Abstract
Tijuana is situated on Mexico’s northern border with the U.S., where sex work is quasi-legal. Whereas previous work has focused on the risk behaviors of female sex workers (FSWs), less is known about the risk behaviors of their male clients. Further, research has not examined structural factors as moderators of the association between substance use and condom use, including the contexts in which sex takes place. The purpose of the current study is to examine whether having sex with FSWs in a bar moderates the link between alcohol intoxication during sex and condom use. We recruited 375 male clients of FSWs in Tijuana, Mexico from San Diego, California and Tijuana. Using computer assisted interviewing, we surveyed participants on their alcohol use, condom use, and physical contexts of sex with FSWs in the past four months. Results showed that more frequent intoxication during sex with FSWs is associated with more unprotected sex, but only among clients having sex with FSWs in a bar context. Results point to potential reasons for inconsistent condom use with FSWs in this context, including lower risk perceptions of sex with FSWs in bars. Future research should examine structural factors that underlie clients’ risk behavior in bars in order to inform structural-level HIV prevention interventions.
Keywords: HIV risk, male clients, female sex workers, alcohol use, risk environment, structural interventions
Introduction
The U.S.-Mexico border region is a nexus for sex work, substance use and sexual tourism, and rising rates of HIV and other sexually transmitted infections (STIs). In June 2012, the estimated number of individuals living with HIV in Mexico was about 179,500, with an HIV prevalence of 0.2% [1]. However, HIV prevalence among adults in Baja California, which includes Tijuana, the state’s major city, was double (0.54%) [2,3]. San Diego, California abuts Tijuana along the extreme western end of the U.S.–Mexico border. Among the more than 3 million individuals living in San Diego, approximately 4,800 were living with HIV in 2012 for an HIV prevalence similar to that of Mexico overall, but less than Tijuana (0.2%) [4]. Together, Tijuana and San Diego form the world’s largest binational metropolis and share its busiest land border crossing [5]. Because prostitution is illegal in San Diego, U.S. citizens will travel to Tijuana for sex, where it is quasi-legal in the zona roja (red light zone). Estimates of the number of female sex workers (FSWs) in Tijuana range from 6,000 to 10,000 and using census data across years, HIV prevalence among these women was estimated to rise from 2% in 2003 to 6% in 2006 [6]. Data from 70 countries suggest that the number of HIV-infected FSWs is the strongest predictor of countrywide HIV prevalence in the general population [7]. Whereas research has focused on the HIV risk behaviors among female sex workers in Tijuana, less is known about the risk behaviors of their male clients. These clients may serve as a bridge population not only between high-risk (i.e., FSWs) and low-risk (i.e., their non-commercial partners) populations [8], but clients residing in the United States may also bridge HIV/STI epidemics in Mexico and the U.S.
Globally, it is estimated that approximately 15% of men have ever paid a woman for sex [9]. Partly because of the desired anonymity and separation from spouses and girlfriends, a substantial proportion (i.e., 15% to 43%) of men who have ever paid for sex with a FSW report doing so overseas [9,10]. Research examining the characteristics of 400 U.S. and Mexican male clients of FSWs in Tijuana has shown that on average these men have frequented FSWs for more than ten years, and that half report both recent unprotected sex with a FSW and being high on illicit drugs when having sex with a FSW [11]. Alcohol and drug use during commercial sex by both FSWs and their male clients help to foster high-risk sexual encounters characterized by unprotected sex [12].
While studies show a consistent positive link between drug use and sexual risk behavior [13-16], the link between alcohol use and sexual risk appears less consistent, even among FSWs and their male clients [17, 18] This may be due in part to temporal and contextual considerations, as research shows that alcohol use in sexual contexts is more influential on condom use than general frequency and quantity of alcohol consumption [19]. The relationship between alcohol use during sex and sexual risk behavior has also been shown to be dependent on sensation seeking and average alcohol use among men who have sex with men [17]. Whereas individual-level factors have been shown to moderate the relationship between alcohol use during sex and condom use, factors at the structural level exogenous to the individual may also help shed further light on this association.
FSWs in Tijuana operate out of and serve clients in different environmental contexts, including bars/cantinas, nightclubs, and street corners. Rhodes’ “risk environment” framework gives primacy to context in understanding HIV risk [20,21]. Essentially, this framework emphasizes the role of both macro and micro- level environmental factors (e.g., social, economic, physical, policy) that are influential in shaping people’s risk behavior. By also recognizing and addressing the role of environment or context, HIV prevention interventions are ultimately more likely to lead to sustainable behavior change than interventions that address individual-level factors alone [22-24].
Previous research on the risk environment of male clients of FSWs in Tijuana has identified important contextual factors related to substance use and condom use [25]. For example, clients have described Tijuana as a “risky place” where it is relatively easy to “get lost in the moment” when under the influence of substances during sex [25]. In the current study, we focused on the intersection between alcohol use during sex and the physical context wherein sex takes place to examine condom use with FSWs among male clients in Tijuana. Specifically, we focused on the context of sex with FSWs in bars/cantinas in Tijuana as they represent places where simultaneous alcohol use and sexual encounters are likely.
In Tijuana, FSWs who operate in bars/cantinas are typically referred to as ficheras. Ficheras are similar to waitresses that sit and drink alcohol with clients. In bars in the zona roja, particularly in zona norte, there are rooms or small spaces, with or without a bed, located adjacent to or above the bar that are designated for sexual encounters. In sum, whereas previous work has shown how individual-level characteristics moderate the relationship between alcohol use and condom use, the evidence suggests that the structural environment may also influence this relationship among clients of FSWs in Tijuana. In the current study, we examined whether sex with FSWs in a bar (vs. not) moderates the relationship between alcohol and drug use during sex and condom use. Applying the risk environment framework, we hypothesized that among male clients of FSWs in Tijuana, higher alcohol intoxication during sex, but not necessarily drug use during sex is related to more unprotected sex if clients reported sex with FSWs in a bar than if they did not report sex in this context. Thus, we also included drug use during sex in this study to examine whether sex in a bar particularly matters for the relationship between condom use and alcohol use, but not the relationship between condom use and drug use. In comparison with previous research also examining male clients of FSWs in Tijuana [11,12], this is the first study to explicitly examine alcohol use. Specifically, this study has the potential to illustrate the important moderating role of the risk environment in explaining the link between alcohol intoxication during sex and condom use. Ultimately, these findings may help inform structural-level HIV/STI risk reduction interventions targeted towards male clients of FSWs.
