Abstract
Pulmonary arterial hypertension (PAH) is a progressive and life-threatening disease. Understanding of PAH prevalence remains limited, but PAH has been reported as a frequent complication in connective tissue diseases. This study estimated prevalence of PAH in patients with connective tissue diseases and prevalence of idiopathic PAH using a systematic review of the literature. We searched PubMed through May 19, 2012 for all studies on prevalence of PAH in patients with connective tissue diseases or prevalence of idiopathic PAH. To be included, studies had to be in English, have humans as subjects, and determine prevalence within a time interval of up to 2 years. Studies only investigating pediatric patients were excluded. Pooled prevalence estimates were calculated. Twenty studies were identified in the review. Seventeen of the 20 studies reported prevalence of PAH in connective tissue diseases and three reported prevalence of idiopathic PAH. The pooled prevalence estimate of idiopathic PAH was 12 cases per million population (95 % CI 5 cases per million to 22 cases per million) with estimates ranging from 5.9 cases per million population to 25 cases per million population. The pooled prevalence estimate of PAH in patients with connective tissue diseases was 13 % (95 % CI, 9.18 % to 18.16 %) with reported estimates ranging from 2.8 % to 32 %. Prevalence of PAH in patients with connective tissue diseases was substantially higher than that of idiopathic PAH based on pooled prevalence estimates. Comparisons of PAH prevalence in persons with connective tissue disease and idiopathic PAH using a large observational study would be helpful in better assessing relative prevalence.
Keywords: Connective tissue diseases, Prevalence, Pulmonary hypertension, Review
Introduction
Pulmonary hypertension is defined as a mean pulmonary artery pressure of at least 25 mm Hg at rest [1]. One subgroup of pulmonary hypertension, pulmonary arterial hypertension (PAH), is a progressive and life-threatening disease characterized by elevation of mean pulmonary arterial pressure and pulmonary vascular resistance, leading to right heart failure and death [2].
PAH is an important complication of connective tissue diseases, a group of disorders characterized by vascular injury, autoimmunity, tissue inflammation, and organ dysfunction [3, 4] including systemic sclerosis [5], systemic lupus erythematosus [6], mixed connective tissue diseases [7, 8], and to a lesser extent, rheumatoid arthritis, polymyositis/dermatomyositis, and Sjogren’s syndrome [9].
Data on prevalence of PAH in patients with connective tissue diseases remain limited due to rare occurrence of the disease [10–12] and challenges to obtain high-quality data appropriate for prevalence estimation [9]. This systematic literature review was conducted to estimate prevalence of PAH in patients with connective tissue diseases and prevalence of idiopathic pulmonary arterial hypertension based on data from the literature.
Materials and methods
Literature search strategy
Publications examining prevalence of idiopathic pulmonary arterial hypertension and prevalence of pulmonary arterial hypertension in patients with connective tissue diseases were identified by a PubMed search specifying publication date from inception through May 19, 2012. To identify studies estimating prevalence of idiopathic pulmonary arterial hypertension, a search combined the medical subject heading “Hypertension, Pulmonary/epidemiology” or supplementary concept “Pulmonary arterial hypertension” with the term idiopathic was used, and the medical subject heading “Hypertension, Pulmonary” combined with any of the terms “epidemiology,” “prevalence,” “frequency,” “occurrence,” or “incidence”, and with the term idiopathic was also used. In addition, a search restricted to studies, in which the medical subject heading "Hypertension, Pulmonary/epidemiology” was identified as the main topic was conducted. To identify studies, which estimated prevalence of PAH in patients with connective tissue diseases, a search combined the medical subject headings “Hypertension, Pulmonary,” or supplementary concept “Pulmonary arterial hypertension,” or term “pulmonary arterial hypertension,” with the medical subject heading “Connective tissue disease,” or either of the terms “connective tissue diseases,” “scleroderma,” “systemic sclerosis,” “lupus,” “mixed connective tissue disease,” “rheumatoid arthritis,” “Sjogren's,” “Sjogren, ” “polymyositis,” or “dermatomyositis” was conducted. A search with the medical subject heading “Prevalence” or medical subheading “epidemiology” or terms including “prevalence,” “frequency,” “occurrence,” or “incidence” combined with the above search was also conducted. Reference lists of articles obtained from the results in PubMed search were also examined to identity articles.
Inclusion and exclusion criteria
All the titles and abstracts of the results in searches were reviewed to determine if the objectives of the studies were relevant to prevalence of idiopathic pulmonary arterial hypertension or prevalence of PAH in patients with connective tissue diseases. To be included, articles had to be written in English and have human subjects. Studies were required to have reported a PAH prevalence in patients with connective tissue diseases or an idiopathic pulmonary arterial hypertension prevalence. Studies were required to report prevalence for an interval less than or equal to 2 years. Articles only investigating pediatric patients, i.e., with age less than 18 years old were excluded. Articles which only reviewed prior studies were excluded, since the original studies were examined in this review. Only studies with full text in English were included. Case reports, letters to the editor, and editorials were excluded.
Data analysis
Estimates of prevalence of PAH in patients with each type of connective tissue disease including systemic sclerosis, systemic lupus erythematosus, mixed connective tissue diseases, and rheumatoid arthritis and estimates of the prevalence of idiopathic pulmonary arterial hypertension were extracted from reviewed articles. A summary table including author, title, journal, published year, study period, objectives, data source, disease definition, country in which the study was conducted, and main findings of each study was created (Table 1). To estimate the prevalence of idiopathic pulmonary arterial hypertension and prevalence of PAH in patients with each type of connective tissue disease for which more than one study was found, proportion meta-analyses were conducted.
Table 1.
