Abstract
Introduction and Aims:
Diabetes is one of the chronic and prevalent diseases in the world. Diabetic patients’ number has increased 7 times during last 20 years. If this current situation continues, diabetic patients’ population will be 350 millions ones in 2030. It means that 7 millions people will be added annually. Up to now, different uncontrollable factors have been monitored in self-caring of this disease for managing and preventing from its early and late side effects. This research is conducted to study the role of self-efficacy as a determinant agent in self-caring of diabetic patients.
Study Method:
This is a narrative review study in which various information banks and search motors such as PubMed, ProQuest, SCOPUS, Elsevier were reviewed. Diabetes, self-care and self efficacy keywords from cross sectional, cohort, clinical experimental studies and systematic review were also used in the study construction. Iranian Banks such as IRANMEDEX, MEDLINE and also different articles from domestic research and scientific magazines were selected. Time spectrum of reviewed studies was supposed to be published from 1990 up to 2011.
Results:
Self-care situation among diabetic patients not only is unsatisfactory but also the studies’ results show that self-efficacy rate is low among them. The findings of the studies prove that there is a direct relation between self-efficacy and self-care in the patients in a way that this construct owns the predictability power of self-care behavior.
Conclusion:
Self-caring has a significant role in controlling of diabetes disease. Self-efficacy can induce motivation directly take health promoting behavior through efficacy expectations. It also affects motivation, indirectly, through perceived barriers and determining commitment or stability for following function map. So, self-efficacy is very important in changing self-care behavior process.
Keywords: Diabetes, self-care, self-efficacy
INTRODUCTION
Today, the process of diseases and mortality has been transformed in the world and communicable diseases have been replaced with and non-communicable diseases. They in many developed and developing countries remain the number one killer. Mortality resulted from these diseases exceeds in Asian countries up to 2-5 times more than other diseases.[1]
Iran as one of developing countries have recently faced with this epidemy. Diabetes is one of these global problems that strictly affect people in the world. Based on the 2004 data, 194 million diabetic patients lived in the world. Estimations of World Health Organization (WHO) indicate this will increase in 2025 to about 333 million people.[2] Studies in Iran show that approximately 7.7% or 2 million adults age between 25-64 years will suffer from diabetes.[3]
Doubtless by increasing life expectancy in Iran, diabetes side effects prevalence increases as well. This and increase of diabetes incidence has changed it to one of main country's health worries within next decades.[3] In fact, increase of diabetes prevalence is for inefficient control of diabetes.
No main treatment at present has been identified though it can be managed. An important fact for health care providers to keep in mind is that the non pharmacological treatment strategies are equally, if not more, important than the pharmacological treatment options available.[4]
Diabetes self-management education (DSME) is the cornerstone in the treatment of diabetes. Knowledge is power, and the more patients know about diabetes and how they can self-manage or control their disease, the better their chances are of minimizing and preventing complications.[5] The ultimate goal of DSME is to empower the patient to be the responsible party in the management of the disease.[6,7]
Although, self-care practices of individuals are influenced by a complex interaction of biological and psychosocial factors, dietary intake, medication use, physical activity and self monitoring of blood glucose (SMBG) are the four main cornerstones of overall diabetes management.[8,9]
Self-care in diabetes is crucial. It has been claimed that as much as 98% of diabetes care is self-care.[10]
Self-care in diabetes falls mostly on the patients and their families (Anderson 1995, Jacobson 1996). It is essential that the individuals with diabetes adhere to self-care, to prevent the complications associated with diabetes (such as retinopathy, nephropathy, neuropathy and cardiovascular disease) (DCCT 1993), to maintain or achieve a good quality of life and, moreover, to achieve subjective well-being and a sense of control over diabetes.[11]
Self-care activities may seem to be more troubling and often involves basic changes in life style in a way that in spite of side effect of disease, many patients partially ignore physicians and consequently diabetes side effects increase. However, Heisler[12], Rubbin[13] and Mahmoudi[14] indicate that positive effect of self-care on glucose and HbA1c control.
Parchman showed that diabetic patients having continuous self-care, had lower Alc hemoglobin.[15] Walston KA,[16] Kitis[17] and Schiling[18] results indicate that low glucose in self-care persons are more appropriate. However, different findings show that self-care condition in diabetic patients is inappropriate.[19,20,21]
Similar condition can be observed in Mahmoudi and Daily studies.[22,23,24] In an study, Jahanlou found that only 27% of diabetes patients follow self-care food behaviors.[25] Jafarian and Shakibazadeh showed that self-care in diabetes patients is inappropriate.[21,26]
Active participation and taking responsibility is the main principle in self-care to control the impact of illness.[27] Although, in general self-care behaviors do not lead to suitable metabolic control, and ignorance causes weakness in patient's metabolic condition.[28]
A few of several factors influence on self-care behaviors whether directly or indirectly that involve biological, psychological, economic, socio-cultural and medical care systems of the community.[29]
Some studies also have measured the role of demographical factor such as age on self-care.[30,31] And some others have assessed socio-economic factors like low education level[32,33], low income[32,34] social factors like low personal and family quality[30] in diabetes self-management and self-care. However, knowledge and attitude role has been assessed in self-care behaviors, other personal factors seem to be necessary.
