Abstract
Previous PET imaging studies have demonstrated mixed findings regarding dopamine D2/D3 receptor availability in obese relative to non-obese humans. Nonspecific D2/D3 radioligands do not allow for separate estimation of D2 receptor (D2R) and D3 receptor (D3R) subtypes of the D2 receptor family, which may play different roles in behavior and are distributed differently throughout the brain. These radioligands are also displaceable by endogenous dopamine, confounding interpretation of differences in receptor availability with differing levels of dopamine release. The present study used PET imaging with the D2R-selective radioligand (N-[11C] methyl)benperidol ([11C]NMB), which is non-displaceable by endogenous dopamine, to estimate D2R specific binding (BPND) and its relationship to body mass index (BMI) and age in 15 normal-weight (mean BMI = 22.6 kg/m2) and 15 obese (mean BMI = 40.3 kg/m2) men and women. Subjects with illnesses or taking medications that interfere with dopamine signaling were excluded. Striatal D2R BPND was calculated using the Logan graphical method with cerebellum as a reference region. D2R BPND estimates were higher in putamen and caudate relative to nucleus accumbens, but did not differ between normal-weight and obese groups. BMI values did not correlate with D2R BPND. Age was negatively correlated with putamen D2R BPND in both groups. These results suggest that altered D2R specific binding is not involved in the pathogenesis of obesity per se and underscore the need for additional studies evaluating the relationship between D3R, dopamine reuptake, or endogenous dopamine release and human obesity.
Keywords: dopamine, obesity, NMB
INTRODUCTION
Obesity is a major health problem worldwide and is associated with serious medical comorbidities and economic consequences (Shamseddeen et al., 2011). Obesity may be neurobiologically and behaviorally similar to drug addiction since both are associated with similar alterations in dopaminergic transmission in rodent models (de Jong et al., 2012). Human studies indicate that drug addiction is associated with reduced striatal D2/D3 dopamine receptor availability, as evaluated in vivo with PET imaging (Hietala et al., 1994; Volkow et al., 1996; Volkow et al., 2001; Wang et al., 1997). However, the relationship between obesity and the dopaminergic system in people remains unclear due to conflicting results among PET studies. Notably, several groups (de Weijer et al., 2011; Haltia et al. 2007; Wang et al., 2001) found that obesity is associated with a decrease while Dunn et al. (2012) found an increase in striatal D2/D3 receptor availability.
The complexity of evaluating striatal dopaminergic signaling may contribute to discrepant results in studies of normal-weight and obese people. PET and SPECT imaging studies of D2/D3 receptor availability in obesity have used [11C]raclopride (Haltia et al., 2007; Wang et al., 2001), [18F]fallypride (Dunn et al., 2012) and [123I]IBZM (de Weijer et al., 2011). These radioligands have important limitations. First, these radioligands do not distinguish between D2 (D2R) and D3 (D3R) receptor subtypes of the D2 dopamine receptor family (Elsinga et al., 2006; Mukherjee et al., 1999; Videbaek et al., 2000). D2R and D3R have different, although somewhat overlapping, distributions throughout the human brain (Beaulieu and Gainetdinov, 2011) and thus could have separate functional roles in reward-related behaviors. Second, endogenous dopamine release decreases specific binding of [11C]raclopride, [18F]fallypride, or [123I]IBZM (Dewey et al., 1993; Laruelle et al., 1995; Riccardi et al., 2006), making these radioligands useful to measure endogenous dopamine release but confounding interpretation of D2/D3 receptor availability in previous studies.
Based on evidence for decreased striatal D2R specific binding and decreased D2/D3 receptor availability in obese rodents (de Jong et al., 2012) and decreased D2/D3 receptor availability in obese humans (de Weijer et al., 2011; Haltia et al., 2007; Wang et al., 2001), we hypothesized that striatal D2R specific binding would be decreased in obese relative to normal-weight men and women. We carefully controlled for age and excluded those who had psychiatric and diabetic conditions that are associated with dopaminergic dysfunction (Blum et al., 2012; DeFronzo, 2011). We used the radioligand (N-[11C] methyl)benperidol ([11C]NMB), which has unique receptor-binding properties. NMB is more than 200 times as selective for D2R than D3R (Karimi et al., 2011), and is specific to D2R over other types of brain receptors (Arnett et al., 1985; Moerlein et al., 1995, 1997; Suehiro et al., 1990). In addition, NMB is non-displaceable by release of endogenous dopamine (Moerlein et al., 1997), which allows an assessment of D2R specific binding unconfounded by synaptic dopamine concentration. Note that NMB can be labeled with either 11C or 18F without changing the molecular structure of the D2 ligand (Moerlein et al., 1992; Moerlein et al., 2004). Thus, [11C]NMB and [18F]NMB are not analogs but are chemically (and therefore pharmacologically) identical, and differ only in being labeled with 11C or 18F, respectively.
MATERIALS AND METHODS
Participants
Fifteen normal-weight (BMI 18.9 – 27.7 kg/m2; age 22.4 – 39.9 years; 4 men) and 15 obese (BMI 33.2 – 47 kg/m2; age 25.4 – 40.9 years; 3 men) men and women participated in this study (Table 1). All potential participants completed a comprehensive medical evaluation, including medical history and physical examination, routine blood tests, hemoglobin A1C, and an oral glucose tolerance test (OGTT). Those with self-reported history of diabetes, A1C ≥ 6.5% (48 mmol/mol), or OGTT results that demonstrated impaired fasting glucose, impaired oral glucose tolerance, or diabetes (≥ 200 mg/dl, (American Diabetic Association, 2010)) were excluded. Participants were also screened for neurological and psychiatric conditions by neurological examination, psychiatric interview (Structured Clinical Interview for DSM-IV (SCID, Steiner et al., 1995), Beck Depression Inventory (BDI-II, Beck et al., 1996), the Wechsler Abbreviated Scale of Intelligence (WASI, Wechsler, 1999), and Part A of the Adult ADHD Self-Report Scale Symptom Checklist (ASRS-v1.1, Kessler et al., 2005). Individuals diagnosed with lifetime psychosis, mania, substance dependence, major depression, social phobia, eating disorders and panic disorder, parkinsonism, IQ <80 or had any psychiatric or neurologic illness (e.g. drug abuse, Parkinson disease, Tourette syndrome, stroke) that could affect the interpretation of the data were excluded from the study. Individuals who smoked, were pregnant or lactating, were postmenopausal, took medications that could influence the study results such as dopamine agonist or antagonist treatment (e.g. antipsychotics or metoclopramide) were excluded. All participants signed informed consents before participating in the study, which was approved by the Washington University Human Research Protection Office.
