Abstract
Objective
To develop and validate the Weight Control Strategies Scale (WCSS), a self-report instrument to assess use of specific behaviors thought to facilitate weight loss.
Design and Methods
Factor analysis was conducted on 323 overweight and obese adults (mean age=48.7±10.9 years, mean BMI=35.4±4.9 kg/m2, 74% female) enrolled in three different behavioral weight loss trials who completed the WCSS prior to starting treatment. To evaluate construct validity, additional data on dietary intake, physical activity, treatment session attendance, and weight change were obtained from a subsample of participants before and after participation in a 48-week weight loss program.
Results
Principal components analysis with varimax rotation revealed a four component solution for the WCSS, representing the following subscales: Dietary Choices, Self-monitoring Strategies, Physical Activity, and Psychological Coping (a’s from 0.79–0.89). Longitudinal analyses showed that WCSS subscale scores increased during treatment (p’s <0.01). In adjusted models, changes in WCSS total and subscale scores were associated with posttreatment weight loss (p’s <0.01). Additionally, changes in WCSS Dietary Choices and Physical Activity subscales were related to posttreatment changes in total daily kilocalorie consumption (p=0.019) and weekly kilocalorie expenditure through physical activity (p<0.001), respectively.
Conclusions
Findings support the validity and reliability of the WCSS in a weight loss treatment seeking sample.
Behavioral obesity treatments that encourage individuals to lose weight by consuming a low-calorie, low-fat diet and engaging in regular physical activity are successful in achieving clinically important weight losses (1). Dietary recommendations for these programs include consumption of fruits, vegetables, whole grains, lean proteins, and low-fat dairy. Participants are given a daily calorie goal range and instructed to monitor calorie intake to stay within that range (2). These programs also promote regular physical activity in the form of brisk walking or similar exercise for 30–40 minutes per day. Individuals are taught a variety of behavioral techniques to help them change their eating and exercise habits, such as self-monitoring, goal-setting, stimulus control, and problem-solving, as well as cognitive and psychological coping skills (1, 2). While studies have shown that regular self-monitoring of eating and body weight promotes successful weight loss and weight loss maintenance (3–5), there is limited empirical evidence testing the effectiveness of other strategies presented in behavioral weight loss programs.
The need to systematically examine the role of specific behaviors involved in weight control was identified over 30 years ago and led to the development of the Eating Behavior Inventory (EBI) (6). The EBI is comprised of items reflecting behaviors theoretically implicated in weight loss and taught in behavioral weight loss treatment programs at the time the EBI was developed. These items focus primarily on eating patterns such as monitoring food intake, restricting amount and type of food consumed, and regulating the location of eating. Research has supported the validity of the EBI, showing that EBI scores increase during weight loss treatment (7–10) and increases in EBI scores are related to posttreatment weight loss (7, 8, 11, 12).
However, in the years since the EBI was developed, behavioral weight loss treatments have evolved to include additional components - beyond changes in eating behavior - that are thought to facilitate weight loss, such as nutrition education, cognitive and psychological coping skills, and physical activity (13–16). These are aspects of current treatments that are not assessed by the EBI. Further, a recent review examining the utility of the EBI in weight loss trials (17) reported that posttreatment EBI scores have declined over time, suggesting that current behavioral weight loss treatments are having a lesser effect on the specific eating behaviors measured by the EBI compared to earlier studies. The authors assert that this finding may be related to observed changes in the content of behavioral weight loss treatment such that present-day programs do not place as much emphasis on certain behaviors identified by the EBI as did earlier programs.
Given the variety of techniques presented in current behavioral weight loss treatments, it would be helpful to identify the specific behaviors that are most effective in helping individuals to manage their weight. Thus, the purpose of the present investigation was to develop a self-report instrument to assess use of specific behaviors thought to facilitate weight loss, the Weight Control Strategies Scale (WCSS).
METHOD
Scale Development
The objective of the WCSS is to assess how often individuals use strategies commonly associated with weight loss. Based on discussions with experts in the field of obesity treatment and a review of treatment materials (13, 16, 18), we identified four domains of behavior represented in behavioral weight loss programs that we felt should be reflected in this instrument. These domains were: behavioral skills, dietary behaviors, physical activity behaviors, and psychological coping skills. Items were developed within each of these domains to describe specific behaviors and strategies taught in behavioral obesity treatment programs and believed to facilitate weight loss. The initial item pool was large (62 items) because we anticipated that many items would be removed following feedback from expert reviewers.
