Abstract
Introduction:
This study was aimed to compare the effect of nutrition educational program based on HBM with traditional education recommended weight gain among pregnant women in Gonabad. Target population was pregnant women who were resided in Gonabad and went to urban health care centers for prenatal cares.
Materials and Methods:
110 pregnant women (case group: 54, control group: 56) were selected who had come to this centers in the first stage of prenatal care (6th -10th week of pregnancy) in 1388 and were consequently classified in case and control group. There is no significant difference for age, education, number of parity, history of abortion and job between case and control groups.
Results:
There was no significant differences in nutritional behavior mean score before intervention in case (74.42 ± 12.78) and control (77.14 ± 15.35) groups (P value = 0.82, independent t- test); but after education, intervention was significant in nutritional behavior between two groups (P value = 0.01, independent t-test);
Discussion:
after intervention, there also was significant difference in HBM structures mean score in case group compare with control group and the highest rise in score was related to perceived benefits (15.13 increment).
Keywords: BMI, health belief model, pregnant women, prenatal nutrition, traditional education
INTRODUCTION
Pregnancy is a great experience associated with many physiologic changes for each woman. It is one of the most important periods for both mothers and fetus which is basically very important for family and society. Mother's health or disease in this period can affect not only her Quality of Life but also the fetus health and life. Many factors can affect mothers and fetus health including appropriate nutrition during pregnancy. Healthy nutrition is very essential in whole life and support humans’ life but in some period including pregnancy persons are more vulnerable and require more attention for nutrition. Pregnant women are more vulnerable to mal nutrition due to physical metabolic and hormonal changes which increases their nutritional needs. In fact the fetus growth and development has a close association with mother nutrition.[1] If mother doesn’t have appropriate nutrition; this will result in side effect in the fetus and can cause irreversible damage in the fetus, as well.[2] Researches have shown that improved mother's nutrition status before and during pregnancy can decrease the neonatal mortality and make better health status and this is more effective than quality and quantity and during neonatal period.[3]
Mother's weight gain is a valid index of control of nutrition status during pregnancy.[4] According to the research recommended weight gain has had significant variability in recent decades.[5] In the early years of previous century it was recommended that mothers’ weight gain had to less than nine Kg to prevent blood pressure abnormality and fatal enlargement.[6] In 1970s pregnant women were encouraged to had at least 14 Kg weight gain to prevent delivery and fetal growth limitation but today after numerous researches, it is concluded that weight gain during pregnancy cannot be same for all women. So, Institute of Medicine (IOM) suggested a weight gain table for pregnant woman according to Body Mass Index (BMI). In this way women were classified according to BMI included four groups: Underweight (BMI less than 19.8), Normal (BMI 19.8-26), Overweight (BMI 26.1-29) and Obese (BMI greater than 29) and suggested weight gain during pregnancy case 12.5-18, 1105-16, 7-11.5 and less than 7 Kg, respectively.[7]
Weight gain less than recommended number supposed to possibly be associated with neural tube defect, preterm labor and low birth weight baby. On the other hand; weight gain higher than recommended amount results in large baby, increase pregnancy induced hypertension, preeclampsia, gestational diabetes and bleeding delivery.[8,9,10] So Cogswell believe that there are many serious challenges regarding weight in recommended range.[11] Consequently pregnant women with any physical situation (Underweight, Normal, Overweight and Obese) must have weight gain which is appropriate with BMI. As a result, one of the most important prenatal cares is education regarding nutrition and diet which explained by health staffs according to prenatal guidelines.