Table 1.
Participant Characteristics
| Normal-weight (n = 15) | Obese (n = 15) | |
|---|---|---|
| BMI Mean (S.D.) | 22.6 kg/m2 (2.2)*** | 40.3 kg/m2 (4.9) |
| Age Mean (S.D.) | 29.7 years (5.6) | 32.5 years (5.9) |
| Education Mean (S.D.) | 16.2 years (1.4) | 15.3 years (1.8) |
| Ethnicity (Caucasian, African American, Hispanic) | 14, 1, 0 | 8, 6, 1 |
| BDI-II Mean (S.D.) | 3.4 (4.6) | 5.9 (5.7) |
| WASI IQ Mean (S.D.)† | 113 (13.6) | 104.5 (10.7) |
| ASRS Part A Mean (S.D.) | 0.9 (1.2) | 1.5 (1.8) |
BMI, body mass index; BDI-II, Beck Depression Inventory-II; WASI IQ, Wechsler Abbreviated Scale of Intelligence Intelligence Quotient; ASRS, Adult ADHD Self-Report Scale Symptom Checklist v1.1, Part A.
p < 0.001 relative to obese group.
WASI IQ scores were not obtained for 3 normal-weight participants.
Radiopharmaceutical preparation
The synthesis of [11C]NMB is an automated adaptation of a published method (Moerlein et al., 2004, 2010). [11C]CO2 was produced via the 14N(p,α)11C reaction on the Washington University JSW BC-16/8 cyclotron, and converted to [11C]CH3I using a GE PETtrace MeI MicroLab (Sandell et al., 2000). [11C]CH3I, benperidol and base were heated to 90°C for 10 minutes, and [11C]NMB isolated using reversed-phase preparative HPLC. Drug reformulation used solid-phase extraction technology to give [11C]NMB in 10% ethanol in Sodium Chloride for Injection, USP. The product was terminally sterilized (0.2 μm filter), and had a radiochemical purity ≥ 95% and specific activity ≥ 1066 Ci/mmol (39 TBq/mmol).
PET acquisition
[11C]NMB (6.4 – 18.1 mCi) was administered intravenously over 20 s through a plastic catheter inserted in an arm vein. For each subject, < 7.3 μg of unlabeled NMB was injected. PET scans were done with Siemens/CTI ECAT EXACT HR+, which has 32 rings of BGO detector elements and acquires 63 simultaneous slices with 2.4 mm spacing with an axial FOV of 15.5 cm. Three retractable 68Ge rod sources are used for transmission scans to measure individual attenuation factors. Transaxial and axial spatial resolution at slice center are 4.3 mm and 4.1 mm full width half maximum (FWHM) in 3D mode (Brix et al., 1997). Emission data were collected in 3D mode for 2 hours with a total of 30 frames: 3 @ 1 min, 4 @ 2 min, 3 @ 3 min, 20 @ 5 min. PET scans were reconstructed with filtered back projection with ramp filter cut off at the Nyquist frequency and included attenuation, scatter and randoms correction.
MRI acquisition
All participants underwent MRI scans in the Siemens MAGNETOM Tim Trio 3T scanner using a 3-D MPRAGE sequence (TR=2400 ms, TE=3.16 ms, flip angle=8, 176 sagittally-oriented frames, FOV=256 mm; voxels=1×1×1 mm).
ROI-based analysis
For each participant, the dynamic PET image frames were co-registered to each other and to the participant's MPRAGE image as described (Eisenstein et al., 2012). MR-defined ROIs and PET data were resampled in Talairach atlas space to (2 mm)3 (Hershey et al., 2003).
Three bilateral striatal regions of interest (ROIs) (putamen, caudate and nucleus accumbens) and cerebellum (the reference region) were identified on each partcipant's MPRAGE using FreeSurfer (available at http://surfer.nmr.mgh.harvard.edu). To minimize partial volume effects, putamen and caudate regions were eroded by one surface voxel using a gaussian smoothing filter combined with thresholding, resulting in removal of 2 mm from the surfaces of these regions (Eisenstein et al., 2012). Nucleus accumbens was not large enough to erode.
The ROIs were resampled in the same Talairach atlas space as the PET images. Decay-corrected tissue activity curves were then extracted from the dynamic PET data for each participant. D2R specific binding potential (BPND) was calculated for each ROI using the Logan graphical method with cerebellum as a reference region (Logan et al., 1996) as previously validated for [18F]NMB with a 3-compartment tracer kinetic model and a graphical method requiring arterial input (Antenor-Dorsey et al., 2008; Eisenstein et al., 2012). The Logan method is appropriate for this analysis because the cerebellum has negligible specific binding for NMB in healthy subjects (Antenor-Dorsey et al., 2008) and it is unlikely that obese subjects would develop specific binding sites in the cerebellum. Furthermore, even if there are differences in the obese group in uptake of [11C] NMB into the cerebellum such as changes in local blood flow, blood brain barrier permeability, or non-specfic binding, the basic assumption of the Logan reference region approach assumes that these changes, similar to non-specific binding, also occur in the target ROI for that subject group or individual. Thus the calculated BPND takes this variation into consideration. Slopes were obtained from Logan plot points for data acquired 60–120 min after [11C]NMB injection. BPND's were averaged for left and right caudate, putamen and nucleus accumbens to minimize regional comparisons and because no evidence suggested that these findings would be asymmetric.
Voxel-based analysis
A voxel-based analysis was performed to detect possible differences in D2R specific binding between normal-weight and obese groups that were not detected with ROI-based analyses as in (Haltia et al., 2007). The freely available PVEOUT software (https://nru.dk/pveout/index.php) and co-registered structural MR images for each subject were used to correct for partial volume effects (PVE) using an published method (Quarentelli et al., 2004; Harri et al., 2007). [11C]NMB PET images corrected for PVE were made for each individual. BPND voxel maps were made for each subject using these images and compared across normal-weight and obese groups at the voxel level using SPM8 (http://www.fil.ion.ucl.ac.uk/spm).
