Abstract
Purpose
This study investigated whether and how trajectories of substance use in adolescence were associated with obesity trajectories in young adulthood. We hypothesized that: (1) exposure to persistent substance use throughout adolescence may heighten obesity risk in young adulthood; and (2) such associations may differ once gender, ethnicity, socioeconomic status, and obesity status in adolescence, are considered.
Methods
The study included 5,141 adolescents from the child sample of the 1979 National Longitudinal Survey of Youth and utilized biennial data across the 12 assessments (1986-2008) to examine trajectories of substance use behaviors (i.e., cigarette smoking, alcohol use, and marijuana use) from ages 12 to 18 and obesity trajectories from ages 20 to 24. Group-based dual trajectory modeling was applied to examine sequential associations of trajectories of each type of substance use behavior with obesity trajectories.
Results
Three distinctive trajectory patterns were respectively identified for cigarette smoking, alcohol use, and marijuana use from ages 12 to 18, as well as for obesity status (BMI ≥ 30) from ages 20 to 24. Taking into account gender, ethnicity, socioeconomic status, and obesity status in adolescence, adolescents with the most problematic smoking trajectory (High-decreasing) were more likely to exhibit a High-obesity trajectory from ages 20 to 24. Also, adolescents with an Increasing marijuana use trajectory were more likely to exhibit an Increased obesity trajectory in young adulthood.
Conclusions
The current study demonstrates that adolescent substance use is associated with subsequent obesity in young adulthood. The associations appear to differ based on type of substance use and patterns of use.
Keywords: adolescence, alcohol use, cigarette smoking, drug use, group-based dual trajectory model, obesity, young adulthood
1. Introduction
Substance use during adolescence contributes to a variety of adverse consequences (e.g., impaired physical heath and psychosocial maladjustment) in adolescence and such negative impacts usually persist throughout subsequent life stages (e.g., Jeynes, 2002; Oesterle et al., 2004). Obesity among adolescents and adults is also a major health concern. Currently, 34% of U.S. adults are obese (Flegal, Carroll, Ogden, & Curtin, 2010). Obesity also is associated with myriad negative physical outcomes, such as cardiovascular problems, diabetes, and hypertension (American Diabetes Association, 2000; Must et al., 1999), as well as poorer psychosocial health (Pearce, Boergers, & Prinstein, 2002; Strauss & Pollack, 2003; Sweeting, Wright, & Minnis, 2005). Extensive research examining risk factors and related consequences of each of these two important public health problems has been separately conducted. In addition to these separate studies, recent research has shifted to examining possible interrelationships between substance use and obesity (e.g., Pasch, Nelson, Lytle, Moe, & Perry, 2008). Substance use may be associated with the development of other detrimental lifestyles such as an unhealthy diet and lack of physical activity, which may heighten the risk of obesity (Pasch, Velazquez, Cane, Moe & Lytle, 2012). For example, smoking, poor food choice, and sedentary activity patterns have been found to be clustered among adolescents (Lytle, Kelder, Perry, & Klepp, 1995); also, adolescent cigarette smoking has been linked to a subsequent increase in body fat (Pasch et al., 2012). However, research on the relationship between different types of substance use and obesity is still limited. In particular, longitudinal studies examining the consequences of adolescent substance use on later obesity status in young adulthood are lacking. It is currently unknown whether certain patterns of substance use behavior in adolescence poses a greater, lower, or insignificant risk to the development of obesity in young adulthood. Thus, a better understanding of the interrelationships of adolescent substance use with subsequent risk of obesity is warranted.
Recently, growing attention has been given to the role of substance use on obesity in adolescence (e.g., Pasch et al., 2008). An association between substance use (i.e., cigarette, alcohol, and marijuana use) and obesity has been reported in cross-sectional studies (e.g., Dhariwal, Rasmussen, & Holstein, 2010; Farhat, Iannotti, & Morton-Simons, 2010; Fonseca, Matos, Guerra, & Pedro, 2009; Leatherdale, Wong, Manske, & Colditz, 2008; Liu et al., 2010). Obese teens were more likely to engage in daily alcohol use than their healthy weight peers (Fonseca et al., 2009). Frequent drinking and smoking as well as marijuana use were significantly associated with obesity among girls, and such relationships were differentiated by younger (age < 15) and older (age ≥ 15) age groups (Farhat et al., 2010). However, cross-sectional studies on associations between substance use and obesity among adults have reported inconsistent findings. Obesity was associated with either lower risk (Simon et al., 2006) or insignificant risk of substance use disorder among adults (Scott, McGee, Wells, & Oakley Browne, 2008). The associations between substance use and obesity among adults may differ by gender or by type of substance. One study (Barry & Petry, 2009) has reported that obesity was associated with alcohol dependence, differing by gender, but was not associated with drug use disorders. Other studies have shown lower obesity prevalence in marijuana users compared to non-users (Le Strat & Le Foll, 2011; Smit & Crespo, 2001; Warren, Frost-Pineda, & Gold, 2005). It has also been reported that alcohol use contributes to obesity risk in different ways (e.g., Wannamethee, Shaper, & Whincup, 2005; Yeomans, 2010). Moderate alcohol intake may be associated with reduced risk of becoming obese, particularly among women, but higher alcohol use (e.g., binge-drinking) may increase obesity risk (Arif & Rohrer, 2005; Tolstrup et al., 2008), particularly in men (Schroder et al., 2007). In general, the major limitation of cross-sectional studies examining substance use and obesity is that baseline weight has not been taken into account (Kvaavik, Tell, & Klepp, 2003). On the other hand, a longitudinal study is more likely to take baseline weight into account and to elucidate the role of substance use on obesity among different genders and ethnicities.
Longitudinal studies examining the association between substance use and obesity over time are limited and reveal mixed findings. A recent longitudinal study that examined two samples of adolescents found that substance use contributed to subsequent body composition; alcohol use predicted decreased BMI and cigarette smoking predicted an increase in body fat percentage 2 years later (Pasch et al., 2012). Another longitudinal study on adolescents (Cooper, Klesges, Robinson, & Zbikowski, 2003) indicated that although smoking initiation predicted an increase in Body Mass Index (BMI) 2 years later, smoking was not predictive of adolescent BMI change at a 3-year follow-up and BMI changes over the 3 years were similar between smokers and non-smokers. Also, the association between weight gain and smoking may differ by ethnicity. One longitudinal study, adjusting for age and baseline body weight, reported that weight gain was similar between smokers and non-smokers among Whites, but was lower in smokers than non-smokers among African Americans (Klesges et al., 1998). Furthermore, a longitudinal study on a cohort of young adults aged 18 to 30 years indicated no relationship between marijuana use and BMI 15 years later (Rodondi, Pletcher, Liu, Hulley, & Sidney, 2006). The limited longitudinal research examining substance use on obesity status suggests that significant associations exist, but inconsistent findings demonstrate a need for additional studies to clarify the underlying mechanisms of these associations.
