Abstract
Objective
The aim of the current study was to examine the moderating effect of emotion regulation on treatment efficacy following a parent-training intervention, Parent-Child Interaction Therapy (PCIT), for young children born preterm.
Method
In this pilot randomized controlled trial, 28 young children who were born preterm (i.e., < 37 weeks gestation) and presented with elevated levels of externalizing behavior problems were randomly assigned to an immediate treatment or waitlist control group. Observers masked to treatment condition coded an index of emotion regulation (i.e., global regulation) during a videotaped 10-min parent-child interaction at the initial baseline assessment. Treatment efficacy was assessed using a parent-report questionnaire of child disruptive behavior.
Results
Results demonstrated that global regulation significantly interacted with treatment condition in predicting change in child disruptive behavior. Specifically, higher levels of distress at baseline were associated with greater improvements in child disruptive behavior following the intervention.
Conclusion
These findings are discussed in the context of the differential susceptibility hypothesis and highlight the importance of considering children’s emotion regulation skills in the course of psychosocial treatment for young children born premature.
KEY TERMS: behavior problems, parent training, premature, emotion regulation
INTRODUCTION
Externalizing behavior problems are common in early childhood1 and are associated with poor outcomes if left untreated.2–4 Two common risk factors for childhood externalizing behavior problems are poor emotion regulation5 and preterm birth.6 Additionally, studies have shown preterm birth is associated with poor subsequent capacity for emotion regulation.7,8 Given the high individual and societal costs of conduct problems,9 it is not only important to identify effective treatments for these problems but also to identify which individual children could benefit most from these treatments. Examining the relationship between emotion regulation and externalizing behavior problems, particularly among children who were born preterm, can help provide further understanding of individual factors that are associated with treatment efficacy.
Emotion Regulation and Externalizing Behavior Problems
Emotion regulation can be conceptualized as the capacity of an individual to control the intensity of his or her response to environmental stressors and the ability to manage or recover from this response (e.g. latency and intensity of distress, ability to self-soothe and recover from a distress response).5 Individual differences in emotion regulation are present at birth,10 and the capacity for emotion regulation begins to consolidate at 18 months,11,12 representing an important developmental accomplishment.12,13 There is consistent evidence demonstrating a negative association between young children’s capacity for emotion regulation and subsequent externalizing behavior problems.14–17 For example, Eisenberg and colleagues15 found that 4- to 8-year-old children (n = 214) with parent- and teacher-reported externalizing problems were prone to parent and teacher report of low emotion regulation. Findings were similar in a study of 3-year-old boys from low-income families (n = 282) in which poor capacity for emotion regulation coded by independent observers during a frustration task was associated with higher teacher-reported externalizing behavior problems. Using respiratory sinus arrhythmia (RSA), a physiological index of emotion regulation, Calkins and Dedmon18 found that 2-year-old children (n = 99) at high-risk for externalizing behavior problems displayed lower emotion regulation during challenging tasks compared to children at low-risk for these problems. Due to its consistent association with child externalizing behavior problems using parent and teacher report, independent observation, and physiological measures, a next important step in this area of research is to examine emotion regulation as a potential moderator of treatment targeting these behavior problems in young children.
Preterm Birth and Externalizing Behavior Problems
In addition to emotion regulation, preterm birth, typically defined as gestation lasting less than 37 weeks, also is associated with an increased likelihood for behavior problems in childhood.19,20 In a meta-analysis, Bhutta and colleagues19 examined behavioral data from 16 case-control studies of children born preterm and found that children born preterm demonstrated increased behavior problems in 13 (81%) of the 16 studies. Specifically, children born preterm were found to have higher rates of externalizing behavior problems in 9 (69%) of the 13 studies examining this relationship. Farooqi and colleagues21 compared 86 children born preterm to an equal number of matched controls at 11 years of age on behavioral and emotional problems, social competencies, and adaptive functioning. This study found significant effects of preterm birth status on parent-reported behavioral problems. Similarly, Stjernqvist and Svenningsen22 compared 65 children born extremely preterm (< 29 weeks gestational age) to full-term control children at 10 years of age in a population-based study and found higher rates of behavior problems in children born preterm (32%) compared to children born full-term (10%).
In a prospective, longitudinal study of 869 children born preterm and low birth weight, Gray and colleagues23 found the prevalence of behavior problems in children born preterm to be double the prevalence of these problems in the general population and relatively stable between the ages of 3 and 8 years. More recently, Bul and van Baar24 compared 348 moderately preterm children (gestational age of 32–36 weeks) to 182 full-term children at 8 years of age and found preterm birth to be associated with elevated parent-reported externalizing behavior problems. Collectively, the higher rates and stability of externalizing behavior problems in children born preterm highlight the importance of early intervention with this population. Additionally, given the higher rates of children born preterm with very low birth weight who now survive due to medical advances,25 it is necessary to examine the various risk factors associated with preterm birth and how they interact with each other to impact treatment efficacy.
Preterm Birth and Emotion Regulation
In addition to higher rates of behavior problems, children who are born preterm also have poorer capacity for emotion regulation. Clark and colleagues13 examined the development of emotional regulation in children born extremely preterm (< 28 weeks gestational age, n = 39) and very preterm (< 34 weeks gestational age, n = 56) compared to children born full-term (n = 103). This prospective, longitudinal study found that lower gestational age was associated with poorer parent-reported emotion regulation and observed emotional regulation during challenging tasks at age 2 and 4 years. Similarly, Evrard and colleagues26 found that, compared to 38 infants born full-term, 74 infants born preterm displayed poorer emotion regulation assessed using the Infant Regulatory Scoring System (IRSS),27 a behavioral coding system. Finally, Spittle and colleagues28 demonstrated higher emotion dysregulation based on parent report among 188 children born very preterm (< 30 weeks gestational age) compared to 70 children born full-term. The early emergence of emotion regulation difficulties in children born preterm, as well as the association between these difficulties and behavior problems, suggest children born preterm with poor emotion regulation are at particular risk for developing and maintaining behavior problems and should be targeted for early intervention.