Statistical analyses
Distribution normality for continuous variables was assessed using D'Agostino and Pearson omnibus normality tests in the normal-weight and obese groups separately. Ethnicity and gender distributions between normal-weight and obese groups was assessed with Chi-square tests. To exclude the possibility that differing distributions of ethnicity in normal-weight and obese groups would affect results, participant characteristics and striatal BPND estimates were compared between Caucasian and African American obese subjects with between-subjects Student's t-tests or univariate general linear models (GLM) using age as a covariate. BMI, age, education level, BDI and ASRS Part A scores were compared between groups with between-subjects Student t-tests, or, in the case of non-normal distributions, non-parametric Mann-Whitney U-tests. BPND estimates for putamen, caudate and nucleus accumbens were compared between groups with a repeated measures GLM using age as a covariate. In an effort to be consistent with the ROIs in similar studies (Volkow et al., 2008; Wang et al., 2001) we also compared a combined striatal BPND ROI (average of putamen and caudate BPND values) between groups with a univariate GLM controlling for age. Relationships between BMI, age and D2R BPND were calculated using Pearson's r or Spearman's rho for each ROI. For voxel-based SPM8 analysis, groups were compared with Student's t-tests using age as a covariate. Results were deemed significant at α ≤ 0.05.
Power analyses
The power of our study to detect differences in D2R BPND estimates between normal-weight and obese groups as well as to detect correlations between D2R BPND estimates and BMI in the obese group was calculated based on results from previous studies of D2/D3 receptor availability (de Weijer et al., 2011; Dunn et al., 2012; Wang et al., 2001) and our own using G*Power 3, available at http://www.psycho.uni-duesseldorf.de/abteilungen/aap/gpower3 (Faul et al., 2007). The effect sizes for differences in striatal D2/D3 receptor availability between non-obese and obese groups using [11C]raclopride (Wang et al., 2001) and [123I]IBZM (de Weijer et al., 2011) were estimated to be 1.35 and 1.13 (Cohen's d), respectively. Assuming similar effects in our study, our sample size of 15 individuals per group had power between 0.85 and 0.95 to detect differences of these effect sizes between normal-weight and obese groups. The correlation between striatal D2/D3 receptor availability and BMI in the obese group was −0.84 using [11C]raclopride (Wang et al., 2001) and 0.5–0.6 using [18F]fallypride (Dunn et al., 2012). Our sample size had power of 0.5–0.97 to detect these medium to large effects.
RESULTS
Assessment of normality
All continuous dependent measures had normal distributions in both groups (p ≥ 0.07 for all tests) except for BDI (p = 0.01) and ASRS Part A (p < 0.05) scores in the normal-weight group and age in the obese group (p = 0.05). These variables were therefore treated as non-normally distributed in subsequent analyses.
Participant characteristics and striatal BPND estimates across ethnicity and gender
Ethnicity distributions between normal-weight and obese groups significantly differed (χ2(2) = 6.2, p = 0.05, Table 1), while gender distribution did not (χ2(1) = 0.19, p = 0.67). BMI, age, and years of education did not differ between obese Caucasian and African American subjects (p ≥ 0.2). When controlling for age, a factor known to negatively correlate with striatal dopamine receptor availability and specific binding (Antonini and Leenders, 1993; Brucke et al., 1993; Eisenstein et al., 2012; Wang et al., 2001), striatal BPND did not differ between Caucasians and African Americans in the obese group (p ≥ 0.14 for all comparisons). To further determine whether gender and ethnicity differences were masking a relationship between obesity and striatal BPND, univariate GLM analyses covarying age, were performed for each striatal region in female Caucasians. Normal-weight and obese Caucasian women did not differ in striatal BPND for any region (p ≥ 0.19 for all analyses). Furthermore, BMI did not correlate with BPND for any region in normal-weight (p ≥ 0.29, controlling for age) or obese (p ≥ 0.11, controlling for age) Caucasian women. Therefore, gender and ethnicity were not controlled for in the rest of the analyses.
Participant characteristics
Obese and normal-weight participants did not differ in age (U28 = 78, p = 0.16), education level (t28 = −1.58, p = 0.13), BDI (U28 = 78, p = 0.16), WASI IQ (t28 = −1.82, p = 0.08), or ASRS Part A (U28 = 93.5, p = 0.44) scores.
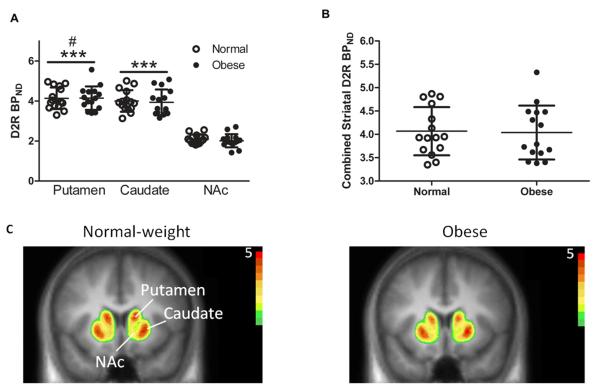
[11C]NMB BPND
Normal-weight and obese groups did not differ in overall D2R BPND estimates (main effect of group, F1,27 = 0.12, p = 0.73; Fig. 1A, C, Table 2). As expected (Eisenstein et al., 2012), there was a main effect of region (F2,54 = 30.88, p < 0.0001), in which putamen BPND estimates were higher than those of caudate (p < 0.05) and nucleus accumbens (p < 0.0001). Caudate BPND estimates were also higher than those of nucleus accumbens (p < 0.0001, Fig. 1A). There was no interaction between group and region (group × region interaction, F2, 54 = 0.86, p = 0.43, Fig. 1A, C). Combined striatal mean BPND estimates of D2R availability did not differ between normal-weight and obese groups (F1,27 = 0.23, p = 0.63; Fig. 1B, C, Table 2). The putamen and mean striatal BPNDs for one obese participant were 2.42 and 2.24 standard deviations above the mean, respectively. Therefore the analyses described above were performed excluding this subject and, similarly, did not reveal differences in striatal BPND between normal-weight and obese groups (main effect of group, F1,26 = 0.05, p = 0.82 for repeated measures GLM; F1,26 = 0, p = 0.98 for univariate GLM).