Prevalence of idiopathic pulmonary arterial hypertension and prevalence of PAH in patients with connective tissue diseases
| Author, title, journal | Published year | Study period | Objectives | Data source | Disease definition | Country | Prevalence (patients with PAH/sample size) |
|---|---|---|---|---|---|---|---|
| Idiopathic pulmonary arterial hypertension | |||||||
| Peacock A.J., et al. An epidemiological study of pulmonary arterial hypertension. Eur Respir J | July 2007 | National hospitalization registry data: between 1986 to 2002 | To determine the epidemiological features of PAH within a whole population over a prolonged period from two perspectives, inexpert and expert, a national hospitalization registry and the specialist center for PAH management in Scotland. | National hospitalization registry data in Scotland | Having code of PAH in the absence of any explanatory concurrent diagnosis from prior hospitalizations based on combination of concurrently recorded diagnoses and coding data from any prior hospitalizations | Scotland | 25 cases per million population (80/3, 200,000) |
| Humbert M, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med | May, 2006 | Between October 2002 to October 2003 | To describe clinical and hemodynamic parameters and to provide estimates for the prevalence of PAH patients diagnosed for PAH according to a standardized definition | National registry in 17 university hospitals in France | Mean pulmonary arterial pressure >25 mm Hg at rest and a pulmonary artery wedge pressure less than 15 mm Hg | France | 5.9 cases per million population (264/44, 700,000) |
| Tueller C, et al. Epidemiology of pulmonary hypertension: new data from the Swiss registry. Swiss Med Wkly | June, 2008 | Between January 1999 to December 2004 | To analyze the epidemiological aspects of data from all pulmonary hypertension (PH) centers in Switzerland and focus on basic clinical characteristics of PH patients and estimated burden of the disease in the population | PH patient registry from all PH centers in Switzerland | Not specified (PH was defined as a mean pulmonary artery pressure of >25 mm Hg at rest or >30 mm Hg during exercise) 72 % of patients underwent right heart catheterization | Switzerland | 8.6 cases per million population (52/6,000,000) |
| PAH in systemic sclerosis | |||||||
| Hachulla E, et al. Early detection of pulmonary arterial hypertension in systemic sclerosis: a French nationwide prospective multicenter study. Arthritis Rheum | 2005 | Between September 2002 to July 2003 | To develop an screening algorithm based on symptoms, echocardiography, and right heart catheterization for application to a nationwide multicenter systemic sclerosis population in France | Data from 21 systemic sclerosis centers in France | A mean pulmonary artery pressure ≥25 mm Hg at rest or ≥30 mm Hg during exercise, with pulmonary artery wedge pressure <15 mm Hg on right heart catheterization | France | 7.85 % (47/599) |
| Hachulla et al. Risk factors for death and the 3-year survival of patients with systemic sclerosis: the French ItinerAIR-Sclerodermie study. Rheumatology | 2009 | Between September 2002 and July 2003 | To investigate survival, risk factors and causes of death in the multicenter ItinerAIR-Sclerodermie cohort of patients with systemic sclerosis without severe pulmonary fibrosis or severe left heart disease at baseline | Data from 20 French specialized scleroderma centers | A mean pulmonary arterial pressure ≥25 mm Hg at rest or ≥30 mm Hg during exercise, with mean pulmonary arterial wedge pressure <15 mm Hg on right heart catheterization | France | 8.6 % (47/546) |
| Avouac, et al. Prevalence of pulmonary hypertension in systemic sclerosis in European Caucasians and metaanalysis of 5 studies. J Rheumatol | 2010 | Not specified. (Point prevalence estimation) | To measure the prevalence of the different types of PH, using right heart catheterization, in 2 large European samples of patients presenting with systemic sclerosis. | Data from patients with systemic sclerosis at 6 French and 5 Italian medical centers | A mean resting pulmonary artery pressure of >25 mm Hg in the presence of a pulmonary capillary wedge pressure of ≤15 mm Hg at right heart catheterization, in the absence of prominent interstitial lung disease | France and Italy | 3.6 % (42/1,165) |
| Vonk et al. Systemic sclerosis and its pulmonary complications in The Netherland: an epidemiological study. Ann Rheum Dis | 2009 | Between 2005 and 2006 | To establish the prevalence and incidence of systemic sclerosis and its pulmonary complications | Combination of “Pulmonary Hypertension Screening, a Multidisciplinary Approach in Scleroderma” registry and a nationwide questionnaire | A mean pulmonary arterial pressure >25 mm Hg at rest with a normal wedge pressure on right heart catheterization | The Netherlands | 9.9 % (113/1,148) |
| Phung et al. Prevalence of pulmonary arterial hypertension in an Australian scleroderma population: screening allows for earlier diagnosis. Intern Med J | 2009 | Between July 1, 2005 and June 30, 2007 | To determine the prevalence of pulmonary complications, and especially PAH in an Australian scleroderma population | Data from Royal Perth Hospital (the state referral center for adult pulmonary hypertension) | A mean pulmonary artery pressure ≥25 mm Hg at rest or ≥30 mm Hg during exercise, with a concomitant pulmonary capillary wedge pressure <15 mm hg and pulmonary vascular resistance of >240 dynes/s per cm−5 on right heart catheterization | Australia | 13 % (24/184) |
| de Azevedo et al. Prevalence of pulmonary hypertension in systemic sclerosis. Clin Exp Rheumatol | 2005 | November 2001 to March 2003 (a cross sectional study) | To determine the prevalence of PAH in patients with a diagnosis of systemic sclerosis followed in a Brazilian tertiary university service | Data from patients with systemic sclerosis followed at the Unit of rheumatology of a university hospital | Pulmonary artery systolic pressure ≥40 mm Hg estimated by ECHO with the estimated right atrial pressure being 14 mm Hg, and/or as the presence of direct or indirect signs of PAH | Brazil | 14 % (8/57) |
| Coral-Alvarado et al. Risk factors associated with pumonary arterial hypertension in Colombian patients with systemic sclerosis: Review of the literature. J Rheumatol | 2008 | Not specified (a cross sectional study) | To investigate the clinical and laboratory characteristics associated with PAH in Colombian patients with systemic sclerosis | Data of patients with systemic sclerosis in five rheumatology units | A mean pulmonary artery systolic pressure >25 mm Hg at rest or a tricuspid regurgitation velocity >3 m/s or 2.5 m/s with unexplained dyspnea by echocardiogram | Colombia | 17 % (61/349) |
| Kumar et al. Prevalence and predictors of pulmonary artery hypertension in systemic sclerosis. J Assoc Physicians India | 2008 | Between 2004 to 2007 (a cross sectional study) | To study the prevalence of PAH in systemic sclerosis; to study the predictors of PAH in systemic sclerosis | Data from patients with systemic sclerosis at All India Institute of Medical Sciences | Transtricuspid gradient >35 mm Hg or right ventricular acceleration time of <90 ms. | India | 32 % (32/100) |
| Pope et al. Prevalence of elevated pulmonary arterial pressures measured by echocardiography in a multicenter study of patients with systemic sclerosis. J Rheumatol | 2005 | Between June 2002 and May 2003 | To estimate the prevalence of elevated pulmonary arterial pressures as a correlate for pulmonary arterial hypertension in patients with systemic sclerosis in rheumatology centers in Canada | Data from systemic sclerosis patients receiving care at rheumatology centers in Canada | systolic pulmonary arterial pressure >30 mm Hg or >35 mm Hg | Canada | 23 % (124/539) |