Method
Participants and Setting
Participants were 375 male clients of female sex workers in Tijuana, Mexico. The current data are from the baseline assessment of participants enrolled in an HIV sexual risk reduction intervention that targeted male clients. Therefore, to be included in the study participants had to be HIV-negative adult males, report recently purchasing sex, and report recent unprotected vaginal or anal sex with a FSW. Baseline data for this study were collected between September 2010 and March 2012. Participants were recruited from the zona roja in Tijuana. Half of the sample were residents of Tijuana (n=191) and half were residents of San Diego County, California (n=184).
Recruitment
To recruit participants we used time-location sampling within different colonias (neighborhoods). We have used this method in our survey and pilot work, and time-location sampling has been employed in other studies to recruit hidden samples of men who have sex with men, including Latinos [26,27]. With the help of outreach workers, we compiled a map of places where male clients of FSWs potentially frequented, including bars, brothels, shooting galleries, hotels, alleys and street corners. Before initiating the project, it was explained to the bar and hotel owners at a community meeting. Thus, our study staff were met with respect and trust as they recruited male clients from these establishments. Trained outreach workers familiar with these establishments and their clientele approached prospective participants. Interested participants were directed to the research office where they completed a screening questionnaire; a total of 678 men completed screening. Men who were eligible (n=412, 61%) and were interested in participating were given a study card and asked to present it when they visited the study office or mobile clinic. A small number (n=12) of participants who were eligible were not interested in being enrolled into the intervention. Reasons for not participating that were informally given to study staff included fear of the required blood draw, or not having the time to complete the entire study.
Procedure
Assessment occurred in the study office to avoid logistical problems in FSWs’ workplaces. Men were reimbursed $20 USD or its equivalent for the interview. The survey was translated into Spanish and back-translated into English and it took about 45 minutes to complete. All measures were administered using computer-assisted personal interviewing (CAPI; NOVA software, MD, USA). Informed consent was obtained and participant anonymity and privacy were ensured during study procedures. All study procedures were approved by ethical review boards for human subjects research at the University of California, San Diego and our local participating institution, the Tijuana General Hospital.
Measures
Demographics
Participants reported on their age, whether they currently lived in the United States, Tijuana, or another city in Mexico, if they have ever been deported from the United States, if they consider themselves Hispanic or Latino (yes/no), and their current marital status. Response choices to the last variable were “married”, “separated or filing for divorce”, “divorced but not remarried”, “widowed but not remarried”, “never married”, and “common law”. For the analyses, other than age each of these variables was dichotomized: Live in U.S. (yes/no), ever deported from the U.S. (yes/no), Hispanic/Latino (yes/no), and married/common law vs. all others.
Context of sex acts with FSWs
Participants were asked to indicate “yes” or “no” to whether they had sex with FSWs in any of the following locations in Tijuana in the past 4 months: bar/cantina, street corner, strip club, vehicle, after hours club, massage parlor, adult theater, hotel or motel, your home, someone else’s home, public park or restroom, adult bookstore, bus station, brothel, shooting gallery, or other. Participants were allowed to check more than one.
Alcohol use
Frequency and quantity of alcohol use over the past year was assessed with items on the Alcohol Use Disorder Identification Test (AUDIT). The first three items on the AUDIT assess quantity and frequency of alcohol consumption, and have been shown to be as reliable and valid as the full-length 10-item scale [28]. Alcohol frequency: Participants were asked to report how often they have a drink containing alcohol; responses ranged from 0 being “never” to 5 being “4 or more times a week”. Alcohol quantity: Participants reported how many drinks containing alcohol they have on a typical day when they are drinking; responses ranged from 1 being “3 or 4” to 4 being “10 or more”. Binge drinking frequency: Participants reported how often they have six or more drinks in a single occasion; responses ranged from 0 being “never” to 4 being “daily or almost daily”. These variables were entered as continuous variables in our analyses.
Substance use during sex
Participants were asked to report about their own and the FSWs’ alcohol and drug use during sex with FSWs. Specifically, they were asked about alcohol intoxication during sex and being high on drugs during sex with a FSW with the following four items that began with the stem, “In the past 4 months, when you had sex with a prostitute in Tijuana…”: 1) “how often were you drunk?”; 2) “how often was she drunk?”; 3) “how often were you high on drugs?”; 4) “how often was she high on drugs?”. Responses were measured on a Likert-type scale with 1 being “never,” 2 being “once in a while,” 3 being “fairly often,” and 4 being “very often.” These variables were entered as continuous variables in our analyses.
Condom use
Participants used an open-response format to report the number of the following during the past four months when they had sex with a FSW in Tijuana: times of vaginal sex, times condom used for vaginal sex, times of anal sex, times condom used for anal sex. We computed the proportion of unprotected sex acts with a FSW in the past four months by subtracting the total number of times a condom was used during vaginal and anal sex from the total vaginal and sex acts, and dividing that difference by total sex acts.
Reasons for inconsistent condom use with FSWs
Participants were asked if any of the following were reasons for not using a condom with a FSW in the past four months: “You were drunk or high;” “You were overcome with sexual passion;” “You didn’t think about using a condom;” “No condoms were available at the time;” “You always have sex with the same prostitute;” “The prostitute did not suggest using a condom;” “The prostitute did not want to use a condom;” “You didn’t think that your prostitute had any sexually transmitted diseases;” “You pulled out before ejaculating;” “Condoms reduce sexual pleasure;” “It is not necessary to use condoms with prostitutes;” and “Other.” Participants were allowed to check more than one. For all measures other than the AUDIT we used a retrospective period of four months because previous research has shown that this recall period produces good reliability for substance use and HIV risk behavior [29]. The AUDIT incorporates time in the response options of specific items and has been previously validated using this format [28].