Figure 1. Striatal D2R specific binding does not differ between obese and normal-weight individuals.
A) D2R specific binding (BPND) estimates (error bars = S.D.) are significantly higher in putamen than in caudate and nucleus accumbens. D2R BPND estimates are significantly higher in caudate than in nucleus accumbens. D2R BPND estimates do not differ between normal-weight and obese subjects in any ROI. B) Combined striatal mean D2R BPND (error bars = S.D) do not differ between normal-weight and obese participants. C) Average [11C]NMB radioactivity levels, represented by distribution volume ratios (DVRs, DVR = BPND +1), in normal-weight (left) and obese (right) groups in striatal ROIs overlaid on MRI in coronal view. Red = peak [11C]NMB radioactivity; Green = lowest [11C]NMB radioactivity. NAc, nucleus accumbens. #, p < 0.05 relative to caudate; ***, p < 0.0001 relative to nucleus accumbens.
Table 2.
Striatal BPND Estimates
| Normal-weight | Obese | 95% CI | |
|---|---|---|---|
| Putamen Mean (S.D.) | 4.13 (0.54) | 4.14 (0.59) | −0.21 to 0.53 |
| Caudate Mean (S.D.) | 4.00 (0.54) | 3.93 (0.64) | −0.43 to 0.47 |
| Nucleus Accumbens Mean (S.D.) | 2.09 (0.23) | 2.01 (0.33) | −0.23 to 0.18 |
| Combined Striatum Mean (S.D.) | 4.07 (0.52) | 4.04 (0.58) | −0.3 to 0.48 |
CI, confidence interval.
Voxel-based analysis
There were no differences between groups in D2R BPND after multiple comparisons correction whether or not the potential outlier was included in the analysis (p > 0.05 for all clusters).
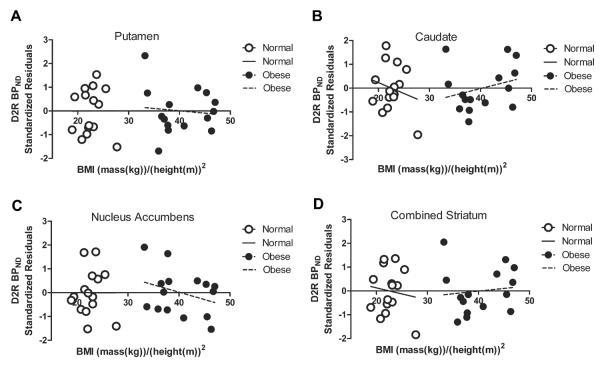
[11C]NMB BPND across BMI
BMI did not correlate with D2R BPND estimates for any individual striatal ROI or combined striatum within the normal-weight group (p ≥ 0.46) or the obese group (p ≥ 0.27; Fig. 2, A–D, Table 3). Excluding the potential outlier, caudate BPND was positively correlated with BMI in the obese group (r11 = 0.58, p < 0.05, 95% confidence interval, 0.08 to 0.85) but there were no significant relationships between BMI and other striatal regions (p ≥ 0.1).
Figure 2. Striatal D2R specific binding is not associated with BMI in obese or normal-weight individuals.
D2R specific binding (BPND) is not significantly correlated with BMI in A) putamen, B) caudate, C) nucleus accumbens or D) combined striatum in normal-weight or obese groups. Correlational analyses are controlled for age. Partial regression plots are shown with standardized values for striatal BPNDs.
Table 3.
Partial Pearson's Correlations (r) Between BMI and Striatal BPND, Controlling for Age
| Normal-Weight BMI | 95% CI | Obese BMI | 95% CI | |
|---|---|---|---|---|
| Putamen | 0.004 | −0.57 to 0.57 | −0.10 | −0.57 to 0.42 |
| Caudate | −0.22 | −0.7 to 0.41 | −0.28 | −0.25 to 0.68 |
| Nucleus Accumbens | −0.002 | −0.57 to 0.57 | −0.32 | −0.71 to 0.21 |
| Combined Striatum | −0.12 | −0.65 to 0.49 | 0.12 | −0.4 to 0.58 |
CI, confidence interval.
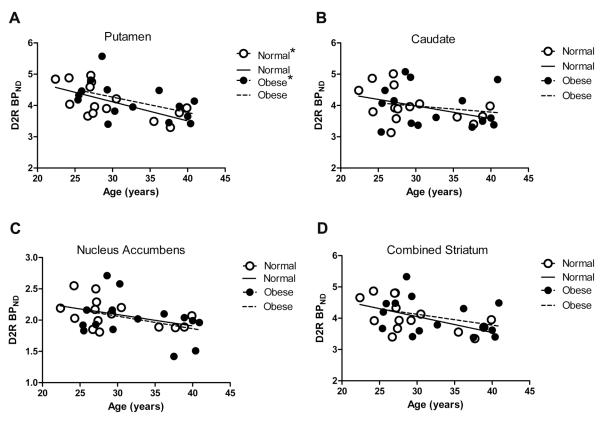
[11C]NMB BPND across age
In normal-weight and obese subjects, age was negatively correlated with D2R BPND estimates for putamen (p < 0.05 for each correlation) but not caudate, nucleus accumbens or combined striatum (p ≥ 0.09, Fig. 3A–D, Table 4). Excluding the obese subject described as a potential outlier in the previous section, age was not significantly correlated with striatal BPND in the obese group (p ≥ 0.07).
Figure 3. Striatal D2R specific binding is associated with age in normal-weight and obese individuals.
Age is negatively associated with D2R specific binding (BPND) in normal-weight and obese participants in A) putamen but not in B) caudate, C) nucleus accumbens or D) combined striatum. *, p < 0.05 for Spearman's rho between BPND and age.
Table 4.