Components of the WCSS, including the items, instructions, and response format were subject to qualitative and quantitative review by a panel of five experts who were not involved in initial item development. Experts completed a questionnaire in which they rated how relevant each item was to the overall construct of the WCSS from 1 (not at all relevant) to 5 (extremely relevant) and the clarity of the WCSS instructions and response format from 1 (not at all clear) to 5 (extremely clear). Experts also were asked to provide suggestions for modifying existing items and/or adding new items. Generally, WCSS items with a mean relevance rating of 4.0 or above were retained; 5 items that fell below this cutoff (4 items with a mean rating of 3.8 and one item with a mean rating of 3.6) were retained by the investigators because we felt these items were important to test. Reverse-scored items were removed. A total of 48 items were retained as originally written or with some modification based on expert review, 6 new items were added, and slight changes were made to the instructions. Modifications made to the WCSS based on the expert review process resulted in a 54-item measure with 23 items reflecting behavioral skills, 16 items reflecting dietary behaviors, 7 items reflecting physical activity, and 8 items reflecting psychological coping skills. We retained a large number of items to maximize representation of the domains of interest; we anticipated that the scale would be further reduced following factor analysis.
Participants
Data were pooled from 323 overweight and obese men and women enrolled in two National Institutes of Health (NIH)-funded behavioral weight loss treatment trials (19, 20) and one pilot study testing behavioral weight loss treatment in young adults (21) who had complete WCSS data at baseline (i.e., prior to the start of treatment) on the set of items used in the final reduced solution. Across the three trials, a total of 63 participants were excluded from the current study because of incomplete data on the WCSS. The majority of these missing cases (n=59) occurred because we began administering the WCSS mid-way through one of the studies (20), and thus were unable to collect baseline data on the first two cohorts of participants. There were no significant differences between included and excluded participants on age, gender, or baseline body mass index (BMI). More participants included in the current study identified themselves as non-White compared to individuals who were excluded (35% v. 10%, p<0.001).
Eligibility criteria varied slightly across studies. Overall, eligible individuals were 21–65 years old with a BMI between 27–50 kg/m2. Individuals were excluded if they were currently/recently participating in a weight loss program or taking weight loss medication, had lost ≥5% of body weight in the last 6 months, had/were planning to have bariatric surgery for weight loss, reported contraindications to unsupervised physical activity, or reported medical conditions that would affect the safety or efficacy of a weight management program involving changes in diet and physical activity (such as uncontrolled hypertension, a history of coronary heart disease, stroke, peripheral arterial disease, hepatitis B or C, cirrhosis, HIV, type 2 diabetes requiring medical therapy that increases the risk of hypoglycemia, cancer within the last 5 years, or significant psychiatric illness). Women who were pregnant, lactating, less than 6 months postpartum, or planning to become pregnant during the study time frames were not eligible. Each study received institutional review board approval at its site and written informed consent was obtained from all participants.
Participant characteristics for each study are presented in Table 1. Across studies, participants were 48.7 ± 10.9 years with a BMI of 35.4 ± 4.9 kg/m2 and were 74% female, 35% non-White, and 12% Hispanic.
Table 1.
Participant Characteristics at Baseline
| Sample 1 (N=144) | Sample 2 (N= 143) | Sample 3 (N=36) | |
|---|---|---|---|
| Age (years) | 49.8 ± 9.3 | 52.4 ± 8.3 | 29.6 ± 3.9 |
| Baseline BMI (kg/m2) | 36.1 ± 5.5 | 35.1 ± 4.5 | 33.4 ± 3.5 |
| Gender (% female) | 90 | 54 | 86 |
| Race (% non-White) | 66 | 8 | 20 |
| Ethnicity (% Hispanic) | 21 | 1 | 17 |
Values are mean ± SD or %.
Procedure
All participants (N=323) completed the WCSS and a measure of social desirability at baseline; factor analysis of WCSS items was conducted using this sample. To assess the construct validity of the WCSS, participants in Sample 1 (19) provided data on dietary intake, physical activity, and weight before and after a 48-week weight loss program; in addition, posttreatment WCSS and treatment session attendance data were collected on this sample of participants. The study design and weight loss treatment conditions in that study have been previously reported (19). Briefly, participants were randomly assigned to receive 48 weeks of group-based behavioral weight loss treatment (BWL), 48 weeks of Weight Watchers (WW), or a combined approach that included 12 weeks of BWL followed by 36 weeks of WW. All treatments promoted weight loss through a moderately reduced calorie low-fat diet and regular physical activity, combined with behavioral skills.
Measures
The following measures were obtained at baseline (prior to the beginning of treatment) from all participants.
Demographic Information
Participants self-reported age, gender, race, and ethnicity.
Social Desirability
To assess the response bias of social desirability, the 12-item Marlowe-Crowne Social Desirability Scale (MCSDS) Short Form (22) was used. Responses were made using true/false format with higher scores indicating more socially desirable responding. Prior studies have shown this short form to be valid and reliable (22, 23).
Height and Weight
Height and weight were measured in light street clothing with no shoes. Height was measured using a wall-mounted stadiometer; weight was measured using a calibrated scale. Body mass index was calculated as kg/m2. For participants in Sample 1, weight also was measured at the end of a 48-week weight loss program.
