Abstract
Background and purpose
Stress contributes to headaches, and effective interventions for headaches routinely include relaxation training (RT) to directly reduce negative emotions and arousal. Yet, suppressing negative emotions, particularly anger, appears to augment pain, and experimental studies suggest that expressing anger may reduce pain. Therefore, we developed and tested anger awareness and expression training (AAET) on people with headaches.
Methods
Young adults with headaches (N = 147) were randomized to AAET, RT, or a wait-list control. We assessed affect during sessions, and process and outcome variables at baseline and 4 weeks after treatment.
Results
On process measures, both interventions increased self-efficacy to manage headaches, but only AAET reduced alexithymia and increased emotional processing and assertiveness. Yet, both interventions were equally effective at improving headache outcomes relative to controls.
Conclusions
Enhancing anger awareness and expression may improve chronic headaches, although not more than RT. Researchers should study which patients are most likely to benefit from emotional expression versus emotional reduction approaches to chronic pain.
Keywords: headaches, relaxation, emotional exposure, emotional processing, anger
Headaches, particularly tension and migraine headaches, are common and frequently disabling. It has been estimated that 47% of the population qualify for a headache disorder diagnosis, and at least 3% have chronic headache, defined as occurring at least 15 days per month. Social functioning and work are often impaired, and almost half of people with chronic headache have a mood or anxiety disorder (1).
Stress, Negative Emotions, and Pain
Psychological stress is elevated in many chronic pain syndromes (2). Life stressors, daily hassles, interpersonal conflict, social rejection, and the resultant negative mood exacerbate both acute and chronic pain (3–5). Childhood adversities and post-traumatic stress are elevated among people with migraines (6, 7), the frequency of stressful events is positively correlated with tension headache frequency (8), and laboratory stress triggers tension headaches, especially in those who are depressed (9). The recognition that stress plays a key role in headaches has led to interventions that directly reduce stress-induced negative emotions and physiological arousal. These interventions usually incorporate various relaxation training (RT) strategies such as progressive muscle relaxation, deep or controlled breathing, guided imagery, distraction, and sometimes biofeedback. A substantial and long-standing literature documents the effectiveness of such emotion- and arousal-reduction interventions for headache (10, 11).
More recent literature, however, suggests that chronic stress and its emotional and physiological consequences are driven, in large part, by the failure to adaptively experience and express key emotions. Both theory and empirical research indicate the value of being aware of and experiencing the primary or activating emotions that are naturally elicited by conflictual or stressful experiences. For example, experiential avoidance theory (12) posits that most psychopathology results from avoiding emotionally provocative experiences, and research on emotion regulation demonstrates that suppressing emotions has pathological cognitive, behavioral, and physiological consequences (13). With respect to chronic pain, both the dynamic model of affect (14), and the stress intolerance and pain hypersensitivity model (15) propose that pain is triggered or augmented by the failure to experience, differentiate, and process emotions. Constructs that are linked with emotional inhibition, such as alexithymia, ambivalence over emotional expression, and self-concealment, also are linked to greater pain (16–19).
Anger Suppression, Expression, and Pain
Emotional states such as anxiety, fear, depression, and anger have been studied in relation to chronic pain (20). Anger, in particular, is generated by interpersonal victimization, violation, or rejection. Because the expression of anger is often viewed by families, cultures, and religions as harmful, anger is routinely suppressed or displaced, particularly among girls and women. Thus, although anger is normal and often adaptive, it is routinely conflicted with guilt, shame, and fear; and the resulting suppression of anger appears to contribute to chronic stress and physical symptoms, including pain. Indeed, a series of studies by Burns and colleagues indicates that purposely inducing anger and then experimentally suppressing it decreases pain tolerance in healthy people and increases pain ratings in people with low back pain (21, 22).
But does reversing anger suppression—that is, expressing anger—reduce pain, or increase it? Research on this topic is mixed and appears to depend on the method used to study anger expression. Most cross-sectional, correlational studies report that self-rated trait anger expression (e.g., “anger-out”) is related to greater pain (23). Two prospective studies using daily diary or experience sampling are mixed, with one showing that self-reported daily anger expression predicts less pain in women with fibromyalgia (24), but the other showing that anger expression predicts greater pain (25). On the other hand, some studies indicate that experimentally assigning people to express anger—rather than relying on the natural experience and expression of anger—is pain-reducing. For example, eliciting anger expression during an interview leads to less laboratory pain (26), and assigning people to expressively write about their anger reduces clinical pain (27). Furthermore, swearing increases pain tolerance, especially among those who do not usually swear (28), as does maintaining a bodily posture that expresses power or dominance (29).
With respect to headaches, the roles of anger awareness, suppression, and expression have been examined in several studies. People with migraine or tension headaches have elevated alexithymia (a lack of emotional awareness and expression) (30), and people with tension headaches have higher anger suppression than headache-free controls (31) as do people with mixed headaches, independent of anxiety and depression (32). Women with mixed headaches report greater anger suppression than those with tension headaches (33). Anger suppression is positively related to depression among both migraine sufferers (34) and mixed headache samples (35). In addition, people with tension headaches are more alexithymic and less assertive than controls (36), and the lack of assertion suggests a failure to express anger in an adaptive, socially appropriate manner (37). All of these studies, however, are cross-sectional and correlational, leaving unanswered questions about causality. In contrast, a daily diary study revealed that increased frustration on one day predicted the development of a headache the next day among adolescents (38). We know of only one relevant experimental study, which found that anger provocation in the laboratory led to less expressed anger among people with migraines compared to healthy controls or those with other pain problems (39). Although these results do not directly link the suppression or expression of anger with the frequency or severity of headaches, these studies suggest that people with headaches have, on average, increased anger suppression, or decreased anger awareness and expression.
Although some authors have advocated emotional awareness and expression interventions to help patients with chronic pain disorders, including headaches (40), such interventions have rarely been developed or tested. There is some evidence, however, that expressive writing about stress (written emotional disclosure), has modest benefits for chronic pain conditions such as fibromyalgia and rheumatoid arthritis (41), and an uncontrolled study of emotional exposure therapy demonstrated some benefits for people with fibromyalgia (42). Yet, interventions that facilitate awareness, experiencing, and expression of negative emotions, particularly anger, need to be tested for chronic pain generally and for headaches specifically. Researchers and clinicians, however, may be hesitant to activate anger out of concern that doing so will not help, and may even exacerbate pain, as suggested by two older studies (43, 44). This concern needs to be addressed through additional research.
Goals and Hypotheses
We developed and tested on people with headaches, a brief group-based anger awareness and expression training (AAET) intervention. This intervention seeks to reduce stress by helping people become aware of and accept their anger as normal and adaptive, to experience it subjectively and bodily, and to use the anger to motivate adaptive behavior, particularly assertive communication in stressful relationships. The intervention is brief (3 sessions) and held in groups, in part, because we are interested in efficient protocols that reduce costs and lead to higher uptake or adherence among patients, but also because we hope to demonstrate that emotionally provocative interventions can be conducted much more quickly and directly than is traditionally thought. In addition, we were guided by many studies that we and others have conducted on emotional disclosure for chronic pain and other disorders, and these studies usually involved only two to four, 20-minute sessions. Admittedly, these emotional disclosure studies demonstrate rather weak effects (41), and perhaps even null effects for headaches (45). But we modeled AAET after the emotional disclosure protocol—3 sessions—and anticipated that a therapist’s direct guidance and clear focus on anger awareness and expression, along with the group modeling and support, would improve headache outcomes. We compared the effects of AAET to RT, which we configured similarly (same frequency, duration, and therapists) to control for non-specific factors, and which we viewed as a standard comparator intervention likely to lead to headache improvements, given the extensive documentation of RT as a successful headache management strategy (10, 11, 46, 47). Both of these interventions (AAET and RT) were also compared to a wait-list control condition.