Spearman's Correlations (rho) Between Age and Striatal BPND
| Normal-Weight Age | 95% CI | Obese Age | 95% CI | |
|---|---|---|---|---|
| Putamen | −0.59* | −0.85 to −0.11 | −0.54* | −0.79 to −0.13 |
| Caudate | −0.35 | −0.73 to 0.46 | −0.13 | −0.54 to 0.33 |
| Nucleus Accumbens | −0.4 | −0.76 to 0.14 | −0.14 | −0.55 to 0.32 |
| Combined Striatum | −0.45† | −0.78 to −0.08 | −0.31 | −0.66 to 0.15 |
CI, confidence interval.
p < 0.05;
p = 0.09
DISCUSSION
We found no difference in striatal D2R specific binding, as estimated by [11C]NMB BPND, between normal-weight and obese people. We used the unique PET radioligand [11C]NMB, so these measurements were not confounded by D3R binding or by endogenous dopamine release (Karimi et al., 2011; Moerlein et al., 1997). Furthermore, our results were not confounded by excluded related conditions that can affect dopamine receptor specific binding, such as diabetes, neurologic illness, or psychiatric and substance abuse disorders (Blum et al., 2012, DeFronzo, 2011).
It is unlikely that we failed to find a difference in D2R specific binding between normal-weight and obese groups due to inadequate sample size. Based on results from previous studies (de Weijer et al., 2011; Dunn et al., 2012; Wang et al., 2001), the number of subjects enrolled in our study provided power sufficient to detect medium to large effect sizes both for the between-group comparisons and for the correlations of D2R specific binding with BMI. It should be noted that our group sizes are larger than or equal to those of several previous D2/D3 PET obesity studies (de Weijer et al., 2011: n = 15/group; Dunn et al., 2012: n = 8–14/group; Wang et al., 2001: n = 10/group). Our findings suggest that when relevant comorbidities are excluded, D2 receptor specific binding is not responsible for the previously observed differences in D2/D3 availability in obesity (de Weijer et al., 2011; Dunn et al., 2012; Haltia et al., 2007; Wang et al., 2001). Other aspects of dopamine signaling should be explored, such as D3R receptors, endogenous dopamine release, reuptake via the dopamine transporter or second messenger systems.
The selectivity of [11C]NMB for the D2R of the D2 receptor family over D3R (Karimi et al., 2011) might explain the differences between our results and previous studies. The PET radioligands used in previous obesity studies such as [11C]raclopride (Haltia et al., 2007; Wang et al., 2001) and [18F]fallypride (Dunn et al., 2012) and the SPECT radioligand [123I] IBZM (de Weijer et al., 2011) do not distinguish well between D2 and D3 subtypes (Elsinga et al., 2006; Mukherjee et al., 1999; Videbaek et al., 2000). If D3R specific binding is altered in obesity, it could explain the difference between our finding and other studies with non-specific D2/D3 radioligands. D2R occur at high levels in the dorsal striatum, nucleus accumbens, extrastriatal subcortical and cortical regions while D3R are present at high levels in ventral (as opposed to lateral) caudate and putamen, the shell of the nucleus accumbens and other limbic regions (Beaulieu and Gainetdinov, 2011) and thus may play a larger role in reward function. While D3R is clearly a factor in drug seeking and addiction in rodents and nonhuman primates (Newman et al., 2012) with some suggestive evidence in humans (Boileau et al., 2012), there is mixed and limited evidence for a role of striatal D3R in rodent (Thanos et al., 2008) and human (Dodds et al., 2012; Nathan et al., 2012) obesity. The data from our study and previous reports underscore the potential importance of D3R in obesity and the need for future studies using a D3R-selective PET radioligand.
The displaceability of PET radioligands by endogenous dopamine might also contribute to the differences between our results and those of previous studies. [11C]NMB is not displaceable by endogenous dopamine (Moerlein et al., 1997), but [11C]raclopride, [18F]fallypride and [123I]IBZM are (Dewey et al., 1993; Laruelle et al., 1995; Riccardi et al., 2006). Thus, if obesity is associated with increased striatal extracellular dopamine content, due to increased dopamine release or reduced uptake, then [11C] raclopride, [18F] fallypride, and [123I]IBZM studies might find reduced D2/D3 receptor availability in striatum, due to displacement, while [11C]NMB would not. Alterations in extracellular dopamine levels in obesity have been studied indirectly in humans. Data from fMRI studies conducted in human subjects indicate greater striatal activation in response to food-related cues (i.e., visual images of high calorie food) in obese than in non-obese individuals (Stoeckel et al., 2008), but blunted striatal activation in response to consumption of a highly palatable food that was negatively correlated with BMI in obese individuals (Stice et al., 2010). Therefore, data from human studies indicate that the striatal system is overactivated in overweight and obese people in response to food stimuli but underactive during palatable food consumption. A major advantage of using [11C]NMB in PET to measure D2R is that it is not sensitive to transient changes in synaptic dopamine concentration. However, these changes may be relevant to obesity. Given that striatal activation is highly dynamic and dependent on the behavior of an individual over time (e.g. response to food stimuli versus food receipt), future studies need to address these possibilities by measuring endogenous dopamine release under different satiety conditions using .ligands that are displaceable by endogenous dopamine (e.g. [11C]raclopride)]..
A possible limitation of this study is that both men and women of several ethnicities were included as subjects. It is possible that variability due to these factors may have influenced the findings reported here. The study was not designed or powered to determine if there are statistically significant differences in D2R specific binding levels between men and women or between different ethnicities. However, D2R specific binding levels did not differ between Caucasian and African Americans in the obese group or between normal-weight and obese Caucasian women. Gender differences at baseline were not reported in previous PET studies of D2/D3 receptor availability in obesity (Haltia et al., 2007; Wang et al., 2001) or in a larger [11C]NMB PET study of healthy men and women (Eisenstein et al., 2012). Therefore, it is unlikely that ethnicity and gender differences contributed to our findings. .Furthermore, it is unlikely that differences between our study and others in subject characteristics (e.g. BMI, sex, or age) explain differences in results. Our study targeted obese individuals with a BMI range of 30 – 50 kg/m2, to ensure that individuals fit the criteria for obesity, but would also avoid major health and age comorbidities and still fit within the confines of the scanners (average obese BMI = 40.3 kg/m2; range = 33.2 – 47 kg/m2). The other studies targeted individuals with similar (Dunn et al., 2012: average obese BMI = 40 kg/m2, range not available) or lower BMI (Haltia et al., 2007: average overweight/obese BMI = 33 kg/m2, range not available), but one study had a higher and only partly overlapping range of BMI (de Weijer et al., 2011: average obese BMI = 46.8 kg/m2, range = 38.7 – 61.3 kg/m2; Wang et al., 2001: average obese BMI = 51 kg/m2, range = 42–60 kg/m2). Differences in D2R specific binding may be detectable only in more severely obese individuals. However, the results of Haltia et al. (2007) and Dunn et al. (2012) would argue against this notion. Interestingly, as in Dunn et al. (2012) but opposite of findings in Wang et al. (2001), caudate D2R specific binding was positively correlated with BMI in the obese group when controlling for age and excluding a potential outlier. It is possible that reduced endogenous dopamine levels and increased BMI in obese subjects contributes to increased D2R in caudate as observed in Dunn et al. (2012).
