | Ref | 88.3% | Ref | |
| Age 65+ | 50.1% | < .001 | 75.1% | < .001 | 89.8% | < .001 | |
| Female | 42.3% | < .001 | 68.1% | < .001 | 86.4% | < .001 | |
| Male | 45.9% | Ref | 71.8% | Ref | 88.1% | Ref | |
| Honolulu | 46.2% | < .001 | 72.2% | < .001 | 88.3% | < .001 | |
| Other regions | 43.2% | Ref | 69.1% | Ref | 86.9% | Ref | |
| High morbidity | 44.9% | .1 | 70.2% | .3 | 87.3% | .7 | |
| Low morbidity | 43.9% | Ref | 70.0% | Ref | 87.3% | Ref | |
| Coronary artery disease | 48.3% | .02 | 73.6% | < .001 | 89.0% | .001 | |
| Congestive heart failure | 45.7% | .005 | 70.8% | .003 | 88.1% | .03 | |
| White | 53.7% | Ref | 76.9% | Ref | 89.7% | Ref | |
| Japanese | 54.4% | .5 | 77.9% | .09 | 90.5% | .008 | |
| Chinese | 51.1% | .004 | 75.8% | .046 | 89.9% | .7 | |
| Filipino | 42.1% | < .001 | 69.5% | < .001 | 87.4% | < .001 | |
| Native Hawaiian | 43.1% | < .001 | 68.0% | < .001 | 86.4% | < .001 | |
| Other Pacific Islander | 30.8% | < .001 | 57.0% | < .001 | 82.6% | .005 | |
| Other race | 47.1% | < .001 | 72.2% | < .001 | 88.4% | .004 | |
|
| |||||||
|
Adherence to Anti-hypertensive Medications (N =87,969 observations
for 33,443 patients) |
Age <35 | 24.2% | < .001 | 48.2% | < .001 | 75.7% | < .001 |
| Age 35-49 | 43.0% | < .001 | 71.6% | < .001 | 89.2% | < .001 | |
| Age 50-64 | 59.7% | Ref | 82.0% | < .001 | 92.9% | < .001 | |
| Age 65+ | 64.3% | < .001 | 84.8% | < .001 | 94.5% | < .001 | |
| Female | 56.4% | .002 | 79.3% | < .001 | 91.8% | < .001 | |
| Male | 57.9% | Ref | 80.6% | Ref | 92.6% | Ref | |
| Honolulu | 58.7% | .06 | 81.1% | .008 | 92.7% | .04 | |
| Other regions | 56.5% | Ref | 79.4% | Ref | 92.0% | Ref | |
| High morbidity | 58.7% | .01 | 81.0% | < .001 | 92.9% | < .001 | |
| Low morbidity | 56.5% | Ref | 79.5% | Ref | 91.9% | Ref | |
| Coronary Artery Disease | 64.0% | < .001 | 84.5% | < .001 | 94.5% | < .001 | |
| Congestive Heart Failure | 63.7% | < .001 | 84.3% | < .001 | 94.8% | < .001 | |
| White | 64.9% | Ref | 84.1% | Ref | 93.8% | Ref | |
| Japanese | 64.6% | .7 | 84.7% | .09 | 94.3% | .008 | |
| Chinese | 62.8% | .006 | 83.5% | .1 | 93.8% | .4 | |
| Filipino | 59.2% | < .001 | 82.0% | .006 | 93.0% | .009 | |
| Native Hawaiian | 57.7% | < .001 | 79.5% | < .001 | 92.2% | < .001 | |
| Other Pacific Islander | 46.9% | .001 | 73.8% | < .001 | 89.5% | .01 | |
| Other Race | 62.3% | .02 | 83.1% | .01 | 93.7% | .3 | |
Note.
Adjusted for all other variables in the model and year (not shown).