Prior longitudinal work examining the relationship between substance use and obesity has generally focused on multiple years within one developmental period (adolescence or adulthood), but has neglected the transitional period between adolescence and young adulthood. To date, only two studies have followed adolescents into young adulthood to assess the relationship between substance use and obesity. One study reported an increased risk of overweight status for adolescents who stopped smoking during the transition into adulthood (Kvaavik et al., 2003). Another study reported that adolescent chronic heavy drinkers were more likely to be overweight/obese in early adulthood than non-drinkers (Oesterle et al., 2004). These studies indicate the need to examine the relationship between substance use and obesity across the two critical developmental periods (i.e., from adolescence to young adulthood), a time when adolescents are gaining additional responsibility over their health behaviors and a period that appears to have a long-lasting impact on their adult health outcomes.
The present study seeks to advance prior research by examining the sequential association of substance use behaviors with obesity from adolescence to young adulthood. By focusing on the heterogeneity of trajectories of substance use among adolescents and the ways in which those patterns influence development of obesity across subsequent life stages, this study specifically investigated whether and how trajectories of each type of substance use (i.e., cigarette smoking, alcohol use, marijuana use) from ages 12 to 18 were respectively associated with the development and maintenance of obesity from ages 20 to 24. We hypothesized that: (1) exposure to persistent substance use through adolescence may heighten the risk of developing obesity in young adulthood and (2) such associations may differ when influences of gender, ethnicity, socioeconomic status, and obesity status in adolescence are examined simultaneously.
2. Method
2.1. Participants
The study utilized the subset of the child sample of the 1979 National Longitudinal Survey of Youth (NLSY79; U.S. Department of Labor, 2008). The original NLSY79 sample consisted of 12,686 young men and women who were from 14 to 21 years old in 1979. These youths were surveyed annually from 1979 to 1994 and biennially from 1996 to present. An additional child survey that longitudinally tracks all children born to female NLSY79 respondents was started in 1986. Comprehensive assessments on children's health, abilities, behavior problems, school and social experiences, home environment, and family background have been conducted biennially since 1986. A total of 11,495 children were included by 2008. Data from 12 assessments (1986-2008) were examined in the present study. To ensure there was sufficient data to examine the children's substance use behaviors from ages 12 to 18 and obesity status from ages 20 to 24, this study examined 5,141 participants (2,568 males and 2,573 females) who completed 8 or more waves of surveys from 1986 to 2008 and provided weight, height, and substance use information across assessments. Of the 5,141 participants, 50.1% were female; 41.7% were White, 34.9% African American, 21.6% Hispanic, and 1.8% of other ethnic groups.
2.2. Measures
In addition to demographics, the following measures were examined in the study.
Total family income
Starting in 1994, children aged 15 and older reported their family's total income from all resources during the past year, including full or part-time jobs, temporary or seasonal work, services in the military, a farm, a business, and welfare. Average annual family income from years 1994 to 2008 was computed and categorized as less than 25k, 25k to 50k, 51k to 100k, and over 100k. Average annual family income was used as a proxy measure of socioeconomic status (SES).
Substance use
Children aged 10 and older reported whether they had ever used cigarettes, alcohol, and marijuana at each assessment, and if so, they reported when the most recent use occurred as well as quantity and frequency of use in the past 30 days for each type of substance. The measure regarding quantity and frequency of use included number of cigarettes smoked per day in the past 30 days, number of alcoholic drinks per day in the past 30 days, and days of marijuana use per week in the past 30 days. Due to the low prevalence of substance use in the study sample, particularly the frequency of marijuana use in the past 30 days, the continuous measure of each substance use behavior generally exhibited a skewed distribution, with a high percentage of participants reporting values of zero (i.e., no use). The skewed distribution made the process of model fitting difficult to converge. Consequently, for each type of substance, “ever used the substance in the past year” was used in the statistical analysis to indicate substance use endorsement at each wave of the survey.
Obesity status
Participants self-reported their weight and height at each wave of the survey. Their obesity status was measured using the Body Mass Index (BMI; kg/m2), a standard measure for classifying individuals as obese (Barlow & The Expert Committee, 2007). As recommended by the Centers for Disease Control and Prevention (CDC), the cut-off criteria of obesity are different for adults and children because the distribution of BMI changes is typically an increasing trend over age for children aged 19 or below. As a result, a BMI percentile standardized to specific ages and gender is most appropriate for defining obesity in children, rather than a raw BMI. When participants were age 19 or below, each BMI raw measure was assigned a BMI age- and gender-specific percentile, which corresponds to the location of the BMI on an age- and gender-specific BMI distribution from the CDC 2000 growth charts (Kuczmarski et al., 2000). Adolescents ≤ 19 years with a BMI percentile of 95% or above were considered obese. When participants became adults (i.e., age 20 or older), obesity was defined as having a BMI at or above 30 (BMI ≥ 30).
2.3. Longitudinal measures across ages
The current study utilized data across 12 assessment points of the study (1986- 2008) to examine trajectories of substance use behaviors from ages 12 to 18 and their association with obesity developmental trajectories from ages 20 to 24. Measures of substance use and obesity across the 12 waves were included and then temporally rearranged based on the participant's age at each interview. For instance, a participant's measure on cigarette smoking for age 12 was obtained from a corresponding wave of interviews at which the respondent was age 12.