| Gińdzieńska-Sieśkiewicz et al. The occurrence of pulmonary hypertension in patients with systemic sclerosis hospitalized in the department of rheumatology and internal diseases medical university of Bialystok in years 2003–2004 | 2005 | Between 2003 and 2004 | To investigate the occurrence of pulmonary hypertension in systemic sclerosis patients hospitalized in Department of Rheumatology and Internal Diseases University Hospital of Bialystok | Data from patients with systemic sclerosis hospitalized in Department of Rheumatology and Internal Diseases University Hospital of Bialystok | A pulmonary artery systolic pressure >35 mm Hg by Doppler echocardiography | Poland | 6 % (3/53) |
| Chang et al. Scleroderma patients with combined pulmonary hypertension and interstitial lung disease. J Rheumatol | 2003 | Between January 1, 1990 and August 31, 2001(a cross-sectional study) | To study the demographics, clinical features, and prognosis of individuals with both vascular and interstitial lung disease | Data from patients with scleroderma seen at least once at a Scleroderma Center | Right ventricular systolic pressure or pulmonary artery pressure >35 by echocardiography | United States | 19.2 % (119/619) |
| Yamane et al. Clinical and laboratory features of scleroderma patients with pulmonary hypertension. Rheumatology (Oxford). | 2000 | Between 1990 and 1999 (a cross sectional study) | To examine the occurrence of pulmonary hypertension and investigated the clinical and laboratory features of systemic sclerosis patients with pulmonary hypertension | Data from 125 Japanese patients with systemic sclerosis | Pulmonary artery systolic pressure >40 mm Hg in absence severe pulmonary fibrosis | Japan | 11.2 % (14/125) |
| PAH in lupus | |||||||
| Pan et al. Primary and secondary pulmonary hypertension in systemic lupus erythematosus. Lupus | 2000 | 1995 | To describe the etiology and clinical profile of primary and secondary pulmonary hypertension in systemic lupus erythematosus patients | Data from 786 systemic lupus erythematosus patients diagnosed with SLE over the last twenty years at Tan Tock Seng Hospital | A pulmonary artery systolic pressure >30 mm Hg measured by Doppler analysis of tricuspid valve regurgitant jet velocity or right heart catheter measurements at angiography | Singapore | 2.8 % (22/786) |
| Prabu et al. Prevalence and risk factors for pulmonary arterial hypertension in patients with lupus. Rheumatology (Oxford) | 2009 | Between January 2004 to December 2005 (a cross-sectional study) | To estimate the point prevalence of PAH and identify risk factors for PAH in a large cohort of systemic lupus erythematosus patients | Data from lupus clinics in Birmingham, UK | Systolic pulmonary artery pressure >30 mm Hg by echocardiography | UK | 4.2 % (12/283) |
| PAH in rheumatoid arthritis | |||||||
| Dawson et al. Raised pulmonary artery pressures measured with Doppler echocardiography in rheumatoid arthritis patients. Rheumatology | 2000 | Not specified (a cross-sectional study) | To study the prevalence of echocardiographic abnormality and pulmonary hypertension in an unselected population of patients with rheumatoid arthritis | Data from 146 patients with rheumatoid arthritis in rheumatology outpatient departments of St Helens and Knowsley Hospitals NHS Trust | Estimated pulmonary arterial systolic pressure ≥30 mm Hg | UK | 21 % (30/146) |
| Keser et al. Pulmonary hypertension in rheumatoid arthritis. Scand J Rheumatol | 2004 | April 2002 and October 2002 | To investigate pulmonary arterial systolic pressure in rheumatoid arthritis using Doppler echocardiography | Data from 40 consecutive rheumatoid arthritis patients attending the Ege University Rheumatology Department | An estimated pulmonary arterial systolic pressure >30 mm Hg | Turkey | 27.5 % (11/40) |
| PAH in combined patients with systemic sclerosis and mixed connective tissue diseases | |||||||
| Wigley et al. The prevalence of undiagnosed pulmonary arterial hypertension in subjects with connective tissue disease at the secondary health care level of community-based rheumatologists (the UNCOVER study). Arthritis Rheum | 2005 | Not specified (point prevalence estimation) | To determine the point prevalence of undiagnosed PAH in community-based rheumatology practice by conducting a survey using Doppler echocardiography technology | Data from patients with connective tissue diseases in fifty community-based centers | According to current rheumatologist at the time of chart review; or estimated right ventricular systolic pressure ≥40 mm Hg | United States and Canada | 26.7 % (211/791) |
The StatsDirect statistical software package version 2.7.8b (StatsDirect Ltd, Cheshire, UK) was used to conduct proportion meta-analysis. The I 2 statistic in proportion meta-analysis, which describes the percentage of variation across studies in the outcome of interest due to heterogeneity rather than chance was used to decide whether a random-effects or fixed-effects model was appropriate for the analysis [13]. If the 95 % confidence interval on I 2 did not contain 0 %, it indicated that use of the random effects model was appropriate. Otherwise, the fixed-effects model should be used. The DerSimonian-Laird random-effects pooling method [14] was used in proportion meta-analysis if a random-effects model was chosen. The 95 % confidence intervals for the pooled prevalence estimate of idiopathic pulmonary arterial hypertension and for the pooled prevalence estimate of PAH in patients with connective tissue diseases, in patients with systemic sclerosis, in patients with systemic lupus erythematosus, and in patients with arthritis rheumatoid were calculated.
Although echocardiography is often used to initially diagnose PAH, right heart catheterization is necessary to confirm diagnosis [15]. Since PAH diagnosis based on echocardiography does not have the specificity of diagnosis by catheterization and therefore may inflate prevalence estimates [16], subgroup analysis was conducted, when possible, based on groups organized by whether right heart catheterization was used for confirmation of PAH diagnosis to assess the effect of not confirming diagnosis by catheterization on prevalence estimates.
Results
Articles on PAH prevalence
Three hundred one studies were screened to decide if inclusion criteria were met for articles reporting PAH prevalence in patients with connective tissue diseases. A total of 284 studies were excluded, 192 because they did not report prevalence of PAH in patients with connective tissue diseases, 34 only mentioned prevalence of PAH in patients with connective tissue disease reported in prior studies, and 24 reported PAH prevalence in patients with connective tissue diseases based on a study interval longer than 2 years. Ten excluded studies did not specify a study period during which PAH prevalence in patients with connective tissue was reported. Four articles were editorials; 14 were case reports, and four were letters or correspondence. Two were excluded because they reported PAH prevalence in patients with systemic sclerosis using the same data bases as other included studies [17, 18]. The remaining 17 articles were used in the meta-analysis of PAH prevalence in patients with connective tissue diseases.
Six hundred ninety-six articles were screened to identify articles which reported prevalence of idiopathic PAH. Ninety-six of the 696 articles also appeared in the search results for PAH prevalence in connective tissue diseases. A total of 693 articles were excluded, 604 because they did not report prevalence of idiopathic PAH, three reported prevalence of idiopathic PAH among pediatric patients only, and four articles only reported prevalence from prior studies. Twenty-eight excluded articles were letters; 25 were case reports; 29 were editorials. The remaining three articles were used in the meta-analysis of idiopathic pulmonary arterial hypertension.