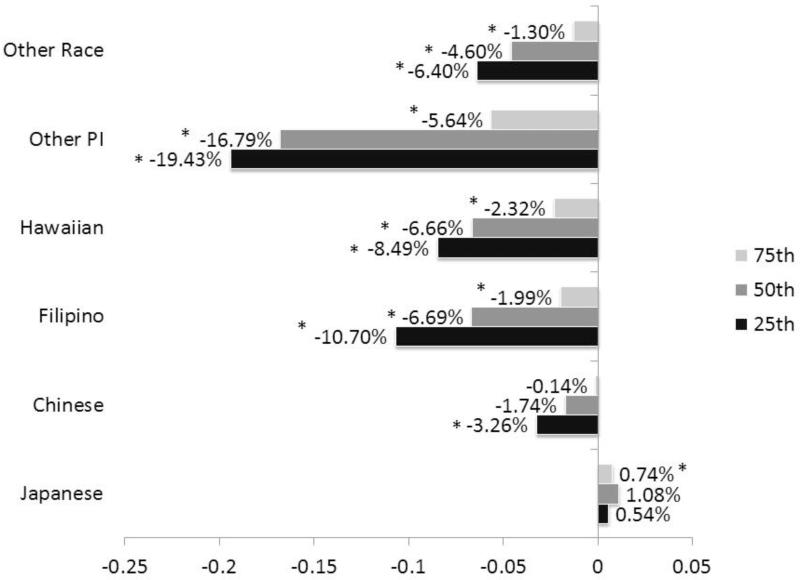
Results for lipid-lowering medications were similar, except the magnitude of the differences between Asian and Pacific Islander sub-groups and Whites was larger and Chinese had lower adherence rates than Whites (Figure 2, Table 2). As with anti-diabetic medications, the largest disparities were found for other Pacific Islanders relative to Whites (−19.4% for 25th, −16.8% for 50th, −5.6% for 75th). Similarly, Filipino (−10.7% for 25th, −6.7% for 50th and −2.3% for 75th) and Native Hawaiian (−8.5% for 25th, −6.7% for 50th, −2.3% for 75th) disparities decreased for higher quantiles. For lipid-lowering medications, “other race” had lower adherence at all quantiles, whereas Chinese had lower adherence than Whites at the 25th quantile. Japanese were significantly more adherent than Whites at the 75th quantile but the magnitude of the difference was small.
Figure 2. Differences in Adherence to Lipid-lowering Medications Relative to Whites for Each Ethnic Group by Quantile (Adjusted).
* = p < .05
Note.
Specific p-values can be found in Table 2. Adjusted for age, sex, living in Honolulu, high morbidity, history of coronary artery disease or congestive heart failure, and year.
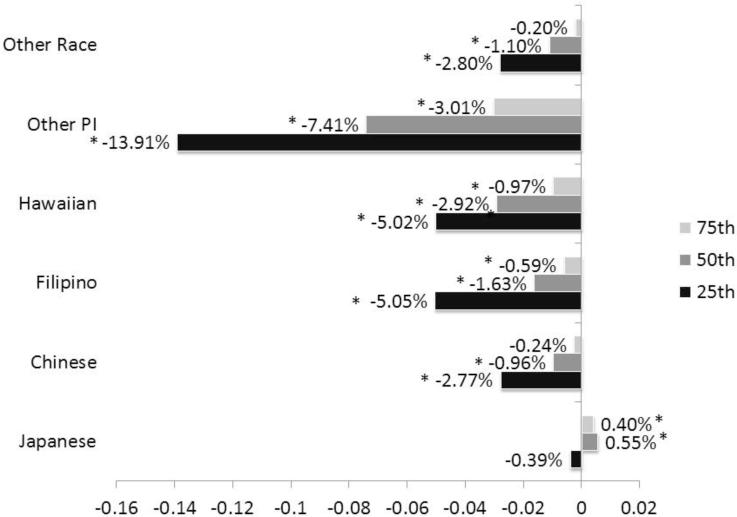
For anti-hypertensive medications we found similar results regarding racial and ethnic disparities in medication adherence (Figure 3, Table 2). Other Pacific Islanders had significantly lower medication adherence than Whites at each quantile (−13.9% at the 25th, −7.4% at the 50th, and −3.0% at the 75th). Once again, Native Hawaiians and Filipinos also had significantly lower adherence than Whites at each quantile, with differences decreasing with increasing quantile. Chinese had significantly lower adherence rates than Whites at the 25th and 50th quantiles; however, the magnitude of the disparity was approximately half the size of that for Filipinos and Native Hawaiians. For antihypertensive medications, Other Race had significantly lower adherence at the 25th and 50th quantiles. Adherence rates of Japanese did not differ significantly from Whites.