2.4. Analyses
Group-based dual trajectory modeling (Jones & Nagin, 2007), in conjunction with group-based trajectory modeling (Jones, Nagin, & Roeder, 2001) were applied to examine the association of adolescent substance use with obesity status in young adulthood. First, group-based trajectory modeling was applied to determine the number of distinct trajectory patterns for each type of substance use behavior (i.e., smoking, alcohol drinking, and marijuana use) from ages 12 to 18 and for obesity status (i.e., BMI ≥ 30) from ages 20 to 24. The modeling assumes that there was a mixture of distinctive subgroups within the sample, each exhibiting a distinct growth trajectory (Jones et al., 2001; Muthén, 2004). Two components of statistical functions were jointly estimated in the model. One was a polynomial regression function that estimated the shape of the trajectory over time; the other was a multinomial function that estimated posterior probabilities of trajectory memberships for each individual. Individuals were placed into their most likely trajectory group based upon the highest posterior probability of their trajectory memberships. Because of the relatively limited number of repeated measures across ages (i.e., 4 for substance use and 3 for obesity status), the trajectories across ages were established as a linear function with intercept and slope parameters and were estimated using a logit transformation. The logit model is particularly fitted for accommodating a binary variable (0=no and 1=yes), such as an incident of each type of substance use behavior and obesity status. Model parameters were estimated using the maximum likelihood approach, which utilized all available data for parameter estimation. Individuals with missing values in some time points were still effective cases in the analysis and were not removed by the process of listwise deletion of cases with missing values (Jones et al., 2001). From a series of fitted models with a different number of trajectory groups, the best model was selected based on the Bayesian Information Criterion (BIC; Schwartz, 1978). To ensure an appropriate selection of the optimal model, additional model selection criteria, including the Akaike Information Criterion (AIC; Akaike, 1974) and the posterior probability of being the correct model, computed as exp(BICj-BICmax)/Σjexp(BICj-BICmax) (Kass & Wasserman, 1995; Nagin, 1999; Schwartz, 1978), were also applied. In general, the optimal model should have a reasonably low absolute value of BIC, coupled with considerations of interpretability of distinguishable trajectories. Also, the optimal model is expected to exhibit a reasonably high posterior probability of being the correct model.
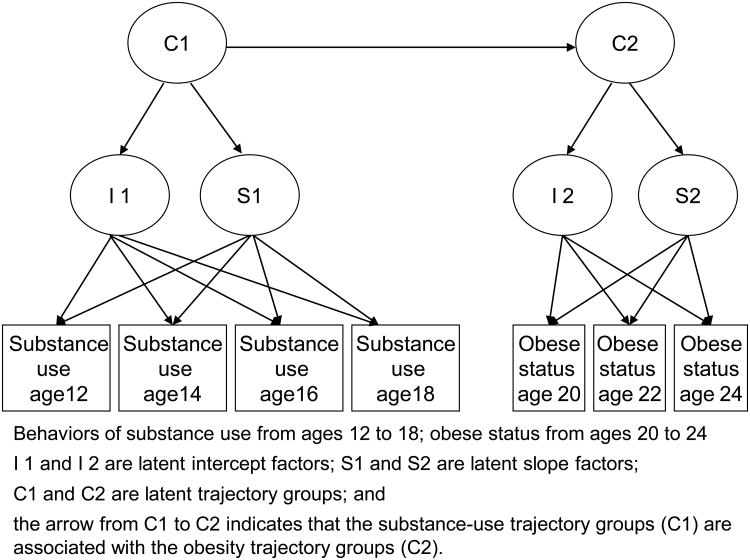
Second, the framework of group-based trajectory modeling was extended by examining trajectories of two outcome measures simultaneously using group-based dual trajectory modeling. Given the optimal number of trajectory groups determined for each outcome measure, group-based dual trajectory modeling links trajectories of each type of substance use behavior with trajectories of obesity status. This is done to assess the transitional impact of each substance use behavior (e.g., smoking) on obesity status across age by estimating the conditional probabilities of membership in the trajectory groups of obesity status, given membership in the trajectory groups of each substance use behavior. Figure 1 shows a diagram of the group-based dual trajectory model applied in this study. The model was conducted using SAS PROC TRAJ (Jones et al., 2001; Jones & Nagin, 2007).
Figure 1. Diagram of group-based dual trajectory model.
Finally, based on the observed relationship between substance use and obesity from the group-based dual trajectory modeling, additional multinomial logistic regression analyses (SAS PROC LOGISTIC) were conducted to further examine whether the observed relationship remained similar when possible confounding effects were considered. The analyses included gender, ethnicity, socioeconomic status (indicated by average annual family income), and adolescent obesity status between the ages of 12 and 18 years as covariates to control for potential confounding effects. Odds ratios of obesity trajectories, given each type of substance use trajectories, were estimated.
3. Results
3.1. Trajectories of adolescent substance use (12 to 18 years) and trajectories of young adult obesity status (20 to 24 years)
A series of group-based trajectory models (from two- to four-group models) were fitted to determine the optimal model for cigarette smoking, alcohol use, and marijuana use, as well as obesity status. Table 1 presents the goodness-of-fit indices of models for each type of substance use and obesity status. For cigarette smoking, alcohol use, marijuana use, and obesity status, the four-trajectory model did not appropriately converge, and the differences on the BIC between the two-trajectory and three-trajectory models showed the three-trajectory model as having a lower absolute BIC value. Similarly, the three-trajectory model was also found to be the best-fit model using the AIC index. Additionally, the three-trajectory model for each substance use behavior and obesity status exhibited a high posterior probability (ranging from 1.0 to 0.82) of being the correct model. Consequently, the three-trajectory model had the best fit with the observed data.
Table 1. Goodness of model fit: Bayesian Information Index (BIC), Akaike Information Index (AIC), and Posterior Probability of being the correct model (PP)by number of trajectory groups.
| Cigarette smoking | Alcohol use | Marijuana use | Obesity status | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||
| Number of trajectory groups | BIC | AIC | PP | BIC | AIC | PP | BIC | AIC | PP | BIC | AIC | PP |
| 2 | -6880.7 | -6864.3 | 0.002 | -7815.1 | -7798.9 | 0.0 | -5380.8 | -5364.5 | 0.08 | -3707.2 | -3691.4 | 0.18 |
| 3 | -6874.2 | -6848.1 | 0.998 | -7803.5 | -7777.4 | 1.0 | -5378.3 | -5352.2 | 0.92 | -3705.7 | -3680.3 | 0.82 |
| 4 | -- | -- | -- | -- | ||||||||
-- No convergence
3.1.1. Cigarette smoking trajectories from ages 12 to 18
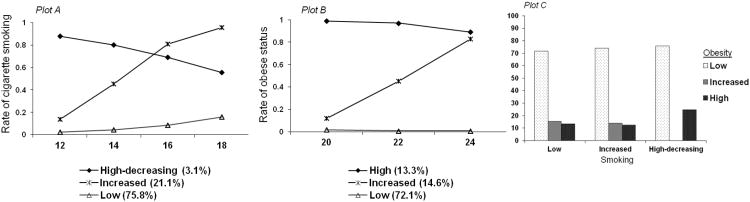
Adolescents exhibited three smoking trajectories (Figure 2A). The majority of adolescents (75.8%) exhibited a low likelihood of cigarette smoking (Low). Another group (21.1%) exhibited a low likelihood of cigarette smoking at age 12, but an increased likelihood of use across adolescence (Increased). A small group of adolescents (3.1%) were characterized as being in a High-decreasing group, indicating a high likelihood of smoking at age 12 with a decreasing rate from ages 12 to 18.