Emotion Regulation as a Moderator of Psychosocial Treatment Efficacy
To our knowledge, only two studies have examined the moderating effect of emotion regulation with psychosocial treatment efficacy in children with externalizing behavior problems. Both studies used correlates of heart rate variability as physiological indexes of emotion regulation because they are thought to be measures of parasympathetic influence of the autonomic nervous system29,30 and are associated with poor emotion regulation.31 Specifically, Beauchaine, Gartner, and Hagen32 found that lower vagal tone was associated with improved treatment response for adolescents with externalizing behaviors who received a multidisciplinary inpatient treatment consisting of a combination of recreational therapy, social skills training, individualized cognitive behavioral treatment, and family therapy. Similarly, the other study33 found that lower respiratory sinus arrhythmia (RSA) during a baseline period was associated with more improvements in child externalizing behavior following Parent-Child Interaction Therapy. Together, these results suggest that poor emotion regulation, assessed using physiological measures, is associated with improved psychosocial treatment efficacy.
These previous results seem counterintuitive, but could be explained by Belsky & Pluess’34 differential susceptibility hypothesis. Briefly, this framework proposes that children vary in their susceptibility (i.e. plasticity) to environmental influences and that some individuals are more susceptible to both positive and negative environments. Specifically, individual characteristics (e.g., negative emotionality) act as “vulnerability factors” when children are exposed to negative environments (e.g., harsh parenting) and as “plasticity factors” when children are exposed to positive environments (e.g., positive parenting), such that children with these characteristics are more adversely affected by negative environments and benefit more from positive environments. For example, Blair35 examined the effects of an early intervention for low birth-weight, preterm infants and found that infant negative emotionality moderated the relationship between intervention and outcome, such that children higher on negative emotionality benefited more from the intervention. In this case, negative emotionality could be conceptualized as representing a plasticity factor.
Temperamental characteristics, such as negative emotionality, also affect the development of children’s capacity to engage in more dynamic self-control processes, such as emotion regulation.5,36 To date, research has generally focused on poor emotion regulation as a vulnerability factor for children’s adaptive functioning, including social, behavioral, and academic outcomes.15,37,38 For example, poor emotion regulation has a greater negative influence on children’s adaptive functioning in the presence of a negative environmental factor, such as marital conflict or parental drinking.39 However, it remains unclear whether dynamic control processes, such as emotion regulation, also can act as plasticity factors, especially in response to an intervention. Examining the potential plasticity of emotion regulation is particularly relevant for children born preterm, who are more likely to exhibit poor self-regulation.7 An important preliminary step in determining whether dynamic processes such as emotion regulation can act as plasticity factors is to document that children with poor emotion regulation benefit most from an intervention designed to target behaviors closely tied to these self-regulatory processes (e.g., temper tantrums, behavioral compliance) via the promotion of positive parenting.
Current Study
Despite the limited work demonstrating a link between emotion regulation and treatment efficacy, emotion regulation in the two studies reviewed above was measured only using a physiological index. Emotion regulation can also be measured using behavioral coding schemes, which are less expensive and easier to use, thereby increasing the likelihood for use in clinical practice. In order to facilitate movement of psychosocial interventions from research to practice settings, Hoagwood, Burns, and Weisz40 recommend developing research protocols that are sensitive to the needs of the setting in which these service will ultimately be delivered. Thus, research examining treatment efficacy should use measures that are readily available and feasible in clinical settings, such as behavioral coding schemes. The current study would be the first to examine the moderating role of emotion regulation on treatment efficacy using a behavioral measure of emotion regulation. Based on previous findings with physiological data,32 as well as the differential susceptibility hypothesis discussed above, we hypothesized that higher levels of distress at baseline, as measured by the behavioral code of emotion regulation, would be associated with greater improvement after treatment, as measured by parent-reported externalizing behavior problems.
METHODS
Participants
Participants were 28 mothers and their young children (Mean age = 37.79 months, SD = 13.29) who were born < 37 weeks gestation and had borderline clinically-significant mother-reported externalizing behavior problems (T-score ≥ 60) on the Child Behavior Checklist (CBCL).41 Participants were referred between 2007 and 2008 by a neonatal follow up clinic (79%), other pediatric sites (9%), state-funded early intervention programs (6%), or self-referred by their mothers. For study inclusion, mothers had to score at least 75 on the Wechsler Abbreviated Scale of Intelligence (WASI),42 a cognitive screening measure, but no mother was excluded based on this criterion. Additionally, mothers had to be able to understand and speak English. Exclusion criteria for children included: major sensory impairments (e.g., deafness, blindness), major motor impairments (e.g., cerebral palsy significantly affecting mobility), and oxygen dependence for chronic lung disease. Of the 53 families who participated in the initial screening assessment, none were excluded based on these exclusion criteria, 11 were not interested in participating in the larger study and 9 did not meet entry criteria. The primary reason for study exclusion was low levels of externalizing behavior problems on the CBCL (n = 7; T-Score < 60). Children with symptoms of autism spectrum disorder were also excluded at the screening evaluation (n = 2). Following this initial screening, consent was obtained for 33 families, and 5 of these families did not attend the baseline assessment and did not continue participation in the study. The final sample of 28 children consisted of mostly boys (71%) and mostly from Caucasian families (82% White, 10% Biracial, 4% African American, 4% Asian, 21% Hispanic). The mean Hollingshead43 score was 43.39 (SD=13.21), suggesting families were mostly in the middle range of socioeconomic status.
Screening Measures
Child Behavior Checklist for 1½ to 5 Year Olds (CBCL 1 ½ –5)41
The CBCL was used to screen potential participants for externalizing behavior problems. This parent-report measure includes 99 items designed to measure the frequency of children’s behavioral and emotional problems. Raw scores on the Externalizing Problems scale (Cronbach’s α = .81 in the current sample) are converted to T-scores, with a mean of 50 and a standard deviation of 10. To be eligible for the study, a T-score greater than 60 (i.e. borderline clinically-significant range) was required on the Externalizing Problems scale.
