Abstract
Varenicline is a partial agonist at the α4β2 nicotinic acetylcholine receptor effective as smoking cessation pharmacotherapy. We present a familial case of severe restless legs syndrome (RLS) resistant to polytherapy who showed a consistent and effective amelioration of RLS symptoms after introduction of varenicline as antismoking drug.
Citation:
Romigi A; Vitrani G. Improvement of restless legs syndrome by varenicline as antismoking treatment. J Clin Sleep Med 2013;9(10):1089-1090.
Keywords: Restless legs syndrome, varenicline, nicotinic acetylcholine receptor agonist
Varenicline is a partial agonist at the α4β2 nicotinic acetylcholine receptor (nAChR). As a partial agonist, varenicline offers the therapeutic benefit of relieving symptoms of nicotine withdrawal and cigarette craving through its agonist actions while blocking the reinforcing effects of continued nicotine use through an antagonist action.1 It is thought that the addictive properties of nicotine are mediated mainly through its action as an agonist at α4β2 nAChRs, which stimulates the release of dopamine.2 It is still debated if nicotine may really modulate RLS symptoms. In addition, cigarette smoking may induce improvement of RLS symptoms in such case reports.3
REPORT OF CASE
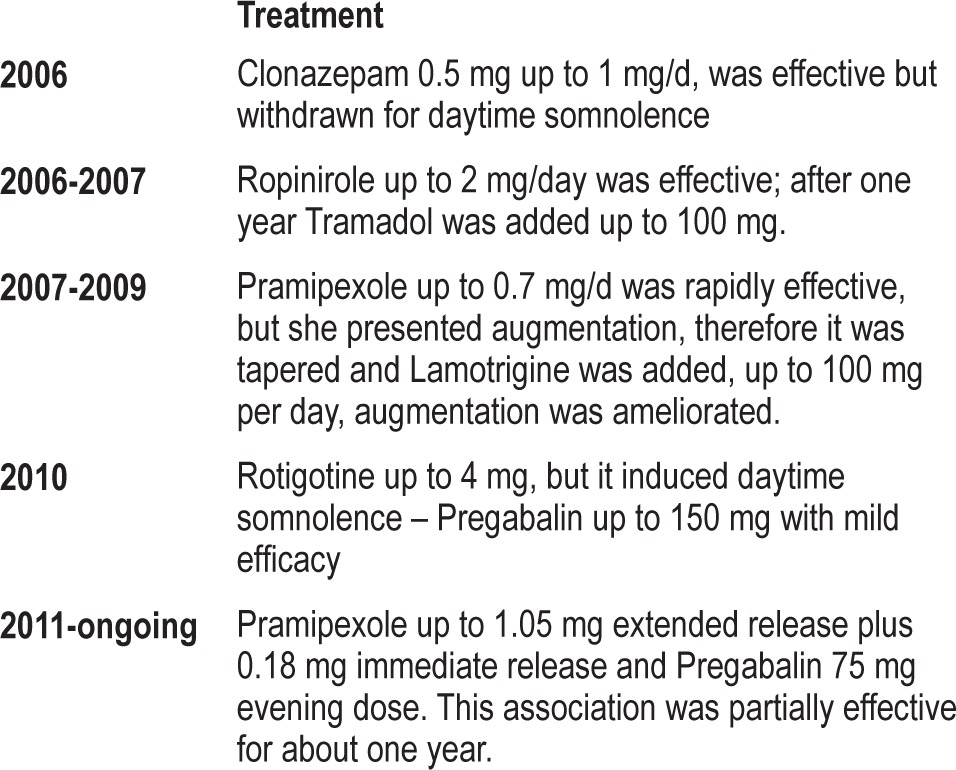
A 74-year-old woman with positive family history of RLS has been suffering from RLS for 6 years, although she referred sporadic symptoms at least 10 years before clinical diagnosis. Neurological examination was negative. Blood investigations and electromyographic exam excluded a secondary form. The severity of RLS symptoms had increased in the last 3 years. Episodes of “crawly” sensations in her legs accompanied by an urge to move them were evident in the evening. Walking was effective to improve the symptoms, but they returned soon after stopping the activity. Her symptoms fulfilled the RLS diagnostic criteria. She was treated with several drugs (see Table 1) but these did not completely control her RLS symptoms. After initial clinical response, she experienced augmentation phenomenon, characterized by earlier symptom onset, greater severity at the same dose, and reduced latency to onset with rest.
Table 1.
Detailed history of RLS treatment
She had a long history of smoking more than 25-30 cigarettes daily during the previous 40 years without any long period of abstinence. To help her stop smoking, her general practitioner prescribed varenicline treatment. She started a 12-week scheduled treatment at a dosage of 1 mg twice daily following a 1-week titration (days 1-3, 0.5 mg once daily; days 4-7, 0.5 mg twice daily). After the first week, varenicline provided a partial but remarkable improvement of RLS symptoms.