To evaluate the construct validity of the WCSS, the following measures were obtained at baseline and end of treatment (48 weeks) for participants in Sample 1.
Dietary Intake
Total daily energy intake (kcals) and percent of kcals from fat were assessed using The Block Food Frequency Questionnaire (FFQ) (24) modified for a 3-month time-frame. The FFQ has been shown to correlate with 4-day diet records (25) and 24-hour dietary recalls (26).
Physical Activity
Physical activity was measured using the Paffenbarger Activity Questionnaire (PAQ) (27). The PAQ estimates calories expended in leisure activity based on number of stairs climbed and blocks walked as well as amount of time spent doing light (5 kcal/min), medium (7.5 kcal/min), and high (10 kcal/min) intensity activity. Previous studies have demonstrated associations between PAQ and weight change (28, 29).
Attendance
Attendance at treatment meetings was recorded by program staff and percent of total meetings attended was computed.
Statistical Analyses
Exploratory dimensional analyses (EDA) were conducted to examine the structure of the WCSS using principal components analysis (PCA) with a varimax rotation (30). Internal consistency of the resulting WCSS subscales and total score was evaluated using Cronbach’s alpha coefficient (31). Pearson correlations were used to evaluate whether WCSS scores were associated with socially desirable responding by examining the relationship between the MCSDS Short Form and the WCSS subscales and total scale scores.
A series of analyses were conducted to investigate the construct validity of the WCSS with a subsample of participants (Sample 1). Pearson correlation coefficients were used to examine the associations between WCSS subscales and validated measures of dietary intake and physical activity at baseline. Repeated measures analyses of covariance (ANCOVA) were used to assess change in WCSS subscale scores from baseline to posttreatment, controlling for treatment group. Partial correlations controlling for treatment group evaluated the relationship between change in WCSS subscale scores and treatment session attendance. To examine whether change in WCSS total score was related to weight loss, a hierarchical linear regression was conducted with posttreatment weight change (i.e., posttreatment – baseline) as the dependent variable; treatment group, baseline weight, and baseline WCSS total score entered in the first step; treatment attendance entered in the second step; and change in WCSS total score from baseline to posttreatment (48 weeks) in the third step. Additionally, we examined whether changes in the individual WCSS subscales were associated with posttreatment weight loss above and beyond the covariates noted above, with a parallel series of four separate hierarchical regressions using each baseline WCSS subscale score in the first step and posttreatment change (posttreatment – baseline) in the WCSS subscale score in the third step in place of baseline WCSS total score and change in WCSS total score, respectively. In addition, weight loss tertiles were computed and differences in WCSS subscale scores by tertile were examined using analysis of variance (ANOVA).
To examine whether changes in the WCSS Dietary Choices and Physical Activity subscales from baseline to posttreatment were related to change in daily kcals consumed and change in weekly kcals expended through physical activity (respectively), two similar hierarchical linear regressions were conducted. In the first analysis, posttreatment change in daily kcals consumed was the dependent variable with treatment group, baseline weight, baseline WCSS Dietary Choices subscale score, and baseline kcals consumed in the first step; treatment attendance in the second step; and change in WCSS Dietary Choices subscale score from baseline to posttreatment in the third step. In the second analysis, posttreatment change in weekly kcals expended in physical activity was the dependent variable with baseline WCSS Physical Activity subscale score and baseline kcals expended in physical activity in the first step (in place of baseline Dietary Choices score and baseline kcals consumed), and change in WCSS Physical Activity subscale score from baseline to posttreatment in the third step (in place of change in Dietary Choices score).
Longitudinal analyses to support the construct validity of the WCSS were conducted using completers only from Sample 1 (n=113) rather than an intent-to-treat approach utilizing all cases assuming no change from baseline for missing values, because of concerns that the latter method may artificially inflate associations of interest. Tests of significance were based on alpha of 0.05. Bonferroni correction for multiple tests was applied where indicated. Statistical analyses were performed using PASW Statistics 18, Release 18.0.0 (©SPSS, Inc., 2009, Chicago, IL, www.spss.com).
RESULTS
Principal Components Analysis of the WCSS
Preliminary item level analyses examined the response distribution, mean, standard deviation, skew and kurtosis of each WCSS item, and the results of the item level analyses were judged adequate to proceed with the EDA on the full set of 54 items. The scree test (32), the minimum average partial procedure (33), and an implementation of the parallel analysis procedure (34, 35) were used to aid in the determination of the underlying dimensional structure of the WCSS. Based on these dimensionality procedures, both the 4- and 5-component PCA solutions with a varimax rotation were initially examined. An iterative process was begun and items with low component loadings (<0.40) and complex items with high loadings on more than one component were removed in the first set of PCA analyses. A second set of PCA analyses on the reduced item set re-examined the 4- and 5-component solutions. It was judged that the items loading on one of the components in the 5-component solution did not form a conceptually similar item set and these items were removed from further consideration. The final PCA indicated a clear 4-component solution that utilized 30 WCSS items with individual item loadings that ranged from 0.50 to 0.83, and accounted for 56% of the variance. The final 30-item scale (see supplementary material) included 4 components (subscales) which were named based on their item content: Dietary Choices (WCSS-DC; 10 items), Self-monitoring Strategies (WCSS-SM; 7 items), Physical Activity (WCSS-PA; 6 items), and Psychological Coping (WCSS-PC; 7 items). Component matrix loadings for each item are presented in Table 2.