The comparison of AAET to RT is particularly important because these two approaches differ fundamentally in their processes. Comparative intervention studies typically find that the interventions yield comparable outcomes (48), leaving unanswered the question of whether the interventions actually are different. Thus, it is important to test whether the processes of the two interventions differ as theorized. In this study, we hypothesized that AAET would increase arousal and negative mood during intervention sessions relative to RT. We also hypothesized that both interventions would increase headache management self-efficacy, but that only AAET would influence processes that are specific to this intervention: increasing assertiveness, emotional processing, and emotional expression; and decreasing alexithymia. Finally, we tested how the two interventions affected headache-related outcomes 4 weeks after the interventions. We hypothesized that both interventions would surpass a wait-list control condition in headache-related improvement, but we had no hypotheses about how AAET would perform relative to RT.
Methods
Participants
Participants were 147 college students who: a) experienced headaches several times per month or more frequently; b) rated their typical headache as “moderate” or “severe” in intensity; and c) desired to engage in a stress management treatment for chronic headaches. (The latter criterion excluded participants who sought only to obtain course credit but were unmotivated to engage in change processes, which could invalidate a trial.) Participants were 87.8% female and 12.2% male; their mean age was 22.1 years (SD = 6.0); and 39.6% identified themselves as Caucasian, 25.7% as African American, 13.2% as Middle Eastern, 11.1% as Asian/Southeast Asian/Indian, 2.8% Hispanic, 0.7% Native American, 3.5% multiracial, and 3.5% other. The sample reported averaging 10.35 (SD = 7.51) days of headache per month, with a mean severity of 6.29 on a 0 to 10 scale (SD = 1.61). We were not able to classify each participant’s headache type, but 26.7% reported that a physician had diagnosed them with migraine. Thus, the current sample is best described as “mixed” with respect to headache type.
Procedures
The study was approved by the institutional review board and registered with Clinicaltrials.gov (NCT00956969) prior to recruitment. Recruitment ran during 4 academic semesters from September 2009 through March 2011, and post-treatment assessments were completed in May 2011. Participants were recruited based upon their responses to screening questions on an internet-based survey of all psychology students at the start of each semester. Over 2,500 students took the survey; approximately 15% of them met the inclusion criteria and were contacted through email and invited to participate by signing up for the study on-line. The initial visit was held in groups of up to seven students simultaneously, during which the study was described in full, and participants provided written informed consent. Students then completed baseline process and outcome measures on-line.
Prior to recruitment, a computer-based randomization scheme was developed (by someone not involved in running participants), which assigned groups of students to one of the three experimental conditions (in a 1:1:1 ratio) in randomized blocks of 3 or 6 (to ensure approximately equal sample sizes in the conditions). Participants and research assistants were blind to condition assignment until after completion of baseline measures. Students assigned to either of the two intervention conditions had intervention session 1 immediately, and then returned at the same day and time 1 and 2 weeks later for intervention sessions 2 and 3. Intervention participants rated their affect before and after each of the three sessions and returned 6 weeks after baseline (i.e., 4 weeks after session 3) for the post-treatment assessment of process and outcomes measures. Participants assigned to the wait-list control condition were dismissed after completing baseline measures and returned 6 weeks later for the post-treatment assessment (i.e., the same time point as the two interventions conditions).
Both of the interventions were conducted according to manuals developed for this study. Therapists were four female doctoral students in clinical psychology who were trained in and provided both interventions, which controlled for therapist effects. Each of the three sessions for both interventions was 1 hour long and conducted in a group format. In total, there were 13 AAET and 12 RT courses of intervention, and the two interventions had very similar group sizes (M = 3.9 participants per group for AAET and 4.0 for RT). Regular supervision during intervention delivery was conducted by a doctoral clinical psychologist. If participants missed a group session of their intervention, they were allowed to make up the session during the subsequent week by coming to the lab and listening to the audiorecording of their session. (For AAET, three participants listened to the recordings of either or both sessions 2 and 3; and for RT: six participants listened to session 2, three listened to session 3, and one listened to both.)
Experimental Conditions
Anger Awareness and Expression Training (AAET)
In session 1, participants were taught that stress triggers or exacerbates headaches; inhibiting emotions—particularly anger—is a key source of stress; and recognizing, experiencing, and expressing anger is adaptive and can reduce stress and improve headaches. Participants engaged in experiential exercises (speaking, yelling, making angry facial expressions and postures) to help them recognize, experience, and express anger, and they kept a log during the next week of times that they experienced anger. In session 2, participants learned to communicate anger adaptively by identifying stressful interpersonal events in their lives when anger should be experienced, including boundary violations and disagreements; recognizing and voicing their anger; and engaging in role-playing exercises to practice assertive communication. Homework was to practice assertive communication for the next week. Session 3 involved troubleshooting difficulties in assertive communication experienced by participants, continued role-plays, and having participants plan in writing an assertive communication for a particularly difficult interpersonal situation.
Relaxation Training (RT)
In session 1, participants were taught that stress can trigger or exacerbate headaches, particularly by increasing muscle tension and physiological arousal, and that directly decreasing arousal and tension can improve headaches. Participants were taught progressive muscle relaxation and given a CD, which contained this exercise plus the exercises taught in sessions 2 and 3, to guide their daily homework of practicing relaxation. In session 2, the therapist explored any difficulties engaging in progressive muscle relaxation and taught deep breathing relaxation as well as brief applied relaxation exercises (“mini-practices”). Homework was to practice these exercises. Session 3 taught guided imagery relaxation and examined how to incorporate relaxation into daily routines.
Wait-list control
Participants in this condition received no intervention but were invited to request an intervention after completing the post-treatment assessment.
Manipulation Check Measures
Affect valence, arousal, and control
Participants in the two intervention conditions rated three affect dimensions at the beginning and end of each of the three sessions, using a pictorial version of the Self-Assessment Manikin, a stylized figure representing the continuum of these dimensions (49). Affect valence was rated from 1 (positive or pleasant) to 9 (negative or unpleasant), arousal was rated 1 (low) to 9 (high), and control was rated from 1 (low) to 9 (high).
Process Measures
Headache management self-efficacy
The 25-item Headache Management Self-Efficacy Scale (50) assessed participants’ perceived efficacy to prevent or manage their headaches. Items were rated on a 1 to 7 scale and averaged. The scale had acceptable internal consistency in this sample at baseline (α = .71) and post-treatment (α = .77). Test-retest reliability over the 6-week period between baseline and post-treatment was r = .80. (This was calculated in the control group only to provide an estimate of stability unbiased by an intervention.)
Alexithymia
The 20-item Toronto Alexithymia Scale-20 (51) assessed three facets of alexithymia: difficulty identifying feelings, difficulty describing feelings, and externally-oriented thinking. Items were rated from on a 1 to 5 scale and summed. This scale is widely used and well-validated (52). Internal consistency in this sample was acceptable at both baseline (α = .82) and post-treatment (α = .78). Test-retest reliability was r = .87.
Assertiveness
The 30-item Rathus Assertiveness Schedule (53) assessed participants’ perceptions of how assertive they are in a range of situations. Items were rated from 0 (very uncharacteristic) to 6 (very characteristic) and averaged. The scale’s validity has been demonstrated in various studies (53). Internal consistency was good in this sample at both baseline (α = .86) and post-treatment (α = .87). Test-retest reliability was r = .88.