Some scholars believe that knowledge increase in diabetes patients alone can not be sufficient enough in initiation and self-care behaviors and assured they are long lasting.[35,36] In other words, knowledge, attitude and performance hold no direct and simple relationship in relation to self-care.[37,38,39]
Today, evidences show that one of effective factors in self-care of chronic patients, especially diabetes, is self-efficacy. Self-efficacy is the pre-requisite of this behavior, since acts as the independent part of basic personal skills. Of course, it can be said that self-efficacy role in initiation and maintenance of medical behaviors have been confirmed by several investigations in other subjects.[40,41]
Self efficacy is defined as “people's judgment of their capabilities to organize and execute courses of action required to attain designed types of performance and expect the outcomes. It is a pre-requisite of behavior, since is considered as an independent part of basic personal skills. Self-efficacy is an important concept derived from Social Cognitive theory that refers to people's beliefs and judgments on for executing the duties and responsibilities. The theorists believe that humans possess a self-management system through which control their own thoughts, emotion and behaviors and thus significantly determine their own destiny.[40] Therefore, this study attempts to explain the self-efficacy role in self-care of diabetes patients.
MATERIALS AND METHODS
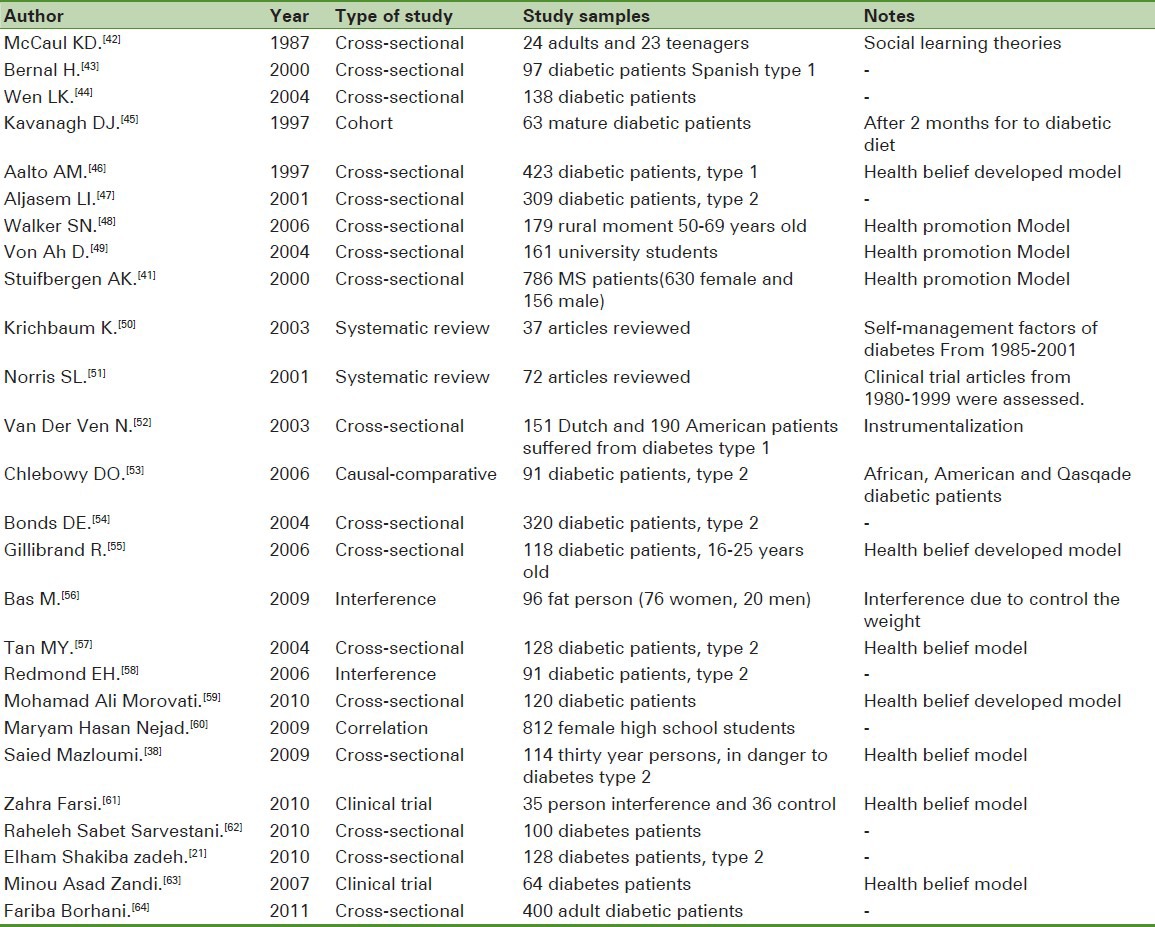
It is a type of review study that data were collected through data bases and search PubMed ‘ProQuest’ SCOPUS engine such as Elsevier and key words of self-efficacy, diabetes, and self-care and cross-sectional, Cohort, clinical trial and systematic review of related articles. Persin language articles were selected by use of data bases such as MEDLIB and IRANMeDEX. The time span for articles was from 1990 to late 2011. Studied articles related to self-efficacy are summarized in Table 1.