Table 2.
Final 30-item WCSS Rotated Component Matrix Loadings
| Component | ||||
|---|---|---|---|---|
| Item | 1 | 2 | 3 | 4 |
| I had several servings of fruits and/or vegetables each day. | .64 | .12 | .15 | .04 |
| I kept high calorie, high fat foods (e.g., chips, cookies, cakes) out of sight so they would not tempt me. | .50 | .16 | −.05 | .36 |
| I avoided fried foods. | .56 | .20 | .10 | .34 |
| I kept low-calorie foods (e.g., fruit, raw vegetables, unbuttered popcorn) accessible for a healthy snack. | .65 | .26 | .16 | .21 |
| I limited my intake of regular soda. | .56 | .08 | .16 | −.05 |
| I ate lower-fat meats (e.g., chicken, turkey, fish) or meat substitutes (e.g., lentils). | .64 | .17 | .14 | .24 |
| When eating dairy products (e.g., milk, yogurt, cheese), I chose reduced fat or fat free options. | .64 | .14 | .11 | .03 |
| I ate meats, fish, or vegetables that were baked, broiled, or grilled. | .72 | .13 | .13 | .16 |
| I chose low-calorie and/or low-fat foods to eat instead of higher calorie options. | .65 | .39 | .11 | .26 |
| I ate high-fiber foods (e.g., whole grain breads or cereals, fruit, vegetables). | .74 | .04 | .25 | .12 |
| I set a daily calorie goal for myself. | .25 | .72 | .18 | .28 |
| I kept a record of the type and amount of food I ate. | .20 | .79 | .06 | .20 |
| I weighed and/or measured the foods I ate. | .34 | .72 | .09 | .20 |
| I kept a record of the calories and fat in the foods I ate. | .18 | .83 | .17 | .18 |
| I kept a record of my minutes of exercise. | .17 | .62 | .44 | .18 |
| I weighed myself daily. | .18 | .51 | .16 | .04 |
| I kept a graph of my weight. | .07 | .81 | .16 | .10 |
| I set exercise goals for myself. | .15 | .41 | .71 | .22 |
| I had a plan for getting my exercise in if the weather was bad and I couldn’t exercise outside. | .20 | .16 | .72 | .17 |
| I engaged in moderate-intensity exercise like brisk walking or something similar to brisk walking for at least 30 minutes a day. | .14 | .09 | .80 | .08 |
| If I missed exercising on one day, I made up for it by exercising longer another day. | .17 | .31 | .60 | .19 |
| I scheduled exercise into my day. | .20 | .23 | .81 | .17 |
| I kept my exercise clothes or shoes where I could see them as a reminder to exercise. | .23 | −.04 | .61 | .31 |
| If I overate, I thought about what led up to my overeating. | .05 | .30 | .05 | .57 |
| If I overate on one day, I made up for it by eating less the next day. | .19 | .16 | .15 | .56 |
| When I reached my calorie goal for the day but still felt hungry, I tried a pleasant activity to take my mind off of the hunger. | .10 | .21 | −.02 | .62 |
| If I got off track with my eating or exercise, I encouraged myself by thinking positively. | .13 | .21 | .34 | .60 |
| When I met a goal related to my eating, exercise, or weight loss, I rewarded myself with something special that did not involve food. | .21 | −.13 | .20 | .57 |
| If I had negative thoughts about my weight loss progress, I tried to catch myself and stop that kind of thinking. | .12 | .18 | .25 | .64 |
| If I regained weight, I thought about my past successes and reminded myself that I could get back on track. | .12 | .10 | .26 | .63 |
Subscale mean scores (ranging from 0–4) were computed by summing the item scores in each subscale and dividing by the number of items in that subscale. A total mean score was computed by summing all item scores and dividing by 30. WCSS subscale scores were positively correlated with each other, with correlations ranging from 0.50 to 0.55 (p<.0.001) at baseline.
All WCSS subscales demonstrated good internal consistency reliability, with Cronbach’s alpha coefficients of 0.87, 0.89, 0.88, and 0.79 for the WCSS-DC, WCSS-SM, WCSS-PA, and WCSS-PC subscales, respectively.
Social Desirability and the WCSS
Correlations between the MCSDS Short Form and WCSS subscales and total score were low and nonsignificant (ranging from −0.10 to 0.09, p>0.05), indicating that participants’ responses on the WCSS were not significantly influenced by social desirability.
