Abstract
Spontaneous OHSS is a rare event in pregnancy following natural conception and only a few cases have been reported in the literature so far. This report is a case of spontaneously conceived pregnancy with Spontaneous OHSS and Primary hypothyroidism
KEY WORDS: Hypothyroidism, spontaneous ovarian hyper stimulation syndrome, thyroid stimulating hormone
INTRODUCTION
Spontaneous ovarian hyperstimulation (spontaneous OHSS) is extremely rare in naturally conceived pregnancies. OHSS in the absence of exogenous gonadotropins is very rare, and only a few cases have been reported in the literature.[1,2,3,4,5,6,7,8] Van Wyk and Grumbach first described the combination of multicystic ovaries, juvenile hypothyroidism and precocious puberty in 1960, since then sporadic cases of this syndrome have been reported in pre-pubertal or adolescent girls.[9,10,11,12] Few cases only have been reported for adults both gestational and non-gestational.[1,2,3,4,5,6,7,8] Spontaneous OHSS likely to occur at 8-14 weeks of gestation, while iatrogenic OHSS usually occurs earlier at 3-8 weeks of gestation.[13,14] The etiopathogenesis of spontaneous OHSS is not studied well.
CASE REPORT
A 22 year old primigravida with spontaneous conception, regular menstrual cycles, married for 3 months and no relevant past medical illness, no clinical or subclinical evidence of hypothyroidism in the past; attended the Department of Obstetrics at 7 weeks of gestation. She was asymptomatic, and ultrasound scan also revealed single live intrauterine pregnancy at 7 weeks and normal appearing ovaries. At 9 weeks of gestation, she developed vomiting, diarrhoea and lower abdominal discomfort. Abdominal examination revealed a non-tender, mobile mass of approximately 10 cm × 10 cm in the right iliac fossa with no clinical evidence of ascites.
Ultrasound scan performed at 9 weeks of gestation revealed a single live intrauterine gestation corresponding to 9 weeks of gestation, bilaterally enlarged multicystic ovaries with right ovary measuring 10 cm × 8 cm, left ovary 8 cm × 6 cm and no ultrasonological evidence of ascites, pleural or pericardial effusion [Figures 1 and 2].
Figure 1.

Transvaginal ultrasonography showing bilateral multilocular ovarian cystic masses with spontaneous ovarian hyperstimulation, spontaneously conceived singleton pregnancy at 9 weeks
Figure 2.
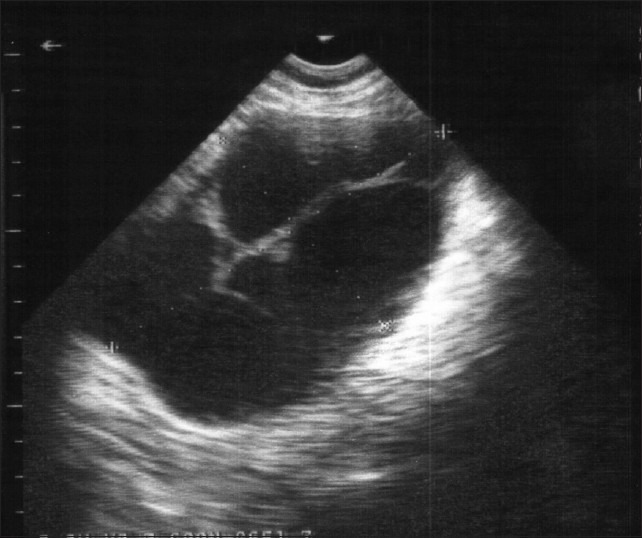
Hyperstimulated right ovary
Started with levothyroxin 150 μg daily. The abdominal discomfort reduced from 14th week onward and the size of the ovaries normalized at 20 weeks. At 17 weeks of gestation, triple screening was performed, and the report showed low risk (1/6500) for chromosomal aneuploidies. Anomaly scan done at 20 weeks showed no fetal or placental anomalies and bilateral maternal ovaries were normal sized.
The patient delivered a term female baby weighing 3300 g at 39 weeks of gestation.
DISCUSSION
Spontaneous OHSS can occur both in pregnant and non-pregnant women. De Leener[15] classified spontaneous OHSS syndrome into three types based on clinical presentation and FSH receptor mutation. Type I is associated with the mutated FSH receptor and this type may cause recurrent spontaneous OHSS. Type II is secondary to high levels of human chorionic gonadotropin (hCG) as in hydatiform mole and multiple gestation and is the most frequent one. Type III is related to hypothyroidism.