Wechsler Abbreviated Scale of Intelligence (WASI)42
The WASI is a short and reliable measure of intelligence, and the two-subtest version yields a Full Scale Intelligence Quotient (FSIQ-2) with a mean score of 100 and a standard deviation of 15. The WASI FSIQ-2 correlated .87 with the FSIQ of the Wechsler Adult Intelligence Scale – Third Edition44 and has high test-retest reliability, ranging from .83 to .90,42 as well as good concurrent validity with other tests of intelligence.45 The WASI FSIQ-2 was used to exclude mothers with cognitive impairment.
Modified Checklist for Autism in Toddlers (M-CHAT)46
The M-CHAT is a 23-item parent-rating scale designed to identify children at risk for autism for children ages 18–48 months.47 Children are identified as at-risk on the M-CHAT with 3 or more failed responses. The standardization sample of 1293 children yielded high internal consistency (.85), as well as moderate sensitivity (.85–.87) and high specificity (.93–.99),46 and Cronbach’s α in the current sample was .56. Parent report in conjunction with clinical judgment was used for identification of autism in children older than 48 months.
Measures of Child Externalizing Behavior and Emotion Regulation
Eyberg Child Behavior Inventory (ECBI)48
The ECBI is a parent-rating scale which consists of 36 items and is designed to measure externalizing behavior problems in children. It yields an Intensity Scale and a Problem Scale. The Intensity Scale measures the frequency with which disruptive behavior occurs, whereas the Problem Scale measures how problematic the parent views their child’s behavior. For the current study, the ECBI Intensity Scale (Cronbach’s α = .90 in the current sample) was used as the primary measure of treatment efficacy and the dependent variable in the current study.
Emotion Regulation
Emotion regulation was measured using a behavioral coding scheme that has been successfully used in previous research with young children.18,49 The scheme includes a measure of global regulation, representing the child’s ability to regulate his or her affective response, ranging from 0 (dysregulated or no control of distress) to 4 (well regulated). Thus, higher global regulation scores represent lower levels of distress during a task. For the current study, participants were coded during a 10-min parent-child interaction that included both a 5-min child-directed play and a 5-min clean up. Coders were masked to treatment status, and 20% of the observations were coded a second time to assess reliability. Inter-rater reliability was assessed using Randolph’s free-marginal multi-rater kappa,50,51 as recommended by Brennan and Prediger,52 and was excellent (.96).
Study Design and Procedure
This study is a secondary analysis of a pilot randomized, controlled trial to determine the efficacy of Parent-Child Interaction Therapy (PCIT) compared to a waitlist control (WL) comparison group that has been published elsewhere.53 After consent and screening, participants were randomly assigned to an immediate treatment (IT) or WL group using two computer-generated random numbers lists, one for girls and one for boys. After the initial screening, families participated in a Time 1 assessment prior to randomization in which the mother completed the ECBI and participated in the observation with her child. Four months after the Time 1 assessment, families completed a Time 2 assessment, which included the same measures as the Time 1 assessment. All assessments were conducted in a clinic setting. Three participants from the IT group withdrew from treatment prior to the Time 2 assessment, but all participants in the WL group completed the Time 2 assessment.
Intervention Description
PCIT is a manualized parent-training intervention with extensive research demonstrating its efficacy and long-term maintenance in treating young children with disruptive behavior disorders54 and showing promise with other at-risk populations, such as children with abuse history,55 chronic illness,56 and mental retardation.57 Treatment progresses through two distinct phases: the Child-Directed Interaction (CDI) and the Parent-Directed Interaction (PDI). During CDI, the parents learn to follow their child’s lead in play and use differential attention to increase positive behaviors and decrease disruptive behaviors. During PDI, the parents learn to use effective commands and timeout for noncompliance. The therapist coaches each parent in-vivo through a one-way mirror (using a wireless headset) in their use of the skills with their child. Sessions were conducted once a week for approximately 1 hour in length. All therapy sessions were videotaped, and 50% were randomly selected and coded for integrity by a research assistant uninvolved in coding behavioral observations. Accuracy, defined as the percent with which the therapist adhered to key elements of each session detailed in the treatment manual, was 94% (range = 89% – 99%).
Data Analysis
The moderating effect of emotion regulation at Time 1 on the effect of PCIT on child disruptive behavior was examined using multiple regression analysis with product terms.58 The independent variable was treatment group and was dummy coded (0 = WL group and 1 = IT or PCIT group). The dependent variable was the Time 2 ECBI Intensity score, and the moderator variable was the index of emotion regulation (i.e., global regulation). All predictor variables were mean centered prior to the analyses. The Time 1 ECBI Intensity score was entered as a covariate in the regression equation, so the analysis reflects the effect of PCIT on covariate adjusted change in ECBI Intensity scores as moderated by emotion regulation. The moderating effect of emotion regulation was represented with a product term between the dummy variable for treatment group and global regulation. The analysis examined whether treatment effects differed depending on the children’s capacity for emotion regulation before treatment.
Outlier Analyses and Evaluation of Non-Normality
Prior to analysis, the data for the continuous variables were evaluated for multivariate outliers by examining leverage indices for each individual and defining an outlier as a leverage score four times greater than the mean leverage. No outliers were identified with this procedure.
RESULTS
Sample Characteristics
IT and WL families were compared on all demographic variables, and there were no demographic differences between groups (Table 1). There also were no differences between the IT and WL groups on baseline global regulation, t(26) = .51, p = .612, or ECBI Intensity scores, t(26) = -.13, p = .900. These results suggest successful random assignment of participants to group. Therefore, no additional demographic variables (e.g., child sex, child age, SES) were included as covariates in the moderation analysis. Global regulation was not related to ECBI Intensity scores at baseline, r(28) = −.23, p = .24. Mothers in the IT group reported lower ECBI Intensity scores at Time 2 than mothers in the WL group, t(26) = 7.01, p < .001, reflecting a main effect of treatment.
Table 1.
