Abstract
Study Objectives:
(1) To describe the incidence rate of motor vehicle crashes (MVCs) in patients with obstructive sleep apnea (OSA); and (2) to investigate MVC risk factors in OSA patients.
Methods:
A retrospective case-series observational study was conducted using data from the West Australian Sleep Health Study at a tertiary hospital-based sleep clinic. Participants were patients (N = 2,673) referred for assessment of suspected sleep disordered breathing. Questionnaire data were collected including age, sex, years of driving, near-misses and MVCs, sleepiness, and consumption of alcohol and caffeinated drinks. Overnight laboratory-based polysomnography was performed using standard methodology.1 Poisson univariate and negative binomial multivariable regression models were used to investigate associations between risk factors and MVC and near-miss risk in patients with untreated OSA.
Results:
In patients with untreated OSA, the crash rate was 0.06 MVC/person-year compared with the general community crash rate of 0.02 MVC/person-year. The rate ratio comparing very sleepy men with normal men was 4.68 (95% CI 3.07, 7.14) for near-misses and 1.27 (95% CI 1.00, 1.61) for crashes, after adjusting for confounders. In women there was a significant association with sleepiness score (p = 0.02) but no dose effect across quartiles.
Conclusions:
Untreated OSA is associated with an increased risk of near-misses in men and women and an increased risk of MVCs in very sleepy men. There is a strong association between excessive daytime sleepiness and increased report of near-misses. Our data support the observation that it is those patients with increased sleepiness regardless of OSA severity who are most at risk.
Citation:
Ward KL; Hillman DR; James A; Bremner AP; Simpson L; Cooper MN; Palmer LJ; Fedson AC; Mukherjee S. Excessive daytime sleepiness increases the risk of motor vehicle crash in obstructive sleep apnea. J Clin Sleep Med 2013;9(10):1013-1021.
Keywords: Motor vehicle crashes, near-misses, sleepiness, obstructive sleep apnea, severity, gender
Obstructive sleep apnea (OSA) is often associated with excessive daytime sleepiness and is a significant independent risk factor for motor vehicle crashes (MVCs).2 Patients with OSA are up to seven times more likely to have a MVC than those without sleep apnea,3 and driver sleepiness has been identified as one of the major causes of highway accidents and fatal crashes.4 It has been shown that personal injury from crashes is much more common in OSA patients,5 and accidents involving OSA patients are more likely to be associated with major injury.5 This is probably due to the fall-asleep nature of these crashes.5,6
BRIEF SUMMARY
Current Knowledge/Study Rationale: The purpose of this study was to determine whether the risk of MVCs was higher in patients with OSA than in the general community and, if so, the nature of the risk. To do so, we examined the relationships of near-misses and MVCs with OSA severity, degree of daytime sleepiness, and other potential risk factors with a study design powered to address these associations using standardized measurement technologies for OSA.
Study Impact: Our study confirms that sleep clinic patients with untreated OSA have significantly more crashes than the general population. There is a strong association between excessive daytime sleepiness and increased report of near-misses supporting the observation that it is those patients with increased sleepiness regardless of OSA severity that are most at risk.
Sleep physicians are regularly confronted with the management dilemma of diagnosing the pathology of and treating sleepiness in occupational drivers. The prevalence of OSA among commercial drivers has been carefully investigated because crashes involving trucks and buses are particularly expensive, calamitous, and associated with higher fatality rates. In a large study of Australian commercial vehicle drivers, Howard et al. showed that 60% of drivers had sleep disordered breathing and 24% were excessively sleepy.7 In 2012, Sharwood reported that 41% of long-distance heavy vehicle drivers were likely to have sleep apnea.8 A recent study conducted in the UK demonstrated high rates of sleepiness and sleep-related accidents among bus drivers, and the authors concluded that screening for OSA among this group should be seriously considered.9 However, there remains a need to establish thresholds of disease severity for OSA that guide driving restriction in a similar way as for levels of alcohol consumption.10
It is unclear which risk factors associated with OSA contribute to motor vehicle crashes. The role of disease severity and daytime sleepiness has been assessed by systematic review. Risk of MVCs in non-commercial drivers with OSA was associated with increased sleepiness in half of the studies reviewed.11 A meta-analysis conducted in 2009 of studies examining commercial drivers with OSA concluded that the disease-related factors of body mass index (BMI), apnea hypopnea index (AHI), hypoxemia, and daytime sleepiness may predict crash risk.2 However, these conclusions were drawn from studies that had small sample sizes (most < 200 subjects), limited adjustment for confounders, and used various measurement technologies and scoring rules to diagnose OSA thresholds. Thus the relative importance of these risk factors remains unclear.
Further problems with the study of accident events are their low occurrence rates and their contentious nature, which creates barriers to data collection. Studying near-miss incidents has advantages in these respects. It is well recognized in safety research that near-misses have a similar profile to accidents and that study of near-misses can identify factors that either exacerbate or mitigate risk.12 There has been little attention given to sleepy near-miss driving crashes in the sleep research literature despite their likely relationship with actual driving crashes.13 However, there have been two large studies of sleepy driver near-misses that suggest such incidents may be precursors to an actual accident.13,14
The purpose of this study was to determine whether the risk of MVCs was higher in patients with OSA than in the general community and, if so, the nature of the risk. To do so, we examined the relationships of near-misses and MVCs with OSA severity, degree of daytime sleepiness, and other potential risk factors in a sleep clinic population with a study design powered to address these associations using standardized measurement technologies for OSA.
METHODS
Study Sample
Patients referred to the West Australian Sleep Disorders Research Institute (WASDRI) for investigation of sleep disorders from January 2006 to April 2009 who had questionnaire and sleep study data available were included in the study (98% consent rate). These patients were part of the West Australian Sleep Health Study (WASHS) cohort.15 This study was approved by the Human Research Ethics Committee at Sir Charles Gairdner Hospital (No. 2004-083).