Data Analyses
Analyses were conducted in four stages. First, we examined the contexts in which participants reported having sex with FSWs in the past four months. We also examined demographics and substance use during sex among male clients who did and did not report having sex with FSWs in a bar/cantina using logistic regression analyses (coded as 1=sex with FSWs in a bar, 0=no sex with FSWs in a bar). Second, we conducted logistic regression analyses to examine self-reported reasons for inconsistent condom use with FSWs by sex in a bar. Third, we conducted a multivariate logistic regression to examine which factors were uniquely associated with sex with FSWs in a bar. Variables that were independently associated with sex in a bar in bivariate analyses (p<.10) were included in this multivariate logistic regression model. Finally, we tested our primary hypothesis that alcohol intoxication during sex with an FSW is positively related to unprotected sex with FSWs among men who had sex with FSWs in a bar, but not among men who did not have sex with FSWs in this context. That is, we examined the interaction between bar context and client intoxication during sex on condom use. To test this, we conducted a hierarchical linear regression in which substance use during sex and sex in a bar were entered in one step of the model, and the two-way interactions between alcohol intoxication during sex and sex in a bar and between drug use during sex and sex in a bar were entered in the last step of the model predicting proportion of unprotected sex acts with FSWs. In this analysis, we importantly controlled for demographics and sex with FSWs in other contexts (e.g., on a street corner) in the first step of the model. To avoid multicollinearity, alcohol use and drug use during sex were mean centered in the hierarchical regression model.
Results
Descriptives of main study variables
Participants were asked to indicate all of the places they had sex with a FSW in the past four months. Among the 375 male clients, 14% (n=54) reported having sex with a FSW in a bar/cantina in the past four months, whereas 86% (n=321) did not. Among the latter group, a majority of clients (92%, n=294) reported having sex with a FSW in a hotel or motel, and a plurality of clients (20%, n=64) reported doing this in their home. Among the 375 clients, mean proportion of unprotected sex with FSWs was 0.77 (SD=0.30). For alcohol intoxication during sex with a FSW (“drunk during sex”), 17% (n=62) reported doing this “very often;” 22% (n=82) “fairly often;” 21% (n=79) “once in a while;” and 41% (n=152) reported “never” being drunk during sex with a FSW in the past four months. For being “high” on drugs during sex with a FSW, 42% (n=158) reported doing this “very often;” 25% (n=97) “fairly often;” 7% (n=27) “once in a while;” and 25% (n=93) reported “never” being high during sex with a FSW in the past four months. Thus, drug use during sex more frequently took place compared to alcohol intoxication during sex.
Sex with FSWs in other contexts other than a bar/cantina
We wanted to examine whether clients who reported sex in bars were also more likely to have sex with FSWs in other contexts. The purpose of this sub-analysis was to identify potential contextual covariates in testing our primary hypothesis. That is, we aimed to control for the fact that clients reported having sex in other contexts other than bars/cantinas when predicting condom use. A multivariate logistic regression revealed that clients having sex with FSWs in bars were also more likely to have sex with FSWs on a street corner (12% among clients having sex in bars vs. 3% among clients not in bars; AOR=65.99, p <.001), in a strip club (11% vs. 5%; AOR=42.97, p <.001), in an after hours club (8% vs. 2%; AOR=5.25, p <.10), in a bus station (2% vs. 0.3%; AOR=37.04, p <.05), in a brothel (3% vs. 0.6%; AOR=49.54, p <.01), and in a shooting gallery (4% vs. 2%; AOR=9.42, p<.05).
Demographics and substance use
Logistic regression analyses showed that having sex with FSWs in a bar (vs. not) was associated with various demographic characteristics, but not with alcohol or drug use during sex. Table 1 summarizes these results. We did not find any differences in age, deportation status, and ethnicity between clients having sex in bars vs. not in bars. We did find that compared to clients not having sex with FSWs in bars, clients having sex in bars were less likely to report living in the US (52% vs. 30%) and more likely to report being married (46% vs. 28%). For alcohol use and substance use during sex, we did not find differences between the two male client groups on alcohol use (e.g., frequency and quantity of alcohol consumption, and binge drinking). We also did not find differences in the client-reported frequency of either the client or FSW being drunk during sex, or being “high” on drugs during sex.
Table 1.