Also many studies have been performed regarding BMI weight gain during pregnancy and its’ outcomes, few researches have been assessed the effect of nutrition and diet educational program especially theory based program for weight gain during pregnancy. Unfortunately theories and their values neglected in education. Lack of appropriate relation between theory and real world has damage to researches and scientific efforts. Health educators assumed that individuals change easily their behaviors according to educational objectives. They also believe that behavior change program occur easily with traditional and ordinary education[12] but today it is believe that the value of education program is related to effectiveness, creation or change health behaviors and change behavior is not an objective which could be easily accessible. The effectiveness of education is related to appropriate behavior science theories usage. These theories have great potential to increase the effectiveness of health education programs.[13]
Health Belief Model is one of the intrapersonal health education models (derived from behavior science theory) which are administered for nutrition education in various subjects. The philosophy of this model that educators can result in creation or behavior change include four characteristics; Firstly; behavior has benefits for health, economy, social, family and cultural, Secondly; health educators know the barriers related to choosing behaviors and consider them for planning. Thirdly; educational program should induce appropriate susceptibility among people that lack of health behavior can result in side effects and complications including health hazards, economic, social and family hazards and fourthly; it is necessary that for choosing health behavior, cues to action including individual training and educational media should be used besides named items.[14,15,16] Therefore this study was performed with the objective of comparison the effect of nutritional educational program based on HBM with traditional education recommended weight gain during pregnant women in Gonabad.
MATERIALS AND METHODS
This research was a quasi-experimental (interventional) study which was performed in two groups including case and control. Target population in this study was pregnant women who were resided in Gonabad and went to urban health care centers for prenatal care. So, 110 pregnant women (case group: 54, control group: 56) were selected who had come to this centers in the first stage of prenatal care (6th-10th week of pregnancy) in 1388 and were classified in case and control group. Case selection was in this way: first person was classified in the case group randomly and next person was classified in control group and this process was continued to last person. Data gathering according to HBM was performed with a 83-questions questionnaire in eight parts including: Demographic characteristics (14 items), Knowledge (25 items), perceived sensitivity (7 items), perceived severity (7 items), perceived benefits (7 items), perceived barriers (7 items), cues to action (2 items) and practice (14 items). Knowledge, HBM structures and practice scale was based on calculated score out of 100. Multiple choice questions, four option Likert scale and yes/no questions were used for knowledge, HBM structures model and practice, respectively. Score 1 for right answer and zero for wrong answer were considered for knowledge and practice questions. Scoring system for HBM was based on like rt scale and score: 1-4 was considered for items.
Validity and reliability was assessed by face and content methods. After primary planning, six professors on health education, nutrition, and midwifery department reviewed the questioner and their suggestions were included in the questionnaire. Reliability was assessed by Test- retest for knowledge and practice questions and internal consistency reliability for HBM structure by means of 14 women (other than case and controls). Validity for knowledge, practice and HBM model was r = 0.86, r = 0.88 and r = 0.82 respectively (α = 0.85).
Before educational intervention, questionnaire was completed by a female researcher in both groups via an organized interview in the first stage of prenatal care. Then the interview based on HBM was performed in two sessions of nutritional education (sixteen minuets for each session) according to nutrition educational Guidelines in health care centers and live lecture, group discussion, Colloquy and individual nutrition consultation for experimental group. In the first session of education plan all case partners were invited to have an active participation. In control group, current education without using educational model for nutrition during pregnancy in health care centers was performed. In this way, two sessions of nutritional education (sixteen minuets for each session) was done. Post-test in a similar pattern to pretest was performed for case and controls groups in 38th to 40th weeks of pregnancy. Finally all data were analyzed with SPSS software via central tendency, Paired- t test, independent test, and correlation coefficient, χ2 and Kruskal-wallis test in the confidence interval of 95%.
RESULTS
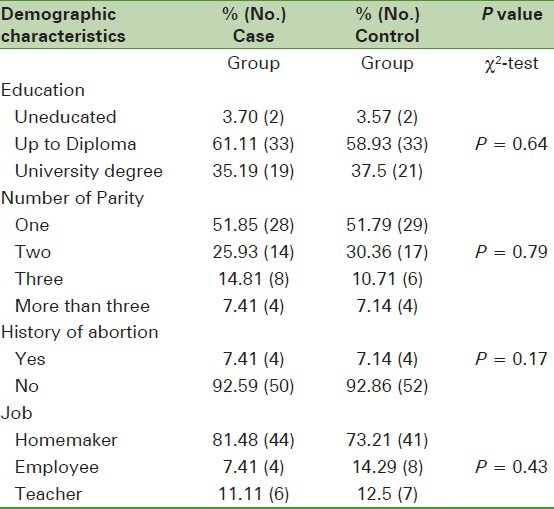
There was no significant difference in mean age in case (26.62 ± 5.62) and control (27.72 ± 5.15) group (independent t- test). Also no significant difference was present in number of parity in case (first pregnancy 51.85%) and control (first pregnancy 51.79%) groups (P value = 0.79,chai square test). Table 1 reveals other demographic characteristics of participants.