Emotional processing and expression
This was assessed with the two, 4-item Emotional Approach Coping scales (54): emotional processing (active attempts to acknowledge and understand emotions) and emotional expression. Items were rated on a 1 to 4 scale and averaged. These two scales are related to adaptive health outcomes and are less confounded by negative affect than are measures of emotion-focused coping (55). Internal consistency was acceptable: (baseline, α = .82 for both scales; post-treatment, processing α = .84, expression α = .83). Test-retest reliability was r = .59 for processing and r = .69 for expression.
Outcome Measures (Primary and Secondary)
Headache frequency
This was the primary outcome. Participants reported the number of days in the last month that they experienced a headache.
Headache severity and duration
Participants reported how painful their headaches during the past month were, on average, from 0 (no pain at all) to 10 (pain as bad as it can be), and how many hours their headaches lasted, on average.
Headache disability
The 5-item Migraine Disability Assessment Scale (56) assessed the number of days in the last month that headaches affected participant’s social, occupational, and daily functioning; the overall score was the total number of days across items. This measure has good reliability and validity and correlates well with diary ratings and physician ratings of disability (56). In this sample, the scale had acceptable reliability at baseline (α = .72) and post-treatment (α = .75).
Psychological symptoms
The 53-item Brief Symptom Inventory (57) assesses psychological symptoms (e.g., anxiety, depression) over the past 2 weeks. Items were rated on a scale of 0 to 4 and averaged. We analyzed the Global Severity Index (mean of all items), which had excellent reliability at both baseline and post-treatment (α = .97 at both times).
Statistical Analyses
A power analysis indicated that a sample of 120 participants (40 per condition) was needed to have 80% power to detect a small between-groups effect size (d = 0.25 SD), given a design with three groups and two time points, assuming an r = .5 correlation between baseline and post-treatment on the primary outcome, and a 2-tailed α of .05. Given expected attrition, we targeted 50 participants per condition.
Preliminary analyses compared the three conditions on demographics and baseline process and outcome measures using chi-square and analysis of variance (ANOVA) to determine the success of randomization. Attrition analyses compared study completers to those who did not complete the post-treatment assessment. To confirm that the two interventions (AAET and RT) had the expected effects on immediate affect, between-groups t-tests compared the two interventions on change in affect valence, arousal, and control during sessions (calculated as the post-session minus pre-session rating, averaged over the 3 sessions). Subsequent 1-sample t-tests examined whether each affect changed significantly (from zero) within each intervention.
Main analyses compared the 3 conditions on each process and outcome measure using analyses of covariance (ANCOVA), covarying each measure’s baseline value. Significant ANCOVAs were followed by pairwise LSD tests to determine differences among conditions. In addition, within-group (paired) t-tests were conducted to determine whether process and outcome measures changed from baseline to 4-week post-treatment for each condition separately. (An alternative approach is repeated-measures ANOVA, comparing the 3 conditions across 2 times and specifically testing condition x time interactions. We conducted such analyses, and the results were largely redundant with those from ANCOVAs. Thus, for simplicity, we present only the latter.)
All process and two outcome measures were normally distributed at baseline and post-treatment, but headache frequency, duration, and disability were positively skewed. Natural logarithm transformations brought these variables to normality; however, analyses yielded the same pattern of results on the original and transformed variables, so we present data only for the original variables. We also verified the homogeneity of slopes assumption of ANCOVA by predicting each post-treatment measure from condition x baseline value interactions. All but one interaction was non-significant, indicating homogeneous slopes; however, headache management self-efficacy had heterogeneous slopes among conditions, rendering the ANCOVA less reliable (although repeated measures ANOVA yielded the same result for this measure as ANCOVA).
We used intent-to-treat (ITT) analyses of the full randomized sample of 147 participants; missing post-treatment values were replaced by participant’s own baseline values. However, we also repeated the ANCOVAs including only people in RT or AAET who were protocol adherent, as defined below.
Effect sizes (partial eta-squared; η2) are given for the overall ANCOVAs; these effect sizes indicate the proportion of variance in the outcome accounted for by the three conditions, while holding constant baseline scores. We also give a potentially more helpful effect size (ES), which is the standardized difference in change between conditions: Condition 1 (post-treatment minus baseline value) minus Condition 2 (post-treatment minus baseline value) divided by the pooled SD of change scores. Finally, following a standard definition of headache improvement, we categorized each participant as improving (or not) at least 50% from his/her baseline to post-treatment value for each outcome. We present the percent of participants in each condition meeting this improvement criterion and compare the three conditions on those percentages using chi-squares. All analyses used a 2-tailed p-value of .05.
Results
Preliminary Analyses
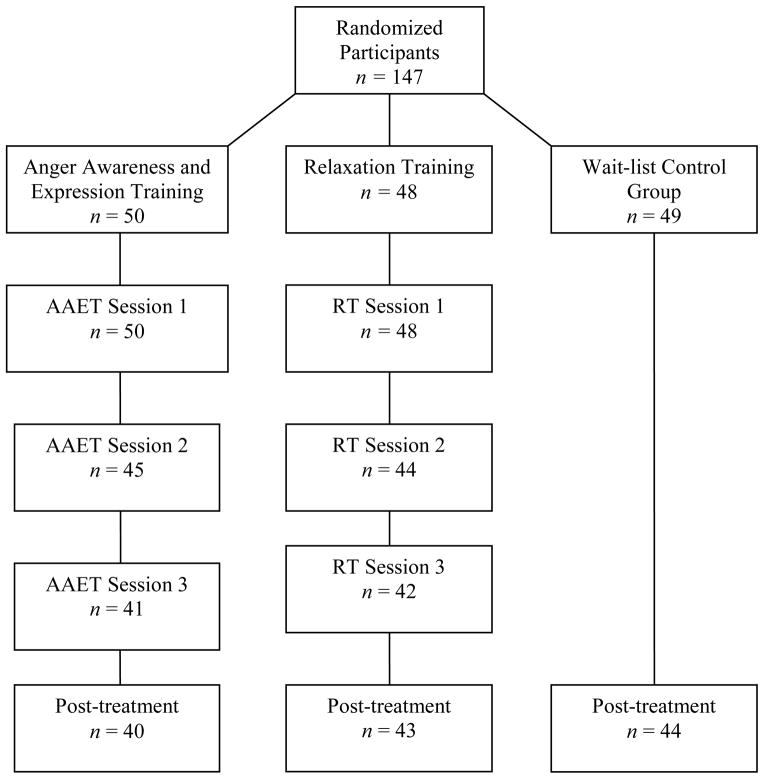
The three conditions did not differ on age, gender, or baseline levels of any process or outcome measures, suggesting that randomization successfully created equivalent groups. Figure 1 depicts participant flow through the study. Of the 147 participants, 20 (13.6%) dropped from the study and did not complete the post-treatment assessment. Completers and non-completers did not differ significantly in demographics or baseline process or outcome measures. Non-completers did not differ significantly (p = .27) among conditions (10 from AAET, 5 from RT, and 5 wait-list controls).
Figure 1.
Flow of participants through the study
Manipulation Check Analyses on Immediate Affect
We next tested whether the two interventions (AAET and RT) differed in their immediate affect reactions (post-session minus pre-session change scores, averaged across the three sessions). The interventions differed on change in negative affect, t(76) = 3.01, p = .004; the RT condition reduced negative affect (M = −1.38, SD = 0.96) more than the AAET condition (M = −0.58, SD = 1.35), although negative affect decreased significantly in both conditions (p < .001 and p = .01, respectively). Similarly, the two interventions differed on change in arousal, t(76) = 4.76, p < .001; RT reduced arousal (M = −1.16, SD = 1.58), whereas AAET increased arousal (M = 0.48, SD = 1.45), and both of these changes differed from zero (p < .001 and p = .045, respectively). Finally, the two interventions did not differ in change in control, t(76) = 0.39, p = .70; both interventions had significant increases in control (RT: M = 0.91, SD = 1.34; AAET: M = 0.80, SD = 1.23, both p < .001).