Demographics and alcohol use by sex with FSW in a bar/cantina vs. not in past 4 months among male clients of FSWs in Tijuana, Mexico (n=375)
| Sex with FSW in a bar in the past 4 mo. | OR (95% CI) | ||||
|---|---|---|---|---|---|
| No (n= 321) | Yes (n= 54) | ||||
|
| |||||
| n | % | n | % | ||
| Age (Mean; SD) | 37.9 | 10.7 | 37.8 | 10.2 | 1.00 (0.97, 1.03) |
| Live in US (vs. Mexico) | 168 | 52.3% | 16 | 29.6% | 0.38 (0.21, 0.72)** |
| Ever deported from US | 111 | 34.6% | 20 | 37.0% | 1.11 (0.61, 2.02) |
| Hispanic/Latino | 277 | 86.3% | 46 | 85.2% | 0.91 (0.40, 2.06) |
| Married/common lawa | 91 | 28.3% | 25 | 46.3% | 2.18 (1.21, 3.92)** |
| Alcohol Frequency | 1.11 (0.89, 1.37) | ||||
| Never to monthly | 146 | 45.5% | 20 | 37.0% | |
| 2 to 4 times a month | 71 | 22.1% | 13 | 24.1% | |
| At least 2 to 3 times a week | 104 | 32.4% | 21 | 38.9% | |
| Alcohol Quantityb | 1.00 (0.81, 1.24) | ||||
| 3 or 4 | 50 | 15.6% | 11 | 20.4% | |
| 5 or 6 | 50 | 15.6% | 5 | 9.3% | |
| 7, 8, or 9 | 18 | 5.6% | 4 | 7.4% | |
| 10 or more | 82 | 25.5% | 13 | 24.1% | |
| Binge Drinking | 1.15 (0.94, 1.40) | ||||
| Never to monthly | 220 | 68.5% | 33 | 61.1% | |
| Weekly | 79 | 24.6% | 16 | 29.6% | |
| Daily or almost daily | 21 | 6.5% | 5 | 9.3% | |
| How often client drunk during sex with FSW | 0.99 (0.76, 1.28) | ||||
| Never | 131 | 40.8% | 21 | 38.9% | |
| Once in a while | 66 | 20.6% | 13 | 24.1% | |
| Fairly often | 70 | 21.8% | 12 | 22.2% | |
| Very often | 54 | 16.8% | 8 | 14.8% | |
| How often FSW drunk during sex | 1.23 (0.92, 1.63) | ||||
| Never | 183 | 57.0% | 22 | 40.7% | |
| Once in a while | 61 | 19.0% | 18 | 33.3% | |
| Fairly often | 58 | 18.1% | 10 | 18.5% | |
| Very often | 19 | 5.9% | 4 | 7.4% | |
| How often client “high” on drugs during sex with FSW | 0.97 (0.77, 1.23) | ||||
| Never | 79 | 24.6% | 14 | 25.9% | |
| Once in a while | 23 | 7.2% | 4 | 7.4% | |
| Fairly often | 83 | 25.9% | 14 | 25.9% | |
| Very often | 136 | 42.4% | 22 | 40.7% | |
| How often FSW “high” on drugs during sex | 1.13 (0.89, 1.43) | ||||
| Never | 105 | 32.7% | 12 | 22.2% | |
| Once in a while | 34 | 10.6% | 8 | 14.8% | |
| Fairly often | 82 | 25.5% | 17 | 31.5% | |
| Very often | 99 | 30.8% | 17 | 31.5% | |
Notes:
p<.10,
p<.05,
p<.01,
p<.001;
Sex with FSW in a bar: 0=no, 1=yes;
vs. separated, divorced widowed, never married;
among men who report drinking (n=298)
Reasons for inconsistent condom use with FSWs
Logistic regressions revealed that compared to clients who did not report having sex with FSWs in a bar/cantina, those who reported sex in this context were more likely to report the following as reasons for not always using a condom with a FSW (Table 2): being drunk or high (67% vs. 48%), being overcome with sexual passion (69% vs. 51%), not thinking about using a condom (63% vs. 40%), no condoms being available at the time (28% vs. 18%), always having sex with the same sex worker (11% vs. 4%), the sex worker not wanting to use a condom (24% vs. 6%), believing that the sex worker did not have any sexually transmitted diseases (32% vs. 7%), and pulling out before ejaculating (20% vs. 2%). These results should be interpreted by remembering that participants were allowed to report more than one reason for not using a condom with a FSW. Therefore these reasons are not mutually exclusive.
Table 2.
Self-reported reasons for not using a condom every time had sex with a FSW in past 4 months among male clients of FSWs in Tijuana, Mexicoa (n=375)
| Sex with FSW in a bar in the past 4 mo. | OR (95% CI) | ||||
|---|---|---|---|---|---|
| No (n= 321) | Yes (n= 54) | ||||
|
| |||||
| n | % | n | % | ||
| “You were drunk or high” | 154 | 48.0% | 36 | 66.7% | 2.14 (1.17, 3.93)* |
| “You were overcome with sexual passion” | 165 | 51.4% | 37 | 68.5% | 2.03 (1.10, 3.76)* |
| “You didn’t think about using a condom” | 127 | 39.6% | 34 | 63.0% | 2.57 (1.42, 4.67)**b |
| “No condoms were available at the time” | 57 | 17.8% | 15 | 27.8% | 1.77 (0.91, 3.42)† |
| “You always have sex with the same prostitute” | 13 | 4.0% | 6 | 11.1% | 2.94 (1.07, 8.11)* |
| “The prostitute did not suggest using a condom” | 80 | 24.9% | 17 | 31.5% | 1.37 (0.73, 2.57) |
| “The prostitute did not want to use a condom” | 20 | 6.2% | 13 | 24.1% | 4.74 (2.19, 10.25)***b |
| “You didn’t think that your prostitute had any sexually transmitted diseases” | 21 | 6.5% | 17 | 31.5% | 6.52 (3.16, 13.46)***b |
| “You pulled out before ejaculating” | 6 | 1.9% | 11 | 20.4% | 13.35 (4.70, 37.93)***b |
| “Condoms reduce sexual pleasure” | 198 | 61.7% | 33 | 61.1% | 0.96 (0.53, 1.74) |
| “It is not necessary to use condoms with prostitutes” | 21 | 6.5% | 5 | 9.3% | 1.45 (0.52, 4.02) |
Notes:
p<.10,
p<.05,
p<.01,
p<.001;
Sex with FSW in a bar: 0=no, 1=yes;
Reasons are not mutually exclusive;
Statistically significant (p <.004) after Bonferroni adjustment
Multivariate logistic regression
Table 3 shows which factors were uniquely associated with having sex with FSWs in a bar. Among male clients of FSWs in Tijuana, Mexico, compared to those who did not have sex with FSWs in a bar, those who have had sex in a bar were less likely to report living in the U.S., more likely to be married, and more likely to report thinking the sex worker did not have any sexually transmitted diseases and withdrawal before climax as reasons for not using condoms consistently with FSWs. They were also marginally more likely to report being drunk or high and the sex worker not wanting to use a condom as other reasons for inconsistent condom use.