Table 1.
Review of related articles
RESULTS
The findings of previous studies show that self-efficacy in diabetes patients is unsuitable. Bernal's study indicates that self-efficacy is average to weak level.[43] Domestic studies show that self-efficacy in diabetes patients is inappropriate as well. Keshavarzi showed that target group had no appropriate self-efficacy to receive healthy nutrition.[65] Some studies like Charron –Prochonwink though showed that self-efficacy of young girls is in reasonable level.[66]
Many findings indicate that self-efficacy influences self-care behaviors. Few studies found no relationship between these two variables. McCaul, et al. investigated diabetes diets behaviors found a positive meaningful correlation between self-efficacy and food self-care behaviors.[42] Bernal,[43] Wen[44] and Kavanagh[45] also indicate that self-efficacy directly relate to self-care. In the regression analysis some variables in Aalto's study[46] self-efficacy had highest relationship with glucose self-care.
In another study, Aljasem studied about the obstacles and self-efficacy of self-care behaviors in diabetes type 2, 4-10% of self-care variance is explained by self-efficacy. It was strongly predicted by it.[47] These results and Walker's result were in a good accordance.[48] Bernal investigated about the correlation of self-efficacy in diabetes self-care of Spanish adults. The result shows that self-efficacy had a relationship with self-care in food and insulin use.[43]
Wen investigated about the family support, diet and physical exercises among Mexican-American people suffering from diabetes type 2, he found that increase in self-efficacy lead to more healthier diet.[44]
Stuifbergen, et al. also found that increase of self-efficacy related to the hygienic behaviors cause the improvement and development of these behaviors.[41]
Krichbaum[50] and Norris[51] indicated that self-efficacy had a significantly positive impact on hygienic behaviors of diabetes patients.
In a study, Bonds, et al.[54] reached a significantly direct relationship between personal self-efficacy and self-care. Walker and Woon's[49] study also indicate the predictive role of self-efficacy on nutrition behaviors based on regression analysis. Tan showed a principally direct relationship between self-efficacy and predictive behaviors in Chinese type 2 diabetic people.[57] Bas study confirmed the self-efficacy role in weight control.[56] Remond has stated similar findings as well.[58]
Few domestic studies have also shown similar results. According to Morovati study, self-efficacy, intensity and perceived sensitivity have considerably been influential on self-efficacy behaviors. It is a strong effect and predicts 38 % of self-efficacy behaviors variance.[59] Hossien Nejad study indicate that a considerable relationship exist between nutrition behaviors mean score and self-efficacy based on bivariable regression.[60]
In his study, Mazloumi found a strong correlation between self-efficacy and predictive behaviors form diabetes type 2.[38] Shakiba zadeh indicate that self-efficacy directly relates to self-care and 51% of self-care changes explained by self-efficacy and obstacles.[21] Unlike previous studies results, Gillibrand[55] and Chlebowy[53] found no meaningful relationship between self-efficacy and glycemic control.
DISCUSSION
As mentioned, some of studies have showed that knowledge plays a vital role in appropriate control of glucose.[67,68,69] Though, a number of investigators expressed that knowledge alone can not lead to increase in self-care.[70]
Knight, et al. states that knowledge and behavior have a quantitative relation and knowledge is necessary for behavior and behavioral changes but not sufficient.[71]
Perhaps, cliché interference repetition and lack of attention to behavioral changes and absolute care to knowledge is an important factor in achievement of interferences.[72] Therefore, it is demanding for medical care providers to know the predictive factors of self-care behaviors in diabetic patients. On the other hand, today, increase in patients trust to their abilities in diabetes care, is a vital factor in active self-management.[73,74]
This study refers to self-efficacy construct in self-care behavior. It shows that self-efficacy provides a suitable framework for understanding and predicting commitment towards self-care behaviors and effectiveness of self-management in diabetes treatment.[74,75,76,77] Problems faced with changes in life style like nutritious habits, smoking, and exercise requires a high level of self-confidence and achieving to self-efficacy is more difficult.[78]
Based on Bandora, self-efficacy is the strongest construct in predicting behavior change in person and usually those show highest behavior change hold higher self-efficacy to act a certain behavior.[78] Self-efficacy affects person's motivation and pushes it to try and continue the behavior. Self-efficacy defined as the person's trust to its abilities for exploring a behavior. In other words, self-efficacy consists of the people's trust to themselves in executing a special act. Self-efficacy feeling is a pre-requisite to behavior change. This factor influences the trial and performance level.[79]
In fact, self-efficacy enables people to use skills in dealing with obstacles and creates fabulous acts. Therefore, self-efficacy is a vital factor in executing successful performance and human skills necessary for doing it. Efficient performance needs either skill or judgment in ability to execute those skills. On the other hand, self-efficacy affects level of attempt in doing a function. People who believe in their self-efficacy double try to resolve obstacles and problems.[80,81]
Self-efficacy refers to people's judgment in relation to their abilities in doing works and inspired by different sources such as achievements, failures, and others success or loss and verbal encourage. Those persons, who possess higher personal self-efficacy, have more perseverance, are luckier and experience less fear.[82,83]
To develop people's belief to their ability self-efficacy due to diabetes care behaviors, their inner control source can be improved.