Finally, our normal-weight and obese participants were younger (normal-weight age range: 22.4 – 39.9 years; obese: 25.4 – 40.9 years) than in Wang et al., (2001) (range: 25–54 years), de Weijer et al. (2011) (range = 20 – 60 years) and Dunn et al. (2012) (mean age = 40 years, range not available). Age is negatively associated with striatal D2/D3 receptor availability as measured by [11C] raclopride, [18F]fallypride and [123I]IBZM (Antonini and Leenders, 1993; Brucke et al., 1993; Wang et al., 2001), and with D2R specific binding as measured by [11C]NMB (Eisenstein et al., 2012), which was found in the current study in both groups for the putamen. In contrast, we did not find a significant relationship between D2R specific binding and age for other striatal regions. This is likely due to the somewhat narrow age range studied, which was chosen intentionally to exclude age as a confounding factor in BPND estimates.
Our findings shed light on the role of striatal dopaminergic signaling in obesity by demonstrating that baseline specific binding of the striatal D2 receptor subtype of the D2 receptor family does not differ between normal-weight and obese adults. Since individuals with diabetes were excluded from this study, it remains unknown whether D2R may play a role in the association between diabetes and obesity. Additional studies are needed to answer this question and to better understand the contribution of striatal dopaminergic transmission and D3R specific binding to dopaminergic signaling in normal-weight and obese individuals.
ACKNOWLEDGEMENTS
This study was supported by the National Institute of Health – NIDDK Grant R01 DK085575-03 (S.A.E., E.C.B., S.A.R., T.H.), T32 DA007261 (S.A.E., J.V.A.-D., D.M.G.), DK 37948, DK 56341 (Nutrition Obesity Research Center), NS41509, NS075321, NS058714 and UL1 TR000448 (Clinical and Translational Science Award).
The authors thank Heather M. Lugar, M.A., Jerrel R. Rutlin, B.A. and Johanna M. Hartlein, M.S.N. for their contributions to the study.
Footnotes
The authors report no conflicts of interest.
REFERENCES
- American Diabetic Association Standards of Medical Care in Diabetes – 2010. Diabetes Care. 2010;33:S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antenor-Dorsey JA, Markham J, Moerlein SM, Videen TO, Perlmutter JS. Validation of the reference tissue model for estimation of dopaminergic D2-like receptor binding with [18F](N-methyl)benperidol in humans. Nucl Med Biol. 2008;35:335–341. doi: 10.1016/j.nucmedbio.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonini A, Leenders KL. Dopamine D2 receptors in normal human brain: Effect of age measured by positron emission tomography (PET) and [11C]-raclopride. Ann NY Acad Sci. 1993;695:81–85. doi: 10.1111/j.1749-6632.1993.tb23033.x. [DOI] [PubMed] [Google Scholar]
- Arnett CD, Shiue CY, Wolf AP, Fowler JS, Logan J, Watanabe M. Comparison of three 18F-labeled butyrophenone neuroleptic drugs in the baboon using positron emission tomography. J Neurochem. 1985;44:835–844. doi: 10.1111/j.1471-4159.1985.tb12891.x. [DOI] [PubMed] [Google Scholar]
- Beaulieu JM, Gainetdinov RR. The physiology, signaling, and pharmacology of dopamine receptors. Pharmacol Rev. 2011;63:182–217. doi: 10.1124/pr.110.002642. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown G. Manual for the Beck Depression Inventory-II. Psychological Corporation; San Antonio, TX: 1993. [Google Scholar]
- Blum K, Chen AL, Giordano J, Borsten J, Chen TJ, Hauser M, Simpatico T, Femino J, Braverman ER, Barth D. The addictive brain: All roads lead to dopamine. J Psychoactive Drugs. 2012;44:134–143. doi: 10.1080/02791072.2012.685407. [DOI] [PubMed] [Google Scholar]
- Boileau I, Payer D, Houle S, Behzadi A, Rusjan PM, Tong J, Wilkins D, Selby P, George TP, Zack M, Furukawa Y, McCluskey T, Wilson AA, Kish SJ. Higher binding of the dopamine D3 receptor-preferring ligand [11C]-(+)-propyl-hexahydro-naphtho-oxazin in methamphetamine polydrug users: A positron emission tomography study. J Neurosci. 2012;32:1353–1359. doi: 10.1523/JNEUROSCI.4371-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brix G, Zaers J, Adam LE, Bellemann ME, Ostertag H, Trojan H, Haberkorn U, Doll J, Oberdorfer F, Lorenz WJ. Performance evaluation of a whole-body PET scanner using the NEMA protocol. National Electrical Manufacturers Association. J Nucl Med. 1997;38:1614–1623. [PubMed] [Google Scholar]
- Brucke T, Wenger S, Asenbaum S, Fertl E, Pfafflmeyer N, Muller C, Podreka I, Angelberger P. Dopamine D2 receptor imaging and measurement with SPECT. Adv Neurol. 1993;60:494–500. [PubMed] [Google Scholar]
- DeFronzo RA. Bromocriptine: A sympatholytic, D2-dopamine agonist for the treatment of Type 2 diabetes. Diabetes Care. 2011;34:789–794. doi: 10.2337/dc11-0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong JW, Vanderschuren LJ, Adan RA. Towards an animal model of food addiction. Obes Facts. 2012;5:180–195. doi: 10.1159/000338292. [DOI] [PubMed] [Google Scholar]