Analyses of Process Measures
Table 1 presents data on the process measures at baseline and post-treatment for the three conditions, along with baseline-adjusted post-treatment values and within-condition change scores. For headache management self-efficacy, the three conditions differed at post-treatment, F(2, 143) = 30.88, p < .001, partial η2 = .30. Compared with wait-list controls, both AAET (ES = 0.96, p < .001) and RT (ES = 1.27, p < .001) had greater self-efficacy, but the two interventions did not differ from each other (ES = 0.31, p = .23). Both interventions had significant increases in self-efficacy from baseline.
Table 1.
Process Measures for all three Conditions: Baseline, Post-treatment, and Baseline-Adjusted Post-treatment Means
| Process Measure | Anger Awareness and Expression Training (n = 50) | Relaxation Training (n = 48) | Wait-list Control Group (n = 49) | |
|---|---|---|---|---|
| Headache self-efficacy | Baseline M (SD) | 4.16 (0.93) | 3.96 (1.00) | 4.00 (1.03) |
| Post-tx M (SD) | 5.06 (1.02) | 5.16 (0.89) | 3.90 (1.15) | |
| Adj. M (SE) | 5.00 (0.12)a | 5.21 (0.13)a | 3.93 (0.12)b | |
| Change M (SD) | 0.90 (1.08)*** | 1.20 (1.14)*** | −0.10 (0.66) | |
| Alexithymia | Baseline M (SD) | 51.80 (12.23) | 48.96 (11.60) | 50.49 (13.37) |
| Post-tx M (SD) | 47.03 (11.32) | 47.52 (11.36) | 50.79 (12.14) | |
| Adj. M (SE) | 46.09 (1.13)a | 48.53 (1.15)ab | 50.75 (1.14)b | |
| Change M (SD) | −4.78 (10.01)*** | −1.44 (9.49) | 0.30 (6.63) | |
| Assertiveness | Baseline M (SD) | 2.87 (0.80) | 3.19 (0.90) | 3.16 (0.94) |
| Post-tx M (SD) | 3.18 (0.90) | 3.28 (0.85) | 3.09 (1.00) | |
| Adj. M (SE) | 3.34 (0.08)a | 3.18 (0.08)ab | 3.02 (0.08)b | |
| Change M (SD) | 0.30 (0.69)** | 0.09 (0.50) | −0.07 (0.47) | |
| Emotional processing | Baseline M (SD) | 2.93 (0.75) | 2.88 (0.72) | 2.75 (0.76) |
| Post-tx M (SD) | 3.13 (0.78) | 2.84 (0.81) | 2.70 (0.71) | |
| Adj. M (SE) | 3.08 (0.0)a | 2.82 (0.09)b | 2.77 (0.09)b | |
| Change M (SD) | 0.20 (0.67)* | −0.04 (0.69) | −0.05 (0.67) | |
| Emotional expression | Baseline M (SD) | 2.66 (0.64) | 2.69 (0.65) | 2.46 (0.80) |
| Post-tx M (SD) | 2.74 (0.68) | 2.63 (0.67) | 2.45 (0.88) | |
| Adj. M (SE) | 2.70 (0.09) | 2.57 (0.09) | 2.55 (0.09) | |
| Change M (SD) | 0.08 (0.68) | −0.06 (0.61) | −0.01 (0.67) |
Note: Adjusted means were compared across the three conditions with ANCOVAs; see text for statistics. Adjusted means with different superscripts differ significantly in post-hoc tests Change scores are the difference between baseline and post-treatment, and the significance of each change score was determine by a paired t-test.
p < .05;
p < .01;
p < . 001
For the other process measures, the pattern was different. Only AAET led to a significant reduction in alexithymia and a significant increase in assertiveness and emotional processing over time. The other two conditions did not change these processes. Analyses comparing the three conditions found that they differed in alexithymia at post-treatment, F(2, 143) = 4.25, p = .016, partial η2 = .06; AAET had less alexithymia at post-treatment than the controls (ES = −0.41, p = .004), but AAET did not differ from RT (ES = −0.29, p = .13), nor did RT differ from control (ES −0.14, p = .17). The conditions also differed on assertiveness at post-treatment, F(2, 143) = 4.20, p = .017, partial η2 = .06; AAET led to greater assertiveness than control (ES = 0.42, p = .004), but AAET did not differ from RT (ES = 0.25, p = .15), nor did RT differ from control (ES = 0.17, p = .15). Similarly, the three conditions differed on emotional processing, F(2, 143) = 3.67, p = .03, partial η2 = .05; in this case, AAET led to greater emotional processing than both RT (ES = 0.31, p = .04) and control (ES = 0.33, p = .01), but RT did not differ from control (ES = 0.01, p = .67). Emotional expression did not change over time for any of the conditions, nor did the three conditions differ at post-treatment, F(2, 143) = 0.90, p = .41, partial η2 = .01.
Additional analyses of protocol adherent participants included only those from AAET or RT who experienced all three sessions, either in person or by listening to the recording (AAET: n = 41, RT: n = 42). The between-condition differences noted above were unchanged. When only participants who attended all three sessions in person were included (AAET: n = 38, RT: n = 32), the effects were the same, except that AAET now led to marginally greater emotional expression than both RT (p = .08) and control (p = .07), as hypothesized.
Analyses of Outcome Measures
Table 2 presents the outcome data by condition. There was a consistent pattern of findings. On almost all measures, both AAET and RT had better outcomes than controls, but the two interventions did not differ between themselves.
Table 2.
Outcome Measures for all three Conditions: Baseline, Post-treatment, and Baseline-Adjusted Post-treatment Means
| Outcome measure | Anger Awareness and Expression Training (n = 50) | Relaxation Training (n = 48) | Wait-list Control Group (n = 49) | |
|---|---|---|---|---|
| Headache frequency | Baseline M (SD) | 10.58 (8.32) | 9.06 (5.92) | 11.37 (7.98) |
| Post-tx M (SD) | 6.71 (7.23) | 6.42 (6.20) | 9.97 (6.39) | |
| Adj. M (SE) | 6.58 (0.72)a | 7.15 (0.74)a | 9.39 (0.73)b | |
| Change M (SD) | −3.87 (6.87)*** | −2.64 (4.78)*** | −1.40 (6.14) | |
| ≥ 50% improve n (%) | 20 (40.0%)a | 17 (35.4%)a | 8 (16.3%)b | |
| Headache severity | Baseline M (SD) | 6.06 (1.54) | 6.37 (1.63) | 6.45 (1.67) |
| Post-tx M (SD) | 4.64 (2.02) | 4.54 (1.86) | 5.65 (2.07) | |
| Adj. M (SE) | 4.72 (0.27)a | 4.51 (0.28)a | 5.60 (0.27)b | |
| Change M (SD) | −1.42 (2.22)*** | −1.83 (1.97)*** | −0.80 (2.34)* | |
| ≥ 50% improve n (%) | 11 (22.0%) | 10 (20.8%) | 5 (10.2%) | |
| Headache | Baseline M (SD) | 6.39 (9.13) | 5.35 (8.17) | 9.88 (12.02) |
| duration | Post-tx M (SD) | 5.56 (9.58) | 2.46 (3.12) | 12.15 (17.36) |
| Adj. M (SE) | 5.80 (1.60)a | 3.01 (1.64)a | 11.36 (1.63)b | |
| Change M (SD) | −0.84 (10.80) | −2.89 (8.63)* | 2.27 (18.23) | |
| > 50% improve n (%) | 15 (30.0%)ab | 23 (47.9%)a | 11 (22.4%)b | |
| Headache disability | Baseline M (SD) | 2.18 (1.62) | 2.27 (1.99) | 3.35 (3.76) |
| Post-tx M (SD) | 1.24 (1.88) | 1.34 (2.62) | 2.73 (2.46) | |
| Adj. M (SE) | 1.40 (0.30)a | 1.46 (0.31)a | 2.44 (0.31)b | |
| Change M (SD) | −0.94 (1.68)*** | −0.93 (2.18)** | −0.62 (3.71) | |
| ≥ 50% improve n (%) | 27 (54.0%)a | 29 (60.4%)a | 13 (26.5%)b | |
| Psychological symptoms | Baseline M (SD) | 1.06 (0.79) | 1.08 (0.65) | 1.03 (0.79) |
| Post-tx M (SD) | 0.74 (0.71) | 0.64 (0.60) | 0.90 (0.72) | |
| Adj. M (SE) | 0.75 (0.07)a,b | 0.63 (0.07)a | 0.91 (0.07)b | |
| Change M (SD) | −0.31 (0.67)** | −0.44 (0.62)*** | −0.13 (0.48) | |
| ≥ 50% improve n (%) | 18 (36.0%)ab | 21 (43.8%)a | 10 (20.4%)b |
Note: Adjusted means were compared across the three conditions with ANCOVAs.