Figure 2. Model A: Distinctive trajectory groups of cigarette smoking from ages 12 to 18 (Plot A) and of obese status from ages 20 to 24 (Plot B); and conditional probability of obesity groups given smoking groups (Plot C).
3.1.2. Alcohol use trajectories from ages 12 to 18
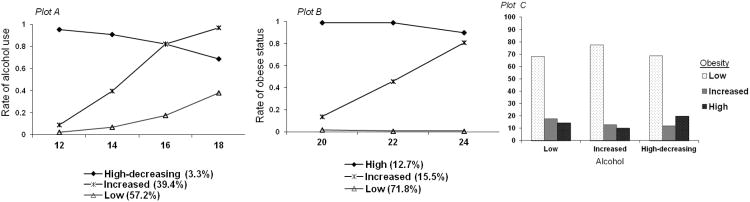
As shown in Figure 3A, the majority of adolescents (57.2%) reported a low likelihood of alcohol use from ages 12 to 18 (Low); 39.4% started with a relatively low likelihood of alcohol use at age 12, but exhibited a significantly increased likelihood of use afterwards (Increased); and another 3.3% of adolescents exhibited a high rate of alcohol use at age 12 with a decreasing rate from ages 12 to 18 (High-decreasing).
Figure 3. Model B: Distinctive trajectory groups of alcohol use from ages 12 to 18 (Plot A) and of obese status from ages 20 to 24 (Plot B); and conditional probability of obesity groups given alcohol groups (Plot C).
3.1.3. Marijuana use trajectories from ages 12 to 18
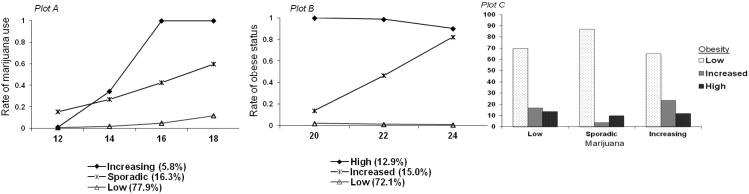
As demonstrated in Figure 4A, the majority of adolescents (77.9%) reported no use or low likelihood of marijuana use from ages 12 to 18 (Low). About 16.3% of adolescents displayed infrequent marijuana use from ages 12 to 18 (Sporadic). A small group (5.8%) of adolescents exhibited an increasing likelihood of marijuana use (Increasing).
Figure 4. Model C: Distinctive trajectory groups of marijuana use from ages 12 to 18 (Plot A) and of obese status from ages 20 to 24 (Plot B); and conditional probability of obesity groups given marijuana groups (Plot C).
3.1.4. Obesity trajectories from ages 20 to 24
Three distinctive obesity trajectories from ages 20 to 24 were identified. The majority of individuals (about 72%) exhibited no or low risk of obesity (Low). Among the rest of individuals, about 15% showed an increasing risk of obesity (Increased), and about 13% displayed a sustained high risk of obesity from ages 20 to 24 (High).
3.2. Joint trajectories of adolescent substance use and young adult obesity status
Group-based dual trajectory models (Models A, B, and C) linked three distinctive trajectory groups for cigarette smoking, alcohol use, and marijuana use from ages 12 to 18, respectively, with the three trajectory groups of obesity status from ages 20 to 24. Plot C in Figures 2, 3, and 4 present conditional probabilities of membership in obesity trajectories, given membership in each one of the respective substance use trajectories. In other words, these conditional probabilities indicate the likelihood of a person becoming obese in young adulthood after engaging in particular substance use behaviors (e.g., alcohol use) in adolescence.
3.2.1. Dual trajectories of cigarette smoking and obesity status
Conditional probabilities for transition to the High obesity trajectory were not significantly different between adolescents in the Low and Increased smoking trajectories. However, in contrast to adolescents in the Low (13.1%) and Increased (12.2%) smoking trajectory groups, adolescents belonging to the High-decreasing smoking trajectory were more likely to belong to the High obesity trajectory group, with 24.4% exhibiting a High obesity trajectory (Figure 2C).
3.2.2. Dual trajectories of alcohol use and obesity status
Adolescents in the High-decreasing alcohol trajectory (19.6%), compared to those in the Low alcohol trajectory (14.2%), were more likely to belong to the High obesity trajectory. Furthermore, adolescents in the Increased alcohol trajectory exhibited the lowest risk of obesity, with 77.5% of these adolescents belonging to the Low obesity trajectory (Figure 3C).
3.2.3. Dual trajectories of marijuana use and obesity status
As shown in Figure 4C, adolescents in the Increasing marijuana trajectory, compared to adolescents in the Low marijuana trajectory, were more likely to belong to the Increased obesity trajectory (23.3% vs. 15.0%). Also, adolescents in the Sporadic marijuana trajectory were more likely to belong to the Low obesity trajectory than those in the Low marijuana trajectory (86.9% vs. 69.6%).
3.3. Odds ratios of young adult obesity trajectories given adolescent substance use trajectories
Table 2 presents estimates of odds ratios of obesity trajectories in young adulthood, given each type of substance use trajectories in adolescence and controlling for gender, ethnicity, adolescent obesity status, and average annual family income. For cigarette smoking (Model A), participants who became obese in adolescence were more likely to belong to the High (OR=30.0; p<0.01) or Increased (OR=4.4; p<0.01) obesity trajectories in young adulthood. In contrast to males, females exhibited a higher likelihood of belonging to the High (OR=1.7; p<0.01) or Increased (OR=1.4; p<0.01) obesity trajectories in young adulthood. African Americans, compared to Whites, also exhibited a higher likelihood of belonging to the High (OR=1.3; p<0.05) or Increased (OR=1.5; p<0.01) obesity trajectories. Adolescents with higher average annual family income were less likely to belong to the High or Increased obesity trajectories.
Table 2.
