Abstract
Herlyn-Werner-Wunderlich (HWW) syndrome is a very rare congenital anomaly of the urogenital tract involving Müllerian ducts and Wolffian structures. It is characterized by the triad of didelphys uterus, obstructed hemivagina, and ipsilateral renal agenesis. Magnetic resonance imaging (MRI) is a sensitive, non-invasive diagnostic modality for demonstrating anatomic variation and associated complications.
KEY WORDS: Herlyn-Werner-Wunderlich, MRI, Müllerian
INTRODUCTION
The association of renal agenesis with ipsilateral blind hemi vagina and didelphys uterus constitutes the uncommon Herlyn-Werner-Wunderlich (HWW) syndrome.[1] [Figure 1a and b] These are the consequence of Müllerian and mesonephric duct anomalies (MDA). The incidence of didelphys uterus, related to HWW, is approximately 1/2,000 to 1/28,000, and it is accompanied by unilateral renal agenesis in 43% of cases.[2] MDA are congenital entities resulting from non-development (agenesia or hypoplasia), defective vertical or lateral fusion, or resorption failure of the Müllerian (paramesonephric) ducts.[3] A complete or partial vaginal septum is present in 75% of females with didelphys uterus.[4] A known variant is obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) such as duplicated kidneys, dysplastic kidneys, or retro vesical bands.
Figure 1.
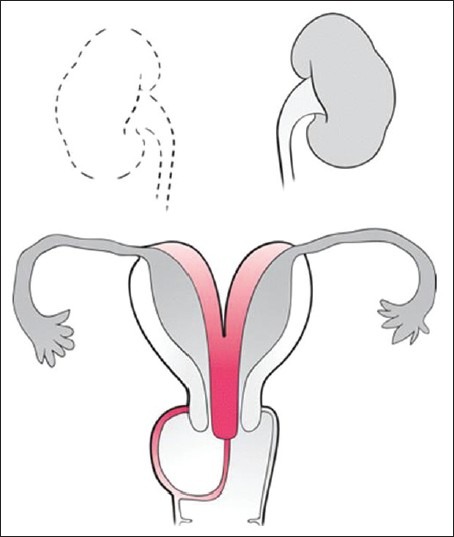
Representative line diagram depicting right renal agenesis, uterine didelphys, and vaginal septum
The various Mullerian duct anomalies can be categorized broadly as follows:
Class 1: Segmental agenesis and variable degrees of uterovaginal hypoplasia
Class 2: Unicornuate uteri that represent partial or complete unilateral hypoplasia
Class 3: Uterus didelphys, in which duplication of the uterus results from complete non-fusion of the mullerian ducts
Class 4: Bicornuate uteri that demonstrate incomplete fusion of the superior segments of the uterovaginal canal
Class 5: Septate uteri that represent partial or complete non-resorption of the uterovaginal septum
Class 6: Arcuate uteri that result from near complete resorption of the septum
Class 7: Comprise sequel of diethylstilbestrol exposure in utero
CASE REPORT
A 13-years-old female presented with a history of severe abdomino-pelvic pain, which increased with each of her menstrual cycles lasting 2–7 days. Gynecological history indicated menarche 3 months back. However, there was no abnormal vaginal bleeding, nausea, vomiting, or diarrhoea. A bimanual physical examination indicated a right-sided cystic and tender pelvic mass, movable, and mildly tender to palpation. Ultrasound showed the absence of right kidney, uterine didelphis, and a caudal cystic lesion with internal echogenicities adjacent to it [Figure 2a and b]. Magnetic resonance imaging (MRI) was performed in order to evaluate the possible genito-urinary anomaly.
Figure 2.
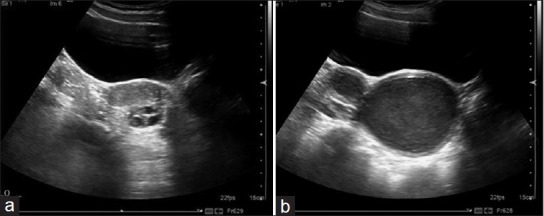
(a) Trans-abdominal sonography in coronal plane demonstrating uterine cornua. (b) Trans-abdominal sonography in the sagittal plane demonstrating cornua and vaginal collection
MRI showed evidence of uterine didelphis, the left segment draining normally through a collapsed left hemivagina, and seen to communicate with left cervix and corresponding uterine horn. The right hemivagina was markedly distended (5.63 cm). Its lower end was convex and placed 4.75 cm above the introitus [Figure 3a]. The upper end communicated with the right uterine horn, which was distended through the right cervix. Signal intensity of the contents of distended right hemi vagina and uterine horn appeared iso-intense on T1WI and hyperintense on T2WI [Figure 3b and c], with thick mucoid collection (hemicolpos and hemimetra). The right kidney was not visualized and the left kidney was marginally enlarged [Figure 4].