Techniques
Questionnaires
Prior to clinical and polysomnography (PSG) evaluation, a self-administered questionnaire was used to collect potential risk factor information including age, sex, number of years driving, MVCs, sleepiness (Epworth Sleepiness Score [ESS]),16 and consumption of alcohol and caffeinated drinks. Weekly alcohol consumption was calculated from the average number of alcoholic drinks patients consumed in a typical week over the past year. The level of consumption was based on their response to the question On days when you drink alcohol, how many drinks of beer, wine and/or other type of alcohol would you have? based on a standard (10 g alcohol) alcoholic drink. Response options were: 0, 1-2, 3-5, 6-9, or 10 or more alcoholic drinks per day.
Caffeine intake was based upon the response to the question During the past month, have you used coffee, tea or other caffeine drinks to stay awake during your normal waking time? Possible responses were: never; rarely (has occurred but less than once a week); sometimes (1-2 times per week); frequently (3-4 times per week); always or almost always (5-7 times per week); or don't know.
To assess driving behavior, patients answered a series of 6 questions about years of driving, falling asleep while behind the wheel, near-miss crashes (How many “near miss” car accidents have you had due to sleepiness?) and actual MVCs (How many car accidents have you ever had while driving a car?). For each patient, the mean crash rate was calculated as MVC/person-year (questionnaire-based self-report). This was compared with data for the general community from the Office of Road Safety annual report (police report).17 The comparison of crash rate was made by calculating the crash rate ratio for subjects with OSA (AHI > 5 events/h) and comparing with the crash rate for the general community.
Polysomnography (PSG)
Overnight laboratory-based PSG was performed using conventional instrumentation (Profusion 2, Compumedics Ltd, Victoria, Australia) and analyzed according to the recommendations published by the American Academy of Sleep Medicine.1 Sleep and its various stages were documented by standard electroencephalographic, electrooculographic, and electromyographic criteria.18
The PSG methodology for this case series has previously been described.1,15 Obstructive apneas were defined as absence of airflow ≥ 10 seconds. Obstructive hypopneas were defined as ≥ 50% decrease in airflow, or a clear but lesser decrease in airflow associated with either 3% desaturation or arousal in the context of ongoing respiratory effort. The complete record was reviewed manually by trained sleep technologists for sleep stage, leg movements, arousals, apneas, and hypopneas. AHI and arousal index (ARI) were defined as the number of events per hour of sleep.
Data Analysis
Data were analyzed using SPSS statistics (GradPack 17.0 Release 17.0.2, March 11, 2009) and R (Version 2.14.1, 2011-12-22). Statistical significance was defined at the 5% level. All data are reported as mean ± SD, or median (interquartile range [IQR]) for non-normal variables. Male and female patient characteristics were compared using independent t-tests or Mann-Whitney U tests. The overall crash rate for all subjects was compared with community crash rate data for Western Australia from the Office of Road Safety 2006 report.17 Near-misses were categorized for all subjects and the proportion of subjects with at least one crash calculated, in addition to the proportion of subjects with near-misses who fell asleep driving. Linear-by-linear association tests were used to assess relationships between these variables.
Patients were stratified by gender and divided into 4 OSA severity categories based upon the AHI: “normal” (AHI < 5 events/h), “mild OSA” (5 ≤ AHI < 15), “moderate OSA” (15 ≤ AHI < 30), and “severe OSA” (AHI ≥ 30).1 Patients were also divided into 4 quartiles of subjective sleepiness according to their ESS: “normal” (0-5), “non-sleepy” (6-9), “sleepy” (10-14), and “very sleepy” (15-24). The latter 3 categories for sleepiness were compared with the reference category (i.e., “normal”). Rate ratios (RRs) and 95% confidence intervals (CIs) were estimated from Poisson univariate regression models, with offset log years driving. Trends across categories were assessed with Cochrane Armitage trend tests. Gender differences within each category of AHI and ESS were compared using rate ratio tests.
Generalized linear models (negative binomial with log link and offset log years driving) were used to test associations between each of the primary risk factors AHI and ESS (as both categorical and continuous variables) with the near-miss rates and crash rates. Models were adjusted for potential confounding variables (neck circumference, proportion of time spent with an arterial oxygen saturation of < 90%, age, sex, and alcohol and caffeine intake). Arousal index, lowest oxygen saturation, OSA presence, smoking, and BMI were tested but were not statistically significant in either univariate or multivariable modelling. As there was significant interaction between each primary risk factor and sex, the dataset was stratified by gender for analysis. Parsimonious models were developed by removing the least significant variable in a stepwise process, resulting in the simplest plausible model. The predictor variable coefficients in the parsimonious model were all significantly different from zero and the model was not a significantly worse fit than the full model.
To assess potential reporting bias, the proportions of missing data for crash questions were calculated. Chi-square tests were conducted across ESS quartiles for each driving question to assess differences in the proportion of missing data relative to sleepiness.