A summary of selected studies reporting prevalence of PAH in patients with connective tissue diseases and prevalence of idiopathic pulmonary arterial hypertension is shown in Table 1. No studies were found that estimated prevalence of PAH in patients with connective tissue diseases in general. After exclusion, a total of 20 studies remained that met inclusion criteria for this study. Seventeen of the 20 studies reported prevalence of PAH in connective tissue diseases, and three reported prevalence of idiopathic pulmonary arterial hypertension. Twelve of the 17 studies reported prevalence of PAH in patients with systemic sclerosis [19–30]. Two of the 17 studies reported prevalence of PAH in patients with systemic lupus erythematosus [31, 32], two reported prevalence of PAH in patients with rheumatoid arthritis [33, 34], and one reported prevalence of PAH in a combined patients group with systemic sclerosis and mixed connective tissue diseases [35]. No studies were found that determined prevalence of PAH in patients with polymyositis/dermatomyositis or Sjogren’s syndrome.
Prevalence of idiopathic pulmonary arterial hypertension
Individual studies reported estimated prevalence of idiopathic pulmonary arterial hypertension ranging from 5.9 cases per million population to 25 cases per million population (Fig. 1). Based on the I 2 statistic, 97.6 % (95 % CI, 96 % to 98.3 %), the random effects model was used to estimate prevalence of idiopathic pulmonary arterial hypertension. The pooled prevalence estimate of idiopathic pulmonary arterial hypertension was 12 cases per million population (95 % CI, five cases per million population to 22 cases per million population). The Harboard test suggested that there was no bias across studies in prevalence of idiopathic pulmonary arterial hypertension (Table 2).
Fig. 1.
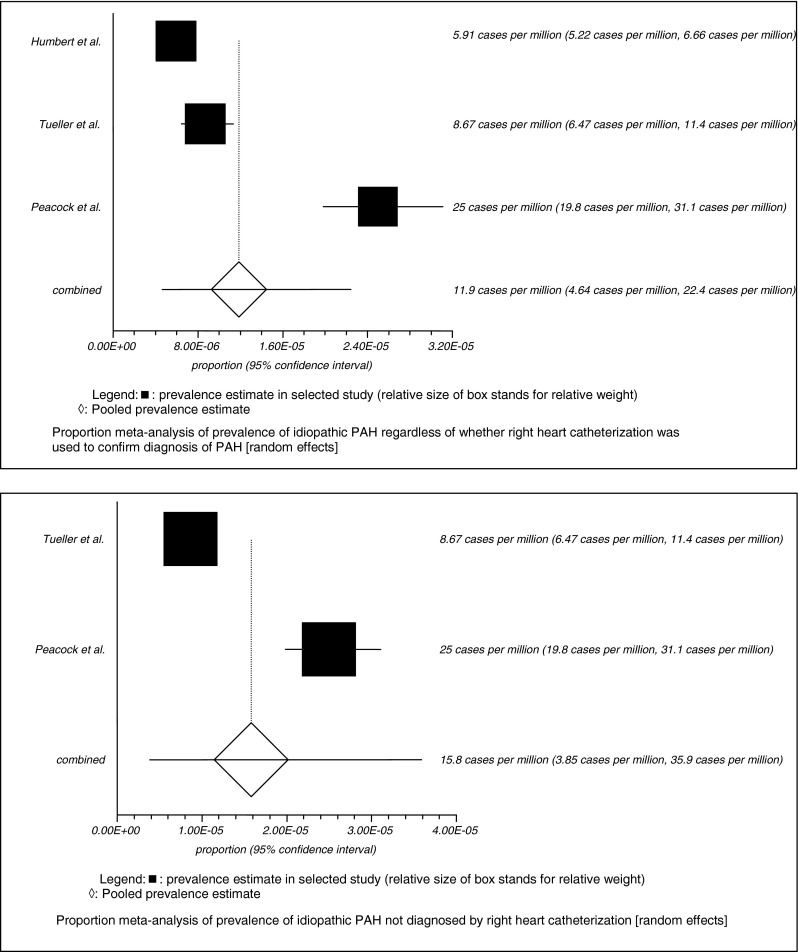
Proportion meta-analysis of prevalence of idiopathic pulmonary arterial hypertension for all groups and for subgroup not diagnosed by right heart catheterization
Table 2.
Results of non-combinability test and bias assessment for prevalence estimation
| Non-combinability | Bias assessment | P value | Confidence interval | |||
|---|---|---|---|---|---|---|
| I 2 | Cochran Q | Egger | Harbord | |||
| Idiopathic pulmonary arterial hypertension | 97.6 % | 96 % to 98.3 % (95 %) | ||||
| 12.11 | 0.3457 | −49.67 to 73.90 (92.5 %) | ||||
| Not diagnosed by right heart catheterization | 35.34 | <0.0001 | ||||
| PAH in connective tissue diseases | 96.8 % | 96.2 % to 97.3 % (95 %) | ||||
| 6.04 | 0.0031 | 2.38 to 9.69 (95 %) | ||||
| 3.37 | 0.3225 | −2.93 to 9.67 (92.5 %) | ||||
| PAH in systemic sclerosis | 95.5 % | 94.1 % to 96.4 % (95 %) | ||||
| 5.34 | 0.0121 | 1.45 to 9.23 (95 %) | ||||
| 4.07 | 0.2382 | −2.37 to 10.51 (92.5 %) | ||||
| Diagnosed by echocardiography | 79.6 % | 50.9 % to 88.5 % (95 %) | ||||
| −1.62 | 0.5386 | −7.91 to 4.68 (95 %) | ||||
| −1.66 | 0.439 | −6.09 to 2.77 (92.5 %) | ||||
| Diagnosed by right heart catheterization | 92 % | 84.4 % to 95 % (95 %) | ||||
| 6.03 | 0.1071 | −2.39 to 14.45(95 %) | ||||
| 5.43 | 0.3774 | −8.66 to 19.53 (92.5 %) | ||||
| PAH in lupus | 1.43 | 0.2313 | ||||
| PAH in rheumatoid arthritis | 0.93 | 0.3351 | ||||
Subgroup analysis by whether right heart catheterization was used for diagnosis
Among three studies reporting prevalence of idiopathic pulmonary arterial hypertension [10–12], diagnosis of PAH was confirmed by right heart catheterization in one study by Humbert et al. The other two studies did not use right heart catheterization for confirmation of all PAH diagnosis, although one of the two estimated prevalence in a cohort in which 72 % of patients underwent right heart catheterization [12]. The other study used International Classification of Diseases to identify idiopathic pulmonary arterial hypertension based on national hospitalization registry data for Scotland [10]. A subgroup proportion meta-analysis was conducted based on the two studies in which right heart catheterization was not used to confirm all diagnoses of PAH, since use of only echocardiograph for diagnosis may inflate prevalence estimates.