Table 3.
Multivariate logistic regression model examining correlates of sex with FSWs in a bar among male clients of FSWs in Tijuana, Mexico (n=375).
| Model | AOR | 95% CI | |
|---|---|---|---|
| Lower | Upper | ||
| Live in US (vs. Mexico) | 0.48* | 0.23 | 1.00 |
| Married/common lawa | 1.98* | 1.01 | 3.89 |
| You were drunk or high | 1.84† | 0.92 | 3.67 |
| You were overcome with sexual passion | 0.92 | 0.43 | 1.93 |
| You didn’t think about using a condom | 1.58 | 0.78 | 3.18 |
| No condoms were available at the time | 0.98 | 0.44 | 2.18 |
| You always have sex with the same prostitute | 1.51 | 0.40 | 5.73 |
| The prostitute did not want to use a condom | 2.37† | 0.94 | 5.97 |
| You didn’t think that your prostitute had any sexually transmitted diseases | 3.26** | 1.38 | 7.73 |
| You pulled out before ejaculating | 7.73*** | 2.25 | 26.61 |
Notes:
p<.10,
p<.05,
p<.01,
p<.001;
Sex with FSW in a bar: 0=no, 1=yes;
vs. separated, divorced widowed, never married; χ2 (10) = 58.27, p <.001, Nagelkerke R2 = 0.26.
Condom use
Table 4 summarizes results from the hierarchical linear regression predicting proportion of unprotected sex acts in the past four months. After controlling for demographics (i.e., living in U.S., and marital status) sex with FSWs in other contexts (entered as dichotomous variables) in Step 1 of the regression model, and frequency of client intoxication during sex, frequency of client being “high” on drugs during sex, and sex with FSWs in a bar in Step 2 of the model, the last step of the regression model revealed a significant interaction between client intoxication during sex with FSWs and bar context. This interaction is depicted in Figure 1. Consistent with our hypothesis, among clients who reported having sex with FSWs in a bar/cantina, more frequent intoxication during sex with a FSW was associated with a higher proportion of unprotected sex with FSWs in the past four months; this relationship is not found among clients who did not report sex with FSWs in this context. Whereas this interaction was found for frequency of alcohol intoxication during sex, we did not find an interaction between sex in a bar context with frequency of client being “high” on drugs. In an effort to unpack potential factors underlying this finding, we examined client-reported reasons for not using condoms consistently with FSWs by sex in a bar context.
Table 4.
Hierarchical linear regression predicting proportion of unprotected sex acts with FSWs in past 4 months among male clients of FSWs in Tijuana, Mexico (n=375)
| Model | b | SE | β | t |
|---|---|---|---|---|
| Step 1. | ||||
| Live in US | -0.03 | 0.03 | -0.05 | -0.96 |
| Married | 0.02 | 0.03 | 0.03 | 0.64 |
| Sex with FSW in… | ||||
| Street corner | -0.17 | 0.06 | -0.19 | -2.95*** |
| Strip club | -0.03 | 0.05 | -0.03 | -0.54 |
| After hours club | 0.03 | 0.07 | 0.03 | 0.44 |
| Bus station | 0.09 | 0.13 | 0.04 | 0.72 |
| Brothel | 0.02 | 0.10 | 0.01 | 0.19 |
| Shooting Gallery | 0.06 | 0.08 | 0.05 | 0.80 |
| R2 = .04, ΔR2 (8, 366) = .04 | ||||
| Step 2. | ||||
| Live in US | -0.05 | 0.03 | -0.08 | -1.54 |
| Married | 0.04 | 0.03 | 0.06 | 1.19 |
| Sex with FSW in… | ||||
| Street corner | -0.07 | 0.07 | -0.08 | -1.03 |
| Strip club | 0.03 | 0.06 | 0.03 | 0.47 |
| After hours club | 0.08 | 0.07 | 0.07 | 1.04 |
| Bus station | 0.09 | 0.13 | 0.04 | 0.74 |
| Brothel | 0.04 | 0.09 | 0.03 | 0.43 |
| Shooting Gallery | 0.05 | 0.07 | 0.04 | 0.64 |
| Frequency of client intoxication during sex with a FSW | 0.02 | 0.01 | 0.08 | 1.65† |
| Frequency of client “high” on drugs during sex with a FSW | 0.04 | 0.01 | 0.17 | 3.21*** |
| Sex with FSW in a bar/cantina | -0.20 | 0.07 | -0.23 | -2.68** |
| R2 = .09, ΔR2 (3, 363) = .05*** | ||||
| Step 3. | ||||
| Live in US | -0.05 | 0.03 | -0.09 | -1.64† |
| Married | 0.05 | 0.03 | 0.07 | 1.34 |
| Sex with FSW in… | ||||
| Street corner | -0.07 | 0.07 | -0.08 | -1.02 |
| Strip club | 0.02 | 0.06 | 0.02 | 0.32 |
| After hours club | 0.08 | 0.07 | 0.07 | 1.10 |
| Bus station | 0.08 | 0.13 | 0.04 | 0.63 |
| Brothel | 0.01 | 0.10 | 0.00 | 0.07 |
| Shooting Gallery | 0.04 | 0.07 | 0.03 | 0.55 |
| Frequency of client intoxication during sex with a FSW | 0.01 | 0.01 | 0.03 | 0.55 |
| Frequency of client “high” on drugs during sex with a FSW | 0.05 | 0.01 | 0.18 | 3.31*** |
| Sex with FSW in a bar/cantina | -0.18 | 0.07 | -0.22 | -2.53** |
| Frequency of client intoxication during sex with a FSW X Sex with FSW in a bar/cantina | 0.11 | 0.04 | 0.16 | 2.80** |
| Frequency of client “high” on drugs during sex with a FSW X Sex with FSW in a bar/cantina | 0.00 | 0.04 | 0.00 | -0.04 |
| R2 = .11, ΔR2 (2, 361) = .02* |
Notes.
p < .001,
p < .01,
p < .05,
p < .10;
Live in US=1, in Mexico=0; Married/common law=1, separated, divorced widowed, never married=0; Sex with FSWs in different contexts are dummy coded with 1=Yes, sex in that context; Both frequency of client intoxication and being “high” on drugs during sex with FSW are mean centered; Sex with FSW in a bar/cantina=1, no sex with FSW in a bar/cantina=0
Figure 1. Client alcohol intoxication during sex predicting condom use with FSWs by sexual context among male clients of FSWs in Tijuana, Mexico (n=375).