Table 1.
Demographic characteristics in both case and control groups
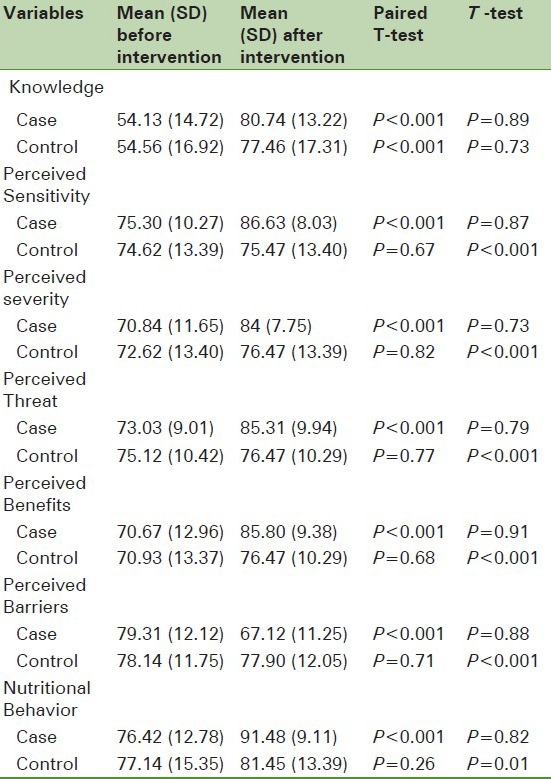
After external cues to action, intervention partner (82.26%) and health care staff (56.56%) were the most important external cues to action for weight gain and in both case and control groups. Fatal health (73.4%) in case group and inability to manage daily routine works (44.65%) in control group were the most important cues to action an appropriate weight gain. There was no significant differences in nutritional behavior mean score before intervention in case (74.42 ± 12.78) and control (77.14 ± 15.35) groups (P value = 0.82, independent t- test); but after education there was significant difference in nutritional behavior between two groups (P value = 0.01, independent t- test); also after intervention there was significant difference in HBM structures mean score in case group compare with control group and the highest rise in score was related to perceived benefits (15.13 increment). Table 2 demonstrates mean score of variables in both groups.
Table 2.
Mean scores of knowledge, HBM structures and nutritional behavior in both case and control groups
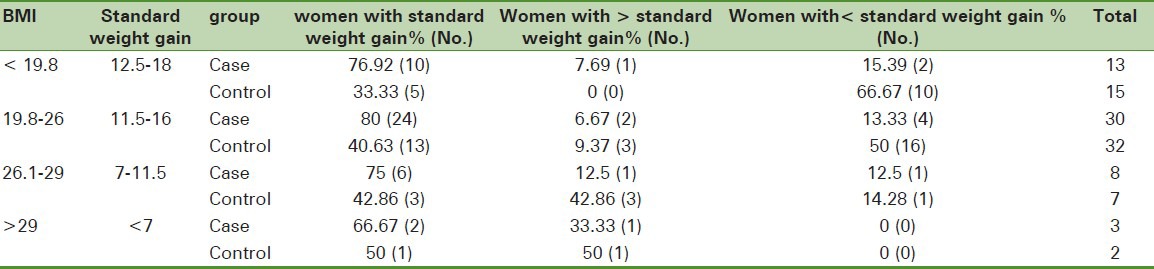
On the other hand; there was direct significant relation between nutritional behavior and perceived sensitivity, severity, threatening and indirect significant relation between named behavior and perceived barriers as well (Correlation Coefficient test). Before intervention underweight, normal, overweight and obese participants (both case and control groups) were 25.45%, 56.34%, 13.64% and 4.55%, respectively.77.78% of pregnant women in case group obtained recommended BMI but 39.25% control group obtained it. Table 3 shows weight gain during pregnancy in case and control compared with IOM standard.