Adjusted means or improvement frequencies with different superscripts differ significantly. Change scores are the difference between baseline and post-treatment, and the significance of each change score was determine by a paired t-test.
p < .05;
p < .01;
p < . 001
The primary outcome, headache frequency, differed among the three conditions at post-treatment, F(2,143) = 4.17, p = .02, partial η2 = .055. Both AAET (ES = −0.33, p = .007) and RT (ES = −0.18, p = .03) had fewer headaches at post-treatment than wait-list controls, but AAET did not differ from RT (ES = −0.18, p = .58). Both interventions had significant reductions in headache frequency from baseline to post-treatment. Fully 40% of AAET and 35.4% of RT participants achieved at least 50% reduction in headache frequency, both of which were significantly greater than the 16.3% of controls who improved.
Similarly, both interventions significantly reduced pain severity over time, and the three conditions differed in severity at post-treatment, F(2,143) = 4.43, p = .01, partial η2 = .058, with both AAET (ES = −0.18, p = .02) and RT (ES = −0.56, p = .006) having lower severity than controls; but again, AAET did not differ from RT (ES = 0.17, p = .60). Headache disability had a similar outcome pattern; both interventions significantly decreased disability over time, and the three conditions differed at post-treatment, F(2,143) = 3.59, p = .03, partial η2 = .048, with both AAET (ES −0.12, p = .02) and RT (ES = −0.11, p = .03) having less disability than controls, but not differing from each other (ES = 0.00, p = .87). Note that disability improved for 54% of AAET and 60.4% of RT participants, compared to only 26.5% of controls.
Headache duration showed a slightly different pattern. Again, the three conditions differed at post-treatment, F(2,143) = 6.67, p = .002, partial η2 = .085; both AAET (ES = −0.24, p = .02) and RT (ES = −0.43, p < .001) led to shorter headaches than did control, and AAET did not differ from RT (ES = −0.25, p = .22). However, only RT led to a significant reduction in duration from baseline. Regarding psychological symptoms, both interventions led to significant reductions over time, and the three conditions differed on outcomes ANCOVA, F(2,143) = 3.75, p = .03, partial η2= .050. Here, however, the RT condition had less psychological symptoms than the controls (ES = −0.45, p = .007), but AAET did not differ from RT (ES = 0.17, p = .26) or control (ES = −0.25, p = .11).
Finally, analyses including only protocol adherent participants who experienced all three sessions in person or by audio-recording revealed condition differences that were stronger than found in the ITT analyses. For example, the condition effect on headache frequency was large rather than moderate in size (partial η2 = .121 vs. .055 for the ITT sample). All significant condition differences in outcomes reported above remained significant, and AAET now had significantly less psychological symptoms than controls. Analyses on only those participants who attended all three sessions in person were stronger yet (headache frequency partial η2 = .159), with the same pattern of condition differences (both AAET and RT improved more than controls on all outcomes, but did not differ from each other.)
Discussion
This study has four central findings. First, and most important, a brief group-based intervention that enhanced the awareness, experience, and adaptive expression of anger reduced headache-related outcomes (frequency, severity, duration, disability) after 4 weeks, and surpassed a wait-list control. Second, a matched comparison intervention that taught various relaxation skills also was effective in improving headache outcomes—a finding that supports prior research (46, 47). Third, the two interventions differentially influenced processes, including in-session arousal and affect valence, as well as assertiveness, alexithymia, and emotional processing, which supports the proposal that these two interventions have different mechanisms. Fourth, despite these unique processes, the outcomes of the two interventions were very similar.
We conceptualize psychological interventions as falling on a continuum of emotional experiencing and processing (58). At one end are techniques that down-regulate, minimize, or directly attenuate negative emotions and arousal. Relaxation training by progressive muscle relaxation, controlled breathing, and distraction exemplifies this approach, as do techniques such as cognitive reappraisal or reframing, engaging in pleasant activities, and logical problem solving. Such approaches have the greatest empirical support for various chronic pain disorders, including headaches, and are front-line interventions for most pain management behavioral interventions (10, 11, 59). Consistent with this literature, we also found that a 3-session relaxation training protocol led to immediate reductions in arousal during sessions and improvements in headaches and psychological symptoms 4 weeks later.
At the other end of the continuum are techniques that enhance the awareness, experiencing, expression, and processing of negative emotions resulting from life stressors or psychological conflicts. Although emotional exposure and processing interventions have long been documented as effective for anxiety and other emotional disorders, there has been little investigation of such approaches for chronic pain. However, we found that a 3-session protocol that emphasized the detrimental effects of anger suppression and encouraged the awareness, experiencing, and adaptive expression of anger also improved outcomes, both over time and compared to a wait-list control group. This finding is consistent with a growing body of theory and research on the functional nature of emotion and the potential benefits that emotional awareness and expression can have for chronic pain disorders (60). These results also counter the generally negative conclusions of two earlier studies of the effects of anger expression for chronic pain (43, 44). Those studies, however, had substantial limitations or differences from ours; one was an uncontrolled trial that examined only six women with the autoimmune disease, rheumatoid arthritis (47), and the other, a controlled study, included only 9 patients per condition (48). Moreover, both studies actually reported mixed rather than all negative findings, with improvements following the anger expression intervention in depression, although not pain.
Both the AAET and RT interventions influenced processes as hypothesized. First, they had very different effects on immediate affect. Relaxation training clearly decreased arousal and reduced negative mood, whereas AAET increased arousal and led to less reduction of negative mood. These affect changes suggest that these two interventions operated as proposed—RT calms and improves mood immediately, whereas AAET activates emotions, thereby increasing arousal. Regarding broader change processes, both interventions increased participants’ self-efficacy to manage headaches, which was expected, given that both interventions had this goal. But only AAET increased assertiveness and emotional processing, whereas RT did not. Also, only AAET reduced alexithymia, a construct that has both trait and state components and that has been found to decrease in response to emotion-oriented interventions (61, 62). Emotional expression, however, did not change significantly in response to AAET, although it showed the expected trend in analyses of those participants who attended all sessions. The weak effect of AAET on emotional expression might mean that this intervention operates by increasing emotional awareness and processing even in the absence of overt emotional expression. It should be noted, however, that the Emotional Approach Coping scale typically is considered a trait measure, and only one published study has reported increases in emotional processing or expression with an emotion-oriented intervention (63); thus further study of how this measure responds to interventions is needed.