During habitual treatment with pramipexole (1.05 mg extended release plus 0.18 mg immediate release) and pregabalin (75 mg in the evening), her IRLS score was 22. After one week of treatment with varenicline, 2 mg daily was added to her treatment regimen for RLS, and her IRLS score decreased to 6. In addition, the patient had complained of RLS symptoms every day before varenicline introduction, but after addition of varenicline, mild RLS symptoms were evident only twice a week. IRLS score was also repeated every 2 weeks (4th week = 4; 6th week = 9; 8th week = 6). At 9 weeks, we attempted to reduce pramipexole dosage, with a slow reduction to 0.52 mg extended release plus 0.18 mg immediate release. The RLS symptoms immediately increased (IRLS score 16), probably due to acute withdrawal effect; therefore, the patient asked to maintain her regular dosages (pramipexole 1.05 extended release plus 0.18 mg immediate release and pregabalin 75 mg daily). At 12 weeks, her IRLS score was 11. In the meantime, the patient obtained the cessation of her smoking. As reported in the standard schedule, varenicline was stopped after 12 weeks. After the withdrawal the patient experienced an increase in RLS symptoms in the evening. They were evident more than 4 days per week, and her IRLS score at both 13 and 15 weeks was 21.
DISCUSSION
We described a case of severe RLS who showed a significant amelioration of evening symptoms after the introduction of varenicline, a partial agonist at the α4β2 nAChRs. Although the exact mechanism responsible for the amelioration of severe RLS symptoms by varenicline is unclear, we suppose that this nicotine partial agonist may stimulate the release of dopamine2 and consequently induce the positive effect on RLS in our patient. Varenicline may induce an elevation of dopa-mine release in the mesolimbic and nigrostriatal dopaminergic pathways, showing a critical and dominant effect from striatal synaptosomes in rat and monkey striatum.4 Therefore, as also suggested in Parkinson disease in several studies,5 the amelioration of RLS may be due to stimulation of dopamine release by means of stimulation of nAChRs. This result is in line with the recent report of alleviation of RLS induced by nicotinic stimulation due to cigarette smoking.3 Our patient experienced augmentation phenomenon as demonstrated by the progressive increase of dosages and the worsening of RLS symptoms not explained by other factors. Therefore varenicline seems to be effective for RLS symptoms in a patient affected by idiopathic RLS who experienced augmentation. It is well known that this phenomenon is treatment-related; of note, a reduction in dopaminergic dose often ameliorates augmentation, returning symptoms to pretreatment levels.6 However, in our case the reduction of pramipexole during varenicline treatment induced a rapid impairment of RLS. In addition, the reappearance of RLS symptoms after varenicline withdrawal and its probable dopamine-mediated mechanism may suggest a direct effect on RLS symptoms and weaken the hypothesis of an augmentation-related effect.
Although a single case report does not allow generalization, our findings should suggest exploration of the possibility of an effective treatment for RLS by means of nicotine-related compounds.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Obach RS, Reed-Hagen AE, Krueger SS, et al. Metabolism and disposition of varenicline, a selective α4β2 acetylcholine receptor partial agonist, in vivo and in vitro. Drug Metab Dispos. 2006;34:121–30. doi: 10.1124/dmd.105.006767. [DOI] [PubMed] [Google Scholar]
- 2.Coe JW, Brooks PR, Vetelino MG, et al. Varenicline: an alpha4beta2 nicotinic receptor partial agonist for smoking cessation. J Med Chem. 2005;48:3474–7. doi: 10.1021/jm050069n. [DOI] [PubMed] [Google Scholar]
- 3.Oksenberg A. Alleviation of severe restless legs syndrome (RLS) symptoms by cigarette smoking. J Clin Sleep Med. 2010;6:489–90. [PMC free article] [PubMed] [Google Scholar]
- 4.Bordia T, Hrachova M, Chin M, McIntosh JM, Quik M. Varenicline is a potent partial agonist at α6β2* nicotinic acetylcholine receptors in rat and monkey striatum. J Pharmacol Exp Ther. 2012;342:327–34. doi: 10.1124/jpet.112.194852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hernán MA, Zhang SM, Rueda-deCastro AM, Colditz GA, Speizer FE, Ascherio A. Cigarette smoking and the incidence of Parkinson's disease in two prospective studies. Ann Neurol. 2001;50:780–6. doi: 10.1002/ana.10028. [DOI] [PubMed] [Google Scholar]
- 6.Garcia-Borreguero D, Allen RP, Kohnen R, et al. Diagnostic standards for dopaminergic augmentation of restless legs syndrome: Report from a World Association of Sleep Medicine—International Restless Legs Syndrome Study Group Consensus Conference at the Max Planck Institute. Sleep Med. 2007;8:520–30. doi: 10.1016/j.sleep.2007.03.022. [DOI] [PubMed] [Google Scholar]