Figure 3. Differences in Adherence to Anti-hypertensive Medications Relative to Whites for Each Ethnic Group by Quantile (Adjusted).
* = p < .05
Note.
Specific p-values can be found in Table 2. Adjusted for age, sex, living in Honolulu, high morbidity, history of coronary artery disease or congestive heart failure, and year.
Medication Adherence and Other Patient Characteristics
Table 2 displays adjusted medication adherence rates, rather than differences in rates, for each type of medication at each quantile related to patient characteristics. For instance, for Whites, an individual at the 25th quantile of the distribution would be expected to have 56.9% adherence, an individual at the 50th quantile would be expected to have 79.6% adherence and an individual at the 75th quantile would be expected to have 92.4% adherence. For all 3 types of medications, antidiabetic, lipid-lowering, and anti-hypertenstives, compared to being age 50 to 64, younger age was significantly associated with lower adherence at every quantile; older age was significantly related to higher adherence (Table 2). Large differences of 10% to 30% were consistently observed at the 25th and 50th quantiles, and differences of 4% to 16% at the 75th quantile. Female sex was significantly associated with reduced adherence for all 3 types of medication at each quantile, though differences tended to be lower at the 75th quantile (Table 2).
Living in Honolulu, relative to a rural area, was significantly and positively associated with medication adherence for each type of medication at each quantile, except for the 25th quantile of antihypertensive adherence (p = .06); however, the magnitude of the differences was small, particularly at the 75th quantile, with 91% adherence among residents of Honolulu compared to 90.1% adherence in other regions. High morbidity was positively and significantly related to medication adherence for anti-diabetic and anti-hypertensive medications, but there were no significant difference in adherence to lipid-lowering medications.
Having a history of coronary artery disease or congestive heart failure was significantly associated with increased medication adherence for anti-hypertensive medications at each quantile (Table 2); however, the association between having a history of these conditions and other types of medications varied. Whereas coronary artery disease was not significantly associated with adherence to antidiabetic medications, congestive heart failure was associated with worse adherence to these medications at each quantile. Having a history of congestive heart failure was significantly associated with lower medication adherence to lipid-lowering medications at the 25th and 50th quantiles, whereas having coronary artery disease was positively associated with adherence to lipid-lowering medications at each quantile.
DISCUSSION
Lack of adherence to medications in patients with diabetes has been associated with increased morbidity, mortality, and costs of care.54-57 As medication adherence has been significantly shown to be higher in certain racial and ethnic groups relative to Whites, improving medication adherence in health disparity subgroups might be one means of reducing health inequalities associated with race and ethnicity. This study sought better understanding of the relationship between race and ethnicity and medication adherence for 3 types of medications (anti-diabetic, lipid-lowering, anti-hypertensives) in a predominantly Asian and Pacific Islander population enrolled in a large health plan in Hawaii (N > 43,000).
We found that consistently across all 3 types of medications other Pacific Islanders (meaning non-Native Hawaiian Pacific Islanders) had the lowest medication adherence rates, followed by Native Hawaiians and Filipinos. Chinese had rates similar to Whites and Japanese had medication adherence rates greater than Whites. Our findings that Native Hawaiians and Filipinos had lower adherence than Whites are consistent with those of other studies.41-44
To our knowledge, however, our study is the first to document the large disparities found between other Pacific Islanders and Whites. The other Pacific Islander category includes Polynesians other than Native Hawaiians (eg, Samoan, Tongan), Micronesians (eg, Guamanian, Marshallese, Chuukese), and Melanesians (eg, Fijian). In Hawaii, the largest groups in the other Pacific Islander category are Samoans and Micronesians.
In addition, we discovered that the disparities, while present at each quantile (25th, 50th, 75th), tended to be most pronounced at the 25th quantile. Further research is needed to determine how best to improve medication adherence among this segment of the population with low adherence. The consistency of our findings across all 3 types of medications suggests that interventions should attempt to target all 3 types of medications (anti-diabetic, lipid-lowering, and anti-hypertensives) when addressing adherence issues among Pacific Islander and Filipinos populations.