It was not possible to obtain an I 2 statistic since there were only two studies in the subgroup, so analyses using both random-effects model and fixed-effects model were conducted. Cochran’s Q, another statistic to measure heterogeneity, has low power as a comprehensive test of heterogeneity [36], especially when the number of studies is small. Even with this low-power Cochran’s Q was 35.34 (P < 0.0001), which suggested a random-effects model should be used in pooled prevalence estimation (Table 2). Bias assessment was not available due to having only two studies. The pooled idiopathic pulmonary arterial hypertension prevalence in the two studies without diagnosis confirmation via heart catheterization was 16 cases per million population (95 % CI, four cases per million population to 36 cases per million population) which was higher than the idiopathic pulmonary arterial hypertension prevalence estimate of 5.9 cases per million population in the one study in which right heart catheterization was used (Fig. 1).
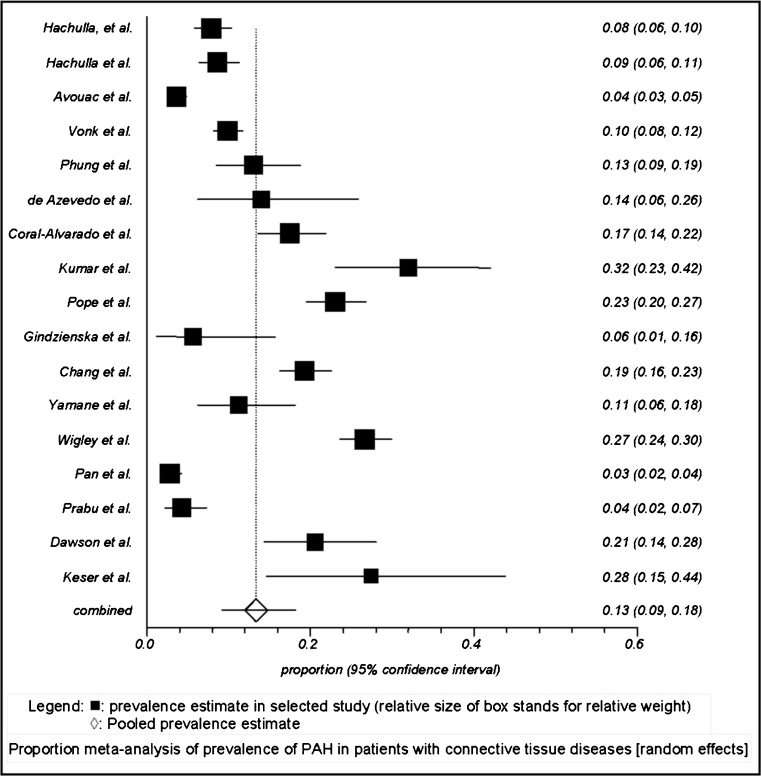
Prevalence of PAH with connective tissue diseases
Among the 17 studies that reported prevalence of PAH in patients with connective tissue diseases, estimates ranged from 2.8 % to 32 %. Based on the I 2 statistic, 96.8 % (95 % CI, 96.2 % to 97.3 %), a random-effects model was used to estimate PAH prevalence in patients with connective tissue diseases (Table 2). The pooled prevalence estimate of PAH in patients with connective tissue diseases was 13 % (95 % CI, 9.18 % to 18.16 %) (Fig. 2).
Fig. 2.
Proportion meta-analysis of prevalence of PAH in patients with connective tissue diseases
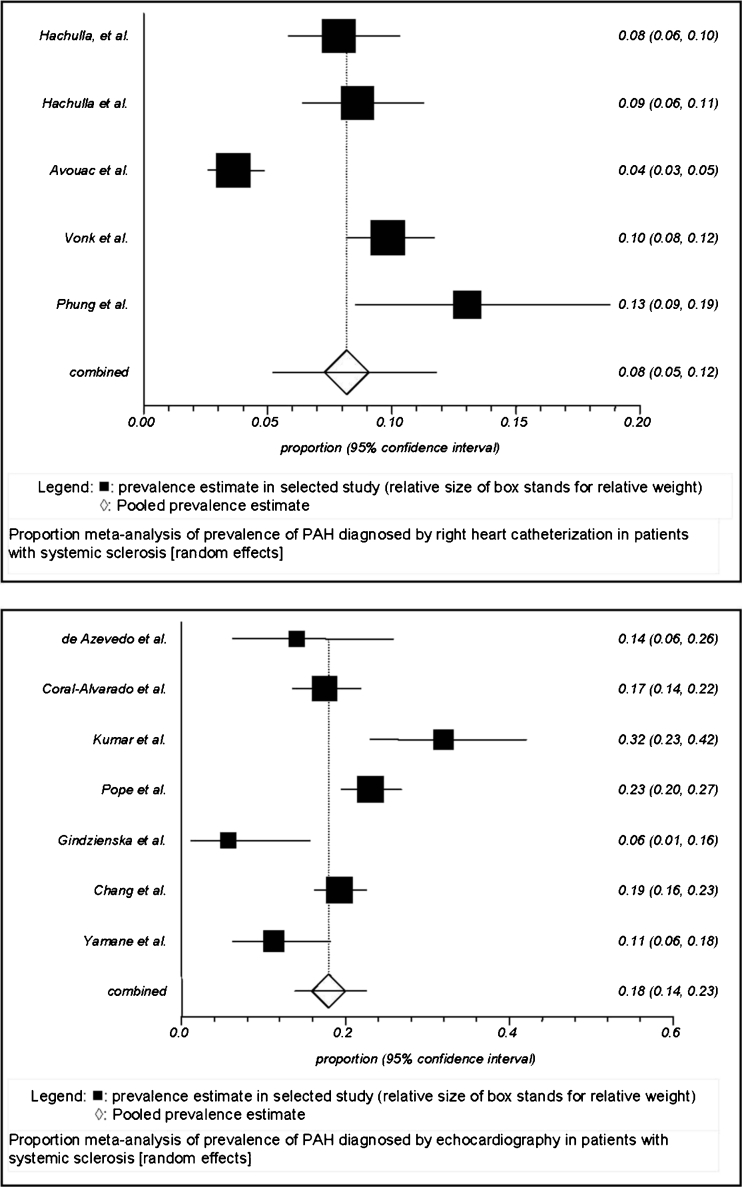
Systemic sclerosis
Twelve individual studies reported PAH prevalence ranging from 3.6 % to 32 % in patients with systemic sclerosis. Based on the I 2 statistic, 95.5 % (95 % CI, 94.1 % to 96.4 %), a random-effects model was used to estimate the prevalence of PAH in patients with systemic sclerosis (Table 2). The pooled prevalence estimate of PAH in patients with systemic sclerosis was 13 % (95 % CI, 8.96 % to 17.87 %) (Fig. 3)
Fig. 3.