RESULTS
Subject Characteristics
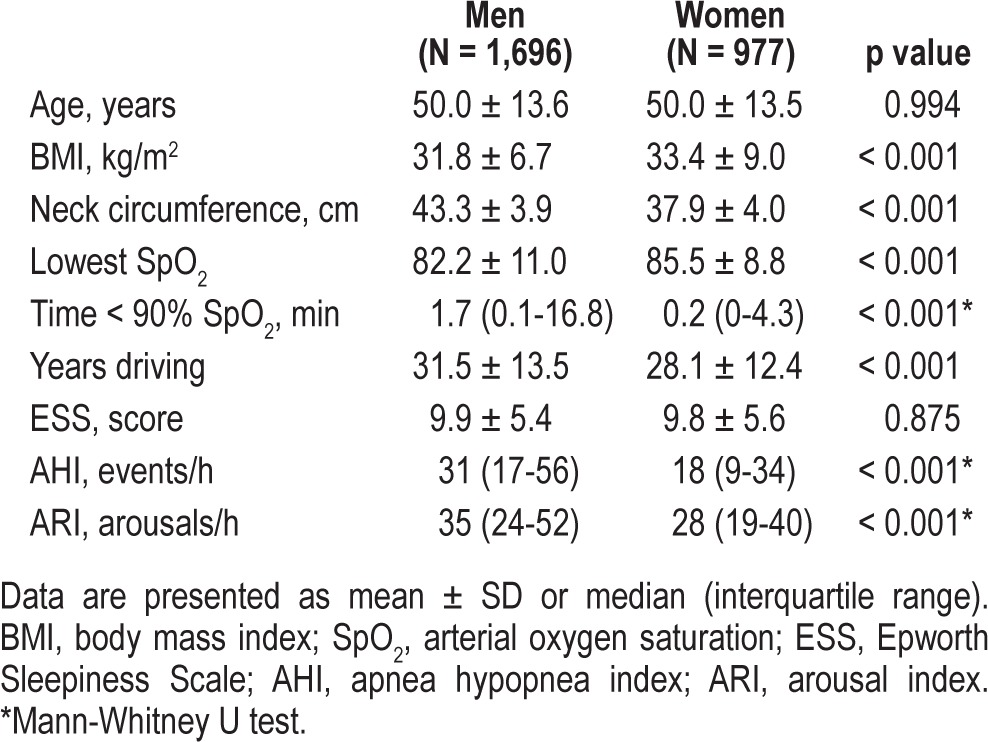
Questionnaire and PSG data were available for 2,673 patients. Patients were predominantly male, middle-aged, and obese (BMI > 30 kg/m2), and mean ± SD duration of driving was 30.2 ± 13.3 years (Table 1). Mean ± SD ESS was 9.9 ± 5.5, and 17% reported moderate to severe excessive sleepiness (ESS ≥ 16). Proportions of missing data for crash questions ranged from 0.4% to 3.4% but did not differ significantly across ESS quartiles. Table 1 presents study population characteristics by gender. Age and ESS did not differ significantly between men and women, but men had significantly higher median scores than women for AHI (31 vs 18 events/h respectively; p < 0.001) and ARI (35 vs 28 events/h respectively; p < 0.001), as well as lower BMI, lower minimum oxygen saturation, and higher proportion of time spent with an oxygen saturation < 90%.
Table 1.
Characteristics of the study population
Motor Vehicle Crashes and Near-Misses
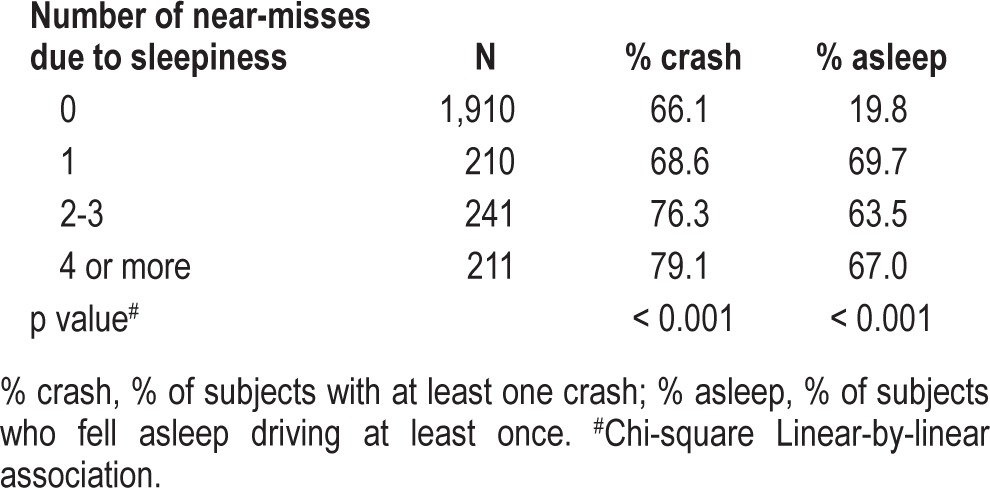
At least one crash was reported by 69% of subjects. Of the reported crashes, 11% of subjects reported having a crash because they felt sleepy or fell asleep behind the wheel. A quarter of subjects (26%) reported at least one near-miss due to sleepiness, and 32% reported having fallen asleep behind the wheel. Table 2 contains data on the association between the number of near-misses and both the percent of subjects with at least one actual crash and those who fell asleep driving at least once. The number of near-misses has a linear relationship (p < 0.001) with the number of actual crashes and with fall-asleep driving episodes (Table 2).
Table 2.
Relationship between near-misses and both actual crashes and episodes of falling asleep driving
The mean overall crash rate of 0.06 MVC/person-year was 3 times higher (p < 0.0001) than the community crash rate of 0.02 MVC/person-year. The mean crash rate ratio for subjects with any OSA (AHI ≥ 5/h, n = 2,486) versus those with no OSA (community) was 3.07 (95% CI 2.98 to 3.17).
Risk Factors for Near-Misses
Trend analysis showed a significant increase (p < 0.001) in the risk of near-misses across OSA categories in men (Table 3, Figure 1). For women, the opposite trend was seen (p < 0.001, Figure 1). The RR comparing severe OSA to no OSA was increased for men (1.50, 95% CI 0.68, 1.97) but decreased (0.65, 95% CI 0.52, 0.82) for women (Table 3). Men reported more near-misses in the moderate and severe categories, while women reported more near-misses in the normal and mild categories (Figure 1).
Table 3.