Demographic Characteristics of Groups
| Characteristic | M (SD) or percent | t(26) | χ2(1) | p | |
|---|---|---|---|---|---|
|
| |||||
| IT (n = 14) | WL (n = 14) | ||||
| Child Age (months) | 39.71 (14.17) | 36.50 (12.96) | −0.63 | -- | .537 |
| Birthweight (grams) | 1157.00 (651.48) | 1246.07 (563.23) | 0.39 | -- | .702 |
| Gestational Age (weeks) | 27.71 (3.99) | 28.93 (2.34) | 0.98 | -- | .335 |
| APGAR 1 mina | 3.70 (2.71) | 5.50 (2.47) | 1.63 | -- | .119 |
| APGAR 5 mina | 5.60 (2.84) | 7.08 (1.73) | 1.51 | -- | .147 |
| Perinatal Morbidity (%)b | 85.7 | 92.9 | -- | 0.37 | .541 |
| Child Sex (% male) | 71.4 | 71.4 | -- | 0.00 | 1.00 |
| Child Ethnicity (% minority) | 35.7 | 21.4 | -- | 0.70 | .403 |
| Hollingshead | 40.04 (12.86) | 46.75 (13.15) | 1.37 | -- | .184 |
| Time 1 ECBI Intensity Score | 147.93 (39.70) | 146.29 (28.08) | −0.13 | -- | .900 |
| Time 2 ECBI Intensity Score | 71.73 (15.34) | 147.79 (33.14) | 7.01 | -- | < .001 |
| Time 1 Global Regulation | 3.61 (0.63) | 3.71 (0.47) | 0.51 | -- | .612 |
Note: IT = Immediate Treatment; WL = Waitlist Control; ECBI = Eyberg Child Behavior Inventory.
APGAR scores, only available from 22 of the 28 children, are a simple method to assess the health of newborns (e.g., breathing, heart rate, skin color) measured both 1 and 5 min after birth. Scores ≥ 8 are considered normal, whereas lower scores may be indicative of longer-term difficulties.
Perinatal morbidity, dummy coded as a dichotomous variable (1 = yes, 0 = no), was based on maternal report of any of the following: newborn difficulties during the neonatal period (i.e., after birth), including respiratory distress; jaundice; problems with breathing, sucking, swallowing, or feeding; intraventricular bleeding; and other neonatal complications. All but one child (IT group) were admitted to the Neonatal Intensive Care Unit, which is common among preemies.
Moderation Analysis
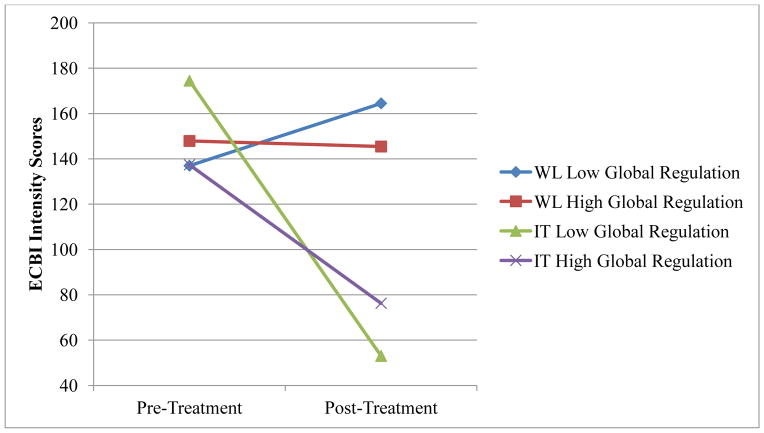
Table 2 displays the results of a linear regression analysis using the behavioral code of global regulation to predict Time 2 ECBI Intensity scores. The interaction between global regulation and treatment group was statistically significant (p < .05), suggesting that global regulation at baseline moderates the effect of PCIT on child externalizing behavior. Specifically, the coefficient suggests that for every 1 unit increase in baseline global regulation (i.e., less child distress), the mean difference between the IT and WL groups on the Time 2 ECBI score (holding the baseline ECBI score constant) is predicted to change, on average, by 49.97 units. The unstandardized regression coefficient for the treatment variable reflects a simple main effect for treatment. This coefficient was statistically significant (p < .001), indicating the children in the IT group had lower Time 2 ECBI scores than children in the WL group, holding all other variables (including global regulation) constant. The coefficient value of −76.68 suggests that when global regulation is at its mean value, the children in the IT group were predicted to have Time 2 ECBI Intensity scores, on average, 76.68 points lower than children in the WL group. This difference between the IT and WL groups is predicted to increase by 49.97 units with every 1 unit increase in baseline global regulation (e.g., for children with a global regulation score 1 unit higher than the mean, the IT group is predicted to have Time 2 ECBI scores 126.65 units lower than the WL group) and decrease by 49.97 units with every 1 unit decrease in baseline global regulation (e.g., for children with a global regulation score 1 unit lower than the mean, the IT group is predicted to have Time 2 ECBI scores 26.71 units lower than the WL group). Figure 1 illustrates the interaction between treatment group and baseline global regulation in predicting post-treatment ECBI Intensity scores. Figure 2 illustrates change in ECBI scores over time in both IT and WL groups across high and low global regulation.
Table 2.
Regressions Predicting Post-Treatment Behavior Problems from Baseline Emotion Regulation
| Time 2 ECBI Intensity Score B (SE) | |
|---|---|
| Global Regulation | |
| Time 1 ECBI Intensity Score | 0.43 (0.15)* |
| Time 1 Global Regulation | 4.44 (9.52) |
| Treatment Group | −76.68 (9.38)** |
| Time 1 Global Regulation * Treatment Group | 49.97 (19.42)* |
Note. ECBI = Eyberg Child Behavior Inventory.
R2 = .80, F(4, 20) = 19.33, p < .05.
p < .05;
p <.01.
Figure 1.
Regression Lines for the Relationship Between Treatment Group and Time 2 ECBI Intensity Scores as Moderated by Global Regulation
Note. ECBI = Eyberg Child Behavior Inventory.
Figure 2.
ECBI Intensity Scores at Pre- and Post-Treatment by Global Regulation and Treatment Group
Note. ECBI = Eyberg Child Behavior Inventory; WL = Waitlist Control; IT = Immediate Treatment.