To reach it, they have to receive trainings in order to plan the diabetes cares due to control their disease and be their main factor in preventing diabetes side effects.
Investigators have stated the following factors in creation of personal self-efficacy:
Primary judgment that a certain work or duty is possible to happen.
This duty or plan (if complicated), is divided into smaller and easier sub-plans. This situation indeed, leads to experience of small achievement feeling in process of learning in person.
Repetition exists in action and behavior to be carried out.
In doing a special behavior, reward, reinforcement, recognition and understanding present.
Except the first factor, others can be controlled and supervised by medical staff. In fact, the instructors easily establish these factors in their training interferences. To reinforce the patient assumption of being practical, the similar behaviors cab be executed by patients highlighted or present evidence in performance of that special behavior by other patients. In regard to second factor, establishment of self-efficacy through behavior division into smaller behaviors or concept to sub-concepts, more emphasis has been put on feedback or reinforcement in the patient in each stage. It certainly depends on the patient's knowledge, skills and experience.
The third factor, is repetition and leads to creation of self-skill and consequently self-efficacy in person, is possible to be used by medical staff. Last but not the least factor, recognition, reward and reinforcement for doing each small behavior can establish self-confidence and self-esteem. This factor is important in low educated patients. Indeed, a reward or honest friendly statement from medical staff may be helpful.[80,84] Studied articles related to self-efficacy are summarized in Table 1.
CONCLUSION
In the process of chronic diseases, self-efficacy is vital and it is expected that diabetic patients control 95% of their own disease personally. A significant part of caring these patients is at home and self-efficacy here plays a vital role. Self-efficacy directly through efficacy expectations causes motivation for health developing behavior. It also indirectly via perceived obstacles and determination of commitment level or patience in following performance-map, influences motivation.
Self-efficacy indeed is people's judgment and expectation in influencing ability on favorite incidence thorough personal trials. In other words, self-efficacy affects motivation. More powerful judgment, more active the person is and do the best in trial and following a behavior to achieve a goal. Therefore, a low self-efficacy person, less possibly tries to change a habit a fixed behavior. According to the studies, since self-efficacy affects performance and behavior, this feeling can be determinant in people's success in self-care of diabetic patients, especially in nutritious behaviors. Therefore, in the process of self-care process in diabetic patients, self-efficacy is crucial.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Vongpatanasin W. Cardiovascular morbidity and mortality in high-risk populations: Epidemiology and opportunities for risk reduction. J Clin Hypertens (Greenwich) 2007;9:11–5. doi: 10.1111/j.1524-6175.2007.07722.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.International Diabetes Foundation. The International Diabetes Federation welcomes adoption of WHO global strategy on diet, physical activity and health. 2009. Available from http://www.idf.org/home/index.cfm .