- de Weijer BA, van de Giessen, van Amelsvoort TA, Boot E, Braak B, Janssen IM, van de Laar A, Fliers E, Serlie MJ, Booij J. Lower striatal dopamine D2/D3 receptor availability in obese compared with non-obese subjects. EJNMMI Res. 2011;1:37. doi: 10.1186/2191-219X-1-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewey SL, Smith GS, Logan J, Brodie JD, Fowler JS, Wolf AP. Striatal binding of the PET ligand 11C-raclopride is altered by drugs that modify synaptic dopamine levels. Synapse. 1993;13:350–356. doi: 10.1002/syn.890130407. [DOI] [PubMed] [Google Scholar]
- Dodds CM, O'Neill B, Beaver J, Makwana A, Bani M, Merlo-Pich E, Fletcher PC, Koch A, Bullmore ET, Nathan PJ. Effect of the dopamine D3 receptor antagonist GSK598809 on brain responses to rewarding food images in overweight and obese binge eaters. Appetite. 2012;59:27–33. doi: 10.1016/j.appet.2012.03.007. [DOI] [PubMed] [Google Scholar]
- Dunn JP, Kessler RM, Feurer IK, Volkow ND, Patterson BW, Ansari MS, Li R, Marks-Shulman P, Abumrad NN. Relationship of dopamine type 2 receptor binding potential with fasting neuroendocrine hormones and insulin sensitivity in human obesity. Diabetes Care. 2012;35:1105–1111. doi: 10.2337/dc11-2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenstein SA, Koller JM, Piccirillo M, Kim A, Antenor-Dorsey JA, Videen TO, Snyder AZ, Karimi M, Moerlein SM, Black KJ, Perlmutter JS, Hershey T. Characterization of extrastriatal D2 in vivo specific binding of [18F](N-methyl)benperidol using PET. Synapse. 2012;66:770–780. doi: 10.1002/syn.21566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsinga PH, Hatano K, Ishiwata K. PET tracers for imaging of the dopaminergic system. Curr Med Chem. 2006;13:2139–2153. doi: 10.2174/092986706777935258. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Haltia LT, Rinne JO, Merisaari H, Maguire RP, Savontaus E, Helin S, Nagren K, Kaasinen V. Effects of intravenous glucose on dopaminergic function in the human brain in vivo. Synapse. 2007;61:748–756. doi: 10.1002/syn.20418. [DOI] [PubMed] [Google Scholar]
- Harri M, Mika T, Jussi H, Nevalainen OS, Jarmo H. Evaluation of partial volume effect correction methods for brain positron emission tomography: Quantification and reproducibility. J Med Phys. 2007;32:108–117. doi: 10.4103/0971-6203.35723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hershey T, Black KJ, Carl JL, McGee-Minnich L, Snyder AZ, Perlmutter JS. Long term treatment and disease severity change brain responses to levodopa in Parkinson's disease. J Neurol Neurosurg Psychiatry. 2003;4:844–851. doi: 10.1136/jnnp.74.7.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hietala J, West C, Syvalahti E, Nagren K, Lehikoinen P, Sonninen P, Ruotsalainen U. Striatal D2 dopamine receptor binding characteristics in vivo in patients with alcohol dependence. Psychopharmacology (Berl) 1994;116:285–290. doi: 10.1007/BF02245330. [DOI] [PubMed] [Google Scholar]
- Karimi M, Moerlein SM, Videen TO, Luedtke RR, Taylor M, Mach RH, Perlmutter JS. Decreased striatal dopamine receptor binding in primary focal dystonia: a D2 or D3 defect? Mov Disord. 2011;26:100–106. doi: 10.1002/mds.23401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, Howes MJ, Jin R, Secnik K, Spencer T, Ustun TB, Walters EE. The World Health Organization Adult ADHD Self-Report Scale (ASRS) Psychol Med. 2005;35:245–256. doi: 10.1017/s0033291704002892. [DOI] [PubMed] [Google Scholar]
- Laruelle M, Abi-Dargham A, van Dyck CH, Rosenblatt W, Zea-Ponce Y, Zoghbi SS, Baldwin RM, Charney DS, Hoffer PB, Kung HF, Innis RB. SPECT imaging of striatal dopamine release after amphetamine challenge. J Nucl Med. 1995;36:1182–1190. [PubMed] [Google Scholar]
- Logan J, Fowler JS, Volkow ND, Wang GJ, Ding YS, Alexoff DL. Distribution volume ratios without blood sampling from graphical analysis of PET data. J Cereb Blood Flow Metab. 1996;16:834–840. doi: 10.1097/00004647-199609000-00008. [DOI] [PubMed] [Google Scholar]
- Moerlein SM, Banks WR, Parkinson D. Production of fluorine-18 labeled (N-methyl)benperidol for PET investigation of cerebral dopaminergic receptor binding. Appl Radiat Isot. 1992;43:913–917. doi: 10.1016/0883-2889(92)90155-8. [DOI] [PubMed] [Google Scholar]
- Moerlein SM, LaVenture JP, Gaehle GG, Robben J, Perlmutter JS, Mach RH. Automated production of N-([11C]methyl)benperidol for clinical application. Eur J Nucl Med Mol Imaging. 2010;37:S366. [Google Scholar]
- Moerlein SM, Perlmutter JS, Markham J, Welch MJ. In vivo kinetics for [18F](N-methyl)benperidol: A novel PET tracer for assessment of dopaminergic D2-like receptor binding. J Cereb Blood Flow Metab. 1997;17:833–845. doi: 10.1097/00004647-199708000-00002. [DOI] [PubMed] [Google Scholar]
- Moerlein SM, Perlmutter JS, Welch MJ. Specific, reversible binding of [18F]benperidol to baboon D2 receptors: PET evaluation of an improved 18F-labeled ligand. Nucl Med Biol. 1995;22:809–815. doi: 10.1016/0969-8051(95)00022-p. [DOI] [PubMed] [Google Scholar]
- Moerlein SM, Perlmutter JS, Welch MJ. Radiosynthesis of (N-[11C]methyl)benperidol for PET investigation of D2 receptor binding. Radiochem Acta. 2004;92:333–339. [Google Scholar]