Table 3.
Comparesion between weight gains during pregnancy in with standard both case and control groups
DISCUSSION
There is no significant difference for age, education, number of parity, history of abortion and job between case and control groups. This could be a common factor evaluating the effect of education based on HBM and traditional (classic) education and also comparison of variables after intervention between two groups. According to IOM definition, 25.45% of total participants had BMI less than 19.8 which was similar to study of Sharifzadeh GH et al. in Birjand.[4] It seems that this similarity which is declared in other BMI subgroups, is due to similar lifestyle and nutritional culture in both cities. In this study, researchers asked the partners to be attended in the educational sessions in case group. Their attendance resulted in greater concern for mother health and increase education effect for nutritional behavior. So, 86.36% mothers in case group chose their partners as the most important factor to adhere diet regime for ideal weight gain. On the other hand before the intervention only 11.65% women chose it but this meaningful change was not present in control group.
In fact, their attendance as external cues to action guaranteed the effectiveness and sustainability healthy behavior and this approach can result in their further participation in the health care district. According to educational content, fetal health was consider as the important factor to induce healthy nutrition behavior and was consider as internal cues to action.
According to HBM structures, mothers’ special consideration for fatal health can result in appropriate capacity for more effective education in them. So the important factors in this field are increased perceived sensitivity and severity beside to perceived barriers promotion and decreased perceived barriers for choosing healthy nutritional behavior for appropriate weight gain. Table 2 shows that education based on named theory was required to make potentially change the effective factors of weight gaining, so nutritional education results in promotion of knowledge, nutritional practice, perceived sensitivity, severity, threatening and benefits, also it was effective to decrease perceived barriers (Paired-t-test).
Abood et al, study suggested HBM for nutritional education;[17] also Anderson et al, study approved the ability of this model for nutritional education.[18] Sharifirad GH et al, study confirmed the effect of nutritional education based on HBM for nutritional practice.[14] Since perceived benefits had greatest increment in case group. It can be concluded that explaining the benefits of appropriate weight gain according to BMI and it's easily achievement had great concern for mothers and their partners, so necessitate special focus.
Also this variable had greatest significant direct correlation with nutritional behavior (r = 0.72). Perceived barriers were the only variable which had significant indirect relation with nutritional behavior and its mean score had significant decrement after intervention in case group.
Table 2 shows that knowledge is the only variable with significant intervention in control group and traditional education in health care centers was effective in their knowledge promotion about nutrition, but knowledge doesn’t result necessarily in nutritional behavior improvement. Other researches including Khajavi Shojaii et al, study showed that the majority of studied women had lowered knowledge or nutrition during pregnancy.[19] Despite positive attitude to nutrition in their study, their practice for nutrition during pregnancy wasn’t appropriate and the majority of pregnant women didn’t change their diet during pregnancy. Mahmood et al, study[20] and Kapil et al,[21] revealed that pregnant women had little knowledge regarding appropriate diet for desirable weight gain. Studied performed on Chinese and Italian pregnant women showed that in spite of relatively appropriate knowledge about nutrition, they had poor nutritional practice[22,23]; also some researchers including Sajadi et al, study have shown the intermediate level of knowledge about nutrition in pregnant women.[24]
There was a significant difference for recommended weight gain between case and control groups (77.78% of case and 39.29% of control groups obtained the recommended weight gain according to BMI). On the other hand some researches including Sharifzadeh et al,[4] Joseph et al[25] and Khosravi et al.[26] revealed that there is no appropriate weight gain in pregnant women in health care centers. So traditional education program in national health care systems, do not have appropriate effect for recommended weight gain during pregnancy and need essential intervention including theory based education. Table 3 showed that this difference is both significant and true in all BMI groups including standard weight gain, higher and lower than standard weight gain. This study demonstrated that nutritional education based on HBM for recommended weight gain during pregnancy has successful results compared with traditional education, consequently appropriate weight gain according to mother BMI was maximum and not standard weight gain was minimum. Since this research was performed in small town (Gonabad), some participants in case and control group had communication and transferred information to each other. Also evaluation of nutritional behavior was based on self-declaration which could be one of the limitations in this study. Also self-efficacy was not evaluated in this research which needs another study. Since health care system emphasize on mother and baby health status during pregnancy, nutritional education based on HBM for recommended weight gain in pregnancy had successful result, but unfortunately few studies have been performed in the field of evaluating the effect of model and theory based education intervention in pregnancy; so according to the result of this study, an appropriate effect of this model of weight gain during pregnancy recommended to performed other researches including theory based interventional studies like Theory of Planned Action (TPA) and Precaution Adoption Process Model (PAPM) in health care system.