Odds ratios of young adult obesity trajectories, given adolescent substance use trajectories and controlling for gender, ethnicity, adolescent obesity status, and average annual family income.
| Young adult obesity trajectories (Model A) | Young adult obesity trajectories (Model B) | Young adult obesity trajectories (Model C) | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Odds Ratio (High vs. Low) | Odds Ratio (Increased vs. Low) | Odds Ratio (High vs. Low) | Odds Ratio (Increased vs. Low) | Odds Ratio (High vs. Low) | Odds Ratio (Increased vs. Low) | |
| Adolescent smoking trajectory groups | ||||||
| High-decreasing (vs. Low) | 2.8 ** | -- | -- | -- | -- | -- |
| Increased (vs. Low) | 0.9 | 1.0 | -- | -- | -- | -- |
| Adolescent alcohol trajectory groups | ||||||
| High-decreasing (vs. Low) | -- | -- | 1.4 | 0.5 | -- | -- |
| Increased (vs. Low) | -- | -- | 0.8 | 0.8 * | -- | -- |
| Adolescent marijuana trajectory groups | ||||||
| Increasing (vs. Low) | -- | -- | -- | 1.1 | 1.6 * | |
| Sporadic (vs. Low) | -- | -- | -- | -- | 0.2 ** | 0.1 ** |
| Gender | ||||||
| Females | 1.7 ** | 1.4 ** | 1.7 ** | 1.5 ** | 1.7 ** | 1.5 ** |
| Ethnicity | ||||||
| African-American (vs. White) | 1.3 * | 1.5 ** | 1.3 | 1.4 * | 1.3 | 1.5 ** |
| Hispanic (vs. White) | 1.1 | 1.5 ** | 1.1 | 1.4 * | 1.1 | 1.5 * |
| Other (vs. White) | 1.6 | 1.0 | 1.7 | 1.0 | 1.5 | 0.7 |
| Adolescent obesity | 30.0 ** | 4.4 ** | 31.5 ** | 4.6 ** | 30.3 ** | 4.5 ** |
| Average annual family income | ||||||
| 25 – 50 k (vs. < 25k) | 0.5 ** | 0.5 ** | 0.6 ** | 0.5 ** | 0.6 ** | 0.6 ** |
| 51-100k (vs. < 25k) | 0.5 ** | 0.3 ** | 0.5 ** | 0.3 ** | 0.5 ** | 0.3 ** |
| Over 100k (vs. < 25 k) | 0.4 ** | 0.3 ** | 0.4 ** | 0.3 ** | 0.3 ** | 0.2 ** |
Chi-square test:
p < 0.05;
p < 0.01
After controlling for the effect of adolescent obesity status, gender, ethnicity, and average annual family income, adolescents in the High-decreasing smoking trajectory, compared to those in the Low smoking trajectory were more likely (OR=2.8; p<0.01) to belong to the High obesity trajectory in young adulthood (Model A). However, compared to those in the Low smoking trajectory, adolescents in the Increased smoking trajectory exhibited a similar likelihood of belonging to the High or Increased obesity trajectory in young adulthood.
Associations between alcohol trajectories and obesity trajectories became less strong after controlling for adolescent obesity status, gender, ethnicity, and average annual family income (Model B). Relative to those in the Low alcohol trajectory, adolescents in the Increased alcohol trajectory exhibited a lower risk (OR=0.8; p<0.05) of belonging to the Increased obesity trajectory in young adulthood; however, adolescents in the High-decreasing alcohol trajectory, exhibited non-significant differences in the likelihood of belonging to the High or Increased obesity trajectory in young adulthood.
After controlling for the effects of adolescent obesity status, gender, ethnicity, and average annual family income, adolescents in the Increasing marijuana trajectory, in contrast to those in the Low marijuana trajectory, exhibited a significantly higher risk (OR=1.6; p<0.05) of belonging to the Increased obesity trajectory but exhibited a similar risk of belonging to the High obesity trajectory (Model C). However, those in the Sporadic marijuana trajectory, compared to those in the Low marijuana trajectory, exhibited a significantly lower likelihood of belonging to the High (OR=0.2; p<0.01) or Increased (OR=0.1; p<0.01) obesity trajectory in young adulthood.
4. Discussion
The group-based dual trajectory models developed in this study indicate that adolescent substance use is associated with obesity risk in young adulthood, and the associations differ based on type and patterns of reported substance use. Such associations are still observed after taking into account factors (i.e., gender, ethnicity, adolescent obesity status, and socioeconomic status) that may influence the relationship between adolescent substance use and obesity risk in young adulthood. Adolescents who reported an initial high rate of smoking but decreased over time were more likely to become obese across young adulthood. Also, adolescents who reported increased and more stable marijuana use across adolescence exhibited an increased risk of becoming obese over the course of young adulthood. On the other hand, adolescents who reported initiated and increased alcohol use in adolescence exhibited a lower risk of becoming obese across young adulthood. These interrelationships suggest that adolescent cigarette smoking and marijuana use increase vulnerability to risk of obesity in young adulthood. Because few prospective studies have examined the role of substance use on obesity, especially during the developmental transition from adolescence to adulthood, our findings significantly extend the literature and are likely to inform future empirical and clinical work.
The current findings also revealed that adolescents who belong to the High-decreasing smoking trajectory were at increased obesity risk in young adulthood compared to non-smokers, but those who belong to the Increased smoking trajectory were not at greater risk. One possible explanation is that obese individuals may begin to smoke in an attempt to offset increasing BMI, as prior studies have shown adolescents view smoking as a weight loss coping strategy (Lowry, Galuska, Fulton, Wechsler, & Kann, 2002; Potter, Pederson, Chan, Aubut, & Koval, 2004). However, because smoking is not an effective weight-loss strategy (Chiolero, Faeh, Paccaud, & Cornuz, 2008), adolescents may begin to decrease level of use. The ineffectiveness of cigarette smoking as a method for offsetting increasing BMI or obesity may also explain why belonging to the Increased smoking trajectory had the same risk as belonging to the High and Increased obesity groups, compared to those in the Low smoking trajectory. Thus, it appears that an earlier onset of cigarette smoking, along with a decreased pattern of cigarette smoking, places an adolescent at higher obesity risk in young adulthood.
Significant positive associations between marijuana use and obesity in adolescence have been found on prior research (e.g., Pasch et al., 2008); however, the majority of studies on adults have revealed negative or insignificant associations between marijuana use and BMI/obesity (e.g., Rodondi et al., 2006; Smit & Crespo, 2001). The current study adds to the prior literature by providing empirical evidence demonstrating that the impact of marijuana use on obesity status varies by duration of marijuana use over time. In contrast to no/low marijuana users, adolescents with an increasing and stable pattern of marijuana use were at greater risk of becoming obese in young adulthood; however, adolescents in the Sporadic marijuana trajectory exhibited lower obesity risk in young adulthood. These findings indicate that level and duration of marijuana use has a vital role in determining its influence on obesity risk; sporadic marijuana use over time may come with a lower obesity risk, but a more consistent pattern of marijuana use over time may lead to a tremendous increase of obesity risk. Probable explanations for the findings are that marijuana use may increase metabolism and raise the amount of fat the body burns and, consequently, lower obesity risk (Rajavashisth et al., 2012; Zwillich, Doekel, Hammill, & Weil, 1978). However, this association may become less strong when marijuana use becomes more persistent. Consistent marijuana use over time may be associated with excessive calorie intake (Kirkham, 2005) and may lead to adolescents becoming more vulnerable to engaging in other unhealthy behaviors, including insufficient physical activity, cigarette smoking, alcohol use, and the consumption of more sodas and salty foods, but fewer fruits and vegetables, all of which contribute to increased risk of obesity (Pasch et al., 2012; Rodondi et al., 2006; Smit & Crespo, 2001).