Following procedures outlined by Aiken and West,59 the interaction was also plotted by regressing Time 2 ECBI Intensity scores(y) on treatment group (x) as a function of two values of global regulation, ZL and ZH (i.e., one standard deviation below the mean and one standard deviation above the mean, respectively). Unstandardized B was used to calculate the regression lines. As depicted in Figure 1, children’s low baseline global regulation (i.e. more distress) enhanced the positive effect of treatment on children’s post-treatment externalizing behavior problems. Additionally, t-tests were computed, using Hayes and Matthes’60 macro, to determine whether the slopes of the lines plotted in Figure 1 were significantly different from zero. The resulting t-tests indicated that in Figure 1, the slope for low global regulation was significantly different from zero, t(26) = −7.38, p < .01, b = −100.72, and the slope for high global regulation was significantly different from zero, t(26) = −3.51, p < .01, b = −48.71.
DISCUSSION
The purpose of the current pilot study was to examine the moderating effect of emotion regulation on treatment efficacy in young children born preterm with externalizing behavior problems. Specifically, this is the first study to examine this relationship using a behavioral coding scheme, a useful alternative to physiological measures in clinical practice. Children’s emotion regulation during free-play and clean-up tasks were coded using a behavioral coding scheme which codes global regulation, reflecting the child’s ability to regulate the intensity of his or her response to the environment. We found an interaction between baseline emotion regulation and treatment, such that children who displayed poorer capacity for emotion regulation at baseline improved significantly more after treatment on parent-reported externalizing behavior than children who displayed better emotion regulation at baseline. Results are consistent with our hypothesis, as well as with previous research findings of improved treatment efficacy for children with poor emotion regulation before treatment.32,33
The finding that children with poorer emotion regulation benefit most from treatment may seem somewhat counterintuitive. However, there could be several reasons for the current findings. For example, it is possible children who are born preterm and have poor emotion regulation are more impaired by their behavior problems than children with only one of these risk factors, and, thus, have more room for improvement in this area. Future studies should include measures of impairment to examine this possibility. Another potential reason for our findings is that mothers of children with poor emotion regulation, whose children are more likely to exhibit undesirable and noticeable behaviors such as temper tantrums, were more motivated to implement the treatment skills. Treatment was delivered equally to all families, but it is possible that more motivated mothers engaged in additional practice or implemented the skills more regularly.
Finally, it is possible that there is something about children born preterm who exhibit poor emotion regulation that makes them particularly good candidates for treatment with a psychosocial parenting intervention like PCIT. Lower vagal tone in preterm infants has been shown to be associated with poor maternal interaction quality,61 and the quality of parent-child interactions predicts emerging emotion regulation capacity in children born preterm.13 Similarly, preterm birth status is associated with poor interaction quality over the first year with both mothers and fathers,62 and preterm infants with difficulties in emotion regulation are particularly susceptible to the effects of early negative parenting.63 As previously described, the differential susceptibility hypothesis contends that children vary in their susceptibility to environmental influences, and PCIT aims to improve parent-child interactions through the use of positive parenting skills, differential attention, and effective discipline.34 Thus, it may be that children who are born preterm and exhibit poor capacity for emotion regulation benefit most from PCIT because their poor emotion regulation acts as a plasticity factor and the treatment targets exactly what they are most susceptible to – negative parenting.
To our knowledge, this is the first study to examine the moderating role of emotion regulation on treatment efficacy using a behavioral measure of emotion regulation. As Hoagwood and colleagues40 discuss, an important step in bridging the research to practice gap is making research protocols ecologically valid. Though physiological measures of emotion regulation may be readily available in research settings, they are not generally available in clinical practice. Behavioral measures, as compared to physiological measures, are relatively inexpensive, straightforward, and can be completed more quickly, all of which can maximize their utility in practice settings. This study replicated results of a previous study examining the role of RSA, a physiological measure of emotion regulation, on treatment efficacy in this sample. Thus, our findings suggest this behavioral coding scheme adequately measures capacity for emotion regulation and can be used to predict treatment efficacy in young children.
There were several limitations in this study. First, there was no control group of children born full-term to compare to the study participants. Future studies should examine the moderating role of emotion regulation on treatment efficacy in children born pre-term and full-term, in order to determine whether gestational age at birth affects this relationship. Second, the study was conducted with a small, relatively homogeneous sample. Thus, results may not be generalizable to larger populations, including children from low socioeconomic backgrounds, who are at higher risk for both prematurity and externalizing behavior problems.64 Third, though treatment dropout rate was relatively low (21%) compared to other psychosocial treatments (40% to 60%)65 it is possible attrition influenced the results. Subsequent analyses comparing individuals who dropped out of treatment to treatment completers revealed no differences between the groups on any of the measured included in the study. However, it is possible families who dropped out differed from other families on constructs not measured in the current study. Fourth, the correlation between RSA and emotion regulation in this sample was relatively low, r(22) = .27, p = .23, which brings into question how to best index emotion regulation. Future research should examine emotion regulation using multiple indicators in larger samples to further clarify the construct of emotion regulation.
Another limitation of the current study is the lack of a measure of impairment of behavioral functioning (e.g., school and family life). As discussed above, it is possible children with poor emotion regulation and behavior problems experience more impairment than other children, which may be driving the current results. We were unable to evaluate this relationship in the current study, however, because impairment was not measured. On a related note, mother’s motivation could be another factor driving the effects, as it is possible mothers of children with poor emotion regulation are more motivated and therefore benefit more from treatment. Mother’s motivation level also was not evaluated, so we were unable to determine whether it was a contributing factor in the current study. Another limitation of the current study is that we did not evaluate negative emotionality and are, thus, unable to directly test the differential susceptibility hypothesis. Future research should directly examine negative emotionality, as well as emotion regulation, in order to fully examine the extent to which the differential susceptibility hypothesis can help explain which children benefit most from psychosocial parenting interventions designed to promote positive parenting. Also, no follow-up data were collected, so we were not able to examine the moderating role of emotion regulation on child externalizing behavior past treatment completion. Finally, it is possible that mothers’ awareness that they received treatment influenced their reporting of their children’s post-treatment behavior problems. However, objective reports of child compliance and parent skill acquisition also improved, suggesting changes in child behavior problems following treatment were not solely due to potential demand characteristics.53
Despite these limitations, this pilot study replicates the finding that children born preterm who exhibit poor emotion regulation and externalizing behavior problems display an enhanced treatment response compared to children without emotion regulation difficulties. Additionally, this study was the first to examine this relationship using a behavioral measure of emotion regulation, which can be readily implemented in practice settings. Together, these findings have implications for improved treatment for children served in practice settings, as children’s emotion regulation could be quickly evaluated during initial assessments and results could help to guide treatment decision-making. Future research should examine this relationship using both physiological and behavioral measures of emotion regulation in larger samples, in order to directly compare the utility of these measures. Understanding the possible mechanisms responsible for this differential treatment response would be another important area of future research.