Age differences in adherence were even greater than differences associated with race and ethnicity. Compared with patients aged 50 to 64, younger age was strongly associated with lower adherence, whereas older age was significantly associated with higher adherence. Differences of 10% to 30% were consistently observed at the 25th and 50th quantiles, and differences of 4% to 16% at the 75th quantile. While the magnitude of the association was not as great, being female was significantly associated with worse medication adherence.
There are several limitations to this study. First, patients were enrolled in a large health plan in Hawaii so results may not be generalizable to uninsured populations, other regions, or other racial and ethnic groups not included in this study. Second, as medication compliance was determined from pharmacy claims, the actual consumption of medication was not assessed and the provision of free drug samples was not captured. Third, race and ethnicity information was only available for 44% of the study population. Even so, due to the large sample size, we were able to find significant racial and ethnic disparities in medication adherence. Fourth, we did not correct for multiple comparisons; however, as most of the p-values were < .001, we would likely retain the same conclusions.
Our study is the first to examine medication adherence using quantile regression analysis in an Asian and Pacific Islander population. Whereas the large sample size undoubtedly contributed to the statistical significance of the findings, the large magnitude of the disparities, particularly for Filipinos, Native Hawaiians, and Other Pacific Islanders at the 25th quantile, suggests that these are meaningful differences that need to be addressed. Further research is needed among other Pacific Islanders to determine which specific ethnic groups had lower adherence.
The fact that the largest disparities were found at the lowest quantile suggests that they may be occurring among the most vulnerable populations with potentially poor access to care. We need to identify effective means of improving adherence, particularly for those with the lowest levels of adherence, including other Pacific Islanders as well as Native Hawaiians and Filipinos in Hawaii. This is particularly important as the Native Hawaiian and other Pacific Islander population was one of the fastest growing ethnic groups between 2000 and 2010. Targeted interventions might also be needed to improve adherence in younger adults and women for all 3 types of medications.
Human Subjects Statement
Our study involved retrospective secondary analysis of an existing dataset. Hence, the only risk to subjects would be related to privacy or confidentiality. Risks to subjects was minimized by conducting the analyses on a de-identified dataset. The University of Hawaii Committee on Human Studies approved this study as exempt.
Acknowledgments
This publication was made possible by Award Numbers P20MD000173 and S21MD999228 from the National Center on Minority Health and Health Disparities. James Davis was partially supported by grants from the National Institute on Minority Health and Health Disparities U54MD007584 and G12MD007601 from the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center on Minority Health and Health Disparities or the National Institutes of Health.
Footnotes
Conflict of Interest Statement
The authors have no financial or other conflicts of interest to disclose.
Contributor Information
Deborah T. Juarez, College of Pharmacy, University of Hawaii, Hilo, HI.
Candace Tan, College of Pharmacy, University of Hawaii, Hilo, HI.
James W. Davis, Department of Native Hawaiian Health, John A. Burns School of Medicine, University of Hawaii, Honolulu, HI.
Marjorie M. Mau, Department of Native Hawaiian Health, John A. Burns School of Medicine, University of Hawaii, Honolulu, HI.