The pathophysiology of spontaneous OHSS associated with hypothyroidism is not studied well. The explanations given are (a) excessive estriol via the 16-hydroxylation pathway instead of the normal 2-hydroxylation that has been demonstrated in hypothyroid patients. Excessive gonadotropin release, due to decreased feedback regulation caused by substitution of estradiol by the less potent estriol, would result in spontaneous OHSS in those subjects;[16](b) High levels of thyroid stimulating hormone can directly stimulate ovaries in women with hypothyroidism and can cause ovarian hyperstimulation.[5]
Mutations in the FSH receptor (FSHR) could be activating, leading to a predisposition to OHSS, or inactivating, resulting in sterility due to poor ovarian response to gonadotropins. Polymorphisms of FSHR have been investigated and about 744 single nucleotide polymorphisms have been identified in the FSHR gene, of which only eight are located in the coding region, exons, with the rest being intronic. Ovarian response is dependent on the FSHR genotype. Clinical studies on the p.N680S polymorphism of the FSHR gene have demonstrated the homozygous Ser/Ser variant to be less sensitive to endogenous or exogenous FSH in terms of oestradiol production. Polymorphism of the FSHR, Ser680Asn, in the FSHR gene is a predictor of the severity of symptoms in patients who develop OHSS.[17,18]
Activating mutations of the FSHR gene that cause ovarian hyper-responsiveness to circulating FSH or even cross-responsiveness of FSHR to hormones having a structure similar to FSH, such as hCG or TSH[19] hCG/LH receptor gene mutation claimed increased response to normal hCG levels and hence ovarian hyper responsiveness because of this mutation.[20]
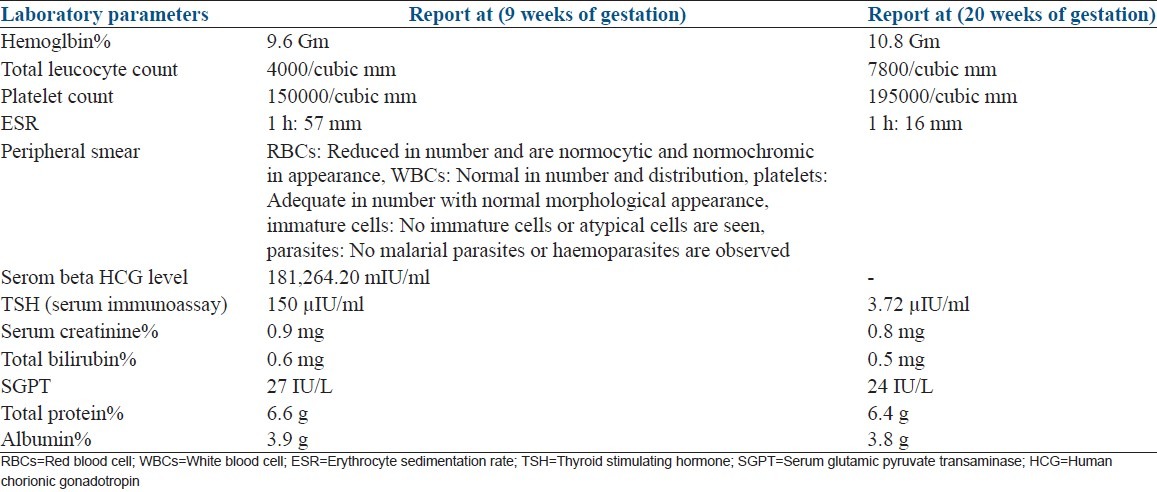
Unlike in iatrogenic OHSS, in spontaneous OHSS extravascular fluid retention may not occur and usually a hemodilution rather than hemoconcentration is seen as in this case (the blood pcture showed anemia instead of hemoconcentration Table 1) and this may be due to the difference in the etiopathogenesis of iatrogenic and spontaneous OHSS. Again if, the spontaneous OHSS is due to high level of hCG concentration as in multiple gestation and trophoblastic disease then as in iatrogenic OHSS extra vascular fluid retention is common, raising the suspicion of difference in clinical presentation and pathogenesis according to the etiology. It is important to diagnose and manage spontaneous OHSS timely to prevent the occurrence of severe complication. Early diagnosis and appropriate treatment will avoid further complications. The OHSS is managed according to the degree of severity.
Table 1.