SUMMARY
Children who are born preterm are more likely to exhibit poor emotion regulation and elevated externalizing behavior problems. Examining the link between emotion regulation and externalizing behavior can help to enhance our understanding of the individual factors associated with treatment efficacy, particularly among children born preterm. This pilot study examined child emotion regulation as a moderator of treatment efficacy for young children born preterm. In this randomized controlled trial, 28 mother-child dyads were randomly assigned to an immediate treatment or waitlist control group. A behavioral coding system was used to index child emotion regulation during a 10-min parent-child interaction at baseline. Results demonstrated a significant interaction between baseline emotion regulation and treatment condition, such that higher levels of distress at baseline were associated with greater improvements in child externalizing behavior following treatment. The current study replicates similar findings in a previous study, but is the first to examine this relationship using a behavioral measure of emotion regulation. A behavioral coding system could be readily implemented in practice settings to evaluate children’s emotion regulation at intake to help guide treatment decision-making.
Acknowledgments
Source of Funding: This study was funded by NICHD (F32 HD056748) and NIMH (K23 MH085659)
Footnotes
Conflicts of Interest: The authors report no conflicts of interest.
References
- 1.Carter AS, Briggs-Gowan MJ, Davis NO. Assessment of young children’s social-emotional development and psychopathology: recent advances and recommendations for practice. J Child Psychol Psychiatry. 2004;45(1):109–134. doi: 10.1046/j.0021-9630.2003.00316.x. [DOI] [PubMed] [Google Scholar]
- 2.Lahey BB, Loeber R, Burke JD, Applegate B. Predicting future antisocial personality disorder in males from a clinical assessment in childhood. J Consult Clin Psychol. 2005;73:389–399. doi: 10.1037/0022-006X.73.3.389. [DOI] [PubMed] [Google Scholar]
- 3.Campbell SB, Shaw DS, Gilliom M. Early externalizing behavior problems: Toddlers and preschoolers at risk for later maladjustment. Dev Psychopathol. 2000;12(03):467–488. doi: 10.1017/s0954579400003114. [DOI] [PubMed] [Google Scholar]
- 4.Loeber R, Green SM, Lahey BB, Kalb L. Physical fighting in childhood as a risk factor for later mental health problems. J Am Acad Child Adolesc Psychiatry. 2000;39:421–428. doi: 10.1097/00004583-200004000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Keenan K, Shaw DS. Starting at the Beginning: Exploring the Etiology of Antisocial Behavior in the First Years of Life. In: Lahey BB, Moffitt TE, Caspi A, editors. Causes of Conduct Disorder and Juvenile Delinquency. New York, NY: Guilford Press; 2003. pp. 153–181. [Google Scholar]
- 6.Aarnoudse-Moens CS, Weisglas-Kuperus N, van Goudoever JB, Oosterlaan J. Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics. 2009;124:717–728. doi: 10.1542/peds.2008-2816. [DOI] [PubMed] [Google Scholar]
- 7.Maclean PC, Erickson SJ, Lowe JR. Comparing emotional reactivity and regulation in infants born ELGA and VLGA. Infant Behav Dev. 2009;32(3):336–339. doi: 10.1016/j.infbeh.2009.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lowe J, Woodward B, Papile LA. Emotional regulation and its impact on development in extremely low birth weight infants. J Dev Behav Pediatr. 2005;26:209–213. doi: 10.1097/00004703-200506000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Loeber R, Pardini D, Homish L, Wei EH, Crawford AM, Farrington DP. The Prediction of Violence and Homicide in Young Men. J Consult Clin Psych. 2005;73(6):1074–1088. doi: 10.1037/0022-006X.73.6.1074. [DOI] [PubMed] [Google Scholar]
- 10.Keenan, Gunthorpe, Young Patterns of cortisol reactivity in African-American neonates from low-income environments. Dev Psychobiol. 2002;41(3):265–276. doi: 10.1002/dev.10048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bates JE, Schermerhorn AC, Goodnight JA. Temperament and personality through the life span. Hoboken, NJ, US: John Wiley & Sons Inc, Hoboken, NJ; 2010. [Google Scholar]
- 12.Vaughn BE, Kopp CB, Krakow JB. The emergence and consolidation of self-control from eighteen to thirty months of age: Normative trends and individual differences. Child Dev. 1984;55(3):990–1004. [PubMed] [Google Scholar]
- 13.Clark CAC, Woodward LJ, Horwood LJ, Moor S. Development of emotional and behavioral regulation in children born extremely preterm and very preterm: Biological and social influences. Child Dev. 2008;79(5):1444–1462. doi: 10.1111/j.1467-8624.2008.01198.x. [DOI] [PubMed] [Google Scholar]
- 14.Berking M, Wupperman P. Emotion regulation and mental health: Recent finding, current challenges, and future directions. Curr Opin Psychiatry. 2012;25(2):128–134. doi: 10.1097/YCO.0b013e3283503669. [DOI] [PubMed] [Google Scholar]
- 15.Eisenberg N, Cumberland A, Spinrad TL, et al. The Relations of Regulation and Emotionality to Children’s Externalizing and Internalizing Problem Behavior. Child Dev. 2001;72(4):1112–1134. doi: 10.1111/1467-8624.00337. [DOI] [PubMed] [Google Scholar]
- 16.Gilliom M, Shaw DS, Beck JE, Schonberg MA, Lukon JL. Anger regulation in disadvantaged preschool boys: Strategies, antecedents, and the development of self-control. Dev Psychol. 2002;38(2):222–235. doi: 10.1037//0012-1649.38.2.222. [DOI] [PubMed] [Google Scholar]