ACKNOWLEDGMENTS
This study financially was supported by Gonabad University of Medical Sciences, Iran. The authors deeply are thankful to participants, Gonabad health care staff and health promotion, social development research center for their support.
Footnotes
Source of Support: Gonabad University of Medical Sciences, Iran
Conflict of Interest: None declared.
REFERENCES
- 1.Safari M, Saadatmand N, Azarman M. Food Intake Pattern and Related Factors in Women Referred to Medical and Health Centers of Yasouj. Dena, Quarterly Journal of Yasuj. 2007;2:27–37. Persian. [Google Scholar]
- 2.Szwajcer EM, Hiddink GJ, Koelen MA, van Woerkum CM. Nutrition awareness and pregnancy: Implications for the life course perspective. Eur J Obstet Gynecol Reprod Biol. 2007;135:58–64. doi: 10.1016/j.ejogrb.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 3.Dnncan SS, Malnutrition CJ. Pregnancy and Infant Mortality. A biometric model of interdisciplinary history. Pregnancy and infant mortality. 1999;30:37–60. doi: 10.1162/002219599551903. [DOI] [PubMed] [Google Scholar]
- 4.Sharifzadeh GH, Moodi M, Nasseh N. Evaluation of pregnant women weight gain in Birjand Health Centers. J Birjand Univ Med Sci. 2009;3:21–7. Persian. [Google Scholar]
- 5.Tabandeh A, Kashani E. Effects of maternal body mass index and weight gain during pregnancy on the outcome of delivery. J Gorgan Univ Med Sci. 2007;1:20–4. Persian. [Google Scholar]
- 6.Cunningham FG, Norman FG, Leveno KJ, Gilstrap LC, Hauth JC, Wenstrom KD. 21st ed. USA: McGraw-Hill Professional; 2001. Williams Obsteetrics; pp. 231–2. [Google Scholar]
- 7.Panahandeh Z, Pour Ghasemi M, Asghar Nia M. Body mass index and prenatal weight gain. J Gilan Univ Med Sci. 2006;57:15–20. Persian. [Google Scholar]
- 8.Kalk P, Guthmann F, Krause K, Relle K, Godes M, Gossing G, et al. Impact of maternal body mass index on neonatal outcome. Eur J Med Res. 2009;14:216–22. doi: 10.1186/2047-783X-14-5-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Valero De Bernabé J, Soriano T, Albaladejo R, Juarranz M, Calle ME, Martínez D, et al. Risk factors for low Birth weight: A review. Eur J Obstet Gynecol Reprod Biol. 2004;116:3–15. doi: 10.1016/j.ejogrb.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 10.Evenson KR, Bradley CB. Belief about exercise and physical activity among pregnant women. Patient Educ Couns. 2010;79:124–9. doi: 10.1016/j.pec.2009.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cogswell ME, Serdula MK, Hungerford DW, Yip R. Gestational weight gains among average- weight and overweight women what is excessive? Am J Obstet Gynecol. 1995;172:705–12. doi: 10.1016/0002-9378(95)90598-7. [DOI] [PubMed] [Google Scholar]
- 12.Whitehead D. Health educations behavioral and social psychology: Nursing contribution to health promotion. J Adv Nurs. 2001;34:822–32. doi: 10.1046/j.1365-2648.2001.01813.x. [DOI] [PubMed] [Google Scholar]
- 13.Whitehead D, Russell G. How effective are health education programmers: Resistance, reactance, rationality and risk? Recommendation for affection practice. Int J Nurs Stud. 2003;41:163–72. doi: 10.1016/s0020-7489(03)00117-2. [DOI] [PubMed] [Google Scholar]