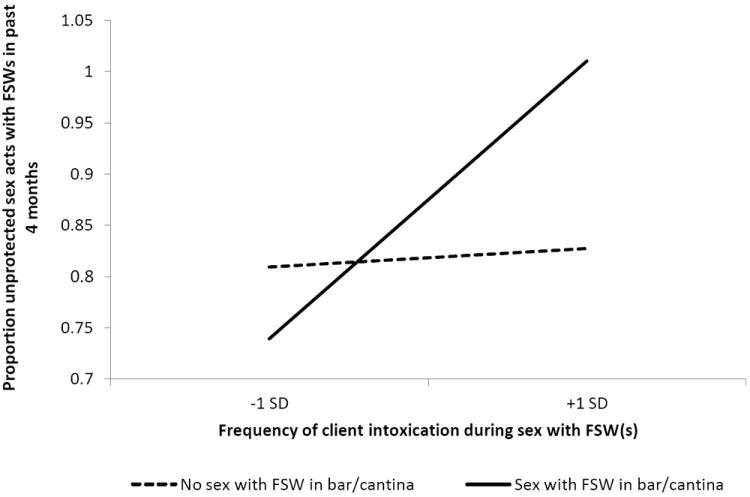
Notes: Frequency of client intoxication during sex with FSWs is mean centered.
Discussion
The purpose of the current study was to examine the moderating role of context in the association between substance use during sex and sexual risk behavior among male clients of FSWs in Tijuana, Mexico. Consistent with our hypothesis, we found that among clients who reported having sex with FSWs in a bar/cantina, more intoxication on alcohol during sex was associated with more unprotected sex; this relationship was not found among clients who did not report having sex in a bar/cantina. We also did not find an interaction between drug use during sex and sex in a bar in predicting unprotected sex. This suggests that it is the particular intersection between alcohol use and sex with FSWs in a bar, and not other substance use during sex, that helps to account for unprotected sex among these clients. Although, we did find higher overall drug use during sex than alcohol use during sex. This is not surprising given that Tijuana is situated along a major drug trafficking route, hence high availability and use of illicit drugs. Drugs and sex are inextricably linked in Tijuana; male clients and FSWs will use drugs during sex to heighten the sexual experience [25]. Our results are similar to research with men who have sex with men that has shown how individual sensation seeking moderates the association between alcohol use before sex and sexual risk behavior [17]. Unlike this previous work, however, the current study shows how a micro-physical aspect of the risk environment (i.e., bar context) rather than individual-level factors may modify the relationship. This role of the physical risk environment in influencing HIV risk is in line with the risk environment theoretical framework put forth by Rhodes and colleagues [21]. Overall, this study builds upon previous work demonstrating the important role of the risk environment in shaping individual behavior [20,25,30].
Although our data are limited in allowing us to characterize the specific structural factors of the bar context that may account for the results, we were able to ascertain some potential underlying characteristics of the bar context from the perspectives of the male clients. That is, we found that clients who reported having sex with a FSW in a bar/cantina were more likely to report inconsistent condom use because they believed that the FSW did not have any sexually transmitted infections and because they withdrew before climaxing. Therefore, it may be that clients who frequent FSWs in bars may be more likely to hold lower risk perceptions and inaccurate knowledge about condoms and HIV/STI transmission compared to clients who do not frequent FSWs in bars. It may be that male clients perceive FSWs in bars to be safer because of the fact that these FSWs tend to be registered, which in actuality is not always the case [31]. Future research should quantitatively and qualitatively examine more social- and structural-level characteristics of the bar context, including surrounding substance use and characteristics of the FSWs operating in bars, to shed further light on this issue.
Research in other regions around the world, like South Africa, has shown how alcohol serving establishments are places that may increase sexual risks for HIV, over and above the alcohol consumption in these places [32,33]. Furthermore, alcohol use has been shown to be associated with unprotected sex [32]. However, research has not systematically combined these two findings to ascertain how drinking contexts may change, or moderate the relationship between alcohol use and unprotected sex. In addition to being the first study to directly examine alcohol use and its relationship to sexual risk behavior among male clients of FSWs, the current study provides support for this moderated association among individuals engaging in high risk behavior in Tijuana, Mexico. Next steps for research in this region include the need to examine physical characteristics of bars (e.g., those with a back room versus those with adjoining rooms for sexual transactions), social norms surrounding substance use and sex, and management policies influencing FSWs’ alcohol use and condom availability in bars. Interestingly, frequency and quantity of alcohol consumption did not differ between men who had sex with FSWs in bars vs. not in bars. This suggests that clients frequenting FSWs in bars/cantinas may be attending these venues with the purpose of seeking sex, and not that they were more likely to drink and perchance engage in commercial sex.
This study also provides additional support of the bridging of male clients between FSWs and their primary partners. Clients who reported sex with FSWs in a bar were more likely to be married than clients who did not have sex with FSWs in a bar. In fact, a substantial proportion of the men who did not report having sex with FSWs in a bar reported having sex with FSWs in a hotel or their own home, suggesting less of a need for anonymity or secrecy from spouses among these men. Also, men having sex with FSWs in bars were more likely to reside in Mexico than in the U.S., which has implications for the local epidemic in Tijuana. Because we found that men who have sex with FSWs in this context also report less condom use the more often they are intoxicated during sex, there may be a need to intervene on both individual alcohol use during sex and in the bars to help prevent a growing concentrated HIV/STI epidemic in Baja California.