How is it, then, that the two interventions had different processes but generally equivalent health outcomes? The finding that different interventions have comparable outcomes is very common in the psychological treatment literature; this so-called “dodo bird” effect has been discussed extensively (48). We do not think that common explanations for this pattern, such as insufficient sample size, lack of treatment fidelity, therapist effects, or insensitive outcome measures, led to the outcome equivalence of the two interventions in this study. Rather, we think that there are three possible explanations.
First, common factors, such as participating in an intervention, obtaining social support, receiving a plausible rationale for change, learning new skills, and practicing new behaviors might lead to equivalent outcomes. Indeed, in this study, both interventions led to comparable increases in self-efficacy to manage headaches, which is a very robust change mechanism (64). Ruling out many of these common factors would have required a well-designed active control condition, which, for example, might have met in groups for the same amount of time and received basic education or engaged in some novel counter-theoretical intervention.
Second, different change processes can yield equivalent outcomes if there are different routes to the same goal. Perhaps stress is reduced—and headaches improved—by both arousal reduction and emotional processing pathways. Unfortunately, we did not include more sensitive measures of stress responses nor repeat them during the intervention to determine whether there were different, specific processes leading to the same outcome of stress reduction.
Third, nearly half of the participants in each intervention improved clinically, but it is possible that different subgroups of participants responded to each intervention. Such subgroup responses would be diluted in the larger pool, resulting in treatment equivalence. It was likely that only some participants were in need of, open to, and able to benefit from each intervention. Individual differences, or patient factors, are increasingly recognized as influencing differential treatment outcomes (65), and we have proposed that emotional awareness and expression interventions are ideal for those people who have emotional stress or conflict, are able to recognize and value negative emotions, but inhibit them due to internal fears or external contingencies (66). Anecdotally, we observed that some participants found AAET to be empowering and freeing, as they accepted the legitimacy of their anger and began to tell others of their needs or opinions, or declined requests, or no longer cried or were passive in key relationships. Yet, not all participants responded positively; for example, a female hockey player who did not benefit from AAET noted that she “has no trouble being angry,” but that she has difficulty opening up to others or being vulnerable. This suggests that an exclusive focus on anger awareness and expression is not relevant to people who need help expressing the connecting or vulnerable emotions of sadness, guilt, or love. With respect to RT, many participants reported enjoying the exercises, which allowed them to “take a break” from and feel less worried about schoolwork and other stressors. It is not clear what types of people might uniquely benefit from RT, but it is likely that some people do not—perhaps those who have trouble engaging in the exercises, dropping their guard, or whose emotional issues are so substantial that relaxation is insufficient. Future analyses of these data will test baseline moderators of the effects of both interventions as well as examine how changes in the process measures predict changes in outcomes.
Limitations
There are several limitations of the study, in addition to those noted above. First, the use of a college student sample limits generalizability; we do not know the effects of AAET on patients in clinical care, who are typically older and have longstanding, more disabling headaches. We did, however, screen thousands of students to identify our sample, which had a mean headache frequency and pain level that were clinically substantial, and participants expressed interest in stress management to reduce headaches, suggesting that these participants are similar to clinical patients in many ways. Nonetheless, clinic patients may be in greater need of AAET, and their openness and response to it need to be studied. Second, we did not obtain diagnostic information about headaches, so our findings apply to a mixed headache sample. It would have been better to distinguish among types of headaches (e.g., migraine, tension-type, or both) and determine whether the findings apply broadly, or only to certain types. Third, all outcome measures were retrospective self-reports, but it would have been preferable to assess headache variables prospectively, such as with daily diaries. Finally, a longer follow-up period would have also been helpful to ascertain the effects of the treatment over time. We hypothesize that effects of AAET in particular might grow over time, as participants make continued shifts in how they experience and express their emotions and interact more genuinely with others.
Theoretical and Clinical Implications
This study suggests that enhancing the awareness and adaptive expression of anger can be an effective intervention, at least for young adults with headaches. This finding has substantial implications and raises questions for both practice and research. Although the dominant intervention for chronic pain and headaches has been the use of various techniques to attenuate negative emotions and physiological arousal, the current findings suggest that the opposite is also helpful. Purposely reversing the suppression or avoidance of negative emotions, particularly anger, in situations where anger is the appropriate and adaptive emotion, can be helpful rather than harmful. This is consistent with an emerging body of literature that views emotions and emotional processes as informative, motivational, and adaptive; and not just as unfortunate consequences of maladaptive coping, needing “management” or “regulation.” We hope that research will continue to explore the value of emotional processing interventions for headaches and other chronic pain disorders.
This study also raises clinical questions. The current study provides no evidence that an anger awareness and expression approach is to be preferred to an arousal reduction approach like RT, which was equivalent to AAET on outcomes. Furthermore, RT has more attractive immediate effects than does AAET—greater calmness and a more positive mood—which likely will lead to greater participation in and adherence to RT than AAET. We suspect that certain types of patients will be helped preferentially by an anger awareness and expression approach, such as those with unresolved victimization and excessive inhibition of anger, but we currently have no evidence-based indicators or predictors to guide such intervention selection. Clearly research is needed on relevant patient characteristics as treatment moderators. It also may be the case that these seemingly different approaches could be integrated or combined. For example, the transtheoretical model of change suggests that interventions that enhance awareness and motivation should occur before those that create behavioral and environmental change (67). Thus, it is possible that emotional awareness and processing should ideally precede cognitive-behavioral skills training. Future studies should explore whether and how the two approaches might be best combined.
In conclusion, this study demonstrated that an intervention focused on anger awareness and expression is comparable in effectiveness to RT in the treatment of chronic headaches. This means that the range of interventions for headache—and likely other chronic pain problems for which stress plays a significant role—is broader than we might have thought, and we encourage further exploration of such emotional activation, experiencing, expression, and processing approaches to physical symptom disorders.
Acknowledgments
This article is based on the doctoral dissertation of the first author, under the supervision of the second author. The study was supported by a grant from the Blue Cross Blue Shield of Michigan Foundation. Preparation of this article was supported NIH grants AR057808 and AR057047.
Footnotes
Conflict of interest statement: The authors have no conflict of interest to disclose.