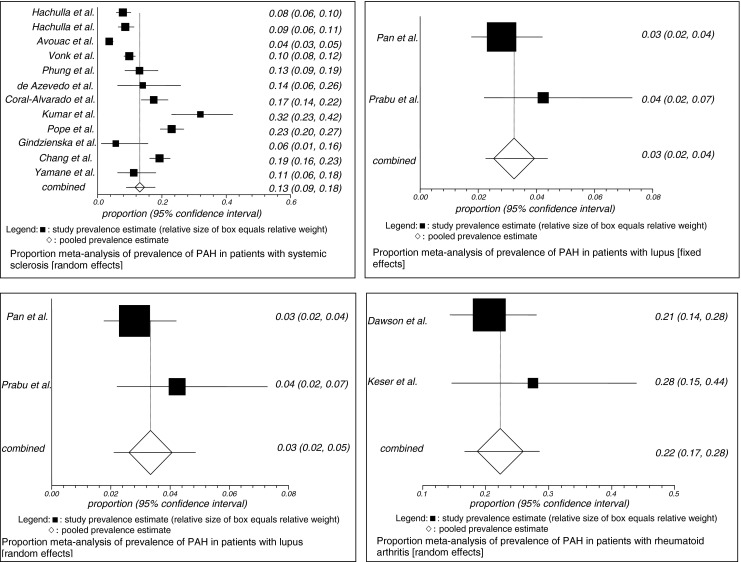
Proportion meta-analysis of prevalence of PAH in patients with systemic sclerosis, lupus, and rheumatoid arthritis
Systemic lupus erythematosus
Two studies reported prevalence of PAH ranging from 2.8 % to 4.2 % in patients with systemic lupus erythematosus. An I 2 statistic could not be obtained since only two studies were included. Cochran’s Q was 1.43 (P = 0.2313). Since Cochran’s Q test has low power to test heterogeneity when the number of studies is small, pooled prevalence of PAH in lupus based on both fixed-effect and random-effect models were calculated. The pooled prevalence estimate of PAH in patients with lupus was 3.34 % (95 % CI, 2.10%to 4.86 %) based on random-effects model and was 3.24 % (95 % CI, 2.26 % to 4.38 %) based on a fixed-effect model (Fig. 3)
Rheumatoid arthritis
Two studies reported prevalence of PAH in patients with rheumatoid arthritis ranging from 21 % to 27.5 %. An I 2statistic could not be obtained since only two studies were included. Both fixed-effect and random-effect models were used. Pooled prevalence of PAH in patients with arthritis rheumatoid was 22.3 % (95 % CI, 16.63 % to 28.48 %) based on both fixed-effect and random-effect models (Fig. 3). No bias indicators were available due to having only two studies. In both studies, PAH diagnosis was based on echocardiography. One study reported PAH prevalence in a patient group with systemic sclerosis and mixed connective tissue disease in which some diagnoses were confirmed with catheterization and some were not, at 26.7 % [35].
Subgroup analysis by whether right heart catheterization was used for diagnosis
Among studies reporting prevalence of PAH in patients with connective tissue diseases, only the studies focusing on systemic sclerosis populations included a mix of studies that used right heart catheterization to confirm diagnosis and studies that only used echocardiograph for PAH diagnosis. That mix of studies allowed subgroup analysis of prevalence of PAH by whether right heart catheterization was used to confirm diagnosis of PAH. Five out of 12 studies reporting prevalence of PAH in systemic sclerosis were based on data with diagnosis confirmed by right heart catheterization [19–23], and seven were based on data from PAH patients diagnosed by echocardiography [24–30].
Based on the I 2 statistic, 92 % (95 % CI, 84.4 % to 95 %), the random-effects model was used for proportion meta-analysis, for estimates of prevalence of PAH among persons with systemic sclerosis with PAH diagnosis confirmed by right heart catheterization (Table 2). The pooled prevalence estimate of PAH diagnosed by right heart catheterization in patients with systemic sclerosis was 8.2 % (95 % CI, 5.2 % to 11.8 %) (Fig. 4). The Harbord test suggested that there was no bias across studies in prevalence of PAH diagnosed by right heart catheterization in patients with systemic sclerosis (Table 2).
Fig. 4.
Proportion meta-analysis of prevalence of PAH by whether diagnosed by right heart catheterization or echocardiograph in patients with systemic sclerosis
Based on the I 2 statistic, 79.6 % (95 % CI: 50.9 % to 88.5 %) (Table 2), a random-effects model was used to estimate the prevalence of PAH diagnosed by echocardiography without catheterization confirmation in patients with systemic sclerosis. The pooled prevalence estimate of PAH diagnosed without catheterization among persons with systemic sclerosis was 18 % (95 % CI, 14 % to 23 %) (Fig. 4). The Harbord test suggested that there was no bias across selected studies estimating prevalence of PAH diagnosed by echocardiography in patients with systemic sclerosis in meta-analysis (Table 2). This higher prevalence estimate (18 %) among studies in systemic sclerosis populations that did not use heart catheterization for PAH diagnosis confirmation as compared with those that did confirm diagnosis with catheterization (8.2 %) likely reflects a tendency for inflation of prevalence estimates when catheterization diagnosis confirmation was not used.
Discussion
The estimate of idiopathic pulmonary arterial hypertension prevalence was 12 cases per million population (95 % CI, five cases per million population to 22 cases per million population), and the estimate of PAH prevalence in patients with connective tissue diseases was 13 % (95 % CI, 9.18 % to 18.16 %) in meta-analysis. These findings confirm that the prevalence of PAH in patients with connective tissue diseases appears much higher than the prevalence of idiopathic pulmonary arterial hypertension.
Current published PAH prevalence studies in patients with connective tissue diseases used inconsistent criteria for identifying PAH. With better understanding of the disease, there have been a series of changes in definition of PAH [37–39]. A resting mean pulmonary arterial pressure greater than or equal to 25 mm Hg and a pulmonary capillary wedge pressure less than 15 mm Hg [38] were proposed at the Fourth World Symposium on Pulmonary Hypertension in 2008. Some definitions also include pulmonary vascular resistance greater than 2 or 3 mm Hg/l/min [15, 38, 40]. The use of various definitions of PAH for diagnosis of PAH impairs comparisons among studies reporting prevalence.
Echocardiography is used to screen for PAH, but right heart catheterization is the gold standard to confirm diagnosis of PAH [40]. Prior studies have shown that discordance exists between estimation of pulmonary hemodynamics in echocardiography and estimation directly by invasive catheterization techniques [15]. PAH diagnosis based on echocardiography does not have the specificity of diagnosis by catheterization [16] and may inflate estimates of the prevalence of PAH.