- 3.Esteghamati A, Gouya MM, Abbasi M, Delavari A, Alikhani S, Alaedini F, et al. Prevalence of diabetes and impaired fasting glucose in the adult population of Iran: National Survey of Risk Factors for Non Communicable Diseases of Iran. Diabetes Care. 2008;31:96–8. doi: 10.2337/dc07-0959. [DOI] [PubMed] [Google Scholar]
- 4.Cornell S, Briggs A. Newer Treatment Strategies for the Management of Type 2 Diabetes Mellitus. J Pharm Pract. 2004;17:49–54. [Google Scholar]
- 5.Cumbie SA, Conley VM, Burman ME. Advanced practice nursing model for comprehensive care with chronic illness: Model for promoting process engagement. ANS Adv Nurs Sci. 2004;27:70–80. doi: 10.1097/00012272-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Allison SE. Self care requirements for activity and rest: An Orem nursing focus. Nurs Sci Q. 2007;20:68–76. doi: 10.1177/0894318406296297. [DOI] [PubMed] [Google Scholar]
- 7.Nelson KM, McFarland L, Reiber G. Factors influencing disease self-management among veterans with diabetes and poor glycemic control. J Gen Intern Med. 2007;22:442–7. doi: 10.1007/s11606-006-0053-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tan MY, Magarey J. Self care practices of Malaysian adults with diabetes and sub-optimal glycaemic control. Patient Educ Couns. 2008;72:252–67. doi: 10.1016/j.pec.2008.03.017. [DOI] [PubMed] [Google Scholar]
- 9.Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A, et al. Nutrition principles and recommendations in diabetes. Diabetes Care. 2004;27:S36–46. doi: 10.2337/diacare.27.2007.s36. [DOI] [PubMed] [Google Scholar]
- 10.Jordan DN, Jordan JL. Self-care behavior of Filipino-American adults with type 2 diabetes mellitus. J Diabetes Complication. 2010;24:250–8. doi: 10.1016/j.jdiacomp.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 11.Toljamo M, Hentinen M. Adherence to self-care and glycemic control among people with insulin-dependent diabetes mellitus. J Adv Nurs. 2001;34:780–6. doi: 10.1046/j.1365-2648.2001.01808.x. [DOI] [PubMed] [Google Scholar]
- 12.Heisler M, Smith DM, Hayward RA, Krein SL, Kerr EA. How well do patients assessments of their diabetes self management correlate with actual glycemic control and receipt of recommended diabetes services? Diabetes Care. 2003;26:738–43. doi: 10.2337/diacare.26.3.738. [DOI] [PubMed] [Google Scholar]
- 13.Rubin RR, Peyrot M, Saudek CD. Differetial effect of diabetes education on self-regulation and life stage behaviors. Diabetes Care. 1998;14:335–8. doi: 10.2337/diacare.14.4.335. [DOI] [PubMed] [Google Scholar]
- 14.Mahmoodi A. Effects of self care planning on reduction of A1C hemoglobin in adults with diabetes mellitus. Medical Science Journal of Islamic Azad University. 2006;16:171–6. [Google Scholar]
- 15.Parchman ML, Pugh JA, Noël PH, Larme AC. Continuity of care, self management behaviors and glucose control in patients with type 2 diabetes. Med Care. 2002;40:137–44. doi: 10.1097/00005650-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Wallston KA, Rothman RL, Cherrington A. Psychometric properties of perceived diabetes self-management scale (PDSMS) J Behav Med. 2007;30:395–401. doi: 10.1007/s10865-007-9110-y. [DOI] [PubMed] [Google Scholar]
- 17.Kitis Y, Emiroglu ON. The effects of home monitoring by public health nurse on individuals diabetes control. Appl Nurs Res. 2006;19:134–43. doi: 10.1016/j.apnr.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 18.Schilling LS, Dixon JK, Knafl KA, Lynn MR, Murphy K, Dumser S, et al. A new self-report measure of self-management of type 1 diabetes for adolescents. Nurs Res. 2009;58:228–36. doi: 10.1097/NNR.0b013e3181ac142a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morowati Sharifabad M, Rouhani Tonekaboni N. Social support and Self-care Behaviors in Diabetic Patients Referring to Yazd Diabetes Research Center. ZJRMS. 2008;9:275–84. [Google Scholar]
- 20.Morowatisharifabad MA, Rouhani Tonekaboni N. The Relationship between Perceived Benefits/Barriers of Self-care Behaviors and Self Management in Diabetic Patients. JFNM. 2007;13:17–27. [Google Scholar]
- 21.Shakibazadeh E, Rashidian A, Larijani B, Shojaeezadeh D, Forouzanfar MH, Karimi Shahanjarini A. Perceived Barriers and Self-efficacy: Impact on Self-care Behaviors in Adults with Type 2 Diabetes. JFNM. 2010;15:69–78. [Google Scholar]
- 22.Dailey George. A timely transition to insulin: Identifying type 2 diabetes patients failing oral therapy. Formulary. 2005;40:114–30. [Google Scholar]