Studies examining associations between alcohol use and obesity among adolescents and adults have had mixed findings (Arif & Rohrer, 2005; Pasch et al., 2008; Pasch et al., 2012; Schroder et al., 2007; Tolstrup et al., 2008). Alcohol drinking has been associated with the excessive consumption of calories, which may result in weight gain (Schroder et al., 2007). However, other studies have shown inconsistent associations between alcohol intake and elevated obesity risk. Heavy alcohol drinking may increase obesity risk, whereas light to moderate alcohol drinking may have a beneficial effect in reducing obesity risk (Arif & Rohrer, 2005). Consistent with prior findings, the current study showed that adolescents in the Increased alcohol trajectories were at lower risk of obesity in young adulthood; however, the relationship between High (or heavy) alcohol use and obesity became less strong after controlling for gender, ethnicity, adolescent obesity status and socioeconomic status. Consequently, level of alcohol use was an important factor that moderated the relationship between alcohol use and obesity.
The findings of the study can inform both future empirical and clinical work. First, the findings demonstrate that substance use and obesity should be perceived as two interrelated health risks and that adolescent substance use behaviors have a long-term impact on physical health. Associations of cigarette smoking and marijuana use in adolescence to obesity in young adulthood are robust even after controlling for other salient factors (i.e., gender, ethnicity, adolescent obesity status, and socioeconomic status). Significant associations between substance use and obesity exist, and future empirical work should examine the underlying processes thatmay explain how substance use influences obesity risk during the transition from adolescence to young adulthood. Furthermore, obesity prevention efforts for adolescents focusing on health-risk behaviors marked by low nutrient/high caloric food consumption and lack of physical activity may also benefit from integrating other behaviors, such as smoking and marijuana use as markers for future obesity risk. The current findings imply that timely interventions targeting substance use, particularly cigarette smoking and marijuana use, in adolescence are likely to enhance prevention of supplementary adverse consequences (e.g., obesity) in young adulthood, in addition to mitigating the harms of substance use in adolescence.
Several limitations need to be considered. First, the group-based dual trajectory model only links two sets of trajectories; thus, the interrelationship of three types (alcohol, smoking, marijuana) of substance use trajectories over time and estimates of their subsequent impact on obesity risk were not assessed. Another technique, such as the parallel process growth mixture model (Wu et al., 2010), may be useful for examining associations of multiple risk behaviors and obesity status simultaneously. Second, the reporting other types of drug use by participants (e.g., cocaine, heroin, or methamphetamine) was incomplete across multiple waves of data collection; therefore, associations between trajectories of these types of drug use in adolescence and later obesity risk constitute an area for future research. Third, although the current study employed data from a large subsample of the NLSY79 child sample, about half of the children assessed in the child survey were not included because there was insufficient information about them across their adolescence and young adulthood. As a result of this, the study sample, in contrast to the group of individuals excluded, consisted of more females (50.1% vs. 48.0%), more minorities (34.9% African Americans and 21.6% Hispanics vs. 21.8% African Americans and 17.3% Hispanics), and more older subjects (24.3 vs. 20.0 years old in 2008). The over-representation ofAfrican Americans and Hispanics may limit the generalizability of findings. Last, self-reported weight and height, compared to a direct measurement, may limit the reliability of the BMI measures in that the prevalence of being obese may be underestimated. Past studies have suggested that females are more likely than males to underreport their weight (Brener, McManus, Galuska, Lowry, & Wechsler, 2005; Sherry, Jefferds, & Grummer-Strawn, 2007). Obese individuals underestimate their weight more than non-obese individuals (Elgar, Roberts, Tudor-Smith & Moore, 2005; Sherry et al., 2007). However, several studies have reported that correlation coefficients between self-reported and direct measurement of BMI are high (Brener et al., 2003; Goodman, Hinden & Khandelwal, 2000; Sherry et al., 2007) and self-reported height and weight are generally reliable and valid among young adults (Kuczmarski, Kuczmarski, & Najjar, 2001). Since direct measurement of BMI is costly and not practically feasible for a large-scale nationwide survey, self-reported data are still a valuable resource for health surveillance. Generally, estimated prevalence of obesity from self-reported data may be considered as a proxy of the lower bound of the actual obesity prevalence.
Despite these limitations, the current study addresses many gaps in the literature. The child sample of the NLSY79 allowed for multiple measurements of health-risk behaviors and physical health outcomes, which enabled a better identification of stable versus emerging problematic behaviors and health status. Furthermore, this sample was followed from adolescence into young adulthood, a transition period that has been understudied. The utilization of group-based dual trajectory modeling allowed for multiple waves of measurement across both adolescence and young adulthood, making it possible to evaluate how certain patterns of substance use are related to particular patterns of obesity risk. This statistical approach demonstrated strong interrelationships between substance use and obesity, revealing thatparticular substance use and patterns of use in adolescence increase the probability of obesity in young adulthood. The differential pathways of substance use to obesity reflect the complex interplay between substance use and obesity. The findings indicate a need for integrated intervention efforts aimed at simultaneously diminishing adverse impacts of substance use and obesity among adolescents as they transition into more autonomous individuals responsible for their health behaviors and outcomes.
Highlights.
Adolescent substance use is related to subsequent obesity in young adulthood.
The High-decreasing smoking trajectory is associated with the High obesity trajectory.
The Increasing marijuana trajectory is associated with the Increased obesity traj ectory.
The associations differ based on type of substance use and patterns of use.
Acknowledgments
Role of Funding Sources: This study is supported by Grant Number R03HD064619 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development and partially supported by the University of California, Los Angeles, Center for Advancing Longitudinal Drug Abuse Research (CALDAR) under Grant P30DA016383 from the National Institute on Drug Abuse (NIDA) and the University of California, Los Angeles, Drug Abuse Research Training Center sponsored by NIDA (5T32DA007272-19). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders or the National Institutes of Health.