Rate ratios across OSA categories and ESS quartiles for near-misses and crashes in men and women
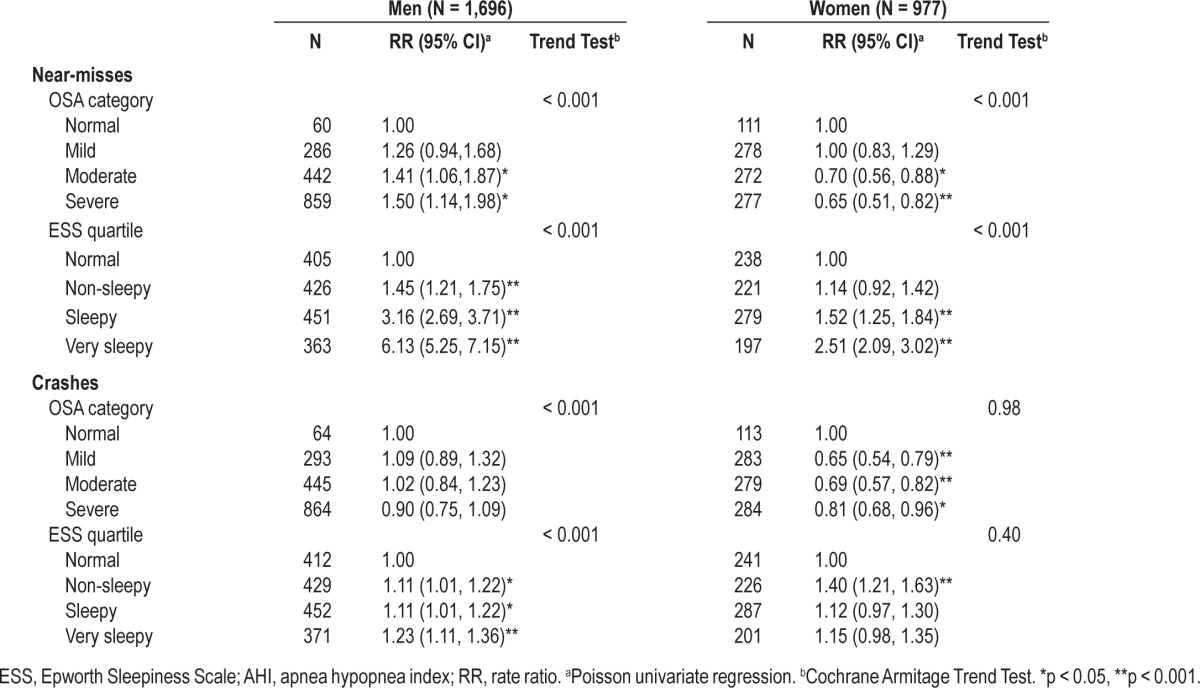
Figure 1. Near-miss rate and severity of OSA for men and women.

Error bars represent 95% CI. Asterisks represent a significant difference between men and women where p < 0.001. See Table 3 for number of subjects in each group.
The near-miss rate increased significantly (p < 0.001) with increased sleepiness score in both men and women. For very sleepy men and women the rates were 6.13 and 2.51 times higher, respectively, than the rates for normal subjects (Table 3). With respect to gender differences within ESS quartiles, men reported more near-misses than women in the moderate (p < 0.001) and severe sleepiness categories (p < 0.001), while women reported more near-misses than men in the normal (p < 0.001) and mild sleepiness (p = 0.06) categories (Figure 2).
Figure 2. Near-miss rate and subjective sleepiness for men and women.

Error bars represent 95% CI. Asterisks represent a significant difference between men and women where p < 0.001. See Table 3 for number of subjects in each group.
Multivariable regression analysis showed that the near-miss rate was associated with sleepiness, age, and caffeine intake, but not with neck circumference, AHI, oxygen saturation, or alcohol intake (Table 4A). After adjustment for significant confounders, very sleepy men were 4.68 times (95% CI 3.07, 7.14) more likely to report a near-miss than normal men (Table 4A, parsimonious model). For women, there was a significant association with sleepiness scores (p = 0.02) but no dose effect across quartiles. When this model was refitted with the very sleepy quartile as the reference category for ESS, the rates in the non-sleepy and sleepy quartiles were significantly lower (sleepy: RR 0.55, 95% CI 0.35, 0.86, p = 0.01; non-sleepy: RR 0.44, 95% CI 0.23, 0.84, p = 0.01).
Table 4.
Negative binomial regressions modelling (A) near-misses, stratified by gender and (B) crashes, stratified by gender
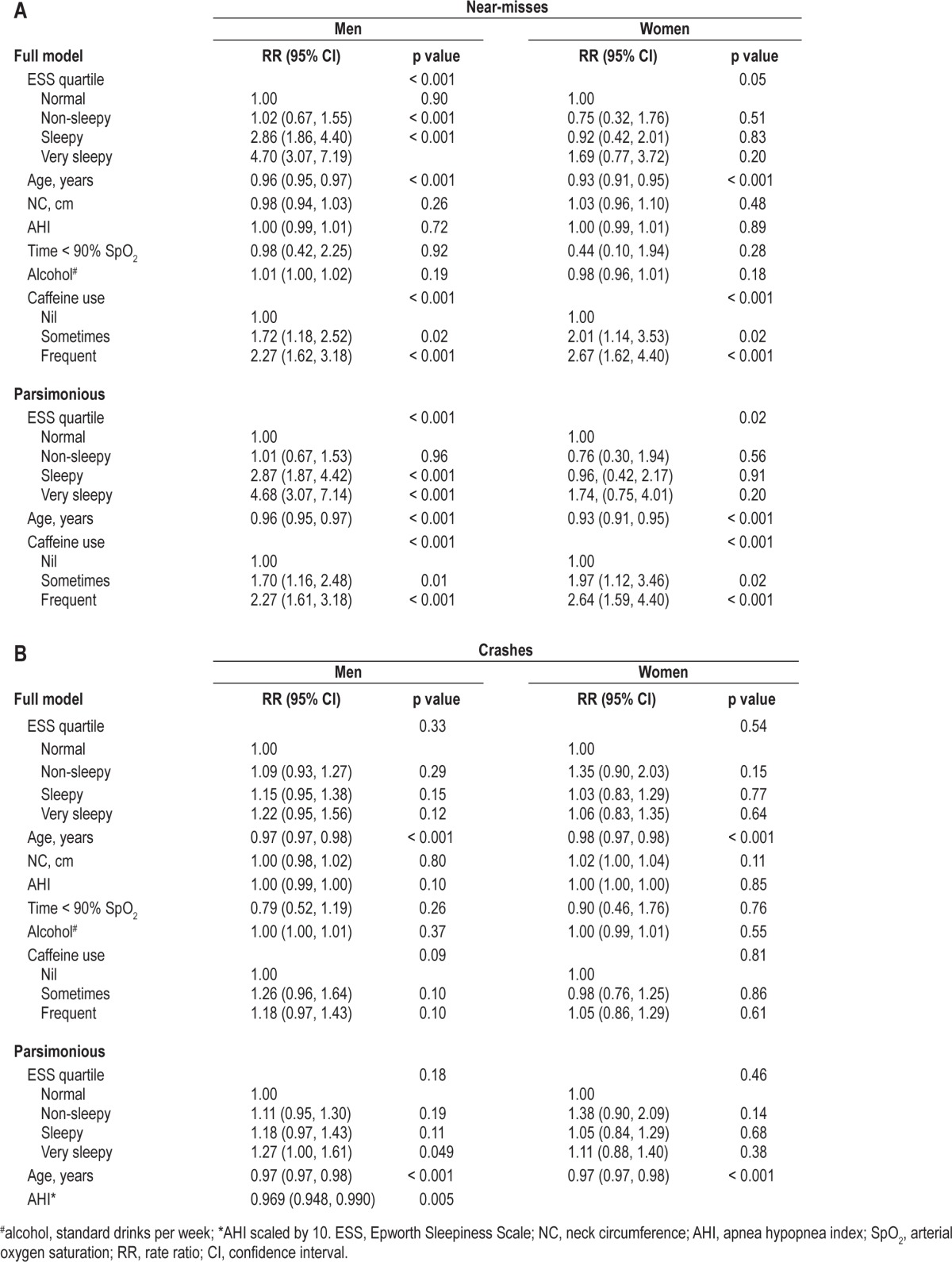
Caffeine use was significantly related (p < 0.001) to near-misses for both men and women, and there was a dose effect (Table 4A). In multivariable regression analysis with AHI considered as the primary categorical risk factor (and ESS as an adjustment continuous variable), AHI showed no significant effect for men (p = 0.71) or women (p = 0.80).
Risk Factors for Crashes
Trend analysis showed a significant decrease (p < 0.001) in the risk of crashes across AHI categories in men (Table 3, Figure 3). For women there was no significant trend across OSA categories (p = 0.98). With respect to gender differences within OSA categories, men with mild and moderate OSA reported significantly more crashes (p < 0.001) than women (Figure 3).
Figure 3. Crash rate and severity of OSA for men and women.

Error bars represent 95% CI. Asterisks represent a significant difference between men and women where p < 0.001. See Table 3 for number of subjects in each group.
There was a significant increase in crash rate with increased sleepiness score for men and women combined (p < 0.001). When men were analyzed separately (Table 3), there was a significant (p < 0.001) upward trend in crash rate with sleepiness. For women there was no significant trend (p = 0.40). With respect to gender differences within quartiles, men reported more crashes than women (p < 0.001) in the normal, sleepy, and very sleepy quartiles (Figure 4).