Construct Validity of the WCSS
To demonstrate convergent validity of the WCSS, it was expected that greater use of dietary strategies would be associated with lower calorie and fat intake, and more use of physical activity strategies would be associated with greater calorie expenditure through physical activity. Consistent with these hypotheses, cross-sectional analyses at baseline showed that WCSS-DC was negatively related to daily kcals consumed (p=0.004) and percent kcals consumed from fat (p=0.001) and WCSS-PA was positively related to weekly kcals expended in physical activity (p<0.001). Refer to Table 3 for correlations between WCSS subscales and measures of dietary intake and physical activity. We also found that WCSS total score at baseline was negatively related to baseline weight (r=−0.28, p=0.001), indicating that more use of weight management strategies was associated with lower weight. To demonstrate discriminant validity, we expected that, relative to other WCSS subscales, WCSS-DC would have the strongest association with calorie and fat intake and WCSS-PA would have the strongest association with calorie expenditure through physical activity. These hypotheses were confirmed (Table 3).
Table 3.
Correlations between WCSS subscales, energy intake, fat intake, and energy expenditure
| WCSS-DC | WCSS-SM | WCSS-PA | WCSS-PC | |
|---|---|---|---|---|
| Energy intake (kcals/day) | −0.24b | −0.13 | −0.18a | −0.13 |
| Percent daily kcals from fat | −0.27b | −0.04 | 0.00 | −0.03 |
| Energy expended (kcals/week) | 0.19a | 0.04 | 0.34c | 0.10 |
p<0.05;
p<0.01,
p<0.001.
WCSS-DC = Dietary Choices; WCSS-SM = Self-monitoring Strategies; WCSS-PA = Physical Activity; WCSS-PC = Psychological Coping. Data are from all participants in Sample 1 at baseline (N=144).
Since WCSS items were developed to reflect strategies and skills taught in behavioral weight loss programs, we hypothesized that scores would increase during treatment and that these increases would be related to session attendance and weight loss. Consistent with this, we found that all WCSS subscales increased significantly over the course of 48 weeks of behaviorally oriented weight loss treatment (Table 4). Controlling for treatment group, changes in WCSS subscale scores were positively related to session attendance as follows: Self-monitoring Strategies (rp = 0.40, p<0.001), Physical Activity (rp = 0.27, p=0.004), and Psychological Coping (rp = 0.20, p=0.031); the association with Dietary Choices was not significant (rp = 0.16, p=0.093). Further, change in WCSS total score from baseline to 48 weeks was significantly related to mean weight loss at 48 weeks (M=−5.3 ± 6.6 kg) without adjusting for covariates (r=−0.48, p<0.001) and after adjusting for covariates (R2Δ= 0.175, p<0.001). Refer to Table 5 for individual covariates in the final model with their standardized and unstandardized regression weights. Results of separate hierarchical regressions revealed that posttreatment changes (i.e., posttreatment – baseline) in each WCSS subscale also were significantly associated with posttreatment weight loss (Dietary Choices: R2Δ= 0.177, p<0.001; Self-monitoring Strategies: R2Δ =0.066, p=0.002; Physical Activity: R2Δ =0.105, p<0.001; Psychological Coping: R2Δ =0.141, p<0.001).
Table 4.
Mean WCSS subscale and total scores at baseline and posttreatmenta
| Baseline | Posttreatment | p-value | |
|---|---|---|---|
| Dietary Choices | 2.11 ± 0.08 | 2.73 ± 0.07 | 0.001 |
| Self-monitoring Strategies | 0.59 ± 0.05 | 1.43 ± 0.09 | <0.001 |
| Physical Activity | 1.09 ± 0.09 | 1.70 ± 0.09 | <0.001 |
| Psychological Coping | 1.19 ± 0.06 | 2.01 ± 0.07 | <0.001 |
| WCSS Total Score | 1.34 ± 0.05 | 2.05 ± 0.06 | <0.001 |
Values are mean ± standard error for complete cases adjusted for weight loss treatment group; N=113.
Note: Subscale and total scores range from 0–4.
Table 5.
Hierarchical regression model predicting mean weight change at 48 weeks (N=113)
| B | SE | β | P | |
|---|---|---|---|---|
| Step 1a | ||||
| Treatment Group† | ||||
| Weight Watchers | −0.706 | 1.218 | −0.052 | 0.564 |
| Combined Treatment | 0.420 | 1.278 | 0.030 | 0.743 |
| Baseline weight | 0.007 | 0.030 | 0.019 | 0.812 |
| Baseline WCSS total score | −2.982 | 1.014 | −0.261 | 0.004 |
| Step 2b | ||||
| Treatment session attendance | −0.075 | 0.022 | −0.289 | 0.001 |
| Step 3c | ||||
| Change in WCSS Total Score (posttreatment – baseline) | −4.658 | 0.838 | −0.503 | <0.001 |
Coefficients are from the final model. SE = standard error. Weight change is computed as posttreatment (48-week) weight – baseline weight.