References
- 1.Jensen R, Stovner LJ. Epidemiology and comorbidity of headache. Lancet Neurol. 2008;7:354–361. doi: 10.1016/S1474-4422(08)70062-0. [DOI] [PubMed] [Google Scholar]
- 2.Davis DA, Luecken LJ, Zautra AJ. Are reports of childhood abuse related to the experience of chronic pain in adulthood? A meta-analytic review of the literature. Clin J Pain. 2005;5:398–405. doi: 10.1097/01.ajp.0000149795.08746.31. [DOI] [PubMed] [Google Scholar]
- 3.Davis MC, Zautra AJ, Reich JW. Vulnerability to stress among women in chronic pain from fibromyalgia and osteoarthritis. Ann Behav Med. 2001;23:215–226. doi: 10.1207/S15324796ABM2303_9. [DOI] [PubMed] [Google Scholar]
- 4.Eisenberger NI, Jarcho JM, Lieberman MD, Naliboff BD. An experimental study of shared sensitivity to physical pain and social rejection. Pain. 2006;126:132–138. doi: 10.1016/j.pain.2006.06.024. [DOI] [PubMed] [Google Scholar]
- 5.Rhudy JL, Williams AE, McCabe KM, Russell JL, Maynard LJ. Emotional control of nociceptive reactions (ECON): Do affective valence and arousal play a role? Pain. 2008;136:250–261. doi: 10.1016/j.pain.2007.06.031. [DOI] [PubMed] [Google Scholar]
- 6.Sumanen M, Rantala A, Sillanmäki LH, Mattila KJ. Childhood adversities experienced by working-age migraine patients. J Psychosom Res. 2007;62:139–143. doi: 10.1016/j.jpsychores.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Peterlin BL, Tietjen GE, Brandes JL, et al. Posttraumatic stress disorder in migraine. Headache. 2009;49:541–551. doi: 10.1111/j.1526-4610.2009.01368.x. [DOI] [PubMed] [Google Scholar]
- 8.White KS, Farrell AD. Anxiety and psychosocial stress as predictors of headache and abdominal pain in urban early adolescents. J Pediatr Psychol. 2006;31:582–596. doi: 10.1093/jpepsy/jsj050. [DOI] [PubMed] [Google Scholar]
- 9.Janke EA, Holroyd KA, Romanek K. Depression increases onset of tension-type headache following laboratory stress. Pain. 2004;111:230–238. doi: 10.1016/j.pain.2004.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buse DC, Andrasik F. Behavioral medicine for migraine. Neurol Clin. 2009;27:445–465. doi: 10.1016/j.ncl.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 11.Rains JC, Penzien DB, McCrory DC, Gray RN. Behavioral headache treatment: History, review of the empirical literature, and methodological critique. Headache. 2005;45:S91–S108. doi: 10.1111/j.1526-4610.2005.4502003.x. [DOI] [PubMed] [Google Scholar]
- 12.Hayes SC, Wilson KG, Gifford EV, Follette VM, Strosahl K. Experimental avoidance and behavioral disorders: a functional dimensional approach to diagnosis and treatment. J Cons Clin Psychol. 1996;64:1152–1168. doi: 10.1037//0022-006x.64.6.1152. [DOI] [PubMed] [Google Scholar]
- 13.Gross JJ. Emotion regulation: Affective, cognitive, and social consequences. Psychophysiology. 2002;39:281–291. doi: 10.1017/s0048577201393198. [DOI] [PubMed] [Google Scholar]
- 14.Davis MC, Zautra AJ, Smith BW. Chronic pain, stress, and the dynamics of affective differentiation. J Pers. 2004;72:1133–1160. doi: 10.1111/j.1467-6494.2004.00293.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Houdenhove B, Egle U, Luyten P. The role of life stress in fibromyalgia. Curr Rheumatol Rep. 2005;7:365–370. doi: 10.1007/s11926-005-0021-z. [DOI] [PubMed] [Google Scholar]
- 16.Carson JW, Keefe FJ, Lowrey KP, Porter LS, Goli V, Fras AM. Conflict about expressing emotions and chronic low back pain: Associations with pain and anger. J Pain. 2007;8:405–411. doi: 10.1016/j.jpain.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Lumley MA, Neely LC, Burger AJ. The assessment of alexithymia in medical settings: Implications for understanding and treating health problems. J Pers Assess. 2007;89:230–246. doi: 10.1080/00223890701629698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uysal A, Lu Q. Is self-concealment associated with acute and chronic pain? Health Psychol. 2011;30:606–614. doi: 10.1037/a0024287. [DOI] [PubMed] [Google Scholar]
- 19.van Middendorp H, Lumley MA, Jacobs JWG, van Doornen LJP, Bijlsma JWJ, Geenen R. Emotions and emotional approach and avoidance strategies in fibromyalgia. J Psychosom Res. 2008;64:159–167. doi: 10.1016/j.jpsychores.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 20.Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: Scientific advances and future directions. Psychol Bull. 2007;133:581–624. doi: 10.1037/0033-2909.133.4.581. [DOI] [PubMed] [Google Scholar]
- 21.Burns JW, Quartana PJ, Bruehl S. Anger inhibition and pain: Conceptualizations, evidence, and new directions. J Behav Med. 2008;31:259–279. doi: 10.1007/s10865-008-9154-7. [DOI] [PubMed] [Google Scholar]
- 22.Quartana PJ, Bounds S, Yoon KL, Goodin BR, Burns JW. Anger suppression predicts pain, emotional, and cardiovascular responses to the cold pressor. Ann Behav Med. 2010;39:211–221. doi: 10.1007/s12160-010-9182-8. [DOI] [PubMed] [Google Scholar]
- 23.Bruehl S, Burns JW, Chung OY, Chont M. Pain-related effects of trait anger expression: neural substrates and the role of endogenous opioid mechanisms. Neurosci Biobehav Rev. 2009;33:475–491. doi: 10.1016/j.neubiorev.2008.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van Middendorp H, Lumley MA, Moerbeek M, Jacobs JWG, Bijlsma JWJ, Geenen R. Effects of anger and anger regulation styles on pain in daily life of women with fibromyalgia: A diary study. Eur J Pain. 2010;14:176–182. doi: 10.1016/j.ejpain.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 25.Bruehl S, Liu XX, Burns JW, Chont M, Jamison RN. Associations between daily chronic pain intensity, daily anger expression, and trait anger expressiveness: An ecological momentary assessment study. Pain. 2012;153:2352–2358. doi: 10.1016/j.pain.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burns JW, Kubilus A, Bruehl S. Emotion induction moderates effects of anger management style on acute pain sensitivity. Pain. 2003;106:109–118. doi: 10.1016/s0304-3959(03)00298-7. [DOI] [PubMed] [Google Scholar]
- 27.Graham J, Lobel M, Glass P, Lokshina I. Effects of written anger expression in chronic pain patients: making meaning from pain. J Behav Med. 2008;31:201–212. doi: 10.1007/s10865-008-9149-4. [DOI] [PubMed] [Google Scholar]
- 28.Stephens R, Umland C. Swearing as a response to pain: Effect of daily swearing frequency. J Pain. 2011;12:1274–1281. doi: 10.1016/j.jpain.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 29.Bohns VK, Wiltermuth SS. It hurts when I do this (or you do that): Posture and pain tolerance. J Exp Soc Psychol. 2012;48:341–345. [Google Scholar]
- 30.Wise TN, Mann LS, Jani N, Jani S. Illness beliefs and alexithymia in headache patients. Headache. 1994;34:362–365. doi: 10.1111/j.1526-4610.1994.hed3406362.x. [DOI] [PubMed] [Google Scholar]
- 31.Hatch JP, Schoenfeld LS, Boutros NN, Seleshi E, Moore PJ, Cyr-Provost M. Anger and hostility in tension-type headache. Headache. 1991;31:302–304. doi: 10.1111/j.1526-4610.1991.hed3105302.x. [DOI] [PubMed] [Google Scholar]
- 32.Nicholson RA, Gramling EG, Ong JC, Buenevar L. Differences in anger expression between individuals with and without headache after controlling for depression and anxiety. Headache. 2003;43:651–663. doi: 10.1046/j.1526-4610.2003.03108.x. [DOI] [PubMed] [Google Scholar]
- 33.Venable VL, Carlson CR, Wilson J. The role of anger and depression in recurrent headache. Headache. 2001;41:21–30. doi: 10.1046/j.1526-4610.2001.111006021.x. [DOI] [PubMed] [Google Scholar]