- 23.Dailey G. Fine-Tuning therapy with basal insulin for optimal glicemic control diabetes: A review. Curr Med Res Opin. 2004;20:2007–14. doi: 10.1185/174234304X15183. [DOI] [PubMed] [Google Scholar]
- 24.Mahmood K, Aamir AH. Glycemic control status in patients with type 2 diabetes. J Coll Physicians Surg Pak. 2005;15:323–25. [PubMed] [Google Scholar]
- 25.Shahab Jahanlo AR, GHofrani Poor FA, Vafaie M, Kimiyagar M, Heidarnia AR, Sobhani AR. Structures measuring health belief model with HbA1c in diabetic patients with good control and poor. JHUMS. 2008;12:37–42. [Google Scholar]
- 26.Jafarian Amiri SR, Zabihi A, Babaieasl F, Eshkevari N, Bijani A. Self Care Behaviors in Diabetic Patients Referring to Diabetes Clinics in Babol City, Iran. JBUMS. 2010;12:72–8. [Google Scholar]
- 27.Schreurs KM, Colland VT, Kuijer RG, de Ridder DT, van Elderen T. Development, content, and process evaluation of a short self-management intervention in patients with chronic diseases requiring self-care behaviors. Patient Educ Couns. 2003;51:133–41. doi: 10.1016/s0738-3991(02)00197-0. [DOI] [PubMed] [Google Scholar]
- 28.Park H, Hong YS, Lee H, Ha E, Sung Y. Individuals with type 2 diabetes and depressive symptoms exhibited low adherence with self-care. J Clin Epidemiol. 2004;57:978–84. doi: 10.1016/j.jclinepi.2004.01.015. [DOI] [PubMed] [Google Scholar]
- 29.Bell RA, Arcury TA, Snively BM, Smith SL, Stafford JM, Dohanish R, et al. Diabetes foot self-care practices in a rural triethnic population. Diabetes Educ. 2005;31:75–83. doi: 10.1177/0145721704272859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alberti H, Boudriga N, Nabli M. Factors affecting the quality of diabetes care in primary health care centres in Tunis. Diabetes Res Clin Pract. 2005;68:237–43. doi: 10.1016/j.diabres.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 31.Adams AS, Mah C, Soumerai SB, Zhang F, Barton MB, Ross-Degnan D. Barriers to self-monitoring of blood glucose among adults with diabetes in an HMO: A cross sectional study. BMC Health Serv Res. 2003;3:1–8. doi: 10.1186/1472-6963-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karter AJ, Ferrara A, Darbinian JA, Ackerson LM, Selby JV. Self monitoring of blood glucose: Language and financial barriers in a managed care population with diabetes. Diabetes Care. 2000;23:477–83. doi: 10.2337/diacare.23.4.477. [DOI] [PubMed] [Google Scholar]
- 33.Goldman D, Smith J. Can patient self-management help explain the SES health gradient. Proc Natl Acad Sci USA. 2002;99:10929–34. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Piette J, Heisler M, Wagner T. Problems paying outof-pocket costs among older adults with diabetes. Diabetes Care. 2004;27:384–91. doi: 10.2337/diacare.27.2.384. [DOI] [PubMed] [Google Scholar]
- 35.Susan LN. Recommendation for healthcare system and self-management education interventions to reduce morbidity and mortality from diabetes. Am J Prev Med. 2002;22:10–4. doi: 10.1016/s0749-3797(02)00422-1. [DOI] [PubMed] [Google Scholar]
- 36.Heisler M, Piette JD, Spencer M, Kieffer E, Vijan S. The relationship between knowledge of rec15793179ent HbA1c values and diabetes care understanding and self-management. Diabetes Care. 2005;28:816–22. doi: 10.2337/diacare.28.4.816. [DOI] [PubMed] [Google Scholar]
- 37.Acuña K, Muniz P, Formiga C, Bastos G, Camilo M, Hashimoto R, et al. A proposal for clinical nutrition education for health care university students and professionals in the Amazon. Nutr Hosp. 2004;19:353–61. [PubMed] [Google Scholar]
- 38.Mazloomy S, Mirzaei A, Afkhami Ardakani M, Baghiani Moghadam M, Fallahzadeh H. The Role of Health Beliefs in Preventive Behaviors of Individuals at High-Risk of Type 2 Diabetes Mellitus. JSHSUMS. 2010;18:24–31. [Google Scholar]
- 39.Shahab Jahanlo AR, GHofrani Poor FA, Kimiyagar M, Vafaie M, Heidarnia AR, Sobhani AR, Jahani JH. Relationship between knowledge, efficacy and quality of life in diabetic patients with blood glucose control and lipid consumer tobacco. JHUMS. 2008;11:261–6. [Google Scholar]
- 40.Shortridge-Baggett LM. Self-efficacy: Measurement and intervention in nursing. Sch Inq Nurs Pract. 2001;15:183–8. [PubMed] [Google Scholar]
- 41.Stuifbergen AK, Seraphine A, Roberts G. An explanatory model of health promotion and quality of life in chronic disabling conditions. Nurs Res. 2000;49:122–9. doi: 10.1097/00006199-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 42.McCaul KD, Glasgow RE, Schafer LC. Diabetes regimen behaviors Predicting adherence. Med Care. 1987;25:868–81. [PubMed] [Google Scholar]