For studies in systemic sclerosis, when right heart catheterization was not used to confirm PAH diagnosis, the PAH prevalence estimate was 18 % (95 % CI, 14 % to 23 %). When right heart catheterization was used, PAH prevalence estimate in systemic sclerosis was 8.2 % (95 % CI, 5.2 % to 11.8 %). The higher prevalence estimates when only echocardiography was used is consistent with prior evidence that PAH diagnosis by echocardiography may inflate PAH prevalence estimate [16].
Two registry studies focusing on patients with PAH associated with connective tissue diseases were found in the literature search. Condliffe et al. reported prevalence of PAH associated with connective tissue diseases in a UK population, on June 31, 2006, of 4.23 per million or 0.000423 % [41]. Chung et al. reported percentages of patients with PAH associated with systemic sclerosis, lupus, mixed CTD, and rheumatoid arthritis among all known PAH–CTD patients, respectively [42]. However, the focus of our analysis was to estimate PAH prevalence in CTD populations.
In studies in which PAH prevalence was estimated in patients with rheumatoid arthritis or in patients with systemic lupus erythematosus, PAH was not confirmed by right heart catheterization among all patients. Therefore, the estimates of PAH prevalence in patients with rheumatoid arthritis or in patients with systemic lupus erythematosus may be inflated and questionable.
Wigley and colleagues [35] estimated PAH prevalence of 26.7 % among patients with systemic sclerosis or mixed connective tissue disease in community-based rheumatology practices. Since less severe cases may be more likely to be seen in such setting as compared with tertiary centers, lack of confirmation of PAH diagnosis by right heart catheterization for many of the patients in their study may have been particularly likely to inflate the PAH prevalence estimate such that the estimate may be questionable.
Limitations
A limitation in the current study was that not all of the selected studies defined PAH using the definition of a mean pulmonary arterial pressure greater than 25 mm Hg and pulmonary capillary wedge pressure less than 15 mm Hg. Most of the studies did not require pulmonary capillary wedge pressure less than 15 mm Hg, and most selected studies did not use right heart catheterization to confirm diagnosis of PAH.
Conclusions
Prevalence of PAH in patients with connective tissue diseases was substantially higher than that of idiopathic pulmonary arterial hypertension based on pooled prevalence estimates. Comparisons of PAH prevalence in persons with connective tissue disease and idiopathic pulmonary arterial hypertension using a large observational study would be helpful in better assessing relative prevalence. Nevertheless, the current finding underscores the need for monitoring for PAH in patients with connective tissue disease.
Acknowledgments
Acknowledgment
Funding for this research was provided by Pfizer, Inc., New York, NY.
Conflict of interest
Xiaoqin Yang and Joseph Thomas III are employees of Purdue University. Xiaoqin Yang was also a paid consultant to Pfizer, Inc. Jack Mardekian, Kafi N. Sanders, and Marko A. Mychaskiw are employees of Pfizer, Inc.
Joseph Thomas III and Xiaoqin Yang are employees of Purdue University who were paid consultants to Pfizer, Inc. in connection with the development of this manuscript.
Contributor Information
Xiaoqin Yang, Email: yang30@purdue.edu.
Jack Mardekian, Email: Jack.Mardekian@Pfizer.com.
Kafi N. Sanders, Email: Kafi.Sanders@pfizer.com
Marko A. Mychaskiw, Email: Marko.Mychaskiw@pfizer.com
Joseph Thomas, III, Phone: +1-765-4941477, FAX: +1-765-4961886, Email: jt3@purdue.edu.
References
- 1.McLaughlin VV, ACCF/AHA et al. Expert consensus document on pulmonary hypertension a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association developed in collaboration with the American College of Chest Physicians; American Thoracic Society, Inc.; and the Pulmonary Hypertension Association. J Am Coll Cardiol. 2009;53(17):1573–1619. doi: 10.1016/j.jacc.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 2.Gaine SP, Rubin LJ. Primary pulmonary hypertension. Lancet. 1998;352(9129):719–725. doi: 10.1016/S0140-6736(98)02111-4. [DOI] [PubMed] [Google Scholar]
- 3.Baughman RP, Carbone, RG, Bottino G (2009) Pulmonary arterial hypertension and interstitial lung diseases: a clinical guide. R.G.C. Robert P. Baughman, Giovanni Bottino (ed) Humana Press: New York, NY
- 4.Kimberly (2001) Primer on the rheumatic diseases. J.H. Klippel (ed) Arthritis Foundation: Atlanta, GA. p. 325–8
- 5.Trell E, Lindstrom C. Pulmonary hypertension in systemic sclerosis. Ann Rheum Dis. 1971;30(4):390–400. doi: 10.1136/ard.30.4.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perez HD, Kramer N. Pulmonary hypertension in systemic lupus erythematosus: report of four cases and review of the literature. Semin Arthritis Rheum. 1981;11(1):177–181. doi: 10.1016/0049-0172(81)90098-6. [DOI] [PubMed] [Google Scholar]
- 7.Sullivan WD, et al. A prospective evaluation emphasizing pulmonary involvement in patients with mixed connective tissue disease. Med (Baltimore) 1984;63(2):92–107. doi: 10.1097/00005792-198403000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Wiener-Kronish JP, et al. Severe pulmonary involvement in mixed connective tissue disease. Am Rev Respir Dis. 1981;124(4):499–503. doi: 10.1164/arrd.1981.124.4.499. [DOI] [PubMed] [Google Scholar]
- 9.Galie N, et al. Pulmonary arterial hypertension associated to connective tissue diseases. Lupus. 2005;14(9):713–717. doi: 10.1191/0961203305lu2206oa. [DOI] [PubMed] [Google Scholar]
- 10.Peacock AJ, et al. An epidemiological study of pulmonary arterial hypertension. Eur Respir J. 2007;30(1):104–109. doi: 10.1183/09031936.00092306. [DOI] [PubMed] [Google Scholar]
- 11.Humbert M, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Respir Crit Care Med. 2006;173(9):1023–1030. doi: 10.1164/rccm.200510-1668OC. [DOI] [PubMed] [Google Scholar]
- 12.Tueller C, et al. Epidemiology of pulmonary hypertension: new data from the Swiss registry. Swiss Med Wkly. 2008;138(25–26):379–384. doi: 10.4414/smw.2008.11915. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JPT, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539-1558 [DOI] [PubMed]