- 34.Materazzo F, Cathcart S, Pritchard D. Anger, depression, and coping interactions in headache activity and adjustment: a controlled study. J Psychosom Res. 2000;49:69–75. doi: 10.1016/s0022-3999(00)00144-6. [DOI] [PubMed] [Google Scholar]
- 35.Tschannen TA, Duckro PN, Margolis RB, Tomazic TJ. The relationship of anger, depression, and perceived disability among headache patients. Headache. 1992;32:501–503. doi: 10.1111/j.1526-4610.1992.hed3210501.x. [DOI] [PubMed] [Google Scholar]
- 36.Yucel B, Kora K, Ozyalcin S, Alacalar N, Ozdemir O, Yucel A. Depression, automatic thoughts, alexithymia, and assertiveness in patients with tension-type headache. Headache. 2002;42:194–199. doi: 10.1046/j.1526-4610.2002.02051.x. [DOI] [PubMed] [Google Scholar]
- 37.Rakos RF. Assertive behavior: Theory, research, and training. London: Routledge Press; 1991. [Google Scholar]
- 38.Massey EK, Garnefski N, Gebhardt WA, Van Der Leeden R. Daily frustration, cognitive coping and coping efficacy in adolescent headache: A daily diary study. Headache. 2009;49:1198–1205. doi: 10.1111/j.1526-4610.2009.01492.x. [DOI] [PubMed] [Google Scholar]
- 39.Grothgar B, Scholz OB. On specific behavior of migraine patients in an anger-provoking situation. Headache. 1987;27:206–210. doi: 10.1111/j.1526-4610.1987.hed2704206.x. [DOI] [PubMed] [Google Scholar]
- 40.Abbass A, Lovas D, Purdy A. Direct diagnosis and management of emotional factors in chronic headache patients. Cephalalgia. 2008;28:1305–1314. doi: 10.1111/j.1468-2982.2008.01680.x. [DOI] [PubMed] [Google Scholar]
- 41.Lumley MA, Sklar ER, Carty JN. Emotional disclosure interventions for chronic pain: From the laboratory to the clinic. Translational Behav Med. 2012;2:73–81. doi: 10.1007/s13142-011-0085-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lumley MA, Cohen JL, Stout RL, Neely LC, Sander LM, Burger AJ. An emotional exposure-based treatment of traumatic stress for people with chronic pain: Preliminary results for fibromyalgia syndrome. Psychother. 2008;45:165–172. doi: 10.1037/0033-3204.45.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beutler LE, Daldrup RJ, Engle D, Oro’-Beutler ME, Meredith K, Boyer JT. Effects of therapeutically induced affect arousal on depressive symptoms, pain and beta-endorphins among rheumatoid arthritis patients. Pain. 1987;29:325–334. doi: 10.1016/0304-3959(87)90047-9. [DOI] [PubMed] [Google Scholar]
- 44.Beutler LE, Daldrup R, Engle D, Guest P, Corbishley A, Meredith KE. Family dynamics and emotional expression among patients with chronic pain and depression. Pain. 1988;32:65–72. doi: 10.1016/0304-3959(88)90024-3. [DOI] [PubMed] [Google Scholar]
- 45.D’Souza PJ, Lumley MA, Kraft C, Dooley J. Relaxation training and written emotional disclosure for tension or migraine headaches: A randomized, controlled trial. Ann Behav Med. 2008;36:21–32. doi: 10.1007/s12160-008-9046-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Blanchard EB. Behavioral therapies in the treatment of headache. Headache Q. 1993;4:53–56. [Google Scholar]
- 47.Duckro PN, Cantwell-Simmons E. A review of studies evaluating biofeedback and relaxation training in the management of pediatric headache. Headache. 1989;29:428–433. doi: 10.1111/j.1526-4610.1989.hed2907428.x. [DOI] [PubMed] [Google Scholar]
- 48.Lambert MJ, Ogles BM. The efficacy and effectiveness of psychotherapy. In: Lambert MJ, editor. Handbook of psychotherapy and behavior change. 5. New York: Wiley; 2004. pp. 139–193. [Google Scholar]
- 49.Bradley MM, Lang PJ. Measuring emotion: The self-assessment manikin and the semantic differential. J Behav Ther Exp Psychiatry. 1994;25:49–59. doi: 10.1016/0005-7916(94)90063-9. [DOI] [PubMed] [Google Scholar]
- 50.French DJ, Holroyd KA, Pinell C, Malinoski PT, O’Donell F, Hill KR. Perceived self-efficacy and headache-related disability. Headache. 2000;40:647–656. doi: 10.1046/j.1526-4610.2000.040008647.x. [DOI] [PubMed] [Google Scholar]
- 51.Bagby RM, Parker JD, Taylor GJ. The twenty-item Toronto Alexithymia Scale--I. Item selection and cross-validation of the factor structure. J Psychosom Res. 1994;38:23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]
- 52.Taylor GJ, Bagby RM, Parker JDA. Disorders of affect regulation: Alexithymia in medical and psychiatric illness. New York, NY: Cambridge University Press; 1997. [Google Scholar]
- 53.Rathus SA. A 30-item schedule for assessing assertive behavior. Behav Ther. 1973;4:398–406. [Google Scholar]
- 54.Stanton AL, Kirk SB, Cameron CL, Danoff-Burg S. Coping through emotional approach: scale construction and validation. J Pers Soc Psychol. 2000;78:1150–1169. doi: 10.1037//0022-3514.78.6.1150. [DOI] [PubMed] [Google Scholar]
- 55.Austenfeld JL, Stanton AL. Coping through emotional approach: A new look at emotion, coping, and health-related outcomes. J Personality. 2004;72:1336–1364. doi: 10.1111/j.1467-6494.2004.00299.x. [DOI] [PubMed] [Google Scholar]
- 56.Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology. 2001;56:S20–S28. doi: 10.1212/wnl.56.suppl_1.s20. [DOI] [PubMed] [Google Scholar]
- 57.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 58.Lumley MA. Beyond cognitive-behavioral therapy for fibromyalgia: Addressing stress by emotional exposure, processing, and resolution. Arthr Res Ther. 2011;13:136–137. doi: 10.1186/ar3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gatchel RJ, Rollings KH. Evidence-informed management of chronic low back pain with cognitive behavioral therapy. Spine J. 2008;8:40–44. doi: 10.1016/j.spinee.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lumley M, Cohen J, Borszcz G, et al. Pain and emotion: a biopsychosocial review of recent research. J Clin Psychol. 2011;67:1–27. doi: 10.1002/jclp.20816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Becker-Stoll F, Gerlinghoff M. The impact of a four-month day treatment programme on alexithymia in eating disorders. Eur Eating Dis Rev. 2004;12:159–163. [Google Scholar]
- 62.Clyne C, Blampied NM. Training in emotion regulation as a treatment for binge eating: A preliminary study. Behav Change. 2004;21:269–281. [Google Scholar]
- 63.Zangi HA, Garratt A, Hagen KB, Stanton AL, Mowinckel P, Finset A. Emotion regulation in patients with rheumatic diseases: validity and responsiveness of the Emotional Approach Coping Scale (EAC) BMC Musculoskeletal Disorders. 2009;10:107. doi: 10.1186/1471-2474-10-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Holroyd KA, Labus JS, Carlson B. Moderation and mediation in the psychological and drug treatment of chronic tension-type headache: the role of disorder severity and psychiatric comorbidity. Pain. 2009;143:213–222. doi: 10.1016/j.pain.2009.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Norcross JC, Wampold BE. What works for whom: Tailoring psychotherapy to the person. J Clin Psychol. 2011;67:127–132. doi: 10.1002/jclp.20764. [DOI] [PubMed] [Google Scholar]
- 66.Lumley M, Tojek T, Macklem D. The effects of written emotional disclosure among repressive and alexithymic people. In: Lepore SJ, Smyth JM, editors. The writing cure: How expressive writing promotes health and emotional well-being. Washington, DC: American Psychological Association; 2002. pp. 75–95. [Google Scholar]
- 67.Norcross JC, Krebs PM, Prochaska JO. Stages of change. J Clin Psychol. 2011;67:143–154. doi: 10.1002/jclp.20758. [DOI] [PubMed] [Google Scholar]