Figure 4. Crash rate and subjective sleepiness for men and women.

Error bars represent 95% CI. Asterisks represent a significant difference between men and women where p < 0.001. See Table 3 for number of subjects in each group.
Multivariable regression analysis showed that crash rate was related to age only and not sleepiness, AHI, neck circumference, oxygen saturation, or alcohol or caffeine intake in the full model (Table 4B). In the parsimonious model, although very sleepy men reported crashes 1.3 times more often than normal men (p = 0.049), ESS was not a significant predictor of crash rate.
DISCUSSION
This large study investigated risk factors for motor vehicle crashes and near-misses in sleep clinic patients. The study found that subjects with untreated OSA (AHI > 5 events per hour) reported crashes at a rate three times higher than the general community. However, in multivariable regression analysis the rates of reported near-misses in men and women were related more strongly to daytime sleepiness and not the severity of OSA as defined by the AHI metric. In subjects with moderate to severe OSA or sleepiness, women tended to report fewer near-misses and crashes than men.
The mean crash rate ratio (3.07) for our patients with OSA is consistent with a recent meta-analysis, which found that OSA was associated with a 1.21 to 4.89 increase in the mean crash rate ratio. It was reported that the characteristics that predicted crashes in drivers with OSA included AHI, hypoxemia during sleep, BMI, and possibly daytime sleepiness.2
We found a strong association between sleepiness and increased rate of reported near-misses. Very sleepy men (ESS 15-24) reported near-misses 4.68 (95% CI 3.07-7.14) times more often than normal men (ESS 0-5; Table 4A). For women there was a significant association with sleepiness score (p = 0.02, Figure 2), but no dose effect across quartiles. The relationship between sleepiness and increased risk of crash or near-miss has not been consistently demonstrated in past studies.2 Our results agree with one study that was adequately powered (n = 150) and adjusted for confounders, which found a significantly higher risk of near-misses in patients with higher ESS scores.19
More recently, two large community studies provided evidence that sleepy near-misses may be dangerous precursors to an actual accident, and that ESS score had an independent association with having a near-miss or actual accident.13,14 We found a relationship between the number of near-misses and the number of actual crashes (p < 0.001). Disturbingly, there was a relationship of similar magnitude between near-misses and fall asleep driving episodes. Thus our study confirms the findings of Powell and Phillip, who both reported a relationship between sleepiness at the wheel, near-misses, and actual crashes in large community-based samples.13,20
Patients who are referred to sleep clinics show higher levels of daytime sleepiness than the general population.21,22 The mean ESS of 9.9 for our patients was approximately double the mean ESS of 4.6 seen in 72 subjects without sleep disorders.23 Our data show that sleep clinic patients with an ESS > 10 have approximately 1.7 to 4.7 times higher risk of a near-miss. Although these data are self-reported, the large sample size and narrow confidence intervals further strengthen our results.