Footnotes
Contributors: Dr. David Huang and Dr. Isabella Lanza developed research ideas, conducted literature review, and wrote the manuscript. Dr. David Huang also conducted all statistical analyses and provided interpretations of statistical findings. Dr. Douglas Anglin reviewed and revised the drafts of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of Interest: All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
H. Isabella Lanza, Email: hilanza@ucla.edu.
M. Douglas Anglin, Email: doug_anglin@hotmail.com.
References
- Akaike H. A new look at the statistical model identification. IEEE Transaction on Automatic Control. 1974;19:716–723. [Google Scholar]
- American Diabetes Association. Type 2 diabetes in children and adolescents. Pediatrics. 2000;105:671–680. doi: 10.1542/peds.105.3.671. [DOI] [PubMed] [Google Scholar]
- Arif AA, Rohrer JE. Patterns of alcohol drinking and its association with obesity: Data from the Third National Health and Nutrition Examination Survey, 1988-1994. BMC Public Health. 2005;5:126. doi: 10.1186/1471-2458-5-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow SE The Expert Committee. Expert Committee recommendation regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary. Pediatrics. 2007;120:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- Barry D, Petry NM. Associations between body mass index and substance use disorders differ by gender: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Addictive Behaviors. 2009;34:51–60. doi: 10.1016/j.addbeh.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener ND, McManus T, Galuska DA, Lowry R, Wechsler H. Reliability and validity of self-reported height and weight among high school students. Journal of Adolescent Health. 2003;32:281–287. doi: 10.1016/s1054-139x(02)00708-5. [DOI] [PubMed] [Google Scholar]
- Chiolero A, Faeh D, Paccaud F, Cornuz J. Consequences of smoking for body weight, body fat distribution, and insulin resistance. American Journal of Clinical Nutrition. 2008;87:801–809. doi: 10.1093/ajcn/87.4.801. [DOI] [PubMed] [Google Scholar]
- Cooper TV, Klesges RC, Robinson LA, Zbikowski SM. A prospective evaluation of the relationships between smoking dosage and body mass index in anadolescent, biracial cohort. Addictive Behaviors. 2003;28:501–512. doi: 10.1016/s0306-4603(01)00258-1. [DOI] [PubMed] [Google Scholar]
- Dhariwal M, Rasmussen M, Holstein BE. Body mass index and smoking: Cross-sectional study of a representative sample of adolescents in Denmark. International Journal of Public Health. 2010;55:307–314. doi: 10.1007/s00038-009-0115-x. [DOI] [PubMed] [Google Scholar]
- Elgar FJ, Roberts C, Tudor-Smith C, Moore L. Validity of self-reported heightand weight and predictors of bias in adolescents. Journal of Adolescent Health. 2005;37:371–375. doi: 10.1016/j.jadohealth.2004.07.014. [DOI] [PubMed] [Google Scholar]
- Farhat T, Iannotti RJ, Morton-Simons BG. Overweight, obesity, youth, and health-risk behaviors. American Journal of Preventive Medicine. 2010;38:258–267. doi: 10.1016/j.amepre.2009.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends inobesity among US adults, 1999-2008. Journal of the American Medical Association. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Fonseca H, Matos MG, Guerra A, Pedro JG. Are overweight and obeseadolescents different from their peers? International Journal of Pediatric Obesity. 2009;4:166–174. doi: 10.1080/17477160802464495. [DOI] [PubMed] [Google Scholar]
- Goodman E, Hinden BR, Khandelwal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics. 2000;106:52–58. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- Jeynes WH. The relationship between the consumption of various drugs by adolescents and their academic achievement. American Journal of Drug and Alcohol Abuse. 2002;28(1):15–35. doi: 10.1081/ada-120001279. [DOI] [PubMed] [Google Scholar]
- Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociological Methods and Research. 2007;35(4):542–571. doi: 10.1177/0049124106292364. [DOI] [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods and Research. 2001;29:374–394. [Google Scholar]
- Kass RE, Wasserman L. A reference Bayesian test for nested hypotheses and itsrelationship to the Schwarz criterion. Journal of the American Statistical Association. 1995;90:928–934. [Google Scholar]
- Kirkham TC. Endocannabinoids in the regulation of appetite and body weight. Behavioural Pharmacology. 2005;16:297–313. doi: 10.1097/00008877-200509000-00004. [DOI] [PubMed] [Google Scholar]
- Klesges RC, Ward KD, Ray JW, Cutter G, Jacobs DR, Wagenknecht LE. The prospective relationships between smoking and weight in a young, biracial cohort: The Coronary Artery Risk Development in Young Adults Study. Journal of Consulting and Clinical Psychology. 1998;66:987–993. [PubMed] [Google Scholar]
- Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: Findings from the third National Health and Nutrition Examination Survey, 1988-1994. Journal of the American Dietetic Association. 2001;101:28–34. doi: 10.1016/S0002-8223(01)00008-6. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC Growth Charts: United States advance data from vital and health statistics No 314. National Center for Health Statistics; 2000. [Google Scholar]
- Kvaavik E, Tell GS, Klepp KI. Predictors and tracking of body mass index from adolescence into adulthood: follow-up of 18 to 20 years in the Oslo Youth Study. Archives of Pediatric and Adolescent Medicine. 2003;157:1212–1218. doi: 10.1001/archpedi.157.12.1212. [DOI] [PubMed] [Google Scholar]
- Leatherdale ST, Wong SL, Manske SR, Colditz GA. Susceptibility to smoking and its association with physical activity, BMI, and weight concerns among youth. Nicotine & Tobacco Research. 2008;10:499–505. doi: 10.1080/14622200801902201. [DOI] [PubMed] [Google Scholar]
- Le Strat Y, Le Foll B. Obesity and cannabis use: results from 2 representative national surveys. American Journal of Epidemiology. 2011;174:929–933. doi: 10.1093/aje/kwr200. [DOI] [PubMed] [Google Scholar]
- Liu T, Yen J, Ko C, Huang M, Wang P, Yeh Y, et al. Associations between substance use and body mass index: Moderating effects of sociodemographic characteristics among Taiwanese adolescents. Kaohsiung Journal of Medical Sciences. 2010;26:281–289. doi: 10.1016/S1607-551X(10)70041-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowry R, Galuska DA, Fulton JE, Wechsler H, Kann L. Weight management goals and practices among U.S. high school students: Associations with physical activity, diet, and smoking. Journal of Adolescent Health. 2002;31:133–144. doi: 10.1016/s1054-139x(01)00408-6. [DOI] [PubMed] [Google Scholar]