- 43.Bernal H, Woolly S, Schensul JJ, Dickinson JK. Correlates of self-efficacy in diabetes self-care among Hispanic adults with diabetes. Diabetes Edue. 2000;26:673–80. doi: 10.1177/014572170002600415. [DOI] [PubMed] [Google Scholar]
- 44.Wen LK, Shepherd MD, Parchman ML. Family support, diet, and exesice among older Mexican Americans with type 2 diabetes. Diabetes Edue. 2004;30:980–93. doi: 10.1177/014572170403000619. [DOI] [PubMed] [Google Scholar]
- 45.Kavanagh DJ, Gooley S, Wilson PH. Prediction of adherence and control in diabetes. J Behav Med. 1993;16:509–22. doi: 10.1007/BF00844820. [DOI] [PubMed] [Google Scholar]
- 46.Aalto AM, Uutela A. Glycemic control, self_care behaviors, and Psychosocial factors among insulin treated diabetics: a test of an extended health belief model. Int J Behav Med. 1997;4:191–214. doi: 10.1207/s15327558ijbm0403_1. [DOI] [PubMed] [Google Scholar]
- 47.Aljasem LI, Peyrot M, Wissow L, Rubin RR. The impact of barriers and self_ efficacy on self_care behaviors in type 2 diabetes. Diabetes Educ. 2001;27:393–404. doi: 10.1177/014572170102700309. [DOI] [PubMed] [Google Scholar]
- 48.Walker NS, Pullen HC, Herzog M, Boeckner L, Hageman PA. Determinants of older rural women activity and eating. West J Nurs Res. 2006;28:449–66. doi: 10.1177/0193945906286613. [DOI] [PubMed] [Google Scholar]
- 49.Von Ah D, Ebert S, Ngamvitroj A, Park N, Kang DH. Predictors of health behaviors in college students. J Adv Nurs. 2004;48:463–74. doi: 10.1111/j.1365-2648.2004.03229.x. [DOI] [PubMed] [Google Scholar]
- 50.Krichbaum K, Aarestadt V, Buethe M. Exploring the connection between self-efficacy and effective diabetes self-management. Diabetes Educ. 2003;29:653–62. doi: 10.1177/014572170302900411. [DOI] [PubMed] [Google Scholar]
- 51.Norris SL, Engelgau MN, Narayan KM. Effectiveness of self management training in type 2 diabetes: Systematic review of randomised controlled trials. Diabetes Care. 2001;24:561–87. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 52.Van Der Ven NC, Weinger K, Yi J, Pouwer F, Adèr H, Van Der Ploeg HM, et al. The confidence in diabetes self care scale, psychometric properties of a new measure of diabetes-specific self efficacy in Dutch and Us patient with type 1 diabetes. Diabets Care. 2003;26:713–8. doi: 10.2337/diacare.26.3.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chlebowy DO, Garvin BJ. Social support, self-efficacy, and outcome expectations: Impact on selfcare behaviors and glycemic control in Caucasian and African American adults with type 2 diabetes. Diabetes Educ. 2006;32:777–86. doi: 10.1177/0145721706291760. [DOI] [PubMed] [Google Scholar]
- 54.Bonds DE, Camacho F, Bell RA, Duren-Winfield VT, Anderson RT, Goff DC. The association of patient trust and self-care among patients with diabetes mellitus. BMC Fam Pract. 2004;5:2291–98. doi: 10.1186/1471-2296-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gillibrand R, Stevenson J. The extended health belief model applied to the experience of diabetes in young people. Br J Health Psychol. 2006;11:155–69. doi: 10.1348/135910705X39485. [DOI] [PubMed] [Google Scholar]
- 56.Bas M, Donmez S. Self-efficacy and restrained eating in relation to weight loss among overweight men and women in Turkey. Appetite. 2009;52:209–16. doi: 10.1016/j.appet.2008.09.017. [DOI] [PubMed] [Google Scholar]
- 57.Tan MY. The relationship of health beliefs and complication prevention behaviors of Chinese individuals with Type 2 Diabetes Mellitus. Diabetes Res Clin Pract. 2004;66:71–7. doi: 10.1016/j.diabres.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 58.Redmond EH, Burnett SM, Johnson MA, Park S, Fischer JG, Johnson T. Improvement in A1C levels and diabetes self-management activities following a nutrition and diabetes education program in older adults. J Nutr Elder. 2006;26:83–102. doi: 10.1300/J052v26n01_05. [DOI] [PubMed] [Google Scholar]
- 59.Morowati Sharifabad M, Rouhani Tonekaboni N. Perceived self-efficacy in self-care behaviors among diabetic patients referring to Yazd Diabetes Research Center. JBUMS. 2009;15:91–9. [Google Scholar]
- 60.Hosein-Nejad M, Aziz-zadeh-Forozi M, Mohammad-Alizadhe S, Haghdoost AA. Role of Self Efficacy Predictors in Nutritional Behaviors of Kerman High School Female Students in 2006-2007 Academic Year. Journal of Shahid Sadoughi University of Medical Sciences And Health Services. 2008;16:49–56. [Google Scholar]