We found no association between OSA severity and near-misses or crashes in women. Although we found that near-misses were related to severity of OSA in Poisson regression analysis for men (Figure 1, Table 3), this relationship was not significant in multivariable analysis (Table 4A). Crash risk was associated with AHI, but the effect size was small and protective (Table 4B). This may be due to reporting bias in the very sleepy males or increased awareness of symptoms leading to driving avoidance behavior. Since report bias was low (< 5%), driving avoidance behavior is the more probable explanation. Our results for AHI are supported by a recent meta-analysis which showed that no definitive conclusion could be drawn for a relationship between severity of OSA and crash risk.2
It has long been recognized that there is a poor relationship between the AHI-defined severity of OSA and the degree of daytime sleepiness.24–27 It remains unclear why one individual with an AHI of 15 may be sleepy whereas another may be asymptomatic.28 This poor correlation between AHI and ESS is reflected in our WASHS cohort data (r = 0.18). Since disease severity does not correspond well with symptomology, it is not surprising that we found an association between risk of near-miss or crash and daytime sleepiness but not the severity of OSA. In our study, we did not find an association between BMI or hypoxemia and risk of near-miss or crash. Although we found an association between neck circumference and crash risk at the univariate level, after adjusting for other covariates this association did not remain statistically significant.
A marked gender difference in crash risk was found with women reporting fewer near-misses and crashes than men, particularly for subjects with moderate or severe OSA or an ESS > 10. The preponderance of men with increased near-miss and crash risk in this study is supported by data from the annual report on road crashes in Western Australia, where 75% of fatalities over the past 10 years were male.17 Similar gender differences have been reported in the community-based Wisconsin Sleep Cohort Study.29 It has been postulated that men and women may perceive internal cues to sleepiness differently.29
The association between caffeine use and near-misses was strong (p < 0.001), and supports the notion that patients accurately perceive their increased sleepiness and self-medicate with caffeine in an attempt to remain functional during waking hours. Given that the question about caffeine use was not asked in relation to driving, it was thus less subject to bias.
Strengths and Limitations
The strong relationship between excessive sleepiness and near-misses demonstrated in this study is credible, since it has been shown previously that daytime sleepiness from any cause is associated with increased crash risk.30–32 Our finding extends existing knowledge because the most recent systematic review of this topic, which utilized mostly underpowered studies, found no substantial association between ESS scores and crash risk in studies of drivers with OSA. The large number of subjects and incidents in our study has provided the power to examine this association following adjustment for confounders. Most studies in this area of research are based on self-reported crashes or near-misses and are thus subject to some bias. The questions about driving in this study were asked as part of a general sleep health questionnaire answered at first attendance at the sleep clinic and not in relation to occupation. A high response rate was recorded, but the problem of non-response for near-miss and crash questions remains. Nevertheless, under-reporting of incidents would tend to bias findings towards the null hypothesis and strengthen the positive findings of our study.
A limitation of the data collection method used in our study relates to use of self-reported crash data over the entire driving history for the WASHS cohort, which may have resulted in some recall or report bias. The overall crash rate for patients was compared with police-reported crash rate for the community, and this difference of method may be confounded by measurement bias. Future studies would benefit from the use of objective crash records to improve accuracy. In general, published data supporting increased crashes in OSA are from studies of patients referred to a sleep clinic. However, Young and colleagues29 found that their results from a community sample free of clinic bias were comparable in magnitude to the clinic-based studies. Thus impaired drivers with sleep apnea were not over represented in clinic populations.29
The gender differences found in our study may be confounded by driving exposure, which we did not measure. More men than women are occupational drivers and thus at higher risk of crash.33 Future research should account for this important denominator when considering crash risk in OSA. Gender differences may be attributable to a higher degree of self-awareness of symptomology in women who self-regulate risk by avoidance of driving.29
Clinical Relevance/Implications of Findings
These results for our sleep clinic patients can be used to guide clinical management. Our data support the belief that untreated patients with OSA have an increased crash risk but add to this the observation that it is those patients with increased sleepiness regardless of OSA severity who are most at risk. Current Australian Fitness to Drive guidelines have recommended that individuals should be advised to avoid or limit driving if they are sleepy, and should not drive if they are at high risk.34 High-risk individuals include: those with moderate to severe excessive daytime sleepiness (ESS 16-24), those with a history of frequent self-reported sleepiness while driving, and those who have had a crash caused by inattention or sleepiness. These guidelines are particularly relevant for commercial vehicle drivers, given that OSA approximately doubles crash risk and close to half of commercial drivers have OSA.7–9,35 Clearly it is important that OSA is diagnosed and the degree of associated sleepiness assessed to expedite treatment and minimize risk. It is known that effective treatment of OSA (e.g., with continuous positive airways pressure) reduces the risk of crash.36 Recently Sunwoo et al. have shown that a single administration of some objective tests of sleepiness (in particular, the psychomotor vigilance test and the divided attention driving task) can be used routinely in clinical practice to assess sleepiness for diagnostic purposes and for follow-up of outcomes of therapy.37 This study of commercial drivers provides evidence for a cost-effective routine test that can be applied to occupational drivers to assess risk.