- Mukherjee J, Yang ZY, Brown T, Lew R, Wernick M, Ouyang X, Yasillo N, Chen CT, Mintzer R, Cooper M. Preliminary assessment of extrastriatal dopamine D-2 receptor binding in the rodent and nonhuman primate brains using the high affinity radioligand, 18F-fallypride. Nucl Med Biol. 1999;26:519–527. doi: 10.1016/s0969-8051(99)00012-8. [DOI] [PubMed] [Google Scholar]
- Nathan PJ, O'Neill BV, Mogg K, Bradley BP, Beaver J, Bani M, Merlo-Pich E, Fletcher PC, Swirski B, Koch A, Dodds CM, Bullmore ET. The effects of the dopamine D3 receptor antagonist GSK598809 on attentional bias to palatable food cues in overweight and obese subjects. Int J Neuropsychopharmacol. 2012;15:149–161. doi: 10.1017/S1461145711001052. [DOI] [PubMed] [Google Scholar]
- Newman AH, Blaylock BL, Nader MA, Bergman J, Sibley DR, Skolnick P. Medication discovery for addiction: Translating the dopamine D3 receptor hypothesis. Biochem Pharmacol. 2012;84:882–890. doi: 10.1016/j.bcp.2012.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quarentelli M, Berkouk K, Prinster A, Landeau B, Svarer C, Balkay L, Alfano B, Brunetti A, Baron JC, Salvatore M. Integrated software for the analysis of brain PET/SPECT studies with partial-volume-effect correction. J Nucl Med. 2004;45:192–201. [PubMed] [Google Scholar]
- Riccardi P, Li R, Ansari MS, Zald D, Park S, Dawant B, Anderson S, Doop M, Woodward N, Schoenberg E, Schmidt D, Baldwin R, Kessler R. Amphetamine-induced displacement of [18F] fallypride in striatum and extrastriatal regions in humans. Neuropsychopharmacology. 2006;31:1016–1026. doi: 10.1038/sj.npp.1300916. [DOI] [PubMed] [Google Scholar]
- Sandell J, Langer O, Larsen P, Dolle F, Vaufrey F, Demphel S, Crouzel C, Halldin C. Improved specific activity of the PET radioligand [11C]FLB 457 by use of the GE medical systems PETtrace MeI microlab. J Lab Comp Radiopharm. 2000;43:331–338. [Google Scholar]
- Shamseddeen H, Getty JZ, Hamdallah IN, Ali MR. Epidemiology and economic impact of obesity and type 2 diabetes. Surg Clin North Am. 2011;91:1163–1172. doi: 10.1016/j.suc.2011.08.001. [DOI] [PubMed] [Google Scholar]
- Steiner JL, Tebes JK, Sledge W, Walker ML. A comparison of the structured clinical interview for DSM-III-R and clinical diagnoses. J Nerv Ment Dis. 1995;183:365–369. doi: 10.1097/00005053-199506000-00003. [DOI] [PubMed] [Google Scholar]
- Stice E, Yokum S, Blum K, Bohon C. Weight gain is associated with reduced striatal response to palatable food. J Neurosci. 2010;30:13105–13109. doi: 10.1523/JNEUROSCI.2105-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoeckel LE, Weller RE, Cook EW, 3rd, Twieg DB, Knowlton RC, Cox JE. Widespread reward-system activation in obese women in response to pictures of high-calorie foods. Neuroimage. 2008;41:636–647. doi: 10.1016/j.neuroimage.2008.02.031. [DOI] [PubMed] [Google Scholar]
- Suehiro M, Dannals RF, Scheffel U, Stathis M, Wilson AA, Ravert HT, Villemagne VL, Sanchez-Roa PM, Wagner HN., Jr In vivo labeling of the dopamine D2 receptor with N-11C-methyl-benperidol. J Nucl Med. 1990;31:2015–2021. [PubMed] [Google Scholar]
- Thanos PK, Michaelides M, Ho CW, Wang GJ, Newman AH, Heidbreider CA, Ashby CR, Jr, Gardner EL, Volkow ND. The effects of two highly selective dopamine D3 receptor antagonists (SB-277011A and NGB-2904) on food self-administration in a rodent model of obesity. Pharmacol Biochem Behav. 2008;89:499–507. doi: 10.1016/j.pbb.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Videbaek C, Toska K, Scheideler MA, Paulson OB, Moos Knudsen G. SPECT tracer [(123)I]IBZM has similar affinity to dopamine D2 and D3 receptors. Synapse. 2000;38:338–342. doi: 10.1002/1098-2396(20001201)38:3<338::AID-SYN13>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Chang L, Wang GJ, Fowler JS, Ding YS, Sedler M, Logan J, Franceschi D, Gatley J, Hitzemann R, Gifford A, Wong C, Pappas N. Low level of brain dopamine D2 receptors in methamphetamine abusers: Association with metabolism in the orbitofrontal cortex. Am J Psychiatry. 2001;158:2015–2021. doi: 10.1176/appi.ajp.158.12.2015. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang GJ, Hitzemann R, Logan J, Schlyer DJ, Dewey SL, Wolf AP. Decreased dopamine D2 receptor availability is associated with reduced frontal metabolism in cocaine abusers. Synapse. 1993;14:169–177. doi: 10.1002/syn.890140210. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Telang F, Fowler JS, Thanos PK, Logan J, Alexoff D, Ding YS, Wong C, Ma Y, Pradhan K. Low dopamine striatal D2 receptors are associated with prefrontal metabolism in obese subjects. Neuroimage. 2008;42:1537–1543. doi: 10.1016/j.neuroimage.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang GJ, Volkow ND, Fowler JS, Logan J, Abumrad NN, Hitzemann RJ, Pappas NS, Pascani K. Dopamine D2 receptor availability in opiate-dependent subjects before and after naloxone-precipitated withdrawal. Neuropsychopharmacology. 1997;16:174–182. doi: 10.1016/S0893-133X(96)00184-4. [DOI] [PubMed] [Google Scholar]
- Wang GJ, Volkow ND, Logan J, Pappas NR, Wong CT, Zhu W, Netusil N, Fowler JS. Brain dopamine and obesity. Lancet. 2001;357:354–357. doi: 10.1016/s0140-6736(00)03643-6. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence (WASI) Harcourt Assessment; San Antonio, TX: 1999. [Google Scholar]