- 61.Farsi Z, Jabari-Moroui M, Ebadi A. Application of Health Belief Model in Change of Self Care Behaviors of Diabetic Patients. Ir J Nur. 2010;22:61–72. [Google Scholar]
- 62.Sabet Sarvestani R, Hadian Shirazi Z. Diabetes diagnostic indexes and self efficacy of diabetic patients referred to Nader Kazemi center, Shiraz 2006. Ir J Nur Res. 2009;4:15–21. [Google Scholar]
- 63.Asadzandi M, Farsi Z, Najafi Mehr S, Karimizarchi AA. Educational intervention focusing on heath belief model in health belief, awareness and behavior of diabetic patients. IJDLD. 2006;6:169–76. [Google Scholar]
- 64.Borhani F, Abbas Zadeh A, Taebi M, Kohan S. Communication and health beliefs of personal efficacy in patients with type 2 diabetes. Payesh. 2010;9:371–83. [Google Scholar]
- 65.Keshavarz Z, Simbar M, Ramezankhani A. Effective Factors on Nutritional Behavior of Female Workers Based On “Integrated Model of Planned Behavior and Self-efficacy”: A Qualitative Approach. HRJ. 2010;13:199–209. [Google Scholar]
- 66.Charron-Prochownik D, Sereika SM, Becker D, Jacober S, Mansfield J, White NH, et al. Reproductive health beliefs and behaviors in teens with diabetes: Application of the Expanded Health Belief Model. Pediatr Diabetes. 2001;2:30–9. doi: 10.1046/j.1399-543x.2001.00000.x. [DOI] [PubMed] [Google Scholar]
- 67.Coonrod B. Overcoming Physical Barriers to Diabetes Self-Care: Reframing Disability as an Opportunity for Ingenuity. Diabetes Spectrum. 2001;14:28–32. [Google Scholar]
- 68.Wong LY, Toh MP. Understanding of Diabetes Mellitus and Health-preventive Behavior Among Singaporeans. Ann Acad Med Singapore. 2009;38:478–86. [PubMed] [Google Scholar]
- 69.Barceló A, Aedo C, Rajpathak S, Robles S. The cost of diabetes in Latin America and the Caribbean. Bull World Health Organ. 2003;81:19–27. [PMC free article] [PubMed] [Google Scholar]
- 70.Bandura A. Self efficacy mechanism in human agency. Am Psychol. 1982;37:122–47. [Google Scholar]
- 71.Knight KM, Dornan T, Bundy C. The diabetes educator: Trying hard, but must concentrate more on behavior. Diabet Med. 2006;23:485–501. doi: 10.1111/j.1464-5491.2005.01802.x. [DOI] [PubMed] [Google Scholar]
- 72.Baranowski T. Crisis and chaos in behavioral nutrition and physical activity. Int J Behav Nutr Phys Act. 2006;3:27. doi: 10.1186/1479-5868-3-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Issa BA, Baiyewu O. Quality of life of patients with diabetes mellitus in a Nigerian teaching hospital. Hong kong J Psychiatry. 2001;16:27–33. [Google Scholar]
- 74.Fu D, Fu H, McGowan P, Shen YE, Zhu L, Yang H, et al. Implementation and quantitative evaluation of chronic disease self-management programme in Shanghai, China: Randomized controlled trial. Bull World Health Organ. 2003;81:174–82. [PMC free article] [PubMed] [Google Scholar]
- 75.Ismail K, Winkley K, Rabe-Hesketh S. Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Lancet. 2004;363:1589–97. doi: 10.1016/S0140-6736(04)16202-8. [DOI] [PubMed] [Google Scholar]
- 76.Williams Ke, Bond MI. The roles of self –efficacy, out expectaneies and social support in the self-care behavior of diabetes. Psychology Heath and Medicine. 2002;7:127–41. [Google Scholar]
- 77.Van der Bijl JJ, Shortridge-Baggett LM. The theory and measurement of the self-efficacy construct. Sch Inq Nurs Pract. 2001;15:189–207. [PubMed] [Google Scholar]
- 78.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 79.Glanz K, Rimer BK, Lewis FM. 3rd ed. San Francisco, CA: Jossey-Bass Publishers; 2002. Health behavior and health education: Theory, research and practice. [Google Scholar]
- 80.Bandra A. Self efficacy. V.S. Ramachaudran, encyclopedia of human Behavior. 1994;4:71–8. [Google Scholar]
- 81.Abdollahi B. tasire khodkaramadi dar tavanmand saziye karkonan. [Last accessed on 2007 June 7]. Available from: http://www.imi.ir/tadbir/tadbir-168/article-168/4.asp .
- 82.Howells LA. Self-Efficacy and Diabetes: Why is Emotional‘Education’ Important and How Can It Be Achieved? Horm Res. 2002;57(Suppl 1):S69–71. doi: 10.1159/000053317. [DOI] [PubMed] [Google Scholar]
- 83.Hergenhan R, Olson M, editors. Tehran: Nashr Doran; 2006. Theories of Learning. [Google Scholar]
- 84.Tsay SL. Self-efficacy training for patients with end-stage renal disease. J Adv Nurs. 2003;43:370–5. doi: 10.1046/j.1365-2648.2003.02725.x. [DOI] [PubMed] [Google Scholar]