Blood analysis was performed at 9 and 20 weeks of gestation were as follows
Hyperstimulated ovaries release a number of vasoactive mediators under the influence of hCG. These include vascular endothelial growth factor and several pro-inflammatory cytokines that interact to produce the characteristic pathophysiology of OHSS. This is marked by increased capillary permeability, leakage of fluid from the vasculature, third space fluid accumulation and intravascular dehydration.[21]
Olatunbosun et al.,[22] in 1996 reported a case of spontaneous OHSS in a patient with polycystic ovarian disease, who experienced severe spontaneous OHSS in four consecutive singleton pregnancies and achieved live births in two of the pregnancies. This was the third reported case of spontaneous OHSS associated with pregnancy and the first to result in live births. Ahmed Kamel[1] reported a case of spontaneous OHSS in a woman, who presented in the second trimester of her first pregnancy with persistent abdominal pains, shortness of breath, vomiting, and diarrhea and the author stressed the importance of a thorough evaluation of all women who present with acute abdomen and ovarian masses during pregnancy as even though the condition is extremely rare, it can be lethal in its severe form if not timely diagnosed. Cardoso[2] reported a case of naturally conceived pregnancy associated with spontaneous OHSS and primary hypothyroidism where TSH level and ovarian size returned to normal at 24 weeks of gestation. Edwards-Silva et al.[3] reported a case of pregnancy with spontaneous OHSS syndrome, uncontrolled hypothyroidism, elevated hCG, deep vein thrombosis, and Rh isoimmunization and conservatively managed with levothyroxine and heparin and noted regression of the ovaries by 22 weeks of gestation after adequate thyroid repletion and delivered a non-hydropic preterm baby at 35 weeks of gestation.
It is imperative that all health care providers, including gynecologists, surgeons and physicians should consider hypothyroidism and other endocrine disorders in the differential diagnosis of adult females presenting with multicystic ovarian tumors to avoid unnecessary and catastrophic ovarian resection.[8]
In non-pregnant subjects, the clinical presentation of spontaneous OHSS ascites, ovarian enlargement and pleural effusion may misdiagnose this condition as advanced ovarian malignancy and may ended up in exploratory laparotomy. Hence, proper evaluation and correct diagnosis are important for the prevention of mismanagemen.
Rarity of this condition may also be due to misdiagnosis and by missing the diagnosis that can result in mismanagement or severe complications of this condition.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Ahmed Kamel RM. Spontaneous ovarian hyperstimuation syndrome in a naturally conceived singleton pregnancy. Fertil Steril. 2010;94:351. doi: 10.1016/j.fertnstert.2009.12.076. e.1-4. [DOI] [PubMed] [Google Scholar]
- 2.Cardoso CG, Graça LM, Dias T, Clode N, Soares L. Spontaneous ovarian hyperstimulation and primary hypothyroidism with a naturally conceived pregnancy. Obstet Gynecol. 1999;93:809–11. doi: 10.1016/s0029-7844(98)00435-9. [DOI] [PubMed] [Google Scholar]
- 3.Edwards-Silva RN, Han CS, Hoang Y, Kao LC. Spontaneous ovarian hyperstimulation in a naturally conceived pregnancy with uncontrolled hypothyroidism. Obstet Gynecol. 2008;111:498–501. doi: 10.1097/01.AOG.0000279139.12412.90. [DOI] [PubMed] [Google Scholar]
- 4.Yamashita Y, Kawamura T, Fujikawa R, Mochizuki H, Okubo M, Arita K. Regression of both pituitary and ovarian cysts after administration of thyroid hormone in a case of primary hypothyroidism. Intern Med. 2001;40:751–5. doi: 10.2169/internalmedicine.40.751. [DOI] [PubMed] [Google Scholar]
- 5.Taher BM, Ghariabeh RA, Jarrah NS, Hadidy AM, Radaideh AM, Ajlouni KM. Spontaneous ovarian hyperstimulation syndrome caused by hypothyroidism in an adult. Eur J Obstet Gynecol Reprod Biol. 2004;112:107–9. doi: 10.1016/s0301-2115(03)00283-5. [DOI] [PubMed] [Google Scholar]