- 14.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 15.McGoon M, et al. Screening, early detection, and diagnosis of pulmonary arterial hypertension: ACCP evidence-based clinical practice guidelines. Chest. 2004;126(1 Suppl):14S–34S. doi: 10.1378/chest.126.1_suppl.14S. [DOI] [PubMed] [Google Scholar]
- 16.Denton CP, et al. Comparison of Doppler echocardiography and right heart catheterization to assess pulmonary hypertension in systemic sclerosis. Br J Rheumatol. 1997;36(2):239–243. doi: 10.1093/rheumatology/36.2.239. [DOI] [PubMed] [Google Scholar]
- 17.Humbert M, et al. Screening for pulmonary arterial hypertension in patients with systemic sclerosis: clinical characteristics at diagnosis and long-term survival. Arthritis Rheum. 2011;63(11):3522–3530. doi: 10.1002/art.30541. [DOI] [PubMed] [Google Scholar]
- 18.Meune C, et al. Prediction of pulmonary hypertension related to systemic sclerosis by an index based on simple clinical observations. Arthritis Rheum. 2011;63(9):2790–2796. doi: 10.1002/art.30432. [DOI] [PubMed] [Google Scholar]
- 19.Hachulla E, et al. Early detection of pulmonary arterial hypertension in systemic sclerosis: a French nationwide prospective multicenter study. Arthritis Rheum. 2005;52(12):3792–3800. doi: 10.1002/art.21433. [DOI] [PubMed] [Google Scholar]
- 20.Hachulla E, et al. Risk factors for death and the 3-year survival of patients with systemic sclerosis: the French ItinerAIR-Sclerodermie study. Rheumatology (Oxford) 2009;48(3):304–308. doi: 10.1093/rheumatology/ken488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Avouac J, et al. Prevalence of pulmonary hypertension in systemic sclerosis in European Caucasians and metaanalysis of 5 studies. J Rheumatol. 2010;37(11):2290–2298. doi: 10.3899/jrheum.100245. [DOI] [PubMed] [Google Scholar]
- 22.Vonk MC, et al. Systemic sclerosis and its pulmonary complications in The Netherlands: an epidemiological study. Ann Rheum Dis. 2009;68(6):961–965. doi: 10.1136/ard.2008.091710. [DOI] [PubMed] [Google Scholar]
- 23.Phung S, et al. Prevalence of pulmonary arterial hypertension in an Australian scleroderma population: screening allows for earlier diagnosis. Int Med J. 2009;39(10):682–691. doi: 10.1111/j.1445-5994.2008.01823.x. [DOI] [PubMed] [Google Scholar]
- 24.de Azevedo AB, et al. Prevalence of pulmonary hypertension in systemic sclerosis. Clin Exp Rheumatol. 2005;23(4):447–454. [PubMed] [Google Scholar]
- 25.Coral-Alvarado P, et al. Risk factors associated with pulmonary arterial hypertension in Colombian patients with systemic sclerosis: review of the literature. J Rheumatol. 2008;35(2):244–250. [PubMed] [Google Scholar]
- 26.Kumar U, et al. Prevalence and predictors of pulmonary artery hypertension in systemic sclerosis. J Assoc Phys India. 2008;56:413–417. [PubMed] [Google Scholar]
- 27.Pope JE, et al. Prevalence of elevated pulmonary arterial pressures measured by echocardiography in a multicenter study of patients with systemic sclerosis. J Rheumatol. 2005;32(7):1273–1278. [PubMed] [Google Scholar]
- 28.Gindzienska-Sieskiewicz E, et al. The occurrence of pulmonary hypertension in patients with systemic sclerosis hospitalized in the Department of Rheumatology and Internal Diseases Medical University of Bialystok in years 2003–2004. Rocz Akad Med Bialymst. 2005;50(Suppl 1):297–300. [PubMed] [Google Scholar]
- 29.Chang B, et al. Scleroderma patients with combined pulmonary hypertension and interstitial lung disease. J Rheumatol. 2003;30(11):2398–2405. [PubMed] [Google Scholar]
- 30.Yamane K, et al. Clinical and laboratory features of scleroderma patients with pulmonary hypertension. Rheumatology (Oxford) 2000;39(11):1269–1271. doi: 10.1093/rheumatology/39.11.1269. [DOI] [PubMed] [Google Scholar]
- 31.Pan TL, Thumboo J, Boey ML. Primary and secondary pulmonary hypertension in systemic lupus erythematosus. Lupus. 2000;9(5):338–342. doi: 10.1191/096120300678828361. [DOI] [PubMed] [Google Scholar]
- 32.Prabu A, et al. Prevalence and risk factors for pulmonary arterial hypertension in patients with lupus. Rheumatology (Oxford) 2009;48(12):1506–1511. doi: 10.1093/rheumatology/kep203. [DOI] [PubMed] [Google Scholar]
- 33.Dawson JK, et al. Raised pulmonary artery pressures measured with Doppler echocardiography in rheumatoid arthritis patients. Rheumatology (Oxford) 2000;39(12):1320–1325. doi: 10.1093/rheumatology/39.12.1320. [DOI] [PubMed] [Google Scholar]
- 34.Keser G, et al. Pulmonary hypertension in rheumatoid arthritis. Scand J Rheumatol. 2004;33(4):244–245. doi: 10.1080/03009740410005809. [DOI] [PubMed] [Google Scholar]
- 35.Wigley FM, et al. The prevalence of undiagnosed pulmonary arterial hypertension in subjects with connective tissue disease at the secondary health care level of community-based rheumatologists (the UNCOVER study) Arthritis & Rheumatism. 2005;52(7):2125–2132. doi: 10.1002/art.21131. [DOI] [PubMed] [Google Scholar]
- 36.Gavaghan DJ, Moore RA, McQuay HJ. An evaluation of homogeneity tests in meta-analyses in pain using simulations of individual patient data. Pain. 2000;85(3):415–424. doi: 10.1016/S0304-3959(99)00302-4. [DOI] [PubMed] [Google Scholar]
- 37.Hatano S, Strasser T, WH Organization (1975) Primary pulmonary hypertension: report on a WHO meeting: World Health Organization, Geneva
- 38.Badesch DB, et al. Diagnosis and assessment of pulmonary arterial hypertension. J Am Coll Cardiol. 2009;54(1 Suppl):S55–S66. doi: 10.1016/j.jacc.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 39.Kovacs G, et al. Pulmonary arterial pressure during rest and exercise in healthy subjects: a systematic review. Eur Respir J. 2009;34(4):888–894. doi: 10.1183/09031936.00145608. [DOI] [PubMed] [Google Scholar]
- 40.Galie N, et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension. The Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology. Eur Heart J. 2004;25(24):2243–2278. doi: 10.1016/j.ehj.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 41.Condliffe R, et al. Connective tissue disease-associated pulmonary arterial hypertension in the modern treatment era. Am J Respir Crit Care Med. 2009;179(2):151–157. doi: 10.1164/rccm.200806-953OC. [DOI] [PubMed] [Google Scholar]
- 42.Chung L, et al. Characterization of connective tissue disease-associated pulmonary arterial hypertension from REVEAL: identifying systemic sclerosis as a unique phenotype. Chest. 2010;138(6):1383–1394. doi: 10.1378/chest.10-0260. [DOI] [PMC free article] [PubMed] [Google Scholar]