There have been several large studies that have identified similar relationships between sleepiness on the ESS and MVCs in general driving populations.13,14,20 Phillip et al.20 reported that sleepy driving accidents were associated with an odds ratio of 5 where ESS was greater than 15 in a large sample of French drivers. Powell and colleagues13 conducted a large online survey of drivers in the US and found a significant dose-response relationship between self-report sleepy near-misses and an actual accident. Thus the relationship between sleepy driving and crash risk is not confined to those with sleep disorders, but may result from volitional sleep restriction.38
It is not yet clear why there is a substantial variation in the degree of sleepiness observed among individuals with equivalent severities of OSA as measured by AHI. Intuitively a patient with severely disordered breathing during sleep with consequent frequent arousals might be expected to be more disabled by sleepiness than one with less sleep disruption. Our findings demonstrate this is not consistently the case and the developing field of research addressing differing neurobehavioral vulnerability to sleep loss may shed light on this subject.39 Sleep deprivation studies in normal healthy subjects have shown significant variation between individuals in neurobehavioral deficits with sleep loss, although the effects on each individual are reproducible.40 It appears that up to 92% of the variance in cognitive deficits and subjective sleepiness between individuals may be explained by systematic variability.40
Cluydts et al. have suggested that “trait” or person-specific aspects of sleepiness have been largely ignored in sleep wake research.41 It appears likely that the sleepiness “trait” for an individual is comprised of several endogenous factors such as their genetic phenotype for sleep propensity (morningness or eveningness), arousal threshold, gender differences in perception, and sensitivity to both stimulant (e.g., caffeine) and sedative (e.g., alcohol) compounds. There will be an interactive effect with environmental or situational factors such as shift work and behaviorally induced insufficient sleep, and consideration must be given to medication use and comorbid medical conditions. Thus the sleepiness phenotype for an individual is likely to be defined by a complex interaction of endogenous and environmental factors. An individual's baseline or “trait” level of sleepiness will determine their vulnerability to the additional load of sleep loss imposed by OSA.
In summary, sleep clinic patients with untreated OSA have significantly more crashes than the general population. Our study suggests that sleepiness in untreated OSA is an important contributor to crash risk, particularly in men, underlining the importance of advising such patients, and the community generally, against drowsy driving.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr Hillman has conducted sponsored research for ResMed Incorporated and provided medical advice on the Medical Advisory Committee for Apnex Incorporated. WASHS was supported by Sir Charles Gairdner Hospital Research Foundation, the Hollywood Private Hospital Research Foundation and the ARK, open source software for medical research (National Health and Medical Research Council of Australia Enabling Facility). K. Ward is supported by an Australian Postgraduate Award and Ad Hoc scholarships from the Sir Charles Gairdner Research Foundation and ResMed Ltd. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors gratefully acknowledge E. Hudson, J. Lee, G. Love, and patients who have participated in WASHS.
REFERENCES
- 1.American Academy of Sleep Medicine Task Force, Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 2.Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med. 2009;5:573–81. [PMC free article] [PubMed] [Google Scholar]
- 3.Teran-Santos J, Jimenez-Gomez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. Cooperative Group Burgos-Santander. N Engl J Med. 1999;340:847–51. doi: 10.1056/NEJM199903183401104. [DOI] [PubMed] [Google Scholar]
- 4.Sagaspe P, Taillard J, Chaumet G, et al. Maintenance of wakefulness test as a predictor of driving performance in patients with untreated obstructive sleep apnea. Sleep. 2007;30:327–30. [PubMed] [Google Scholar]
- 5.Mulgrew AT, Nasvadi G, Butt A, et al. Risk and severity of motor vehicle crashes in patients with obstructive sleep apnoea/hypopnoea. Thorax. 2008;63:536–41. doi: 10.1136/thx.2007.085464. [DOI] [PubMed] [Google Scholar]
- 6.Pack AI, Pack AM, Rodgman E, Cucchiara A, Dinges DF, Schwab CW. Characteristics of crashes attributed to the driver having fallen asleep. Accid Anal Prev. 1995;27:769–75. doi: 10.1016/0001-4575(95)00034-8. [DOI] [PubMed] [Google Scholar]
- 7.Howard ME, et al. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170:1014–21. doi: 10.1164/rccm.200312-1782OC. [DOI] [PubMed] [Google Scholar]
- 8.Sharwood LN, Elkington J, Stevenson M, et al. Assessing sleepiness and sleep disorders in Australian long-distance commercial vehicle drivers: self-report versus an “at home” monitoring device. Sleep. 2012;35:469–75. doi: 10.5665/sleep.1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vennelle M, Engleman HM, Douglas NJ. Sleepiness and sleep-related accidents in commercial bus drivers. Sleep Breath. 2010;14:39–42. doi: 10.1007/s11325-009-0277-z. [DOI] [PubMed] [Google Scholar]
- 10.George CF. Sleep apnea, alertness, and motor vehicle crashes. Am J Respir Crit Care Med. 2007;176:954–6. doi: 10.1164/rccm.200605-629PP. [DOI] [PubMed] [Google Scholar]
- 11.Ellen RL, Marshall SC, Palayew M, Molnar FJ, Wilson KG, Man-Son-Hing M. Systematic review of motor vehicle crash risk in persons with sleep apnea. J Clin Sleep Med. 2006;2:193–200. [PubMed] [Google Scholar]