- 14.Sharifirad GH, Entezari MS, Kamran A, Azadbakht L. Effectiveness of nutrition education to type II diabetic patients: Application of Health Belief Model. Iranian J Diabetes Lipid Disord. 2008;4:379–86. Persian. [Google Scholar]
- 15.Sharifirad GH, Hazavehie SM, Mohebi S, Rahimi MA, Hasanzadeh A. The effect of educational program based on Health Belief Model (HBM) on the foot care by type II diabetic patients. Iranian J Endocrinol Metab. 2006;3:231–9. Persian. [Google Scholar]
- 16.Morowati Sharifabad MA, Rouhani Tonekaboni N, Baghianimoghadam MH. Predictors of self-care behaviors among diabetic patients referred to Yazd diabetes research Centre based on extended health belief model. J Shahid Sadoughi Univ Med Sciences Health Serv. 2007;3:85–96. Persian. [Google Scholar]
- 17.Abood DA, Black DR, Feral D. Nutrition education worksite intervention for university staff: Application of the health belief model. J Nut Edu Behav. 2003;35:260–7. doi: 10.1016/s1499-4046(06)60057-2. [DOI] [PubMed] [Google Scholar]
- 18.Anderson AS, Cox DN, McKellar S, Reynolds J, Lean ME, Mela DJ. Take five a nutrition education intervention to increase fruit and vegetable intakes: Impact on attitude towards dietary change. Br J Nutr. 1998;90:133–40. doi: 10.1017/s0007114598001032. [DOI] [PubMed] [Google Scholar]
- 19.Khajavi Shojaii K, Parsay S, Fallah N. Assessment of nutritional knowledge, attitude and practices in pregnant women in university hospitals of Tehran. J Gorgan Uni Med Sci. 2001;8:70–5. Persian. [Google Scholar]
- 20.Mahmood S, Atif MF, Mujeeb SS, Babo N, Mobasher H. Assessment of nutritional beliefs and practices in pregnant and lactating mothers in an urban rural area of Pakistan. J Pak Med Assoc. 1997;47:60–2. [PubMed] [Google Scholar]
- 21.Kapil U, Bhasin S, Manocha S. Knowledge amongst adolescent girls about nutritive value foods and diet during disease pregnancy and lactation. Indian Pediatr. 1992;28:1135–9. [PubMed] [Google Scholar]
- 22.Kozlowska- Wojciechowska M, Wujes MM. Dietary knowledge and practice in pregnant women. Rocz Panstw Zaki Hig. 2002;53:165–75. [PubMed] [Google Scholar]
- 23.Zeng G, Zhang J, Liang JZ, Zhou R, Song MY, Zhang YJ. Study on the knowledge of nutition and related dietary behavior among floating women under pregnancy. Zhonghua Liv Xing Bing Xue Za Zhi. 2005;26:408–11. [PubMed] [Google Scholar]
- 24.Sajadi P, Bakhtiyari A, Haji Ahmadi M. Knowledge of nutritional assessment of pregnant women referred to health centers in Babol city. J Babol Univ Med Sci. 2007;5:50–4. Persian. [Google Scholar]
- 25.Joseph NP, Hunkali KB, Wilson B, Morgan E, Cross M, Freund KM. Pre-Pregnancy body mass index among pregnant adolescents: Gestational weight gain and long term postpartum weight retention. J Pediatr Adolesc Gynecol. 2008;21:195–200. doi: 10.1016/j.jpag.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 26.Khosravi F, Sadeghi Khameneh S, Safaeian AR. Relation between pregnancy weight gain and newborn's weight and size in women referring to health centers in Tabriz. J Shaheed Beheshti Univ Med Sci. 2005;49:41–33. Persian. [Google Scholar]