Reference group is Behavioral Weight Loss Treatment
R2 = 0.03, p=0.501
R2 = 0.224, R2Δ = 0.194, p<0.001
R2 = 0.399, R2Δ= 0.175, p<0.001
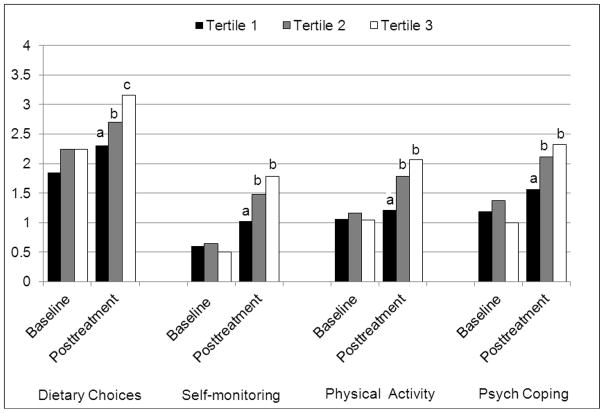
Weight loss tertiles were computed, with mean ± SD weight change as follows: Tertile 1 = 1.7 ± 3.5 kg; Tertile 2 = −5.0 ± 1.8 kg; Tertile 3 = −12.5 ± 3.6 kg. Analyses of WCSS subscales across weight loss tertiles showed that scores did not differ significantly at baseline but did differ at posttreatment such that participants in Tertiles 2 and 3 scored higher on all WCSS subscales at 48 weeks compared to participants in Tertile 1 (Figure 1). In addition, a significant difference was found between Tertiles 2 and 3 on the Dietary Choices subscale at posttreatment (p=0.002).
Figure 1.
Baseline and posttreatment (48-week) WCSS subscale mean scores by weight loss tertiles
No significant baseline differences were found; different letters indicate significant posttreatment differences between tertiles (p<0.05). Mean ± SD weight change for each tertile was as follows: Tertile 1 (1.7 ± 3.5 kg), Tertile 2 (−5.0 ± 1.8 kg), and Tertile 3 (−12.5 ± 3.6 kg).
Finally, in adjusted models, posttreatment change in WCSS-DC was negatively related to posttreatment change in total daily kcals consumed (R2Δ =0.02, p=0.019) and posttreatment change in WCSS-PA was positively related to posttreatment change in kcals expended per week in physical activity (R2Δ =0.15, p<0.001).
DISCUSSION
Results of the current study support the psychometric properties of the WCSS, a self-report measure to assess use of specific strategies for losing weight or maintaining weight loss. The 30-item WCSS contains 4 subscales: Dietary Choices, Self-monitoring Strategies, Physical Activity, and Psychological Coping. Items were developed to reflect the strategies and skills taught in behavioral weight loss programs and that are believed to facilitate weight loss. The WCSS subscales and total score have good internal consistency reliability as measured by Cronbach’s alpha.
The content validity of the WCSS was strengthened by incorporation of expert feedback from independent reviewers on all aspects of scale development. Construct validity of the WCSS subscales and total scale score was evidenced in a number of ways. First, we found that the Dietary Choices and Physical Activity subscales were meaningfully related to validated measures of dietary intake and physical activity at baseline, respectively. Specifically, more frequent use of strategies for making lower calorie/lower fat food choices as measured by the WCSS was associated with consumption of fewer calories, and more frequent use of strategies to increase engagement in physical activity was associated with greater calorie expenditure through physical activity. Second, the WCSS showed good discriminant validity in that relative to the other WCSS subscales, Dietary Choices had the strongest association with calorie and fat intake, and Physical Activity had the strongest association with calorie expenditure through physical activity. Such findings provide support for the specificity of the WCSS subscales and suggest that they measure distinct weight management behaviors. Third, we found that WCSS total scores at baseline were negatively related to baseline weight, indicating that individuals who report more use of weight management strategies assessed by the WCSS tend to weigh less.
Beyond these cross-sectional associations, we found that all WCSS subscale scores increased significantly over the course of behaviorally-oriented weight loss treatment. Importantly, this shows that the WCSS captures specific strategies and skills across key domains that respond to treatment. We expected that participants who reported more use of weight control strategies would have higher rates of attendance at treatment meetings and lose more weight than those who reported less use of these strategies. In support of these hypotheses, our findings showed that increases in the WCSS were associated with better treatment session attendance and greater mean weight loss at 48 weeks. Further, when we divided participants into weight loss tertiles, we found that individuals in the top two tertiles (i.e., greatest and second greatest weight loss) reported more use of weight management strategies across all WCSS domains at the end of treatment compared to individuals in the lowest tertile. Additional support for the content validity of the individual WCSS subscales was evidenced by findings that posttreatment increases in the Dietary Choices and Physical Activity subscales were associated, respectively, with posttreatment reductions in energy intake and increases in energy expenditure through physical activity. Taken together, these results indicate that, as expected, the WCSS appears to measure use of behaviors that promote weight loss.