The results of the current study should be interpreted cautiously in light of its limitations. Data regarding sex with FSWs in the bars were not gathered at the event-level. Since our data were collected using a timeframe of the past 4 months, we do not know that the episodes of sex in a bar, being drunk during sex, and unprotected sex all occurred simultaneously. The data were also gathered cross-sectionally, prohibiting conclusions about the directionality of the relationships. Given the sensitive and private nature of the questions included in this study, participants may have been concerned with social desirability. However should that have been the case the current study provides a conservative test of the hypotheses, as participants would have underreported substance use and sexual risk behaviors. Although the ability to recall condom use may have been affected by substance use during sex, previous work demonstrated adequate reliability of self-report measures of substance use and HIV risk behaviors among drug users, especially when a recall period of no longer than 6 months is used [29,34-36]. Although ideal for the aims of the current paper, our sample consisted of male clients of FSWs in Tijuana, Mexico. Therefore, we cannot infer that our findings are generalizable to other male clients of FSWs around the globe. However, we believe our approach is generalizable and could be tailored to investigate similar questions in different environmental contexts, as the risk environment includes social, physical, policy, and economic factors that all interact to shape different risk-levels and behavior for different individuals.
Border cities in Mexico are economically depressed regions where commercial sex work is quasi-legal, helping to create an intersection between sex work, substance use, and rising HIV/STI rates. The potential for escalating HIV/STI epidemics San Diego, California and Tijuana, Mexico are appreciable. As in other regions, due to their high-risk behaviors FSWs and their male clients represent key populations to study in HIV prevention efforts. Whereas previous work has focused on the risk behaviors of FSWs, less is known about the behaviors of their male clients. Furthermore, even less is known about the risk environment of male clients and the potential role context plays in shaping their sexual risk behavior. The findings of the current study point to both a structural- and individual-level intervention. At the structural-level, results suggest interventions may need to target specific sex work venues, such as bars, where the intersection of alcohol and sex work makes condom use less likely. For example, increasing condom availability in these contexts is crucial, but likely not sufficient. At the individual-level, results show that targeting HIV knowledge and risk perceptions are also necessary. In sum, achieving long-lasting behavior change to reduce HIV risk in the area of sex work would require an integrated approach targeting structural factors, and individual factors among both FSWs and their clients.
Acknowledgments
Preparation of this manuscript was supported by a National Institute on Drug Abuse training fellowship T32DA023356. This project was funded by a National Institute on Drug Abuse grant R01DA029008.
References
- 1.Vigilancia Epidemiológica de casos de VIH/SIDA en México. Registro Nacional de Cases de SIDA Actualización (CENSIDA) 2012 [Google Scholar]
- 2.Iñiguez-Stevens E, Brouwer KC, Hogg RS, et al. Estimating the 2006 prevalence of HIV by gender and risk groups in Tijuana, Mexico. Gac Med Mex. 2009;145(3):189–195. [PMC free article] [PubMed] [Google Scholar]
- 3.Strathdee SA, Magis-Rodriguez C. Mexico’s evolving HIV epidemic. JAMA. 2008;300(5):571–573. doi: 10.1001/jama.300.5.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.HIV/AIDS Surveillance in California. California Department of Public Health; 2012. Available at: http://www.cdph.ca.gov/data/statistics/Documents/SSSemiAnnualRptJune2012.pdf. [Google Scholar]
- 5.Border Crossing: U S -Mexico Border Crossing Data. U.S. Department of Transportations; Available at: http://www.bts.gov/programs/international/border_crossing_entry_data/us_mexico/pdf/entire.pdf#search=’Border%20crossing%20statistics%20US%20Mexico’. [Google Scholar]
- 6.Brouwer KC, Strathdee SA, Magis-Rodríguez C, et al. Estimated numbers of men and women infected with HIV/AIDS in Tijuana, Mexico. J Urban Health. 2006;83(2):299–307. doi: 10.1007/s11524-005-9027-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Talbott JR. Size matters: the number of prostitutes and the global HIV/AIDS pandemic. PLoS ONE. 2007;2(6):e543. doi: 10.1371/journal.pone.0000543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patterson TL, Volkmann T, Gallardo M, et al. Identifying the HIV transmission bridge: which men are having unsafe sex with female sex workers and with their own wives or steady partners? J Acquir Immune Defic Syndr. 2012;60(4):414–420. doi: 10.1097/QAI.0b013e31825693f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rissel CE, Richters J, Grulich AE, De Visser RO, Smith AMA. Sex in Australia: experiences of commercial sex in a representative sample of adults. Aust N Z J Public Health. 2003;27(2):191–197. doi: 10.1111/j.1467-842x.2003.tb00807.x. [DOI] [PubMed] [Google Scholar]
- 10.Day S, Ward H, Perrotta L. Prostitution and risk of HIV: male partners of female prostitutes. BMJ. 1993;307(6900):359–361. doi: 10.1136/bmj.307.6900.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patterson TL, Goldenberg S, Gallardo M, et al. Correlates of HIV, sexually transmitted infections, and associated high-risk behaviors among male clients of female sex workers in Tijuana, Mexico. AIDS. 2009;23(13):1765–1771. doi: 10.1097/QAD.0b013e32832f08a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldenberg SM, Gallardo Cruz M, Strathdee SA, et al. Correlates of unprotected sex with female sex workers among male clients in Tijuana, Mexico. Sex Transm Dis. 2010;37(5):319–324. doi: 10.1097/OLQ.0b013e3181c5334f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Graaf R, Vanwesenbeeck I, Van Zessen G, Straver CJ, Visser JH. Alcohol and drug use in heterosexual and homosexual prostitution, and its relation to protection behaviour. AIDS Care. 1995;7(1):35–47. doi: 10.1080/09540129550126948. [DOI] [PubMed] [Google Scholar]