REFERENCES
- 1.World Health Organization . Adherence to Therapies: Evidence for Action. World Health Organization; Geneva: 2003. [Google Scholar]
- 2.Amarenco P, Labreuche J. Lipid management in the prevention of stroke: review and updated meta-analysis of statins for stroke prevention. Lancet Neurol. 2009;8(5):453–463. doi: 10.1016/S1474-4422(09)70058-4. [DOI] [PubMed] [Google Scholar]
- 3.Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366(9493):1267–1278. doi: 10.1016/S0140-6736(05)67394-1. [DOI] [PubMed] [Google Scholar]
- 4.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. Br Med J. 2009;338:b1665. doi: 10.1136/bmj.b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glader EL, Sjölander M, Eriksson M, Lundberg M. Persistent use of secondary preventive drugs declines rapidly during the first 2 years after stroke. Stroke. 2010;41(2):397–401. doi: 10.1161/STROKEAHA.109.566950. [DOI] [PubMed] [Google Scholar]
- 6.Adams AS, Trinacty CM, Zhang F, et al. Medication adherence and racial differences in A1C control. Diabetes Care. 2008;31(5):916–921. doi: 10.2337/dc07-1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adeyemi A, Rascati K, Lawson K, Strassels S. Adherence to oral antidiabetic medications in the pediatric population with type 2 diabetes: a retrospective database analysis. Clin Ther. 2012 Mar;34(3):712–719. doi: 10.1016/j.clinthera.2012.01.028. [DOI] [PubMed] [Google Scholar]
- 8.Bautista R, Graham C, Mukardamwala S. Health disparities in medication adherence between African-Americans and Caucasians with epilepsy. Epilepsy Behav. 2011;22:495–498. doi: 10.1016/j.yebeh.2011.07.032. [DOI] [PubMed] [Google Scholar]
- 9.Blackwell S, Baugh D, Montgomery M, et al. Noncompliance in the use of cardiovascular medications in the Medicare Part D population. Medicare Medicaid Res Rev. 2011;1(4):E1–E27. doi: 10.5600/MMRR.001.04.A05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bosworth HB, Dudley T, Olsen MK, et al. Racial differences in blood pressure control: potential explanatory factors. Am J Med. 2006;119:70.e9–15. doi: 10.1016/j.amjmed.2005.08.019. [DOI] [PubMed] [Google Scholar]
- 11.Charles H, Good CB, Hanusa BH, et al. Racial differences inadherence to cardiac medications. J Natl Med Assoc. 2003;95:17–27. [PMC free article] [PubMed] [Google Scholar]
- 12.Dickson M, Plauschinat CA. Racial differences in medication compliance and healthcare utilization among hypertensive Medicaid recipients: fixed-dose vs free-combination treatment. Ethn Dis. 2008;18(2):204–209. [PubMed] [Google Scholar]
- 13.Duru OK, Gerzoff RB, Selby JV, et al. Identifying risk factors for racial disparities in diabetes outcomes: the Translating Research into Action for Diabetes (TRIAD) Study. Med Care. 2009;47(6):700–706. doi: 10.1097/mlr.0b013e318192609d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gazmararian J, Kripalani S, Miller M, et al. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Intern Med. 2006;21:1215–1221. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gebregziabher M, Lynch CP, Mueller M, et al. Using quantile regression to investigate racial disparities in medication non-adherence. BMC Med Res Method. 2011;11:88–98. doi: 10.1186/1471-2288-11-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gellad WF, Haas JS, Safran DG. Race/ethnicity and nonadherence to prescription medications among seniors: results of a national study. J Gen Intern Med. 2007;22(11):1572–1578. doi: 10.1007/s11606-007-0385-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gerber BS, Cho YI, Arozullah AM, Lee SY. Racial differences in medication adherence: a cross-sectional study of Medicare enrollees. Am J Geriatr Pharmacother. 2010;8(2):136–145. doi: 10.1016/j.amjopharm.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heisler M, Faul JD, Hayward RA, et al. Mechanisms for racial and ethnic disparities in glycemic control in middle-aged and older Americans in the Health and Retirement Study. Arch Intern Med. 2007;167(17):1853–1860. doi: 10.1001/archinte.167.17.1853. [DOI] [PubMed] [Google Scholar]