In the 30 years since the EBI (6) was developed, behavioral weight loss programs have progressed and now emphasize a variety of behaviors, beyond changes in eating behavior, that are thought to promote weight loss. The WCSS was developed to capture the breadth of skills and strategies that are currently represented in behavioral weight loss programs in an effort to identify specific behaviors that are associated with successful weight loss and weight loss maintenance. The findings of this study suggest that the WCSS may be useful in both research and clinical settings. For example, this instrument can be used to measure adherence to strategies taught in behavioral weight loss programs and behavioral change following treatment. Given the strong association between WCSS score and weight loss, identifying approaches to help individuals increase their engagement in the behaviors assessed by the WCSS may facilitate improved weight loss outcomes. Additional research exploring the frequency with which these strategies are used by successful weight loss maintainers would be beneficial. Research has shown that consuming a calorie- and fat-restricted diet and engaging in high levels of physical activity promote long-term weight loss (36). Thus, attaining a better understanding of how often specific behaviors are used for meeting these goals would provide practical guidance for people who want to achieve long-term weight management. The WCSS may also be useful in identifying which behaviors are most challenging to an individual trying to lose weight. This information can then be used to tailor treatment approaches to individual needs.
Strengths of the current study are its systematic approach to item development and its large and diverse sample of overweight and obese adults. However, since this is the first study to test the WCSS, continued investigation is needed to further evaluate its psychometric properties. For example, testing the validity and reliability of the WCSS in a non-treatment seeking community sample would be an important contribution. In addition, the current study examined the association between WCSS and treatment outcomes using a largely female sample, thus further research is needed to evaluate these associations in men.
In sum, results of this study support the validity and reliability of the WCSS in a sample of overweight and obese adults seeking weight loss treatment and suggest that the WCSS is a promising instrument for assessing use of specific behavioral strategies to facilitate weight loss.
Supplementary Material
Acknowledgments
The authors wish to thank the following individuals who provided expert review of the WCSS: Gary Goldfield PhD, Michael Lowe PhD, Patrick O’Neil PhD, Suzanne Phelan PhD, and Deborah Tate PhD. This project was supported in part by 5K23DK075645 (Pinto) and R01DK074721 (Raynor) from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health.
Footnotes
DISCLOSURES
The authors have no competing interests.
SUPPLEMENTARY MATERIAL
Supplementary material is available at http://onlinelibrary.wiley.com/journal/10.1002/(ISSN)1930-739X.
References
- 1.Wing RR. Behavioral approaches to the treatment of obesity. In: Bray G, Bouchard C, editors. Handbook of Obesity: Clinical Applications. Marcel Dekker, Inc; New York: 2004. pp. 147–67. [Google Scholar]
- 2.Wadden TA, Crerand CE, Brock J. Behavioral treatment of obesity. Psychiatr Clin North Am. 2005;28:151–70. doi: 10.1016/j.psc.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 3.Baker RC, Kirschenbaum DS. Self-monitoring may be necessary for successful weight control. Behavior Therapy. 1993;24:377–94. [Google Scholar]
- 4.Boutelle KN, Kirschenbaum DS. Further support for consistent self-monitoring as a vital component of successful weight control. Obes Res. 1998;6:219–24. doi: 10.1002/j.1550-8528.1998.tb00340.x. [DOI] [PubMed] [Google Scholar]
- 5.Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323–41. doi: 10.1146/annurev.nutr.21.1.323. [DOI] [PubMed] [Google Scholar]
- 6.O’Neil PM, Currey HS, Hirsch AA, et al. Development and validation of the Eating Behavior Inventory. Journal of Behavioral Assessment. 1979;1:123–32. [Google Scholar]
- 7.Guare JC, Wing RR, Marcus MD, Epstein LH, Burton LR, Gooding WE. Analysis of changes in eating behavior and weight loss in type II diabetic patients. Which behaviors to change. Diabetes Care. 1989;12:500–3. doi: 10.2337/diacare.12.7.500. [DOI] [PubMed] [Google Scholar]
- 8.Guare JC, Wing RR, Grant A. Comparison of obese NIDDM and nondiabetic women: short- and long-term weight loss. Obes Res. 1995;3:329–35. doi: 10.1002/j.1550-8528.1995.tb00158.x. [DOI] [PubMed] [Google Scholar]
- 9.Wing RR, Marcus MD, Salata R, Epstein LH, Miaskiewicz S, Blair EH. Effects of a very-low-calorie diet on long-term glycemic control in obese type 2 diabetic subjects. Arch Intern Med. 1991;151:1334–40. [PubMed] [Google Scholar]
- 10.Harvey-Berino J. Calorie restriction is more effective for obesity treatment than dietary fat restriction. Ann Behav Med. 1999;21:35–9. doi: 10.1007/BF02895031. [DOI] [PubMed] [Google Scholar]