- Lytle LA, Kelder SH, Perry CL, Klepp KI. Covariance of adolescent health behaviors: The class of 1989 study. Health Education Research. 1995;10(2):133–146. doi: 10.1093/her/10.2.119-a. [DOI] [PubMed] [Google Scholar]
- Must A, Spadano J, Coakley E, Field A, Colditz G, Dietz W. The diseaseburden associated with overweight and obesity. Journal of the American MedicalAssociation. 1999;282:1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- Muthén B. Latent variable analysis: Growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. Handbook of quantitative methodology for thesocial sciences. Newbury Park, CA: Sage Publications; 2004. pp. 345–368. [Google Scholar]
- Nagin DS. Analyzing developmental trajectories: A semiparametric, group-basedapproach. Psychological Methods. 1999;4:139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Oesterle S, Hill KG, Hawkins JD, Guo J, Catalano RF, Abbott RD. Adolescent heavy episodic drinking trajectories and health in young adulthood. Journalof studies on Alcohol. 2004;65:204–212. doi: 10.15288/jsa.2004.65.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasch KE, Nelson MC, Lytle LA, Moe SG, Perry CL. Adoption of risk-related factors through early adolescence: Associations with weight status and implications for causal mechanism. Journal of Adolescent Health. 2008;43(4):387–393. doi: 10.1016/j.jadohealth.2008.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasch KE, Velazquez CE, Cance JD, Moe SG, Lytle LA. Youth substance use and body composition: Does risk in one area predict risk in the other? Journal of Youth and Adolescence. 2012;41:14–26. doi: 10.1007/s10964-011-9706-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce MJ, Boergers J, Prinstein MJ. Adolescent obesity, overt and relational peer victimization, and romantic relationships. Obesity Research. 2002;10:386–393. doi: 10.1038/oby.2002.53. [DOI] [PubMed] [Google Scholar]
- Potter BK, Pederson LL, Chan SS, Aubut JA, Koval JJ. Does a relationshipexist between body weight, concerns about weight, and smoking among adolescents? An integration of the literature with an emphasis on gender. Nicotine & Tobacco Research. 2004;6:397–425. doi: 10.1080/14622200410001696529. [DOI] [PubMed] [Google Scholar]
- Rajavashisth TB, Megda S, Norris KC, Pan D, Sinha SK, Ortega J, Friedman TC. Decreased prevalence of diabetes in marijuana users: Cross-sectional data from the National Health and Nutrition Examination Survey (NHANES) III. BMJ Open. 2012;2:e000494. doi: 10.1136/bmjopen-2011-000494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodondi N, Pletcher MJ, Liu K, Hulley SB, Sidney S. Marijuana use, diet, body mass index, and cardiovascular risk factors (from the CARDIA study) American Journal of Cardiology. 2006;98:478–484. doi: 10.1016/j.amjcard.2006.03.024. [DOI] [PubMed] [Google Scholar]
- Schroder H, Morales-Molina JA, Bermejo S, Barral D, Mandoli ES, Grau M, et al. Relationship of abdominal obesity with alcohol consumption at population scale. European Journal of Nutrition. 2007;46:369–76. doi: 10.1007/s00394-007-0674-7. [DOI] [PubMed] [Google Scholar]
- Schwartz G. Estimating the dimension of a model. The Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Scott KM, McGee MA, Wells E, Oakley Browne MA. Obesity and mental disorders in the adult general population. Journal of Psychosomatic Research. 2008;64:97–105. doi: 10.1016/j.jpsychores.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Sherry B, Jefferds ME, Grummer-Strawn LM. Accuracy of adolescent self-report of height and weight in assessing overweight status. Archives of Pediatrics andAdolescent Medicine. 2007;161(12):1154–1161. doi: 10.1001/archpedi.161.12.1154. [DOI] [PubMed] [Google Scholar]
- Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, et al. Association between obesity and psychiatric disorders in the US adult population. Archives of General Psychiatry. 2006;63:824–830. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smit E, Crespo CJ. Dietary intake and nutritional status of US adult marijuana users: Results from the Third National Health and Nutrition Examination Survey. Public Health Nutrition. 2001;4:781–786. doi: 10.1079/phn2000114. [DOI] [PubMed] [Google Scholar]
- Strauss RS, Pollack HA. Social marginalization of overweight children. Archives of Pediatric Adolescent Medicine. 2003;157:746–752. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- Sweeting H, Wright C, Minnis H. Psychosocial correlates of adolescent obesity, ‘slimming down’ and ‘becoming obese’. Journal of Adolescent Health. 2005;37:409.e9–409.e17. doi: 10.1016/j.jadohealth.2005.01.008. [DOI] [PubMed] [Google Scholar]
- Tolstrup JS, Halkjaer J, Heitmann BL, Tjonneland AM, Overvad K, Sorensen TI, et al. Alcohol drinking frequency in relation to subsequent changes in waist circumference. American Journal of Clinical Nutrition. 2008;87:947–963. doi: 10.1093/ajcn/87.4.957. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Labor, Bureau of Labor Statistics. The NLSY79 Children and Young Adults. 2011 Retrieved May 18, 2011, from http://www.bls.gov/nls/nlsy79ch.htm.
- Wannamethee SG, Shaper AG, Whincup PH. Alcohol and adiposity: effects of quantity and type of drink and time relation with meals. International Journal of Obesity. 2005;29:1436–1444. doi: 10.1038/sj.ijo.0803034. [DOI] [PubMed] [Google Scholar]
- Warren M, Frost-Pineda K, Gold M. Body mass index and marijuana use. Journal of Addictive Diseases. 2005;24:95–100. doi: 10.1300/J069v24n03_08. [DOI] [PubMed] [Google Scholar]
- Wu J, Witkiewitz K, McMahon RJ, Dodge KA Conduct Problems Prevention Research Group. A parallel process growth mixture model of conduct problems and substance use with risky sexual behavior. Drug and Alcohol Dependence. 2010;111:207–214. doi: 10.1016/j.drugalcdep.2010.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeomans MR. Alcohol, appetite and energy balance: Is alcohol intake a risk factor for obesity? Physiology & Behavior. 2010;100:82–89. doi: 10.1016/j.physbeh.2010.01.012. [DOI] [PubMed] [Google Scholar]
- Zwillich CW, Doekel R, Hammill S, Weil JV. The effects of smoked marijuana on metabolism and respiratory control. The American Review of Respiratory Disease. 1978;118:885–891. doi: 10.1164/arrd.1978.118.5.885. [DOI] [PubMed] [Google Scholar]