- 19.Holmes HM, Luo R, Hanlon JT, et al. Ethnic disparities in adherence to antihypertensive medications of Medicare Part D beneficiaries. J Am Geriatr Soc. 2012;60(7):1298–1303. doi: 10.1111/j.1532-5415.2012.04037.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ishisaka D, Jukes T, Romanelli R, et al. Disparities in adherence to and persistence with antihypertensive regimens: an exploratory analysis from a community-based provider network. J Am Soc Hyp. 2012;6(3):201–209. doi: 10.1016/j.jash.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan R, Bhalodkar N, Brown E, et al. Race, ethnicity, and sociocultural characteristics predict noncompliance with lipid-lowering medications. Prev Med. 2004;39:1249–1255. doi: 10.1016/j.ypmed.2004.04.041. [DOI] [PubMed] [Google Scholar]
- 22.Krousel-Wood MA, Munter P, Islam T, et al. Barriers to and determinants of medication adherence in hypertension management: perspective of the cohort study of medication adherence among older adults. Med Clin North Am. 2009;93(3):753–769. doi: 10.1016/j.mcna.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lafata JE, Cerghet M, Dobie E, et al. Measuring adherence and persistence to disease-modifying agents among patients with relapsing remitting multiple sclerosis. J Am Pharm Assoc. 2008;48(6):752–757. doi: 10.1331/JAPhA.2008.07116. [DOI] [PubMed] [Google Scholar]
- 24.Laine C, Newschaffer CJ, Zhang D, et al. Adherence to antiretroviral therapy by pregnant women infected with human immunodeficiency virus: a pharmacy claims-based analysis. Obstet Gynecol. 2000;95(2):167–173. doi: 10.1016/s0029-7844(99)00523-2. [DOI] [PubMed] [Google Scholar]
- 25.Lowry KP, Dudley TK, Oddone EZ, Bosworth HB. Intentional and unintentional nonadherence to antihypertensive medication. Ann Pharmacother. 2005;39:1198–1203. doi: 10.1345/aph.1E594. [DOI] [PubMed] [Google Scholar]
- 26.Opolka JL, Rascati KL, Brown CM, Gibson PJ. Role of ethnicity in predicting antipsychotic medication adherence. Ann Pharmacother. 2003;37:625–630. doi: 10.1345/aph.1C321. [DOI] [PubMed] [Google Scholar]
- 27.Osborn C, Cavanaugh K, White R, et al. Health literacy explains racial disparities in diabetes medication adherence. J Health Commun. 2011;16:268–278. doi: 10.1080/10810730.2011.604388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Poon I, Lal LS, Ford ME, Braun UK. Racial/ethnic disparities in medication use among veterans with hypertension and dementia: a national cohort study. Annals Pharm. 2009;23:185–193. doi: 10.1345/aph.1L368. [DOI] [PubMed] [Google Scholar]
- 29.Rothman RL, Mulvaney S, Elasy TA, et al. Self-management behaviors, racial disparities, and glycemic control among adolescents with type 2 diabetes. Pediatrics. 2008;121:e912. doi: 10.1542/peds.2007-1484. [DOI] [PubMed] [Google Scholar]
- 30.Schectman JM, Bovbjerg VE, Voss JD. Predictors of medication-refill adherence in an indigent rural population. Med Care. 2002;40:1294–1300. doi: 10.1097/00005650-200212000-00016. [DOI] [PubMed] [Google Scholar]
- 31.Shenolikar R, Balkrishnan R, Camacho F, et al. Race and medication adherence in Medicaid enrollees with type-2 diabetes. J Nat Med Associ. 2006;98(7):1071–1077. [PMC free article] [PubMed] [Google Scholar]
- 32.Siegel D, Lopez J, Meier J. Antihypertensive medication adherence in the Department of Veterans Affairs. Am J Med. 2007;120:26–32. doi: 10.1016/j.amjmed.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 33.Thrasher AD, Earp JA, Golin CE, Zimmer CR. Discrimination, distrust, and racial/ethnic disparities in antiretroviral therapy adherence among a national sample of HIV-Infected patients. J Acq Immun Def Synd. 2008;49:84–93. doi: 10.1097/QAI.0b013e3181845589. [DOI] [PubMed] [Google Scholar]
- 34.Traylor A, Schmittdiel J, Uratsu C, et al. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J Gen Intern Med. 2010;25:1172–1177. doi: 10.1007/s11606-010-1424-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Trinacty CM, Adamd AS, Soumerai SB, et al. Racial differences in long-term adherence to oral antidiabetic drug therapy: a longitudinal cohort study. BMC Health Serv Res. 2009;9:24. doi: 10.1186/1472-6963-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van Houtven CH, Voils CI, Oddone EZ, et al. Perceived discrimination and reported delay of pharmacy prescriptions and medical tests. J Gen Intern Med. 2005;20:578–583. doi: 10.1111/j.1525-1497.2005.0123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weng FL, Israni AK, Joffe MM, et al. Race and electronically measured adherence to immunosuppressive medications after deceased donor renal transplantation. J Am Soc Nephrol. 2005;16:1839–1848. doi: 10.1681/ASN.2004121059. [DOI] [PubMed] [Google Scholar]