- 11.Jakicic JM, Wing RR, Winters-Hart C. Relationship of physical activity to eating behaviors and weight loss in women. Med Sci Sports Exerc. 2002;34:1653–9. doi: 10.1097/00005768-200210000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Qi BB, Dennis KE. The adoption of eating behaviors conducive to weight loss. Eating behaviors. 2000;1:23–31. doi: 10.1016/s1471-0153(00)00003-9. [DOI] [PubMed] [Google Scholar]
- 13.The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care. 1999;22:623–34. doi: 10.2337/diacare.22.4.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ryan DH, Espeland MA, Foster GD, et al. Look AHEAD (Action for Health in Diabetes): design and methods for a clinical trial of weight loss for the prevention of cardiovascular disease in type 2 diabetes. Control Clin Trials. 2003;24:610–28. doi: 10.1016/s0197-2456(03)00064-3. [DOI] [PubMed] [Google Scholar]
- 16.Wadden TA, West DS, Delahanty L, et al. The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity (Silver Spring) 2006;14:737–52. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Neil PM, Rieder S. Utility and validity of the eating behavior inventory in clinical obesity research: A review of the literature. Obesity Reviews. 2005;6:209–16. doi: 10.1111/j.1467-789X.2005.00192.x. [DOI] [PubMed] [Google Scholar]
- 18.Subak LL, Wing R, West DS, et al. Weight loss to treat urinary incontinence in overweight and obese women. N Engl J Med. 2009;360:481–90. doi: 10.1056/NEJMoa0806375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pinto AM, Fava JL, Hoffmann DA, Wing RR. Combining behavioral weight loss treatment and a commercial program: A randomized clinical trial. Obesity. doi: 10.1002/oby.20044. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raynor HA, Steeves EA, Hecht J, Fava JL, Wing RR. Limiting variety in non-nutrient-dense, energy-dense foods during a lifestyle intervention: A randomized controlled trial. The American Journal of Clinical Nutrition. 2012;95:1305–14. doi: 10.3945/ajcn.111.031153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gokee-Larose J, Gorin AA, Wing RR. Behavioral self-regulation for weight loss in young adults: a randomized controlled trial. Int J Behav Nutr Phys Act. 2009;6:10. doi: 10.1186/1479-5868-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reynolds WM. Development of reliable and valid short forms of the Marlowe-Crowne Social Desirability Scale. J Clin Psychol. 1982;38:119–25. [Google Scholar]
- 23.Loo R, Thorpe K. Confirmatory factor analyses of the full and short versions of the Marlowe-Crowne Social Desirability Scale. J Soc Psychol. 2000;140:628–35. doi: 10.1080/00224540009600503. [DOI] [PubMed] [Google Scholar]
- 24.Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124:453–69. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 25.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–35. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 26.Subar AF, Thompson FE, Kipnis V, et al. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: The Eating at America’s Table Study. Am J Epidemiol. 2001;154:1089–99. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
- 27.Paffenbarger RS, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol. 1978;108:161–75. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- 28.Harris JK, French SA, Jeffery RW, McGovern PG, Wing RR. Dietary and physical activity correlates of long-term weight loss. Obes Res. 1994;2:307–13. doi: 10.1002/j.1550-8528.1994.tb00069.x. [DOI] [PubMed] [Google Scholar]
- 29.Ewbank PP, Darga LL, Lucas CP. Physical activity as a predictor of weight maintenance in previously obese subjects. Obes Res. 1995;3:257–63. doi: 10.1002/j.1550-8528.1995.tb00146.x. [DOI] [PubMed] [Google Scholar]
- 30.Kaiser HF. The varimax criterion for analytic rotation in factor analysis. Psychometrika. 1958;23:187–200. [Google Scholar]
- 31.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 32.Cattell RB. The scree test for the number of factors. Mutivariate Behavioral Research. 1966;1:245–76. doi: 10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- 33.Velicer WF. Determining the number of components from the matrix of partial correlations. Psychometrika. 1976;41:321–7. [Google Scholar]
- 34.Horn JL. A rationale and test for the number of factors in factor analysis. Psychometrika. 1965;30:179–85. doi: 10.1007/BF02289447. [DOI] [PubMed] [Google Scholar]
- 35.O’Connor BP. SPSS and SAS programs for determining the number of components using parallel analysis and Velicer’s MAP test. Behav Res Meth Instrum Comput. 2000;32:396–402. doi: 10.3758/bf03200807. [DOI] [PubMed] [Google Scholar]
- 36.Wing RR, Pinto AM, Niemeier H. Maintenance: The ultimate goal. 2007. In: Apovian CM, Lenders CM, editors. A Clinical Guide for Management of Overweight and Obese Children and Adults. Taylor & Francis Group, LLC; Boca Raton, FL: pp. 177–96. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.