- 6.Bassam T, Ajlouni K. A case of ovarian enlargement in severe primary hypothyroidism and review of the literature. Ann Saudi Med. 2006;26:66–8. doi: 10.5144/0256-4947.2006.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kubota K, Itho M, Kishi H, Igarashi S, Minegishi T. Primary hypothyroidism presenting as multiple ovarian cysts in an adult woman: A case report. Gynecol Endocrinol. 2008;24:586–9. doi: 10.1080/09513590802288192. [DOI] [PubMed] [Google Scholar]
- 8.Shu J, Xing L, Zhang L, Fang S, Huang H. Ignored adult primary hypothyroidism presenting chiefly with persistent ovarian cysts: A need for increased awareness. Reprod Biol Endocrinol. 2011;9:119. doi: 10.1186/1477-7827-9-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panico A, Lupoli GA, Fonderico F, Colarusso S, Marciello F, Poggiano MR, et al. Multiple ovarian cysts in a young girl with severe hypothyroidism. Thyroid. 2007;17:1289–93. doi: 10.1089/thy.2007.0056. [DOI] [PubMed] [Google Scholar]
- 10.Gordon CM, Austin DJ, Radovick S, Laufer MR. Primary hypothyroidism presenting as severe vaginal bleeding in a prepubertal girl. J Pediatr Adolesc Gynecol. 1997;10:35–8. doi: 10.1016/s1083-3188(97)70042-1. [DOI] [PubMed] [Google Scholar]
- 11.Ryan GL, Feng X, d’Alva CB, Zhang M, Van Voorhis BJ, Pinto EM, et al. Evaluating the roles of follicle-stimulating hormone receptor polymorphisms in gonadal hyperstimulation associated with severe juvenile primary hypothyroidism. J Clin Endocrinol Metab. 2007;92:2312–7. doi: 10.1210/jc.2006-2086. [DOI] [PubMed] [Google Scholar]
- 12.Browne LP, Boswell HB, Crotty EJ, O’Hara SM, Birkemeier KL, Guillerman RP. Van Wyk and Grumbach syndrome revisited: Imaging and clinical findings in pre- and postpubertal girls. Pediatr Radiol. 2008;38:538–42. doi: 10.1007/s00247-008-0777-1. [DOI] [PubMed] [Google Scholar]
- 13.Smits G, Olatunbosun O, Delbaere A, Pierson R, Vassart G, Costagliola S. Ovarian hyperstimulation syndrome due to a mutation in the follicle-stimulating hormone receptor. N Engl J Med. 2003;349:760–6. doi: 10.1056/NEJMoa030064. [DOI] [PubMed] [Google Scholar]
- 14.Zalel Y, Katz Z, Caspi B, Ben-Hur H, Dgani R, Insler V. Spontaneous ovarian hyperstimulation syndrome concomitant with spontaneous pregnancy in a woman with polycystic ovary disease. Am J Obstet Gynecol. 1992;167:122–4. doi: 10.1016/s0002-9378(11)91642-1. [DOI] [PubMed] [Google Scholar]
- 15.De Leener A, Montanelli L, Van Durme J, Chae H, Smits G, Vassart G, et al. Presence and absence of follicle-stimulating hormone receptor mutations provide some insights into spontaneous ovarian hyperstimulation syndrome physiopathology. J Clin Endocrinol Metab. 2006;91:555–62. doi: 10.1210/jc.2005-1580. [DOI] [PubMed] [Google Scholar]
- 16.Rotmensch S, Scommegna A. Spontaneous ovarian hyperstimulation syndrome associated with hypothyroidism. Am J Obstet Gynecol. 1989;160:1220–2. doi: 10.1016/0002-9378(89)90196-8. [DOI] [PubMed] [Google Scholar]
- 17.Rizk B. Symposium: Update on prediction and management of OHSS. Genetics of ovarian hyperstimulation syndrome. Reprod Biomed Online. 2009;19:14–27. doi: 10.1016/s1472-6483(10)60041-7. [DOI] [PubMed] [Google Scholar]
- 18.Vassart G, Pardo L, Costagliola S. A molecular dissection of the glycoprotein hormone receptors. Trends Biochem Sci. 2004;29:119–26. doi: 10.1016/j.tibs.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 19.Lussiana C, Guani B, Restagno G, Rovei V, Menato G, Revelli A, et al. Ovarian hyper-stimulation syndrome after spontaneous conception. Gynecol Endocrinol. 2009;25:455–9. doi: 10.1080/09513590902898213. [DOI] [PubMed] [Google Scholar]
- 20.Akerman FM, Lei Z, Rao CV, Nakajima ST. A case of spontaneous ovarian hyperstimulation syndrome with a potential mutation in the hCG/LH receptor gene. Fertil Steril. 2000;74:403–4. doi: 10.1016/s0015-0282(00)00628-2. [DOI] [PubMed] [Google Scholar]
- 21.Alper MM, Smith LP, Sills ES. Ovarian hyperstimulation syndrome: Current views on pathophysiology, risk factors, prevention, and management. J Exp Clin Assist Reprod. 2009;6:3. [PMC free article] [PubMed] [Google Scholar]
- 22.Olatunbosun OA, Gilliland B, Brydon LA, Chizen DR, Pierson RA. Spontaneous ovarian hyperstimulation syndrome in four consecutive pregnancies. Clin Exp Obstet Gynecol. 1996;23:127–32. [PubMed] [Google Scholar]