- 17.Rubin KH, Coplan RJ, Fox NA, Calkins SD. Emotionality, emotion regulation, and preschoolers’ social adaptation. Dev Psychopathol. 1995;7(1):49–62. [Google Scholar]
- 18.Calkins SD, Dedmon SE. Physiological and behavioral regulation in two-year-old children with aggressive/destructive behavior problems. J Abnorm Child Psychol. 2000;28(2):103–118. doi: 10.1023/a:1005112912906. [DOI] [PubMed] [Google Scholar]
- 19.Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand KJS. Cognitive and behavioral outcomes of school-aged children who were born preterm: A meta-analysis. JAMA. 2002;288(6):728–737. doi: 10.1001/jama.288.6.728. [DOI] [PubMed] [Google Scholar]
- 20.Scott MN, Taylor HG, Fristad MA, et al. Behavior Disorders in Extremely Preterm/Extremely Low Birth Weight Children in Kindergarten. J Dev Behav Pediatr. 2012;33(3):202–213. doi: 10.1097/DBP.0b013e3182475287. 210.1097/DBP.1090b1013e3182475287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farooqi A, Hägglöf B, Sedin G, Gothefors L, Serenius F. Mental Health and Social Competencies of 10- to 12-Year-Old Children Born at 23 to 25 Weeks of Gestation in the 1990s: A Swedish National Prospective Follow-up Study. Pediatrics. 2007;120(1):118–133. doi: 10.1542/peds.2006-2988. [DOI] [PubMed] [Google Scholar]
- 22.Stjernqvist K, Svenningsen NW. Ten-year follow-up of children born before 29 gestational weeks: health, cognitive development, behaviour and school achievement. Acta Pædiatr. 1999;88(5):557–562. doi: 10.1080/08035259950169594. [DOI] [PubMed] [Google Scholar]
- 23.Gray RF, Indurkhya A, McCormick MC. Prevalence, Stability, and Predictors of Clinically Significant Behavior Problems in Low Birth Weight Children at 3, 5, and 8 Years of Age. Pediatrics. 2004;114(3):736–743. doi: 10.1542/peds.2003-1150-L. [DOI] [PubMed] [Google Scholar]
- 24.Bul KCM, van Baar AL. Behavior problems in relation to sustained selective attention skills of moderately preterm children. J Dev Phys Disabil. 2012;24(2):111–123. doi: 10.1007/s10882-011-9258-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strang-Karlsson, Räikkönen K, Kajantie E, et al. Sleep quality in young adults with very low birth weight--The Helsinki study of very low birth weight adults. J Pediatr Psychol. 2008;33(4):387–395. doi: 10.1093/jpepsy/jsm125. [DOI] [PubMed] [Google Scholar]
- 26.Evrard D, Charollais A, Marret S, Radi S, Rezrazi A, Mellier D. Cognitive and emotional regulation developmental issues in preterm infants 12 and 24 months after birth. Eur J Dev Psychol. 2010;8(2):171–184. [Google Scholar]
- 27.Weinberg MK, Tronick EZ. Beyond the Face: An Empirical Study of Infant Affective Configurations of Facial, Vocal, Gestural, and Regulatory Behaviors. Child Dev. 1994;65(5):1503–1515. doi: 10.1111/j.1467-8624.1994.tb00832.x. [DOI] [PubMed] [Google Scholar]
- 28.Spittle AJ, Treyvaud K, Doyle LW, et al. Early Emergence of Behavior and Social-Emotional Problems in Very Preterm Infants. J Am Acad Child Adolesc Psychiatry. 2009;48(9):909–918. doi: 10.1097/CHI.0b013e3181af8235. [DOI] [PubMed] [Google Scholar]
- 29.Beauchaine TP. Vagal tone, development, and Gray’s motivational theory: toward an integrated model of autonomic nervous system functioning in psychopathology. Dev Psychopathol. 2001;13:183–214. doi: 10.1017/s0954579401002012. [DOI] [PubMed] [Google Scholar]
- 30.Porges SW. The polyvagal theory: phylogenetic substrates of a social nervous system. Int J Psychophysiol. 2001;42:123–146. doi: 10.1016/s0167-8760(01)00162-3. [DOI] [PubMed] [Google Scholar]
- 31.Porges SW. The polyvagal perspective. Biol Psychol. 2007;74:116–143. doi: 10.1016/j.biopsycho.2006.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beauchaine TP, Gartner J, Hagen B. Comorbid depression and heart rate variability as predictors of aggressive and hyperactive symptom responsiveness during inpatient treatment of conduct-disordered, ADHD boys. Aggressive Behav. 2000;26:425–441. [Google Scholar]
- 33.Bagner DM, Graziano PA, Jaccard J, Sheinkopf SJ, Vohr BR, Lester BM. An Initial Investigation of Baseline Respiratory Sinus Arrhythmia as a Moderator of Treatment Outcome for Young Children Born Premature With Externalizing Behavior Problems. Behav Ther. 2012;43(3):652–665. doi: 10.1016/j.beth.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Belsky J, Pluess M. Beyond diathesis stress: Differential susceptibility to environmental influences. Psychol Bull. 2009;135(6):885–908. doi: 10.1037/a0017376. [DOI] [PubMed] [Google Scholar]
- 35.Blair C. Early intervention for low birth weight, preterm infants: The role of negative emotionality in the specification of effects. Dev Psychopathol. 2002;14(2):311–332. doi: 10.1017/s0954579402002079. [DOI] [PubMed] [Google Scholar]
- 36.Rothbart MK, Ahadi SA. Temperament and the development of personality. J Abnorm Psychol. 1994;103(1):55. doi: 10.1037//0021-843x.103.1.55. [DOI] [PubMed] [Google Scholar]
- 37.Graziano PA, Reavis RD, Keane SP, Calkins SD. The role of emotion regulation in children’s early academic success. J Sch Psychol. 2007;45(1):3–19. doi: 10.1016/j.jsp.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blair C. School readiness. Am Psychol. 2002;57(2):111–127. doi: 10.1037//0003-066x.57.2.111. [DOI] [PubMed] [Google Scholar]