- 38.Wu C, Erickson S, Piette J, Balkrishnan R. The association of race, comorbid anxiety, and antidepressant adherence among Medicaid enrollees with major depressive disorder. Res Soc Admin Pharm. 2012;8:193–205. doi: 10.1016/j.sapharm.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 39.Ngo-Metzger Q, Sorkin D, Billimek J, et al. The effects of financial pressures on adherence and glucose control among racial/ethnically diverse patients with diabetes. J Gen Intern Med. 2012;27:432–437. doi: 10.1007/s11606-011-1910-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tseng CW, Tierney EF, Gerzoff RB, et al. Race/ethnicity and economic differences in cost-related medication underuse among insured adults with diabetes: the translating research into action for diabetes study. Diabetes Care. 2008;31(2):261–266. doi: 10.2337/dc07-1341. [DOI] [PubMed] [Google Scholar]
- 41.Lee R, Taira DA. Adherence to oral hypoglycemic agents in Hawaii. Prev Chronic Dis. 2005;2(2):1–7. [PMC free article] [PubMed] [Google Scholar]
- 42.Taira DA, Gelber RP, Davis J, et al. Anti-hypertensive adherence and drug class among Asian Pacific Americans. Ethn Health. 2007;12(3):265–281. doi: 10.1080/13557850701234955. [DOI] [PubMed] [Google Scholar]
- 43.Kretzer K, Taira Juarez D, Davis J. Initial Anti-hypertensive prescriptions switching patterns and adherence among insured patients in Hawaii. Hawaii Med J. 2008;67(4):96–100. [PMC free article] [PubMed] [Google Scholar]
- 44.Saito E, Davis J, Mau M, et al. Copayment level and drug switching: findings for type 2 diabetes. Am J Pharm B. 2010;2(6):412–420. [Google Scholar]
- 45.Office of. Management and Budget. Revisions to the standards for the classification of federal data on race and ethnicity. Federal Register. 1997;62:58781–58790. [Google Scholar]
- 46.Ghosh C. A national health agenda for Asian Americans and Pacific Islanders. JAMA. 2010;304(12):1381–1382. doi: 10.1001/jama.2010.1358. [DOI] [PubMed] [Google Scholar]
- 47.Gould WW, Rogers WH. Quantile Regression as an Alternative to Robust Regression. Proceedings of the Statistical Computing Section. American Statistical Association; Alexandria, VA: 1994. [Google Scholar]
- 48.Atella V, Kopinska J. The Impact of Cost Sharing Schemes on Drug Compliance: Evidence Based on Quantile Regression. Tor Vergata University; CEIS: 2012. CEIS Research Paper 247. [DOI] [PubMed] [Google Scholar]
- 49.Clark DO, Von Korff MV, Saunders K, et al. A chronic disease score with empirically derived weights. Med Care. 1995;33:783–795. doi: 10.1097/00005650-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 50.State of Hawaii Department of Health [Accessed September 10, 2012];Hawai’i Behavioral Risk Factor Surveillance System. Available at: http://hawaii.gov/health/statistics/brfss/index.html.
- 51.Choudhry NK, Shrank WH, Levin RL, et al. Measuring concurrent adherence to multiple related medications. Am J Managed Care. 2009;15:457–464. [PMC free article] [PubMed] [Google Scholar]
- 52.Martin BC, Wiley-Exley EK, Richards S, et al. Contrasting measures of adherence with simple drug use, medication switching, and therapeutic duplication. Ann Pharmacother. 2009;43:36–44. doi: 10.1345/aph.1K671. [DOI] [PubMed] [Google Scholar]
- 53.StataCorp . Stata Statistical Software: Release 11. StataCorp LP; College Station, TX: 2009. [Google Scholar]
- 54.Roebuck MC, Liberman JN, Gemmill-Toyama M, Brennan TA. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff. 2011;30:91–99. doi: 10.1377/hlthaff.2009.1087. [DOI] [PubMed] [Google Scholar]
- 55.Lau DT, Nau DP. Oral antihyperglycemic medication nonadherence and subsequent hospitalization among individuals with type 2 diabetes. Diabetes Care. 2004;27(9):2149–1453. doi: 10.2337/diacare.27.9.2149. [DOI] [PubMed] [Google Scholar]
- 56.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43(6):521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 57.DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40:794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]