- 14.Stueve A, O’Donnell L, Duran R, San Doval A, Geier J. Being high and taking sexual risks: findings from a multisite survey of urban young men who have sex with men. AIDS Educ Prev. 2002;14(6):482–495. doi: 10.1521/aeap.14.8.482.24108. [DOI] [PubMed] [Google Scholar]
- 15.Clatts MC, Goldsamt LA, Yi H. Club drug use among young men who have sex with men in NYC: a preliminary epidemiological profile. Subst Use Misuse. 2005;40(9-10):1317–1330. doi: 10.1081/JA-200066898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clatts MC, Goldsamt LA, Yi H. Drug and sexual risk in four men who have sex with men populations: evidence for a sustained HIV epidemic in New York City. J Urban Health. 2005;82(1 Suppl 1):i9–17. doi: 10.1093/jurban/jti019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Newcomb ME, Clerkin EM, Mustanski B. Sensation seeking moderates the effects of alcohol and drug use prior to sex on sexual risk in young men who have sex with men. AIDS Behav. 2011;15(3):565–575. doi: 10.1007/s10461-010-9832-7. [DOI] [PubMed] [Google Scholar]
- 18.Li Q, Li X, Stanton B. Alcohol use among female sex workers and male clients: An integrative review of global literature. Alcohol and Alcoholism. 2010;45(2):188–199. doi: 10.1093/alcalc/agp095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalichman SC, Simbayi LC, Jooste S, Cain D. Frequency, quantity, and contextual use of alcohol among sexually transmitted infection clinic patients in Cape Town, South Africa. Am J Drug Alcohol Abuse. 2007;33(5):687–698. doi: 10.1080/00952990701522716. [DOI] [PubMed] [Google Scholar]
- 20.Rhodes T. The risk environment’: a framework for understanding and reducing drug-related harm. International Journal of Drug Policy. 2002;13(2):85–94. [Google Scholar]
- 21.Rhodes T. Risk environments and drug harms: a social science for harm reduction approach. International Journal of Drug Policy. 2009;20(3):193–201. doi: 10.1016/j.drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 22.Strathdee SA, Lozada R, Pollini RA, et al. Individual, social, and environmental influences associated with HIV infection among injection drug users in Tijuana, Mexico. J Acquir Immune Defic Syndr. 2008;47(3):369–376. doi: 10.1097/QAI.0b013e318160d5ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morisky DE, Malow RM, Tiglao TV, et al. Reducing sexual risk among Filipina female bar workers: effects of a CBPR-developed structural and network intervention. AIDS Educ Prev. 2010;22(4):371–385. doi: 10.1521/aeap.2010.22.4.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Urada L, Morisky D, Hernandez L, Strathdee S. Social and structural factors associated with consistent condom use among female entertainment workers trading sex in the Philippines. AIDS Behav. 2013;17(2):523–535. doi: 10.1007/s10461-011-0113-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goldenberg SM, Strathdee SA, Gallardo M, et al. “Over here, it’s just drugs, women and all the madness”: The HIV risk environment of clients of female sex workers in Tijuana, Mexico. Soc Sci Med. 2011;72(7):1185–1192. doi: 10.1016/j.socscimed.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stueve A, O’Donnell LN, Duran R, San Doval A, Blome J. Time-space sampling in minority communities: results with young Latino men who have sex with men. Am J Public Health. 2001;91(6):922–926. doi: 10.2105/ajph.91.6.922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.MacKellar D, Valleroy L, Karon J, Lemp G, Janssen R. The Young Men’s Survey: methods for estimating HIV seroprevalence and risk factors among young men who have sex with men. Public Health Rep. 1996;111(Suppl 1):138–144. [PMC free article] [PubMed] [Google Scholar]
- 28.Meneses-Gaya C, Zuardi AW, Loureiro SR, et al. Is the full version of the AUDIT really necessary? Study of the validity and internal construct of its abbreviated versions. Alcohol Clin Exp Res. 2010;34(8):1417–1424. doi: 10.1111/j.1530-0277.2010.01225.x. [DOI] [PubMed] [Google Scholar]
- 29.Napper LE, Fisher DG, Reynolds GL, Johnson ME. HIV risk behavior self-report reliability at different recall periods. AIDS Behav. 2010;14(1):152–161. doi: 10.1007/s10461-009-9575-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goldenberg SM, Strathdee SA, Gallardo M, et al. How important are venue-based HIV risks among male clients of female sex workers? A mixed methods analysis of the risk environment in nightlife venues in Tijuana, Mexico. Health Place. 2011;17(3):748–756. doi: 10.1016/j.healthplace.2011.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Larios SE, Lozada R, Strathdee SA, et al. An exploration of contextual factors that influence HIV risk in female sex workers in Mexico: The Social Ecological Model applied to HIV risk behaviors. AIDS Care. 2009;21(10):1335–1342. doi: 10.1080/09540120902803190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci. 2007;8(2):141–151. doi: 10.1007/s11121-006-0061-2. [DOI] [PubMed] [Google Scholar]
- 33.Cain D, Pare V, Kalichman SC, et al. HIV risks associated with patronizing alcohol serving establishments in South African Townships, Cape Town. Prev Sci. 2012;13(6):627–634. doi: 10.1007/s11121-012-0290-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crosby RA. Condom use as a dependent variable: measurement issues relevant to HIV prevention programs. AIDS Educ Prev. 1998;10(6):548–557. [PubMed] [Google Scholar]
- 35.Dowling-Guyer S, Johnson ME, Fisher DG, et al. Reliability of drug users’ self-reported HIV risk behaviors and validity of self-reported recent drug use. Assessment. 1994;1(4):383–392. [Google Scholar]
- 36.Needle R, Fisher DG, Weatherby N, et al. Reliability of self-reported HIV risk behaviors of drug users. Psychology of Addictive Behaviors. 1995;9(4):242. [Google Scholar]