- 39.El-Sheikh M, Benjamin Hinnant J, Erath S. Developmental trajectories of delinquency symptoms in childhood: The role of marital conflict and autonomic nervous system activity. J Abnorm Psychol. 2011;120(1):16. doi: 10.1037/a0020626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hoagwood K, Burns BJ, Weisz JR. A profitable conjunction: From science to service in children’s mental health. In: Burns BJ, Hoagwood K, editors. Community treatment for youth: Evidence-based interventions for severe emotional and behavioral disorders. NY: Oxford University Press; 2002. pp. 327–338. [Google Scholar]
- 41.Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- 42.Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: Psychological Corporation; 1999. [Google Scholar]
- 43.Hollingshead. A Four Factor Index of Social Status. New Haven, CT: Yale University; 1975. [Google Scholar]
- 44.Wechsler D. Wechsler Adult Intelligence Scale - Third Edition. San Antonio, TX: The Psychological Corporation; 1997. [Google Scholar]
- 45.Hays JR, Reas DL, Shaw JB. Concurrent validity of the Wechsler abbreviated scale of intelligence and the Kaufman brief intelligence test among psychiatric inpatients. Psychol Rep. 2002;90:355–359. doi: 10.2466/pr0.2002.90.2.355. [DOI] [PubMed] [Google Scholar]
- 46.Robins DL, Fein D, Barton ML, Green JA. The Modified Checklist for Autism in Toddlers: An initial study investigating the early detection of autism and pervasive developmental disorders. J Autism Dev Disord. 2001;31(2):131–144. doi: 10.1023/a:1010738829569. [DOI] [PubMed] [Google Scholar]
- 47.Snow AV, Lecavalier L. Sensitivity and specificity of the Modified Checklist for Autism in Toddlers and the Social Communication Questionnaire in preschoolers suspected of having pervasive developmental disorders. Autism. 2008;12(6):627–644. doi: 10.1177/1362361308097116. [DOI] [PubMed] [Google Scholar]
- 48.Eyberg SM, Pincus D. Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Inventory: Professional Manual. Odessa, FL: Psychological Assessment Resources; 1999. [Google Scholar]
- 49.Graziano PA, Keane SP, Calkins SD. Maternal Behaviour and Children’s Early Emotion Regulation Skills Differentially Predict Development of Children’s Reactive Control and Later Effortful Control. Infant Child Dev. 2010;19:333–353. doi: 10.1002/icd.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Randolph JJ. Free-Marginal Multirater Kappa: An Alternative to Fleiss’ Fixed-Marginal Multirater Kappa. Joensuu Learning and Instruction Symposium; Joensuu, Finland. 2005. [Google Scholar]
- 51.Warrens MJ. Inequalities between kappa and kappa-like statistics for k×k tables. Psychometrika. 2010;75(1):176–185. [Google Scholar]
- 52.Brennan RL, Prediger DJ. Coefficient kappa: Some uses, misuses, and alternatives. Educ Psychol Meas. 1981;41(3):687–699. [Google Scholar]
- 53.Bagner DM, Sheinkopf SJ, Vohr BR, Lester BM. Parenting Intervention for Externalizing Behavior Problems in Children Born Premature: An Initial Examination. J Dev Behav Pediatr. 2010;31(3):209–216. doi: 10.1097/DBP.0b013e3181d5a294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Eyberg SM, Nelson MM, Boggs SR. Evidence-Based Psychosocial Treatments for Children and Adolescents With Disruptive Behavior. J Clin Child Adolesc. 2008;37(1):215–237. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- 55.Chaffin M, Silovsky JF, Funderburk B, et al. Parent-Child Interaction Therapy With Physically Abusive Parents: Efficacy for Reducing Future Abuse Reports. J Consult Clin Psych. 2004;72(3):500–510. doi: 10.1037/0022-006X.72.3.500. [DOI] [PubMed] [Google Scholar]
- 56.Bagner DM, Fernandez MA, Eyberg SM. Parent-child interaction therapy and chronic illness: A case study. J Clin Psychol Med S. 2004;11(1):1–6. [Google Scholar]
- 57.Bagner DM, Eyberg SM. Parent-Child Interaction Therapy for Disruptive Behavior in Children with Mental Retardation: A Randomized Controlled Trial. J Clin Child Adolesc. 2007;36(3):418–429. doi: 10.1080/15374410701448448. [DOI] [PubMed] [Google Scholar]
- 58.Jaccard J, Guilamo-Ramos V, Johannson M, Bouris A. Multiple regression analyses in clinical child and adolescent psychology. J Clin Child Adolesc. 2006;35:456–479. doi: 10.1207/s15374424jccp3503_11. [DOI] [PubMed] [Google Scholar]
- 59.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- 60.Hayes AF, Matthes J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Beh Res Methods. 2009;41(3):924–936. doi: 10.3758/BRM.41.3.924. [DOI] [PubMed] [Google Scholar]
- 61.Feldman R. From biological rhythms to social rhythms: Physiological precursors of mother-infant synchrony. Dev Psychol. 2006;42(1):175–188. doi: 10.1037/0012-1649.42.1.175. [DOI] [PubMed] [Google Scholar]
- 62.Harrison MJ, Magill-Evans J. Mother and father interactions over the first year with term and preterm infants. Res Nurs Health. 1996;19(6):451–459. doi: 10.1002/(SICI)1098-240X(199612)19:6<451::AID-NUR1>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 63.Poehlmann J, Schwichtenberg AJM, Shlafer RJ, Hahn E, Bianchi J-P, Warner R. Emerging self-regulation in toddlers born preterm or low birth weight: Differential susceptibility to parenting. Dev Psychopathol. 2011;23(1):177–193. doi: 10.1017/S0954579410000726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Qi CH, Kaiser AP. Behavior Problems of Preschool Children From Low-Income Families: Review of the Literature. Top Early Child Spec. 2003;23(4):188–216. [Google Scholar]
- 65.Wierzbicki M, Pekarik G. A meta-analysis of psychotherapy dropout. Prof Psychol-Res Pr. 1993;24(2):190. [Google Scholar]