- 12.Barach P, Small SD. Reporting and preventing medical mishaps: lessons from non-medical near miss reporting systems. BMJ. 2000;320:759–63. doi: 10.1136/bmj.320.7237.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Powell NB, Schechtman KB, Riley RW, Guilleminault C, Chiang RP, Weaver EM. Sleepy driver near-misses may predict accident risks. Sleep. 2007;30:331–42. doi: 10.1093/sleep/30.3.331. [DOI] [PubMed] [Google Scholar]
- 14.Sagaspe P, Taillard J, Bayon V, et al. Sleepiness, near-misses and driving accidents among a representative population of French drivers. J Sleep Res. 2010;19:578–84. doi: 10.1111/j.1365-2869.2009.00818.x. [DOI] [PubMed] [Google Scholar]
- 15.Mukherjee S, Hillman D, Lee J, et al. Cohort profile: the Western Australian Sleep Health Study. Sleep Breath. 2012;16:205–15. doi: 10.1007/s11325-011-0491-3. [DOI] [PubMed] [Google Scholar]
- 16.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 17.Marchant RJ, Hill DL, Caccianiga RA, Gant PD. Western Australia: Road Safety Council of Western Australia; 2006. Reported road crashes in Western Australia 2006. [Google Scholar]
- 18.Rechstaffen A, Kales A. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Los Angeles: Brain Information Service; 1968. [Google Scholar]
- 19.Turkington PM, et al. Relationship between obstructive sleep apnoea, driving simulator performance, and risk of road traffic accidents. Thorax. 2001;56:800–5. doi: 10.1136/thorax.56.10.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Philip P, Sagaspe P, Lagarde E, et al. Sleep disorders and accidental risk in a large group of regular registered highway drivers. Sleep Med. 2010;11:973–9. doi: 10.1016/j.sleep.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 21.Johns MW. A new perspective on sleepiness. Sleep Biol Rhythms. 2010;8:170–9. [Google Scholar]
- 22.Chervin RD. Sleepiness, fatigue, tiredness, and lack of energy in obstructive sleep apnea. Chest. 2000;118:372–9. doi: 10.1378/chest.118.2.372. [DOI] [PubMed] [Google Scholar]
- 23.Johns M, Hocking B. Daytime sleepiness and sleep habits of Australian workers. Sleep. 1997;20:844–9. doi: 10.1093/sleep/20.10.844. [DOI] [PubMed] [Google Scholar]
- 24.Kribbs NB, Getsy JE, Dinges DF. Investigation and management of daytime sleepiness in sleep apnea. In: Saunders NA, Sullivan CE, editors. Sleep and breathing. New York: Marcel Dekker; 1994. pp. 575–604. [Google Scholar]
- 25.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 26.Gottlieb DJ, Whitney CW, Bonekat WH, et al. Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study. Am J Respir Crit Care Med. 1999;159:502–7. doi: 10.1164/ajrccm.159.2.9804051. [DOI] [PubMed] [Google Scholar]
- 27.Kapur VK, Baldwin CM, Resnick HE, Gottlieb DJ, Nieto FJ. Sleepiness in patients with moderate to severe sleep-disordered breathing. Sleep. 2005;28:472–7. doi: 10.1093/sleep/28.4.472. [DOI] [PubMed] [Google Scholar]
- 28.Stradling JR, Davies RJ. Is it necessary to record sleep? Sleep. 1996;19:S251–4. doi: 10.1093/sleep/19.suppl_10.s251. [DOI] [PubMed] [Google Scholar]
- 29.Young T, Blustein J, Finn L, Palta M. Sleep-disordered breathing and motor vehicle accidents in a population-based sample of employed adults. Sleep. 1997;20:608–13. doi: 10.1093/sleep/20.8.608. [DOI] [PubMed] [Google Scholar]
- 30.Robb G, Sultana S, Ameratunga S, Jackson R. A systematic review of epidemiological studies investigating risk factors for work-related road traffic crashes and injuries. Inj Prev. 2008;14:51–8. doi: 10.1136/ip.2007.016766. [DOI] [PubMed] [Google Scholar]
- 31.Lardelli-Claret P, Jiménez-Moleón JJ, Luna-del-Castillo Jde D, García-Martín M, Moreno-Abril O, Bueno-Cavanillas A. Comparison between two quasi-induced exposure methods for studying risk factors for road crashes. Am J Epidemiol. 2006;163:188–95. doi: 10.1093/aje/kwj015. [DOI] [PubMed] [Google Scholar]
- 32.Connor J, Norton R, Ameratunga S, et al. Driver sleepiness and risk of serious injury to car occupants: population based case control study. BMJ. 2002;324:1125. doi: 10.1136/bmj.324.7346.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Knipling RR, Boyle LN, Hickman JS, et al. CTBSSP Synthesis Report 4: Individual Differences and the High-Risk Commercial Driver. Washington, DC: Commercial Truck and Bus Safety Synthesis Program, Transportation Research Board; 2004. [Google Scholar]
- 34.Austroads. Assessing fitness to drive. Sydney, Australia: Austroads Ltd; 2012. p. 160. [Google Scholar]
- 35.Pack AI, Maislin G, Staley B, et al. Impaired performance in commercial drivers: role of sleep apnea and short sleep duration. Am J Respir Crit Care Med. 2006;174:446–54. doi: 10.1164/rccm.200408-1146OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tregear S, Reston J, Schoelles K, Phillips B. Continuous positive airway pressure reduces risk of motor vehicle crash among drivers with obstructive sleep apnea: systematic review and meta-analysis. Sleep. 2010;33:1373–80. doi: 10.1093/sleep/33.10.1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sunwoo BY, Jackson N, Maislin G, Gurubhagavatula I, George CF, Pack AI. Reliability of a single objective measure in assessing sleepiness. Sleep. 2012;35:149–58. doi: 10.5665/sleep.1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Powell NB, Chau JK. Sleepy driving. Med Clin North Am. 2010;94:531–40. doi: 10.1016/j.mcna.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 39.Van Dongen HP, Vitellaro KM, Dinges DF. Individual differences in adult human sleep and wakefulness: Leitmotif for a research agenda. Sleep. 2005;28:479–96. doi: 10.1093/sleep/28.4.479. [DOI] [PubMed] [Google Scholar]
- 40.Van Dongen HP, Baynard MD, Maislin G, Dinges DF. Systematic interindividual differences in neurobehavioral impairment from sleep loss: evidence of trait-like differential vulnerability. Sleep. 2004;27:423–33. [PubMed] [Google Scholar]
- 41.Cluydts R, De Valck E, Verstraeten E, Theys P. Daytime sleepiness and its evaluation. Sleep Med Rev. 2002;6:83–96. doi: 10.1053/smrv.2002.0191. [DOI] [PubMed] [Google Scholar]