Figure 3.
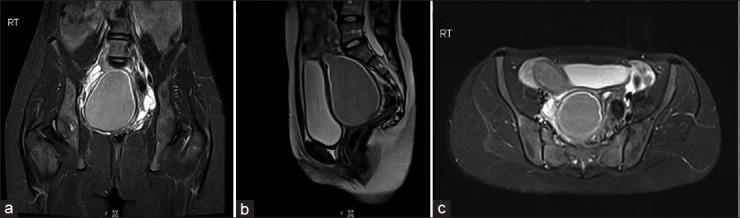
(a) MRI abdomen and pelvis, coronal T2FS showing the collection in the septated vagina extending into the cervix. (b) MRI saggital T2WI showing the collection in the septated vagina extending into the cervix. (c) MRI axial, T2FS showing the cornua of the uterus and the collection in the septated vagina
Figure 4.

Coronal T1WI reveals well-defined pelvic collection, absence of the right kidney, and slightly enlarged kidney on the left
DISCUSSION
The HWW syndrome is usually discovered at puberty with complains of dysmenorrhoea and clinically palpable mass due to the associated hematocolpos or hematometra, which result from retained, long-standing menstrual products in the obstructed vagina. Hence, a diagnosis may be delayed because menstruation is often regular in these patients, who are erroneously managed with anti-inflammatory drugs and oral-contraceptives. The potential acute complications such as pyohematocolpos, pyosalpinx, or pelvi-peritonitis, and long-term complications such as endometriosis, pelvic adhesions, and increased risk of abortion or infertility[5] may also be encountered.
Ultrasonography (US) is a very helpful tool in the diagnosis of Müllerian duct anomalies (MDA). The detection of hematocolpos at puberty, which appears as a fluid collection with low-level echoes, can make the diagnosis of genito-urinary tract anomaly (didelphic uterus) easier, although it cannot identify the type of MDA. In situations when the precise differentiation of the uterine anomaly is not achievable by means of previous examinations, MRI, due to its multiplaner and tissue characterization capability, is a suitable technique for non-invasive evaluation of female pelvic anatomy. It provides more detailed information regarding uterine morphology, the continuity with each vaginal (obstructed and non-obstructed) lumen, and nature of fluid content.[6] Although US, CT scan, and hystero-salpingography are commonly used for diagnosis because of their low cost, MRI is the most accurate method for diagnosis, and it can help patients maintain fertility by allowing the most appropriate treatment option to be used.[7]
MRI also has been more sensitive in detecting the uterine contour, the shape of the intrauterine cavity, the character of the septum, as well as the associated aspects such as endometriosis, pelvic inflammation, and adhesions. Laparoscopy is now considered to be more popular for the evaluation of female reproductive tract anomaly, although it could be reserved when the diagnosis is not clear after imaging or when MRI is not available and not performed as a routine procedure.
Surgical intervention in the form of excision of vaginal septum following a simple drainage procedure for the collection to relieve obstruction is the treatment of choice. Surgery also reduces chances of pelvic endometriosis due to retrograde menstrual seeding.
The consequences that can potentially occur due to the failure of treatment include urinary retention, hematosalpinx, endometriosis, and even rupture of the tubo-ovarian abscess.[8]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Zurawin RK, Dietrich JE, Heard MJ, Edwards CL. Didelphic uterus and obstructed hemivagina with renal agenesis: Case report and review of the literature. J Pediatr Adolesc Gynecol. 2004;17:137–41. doi: 10.1016/j.jpag.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 2.Del Vescovo R, Battisti S, Di Paola V, et al. Herlyn-Werner-Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Med Imaging. 2012;12:4. doi: 10.1186/1471-2342-12-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orazi C, Lucchetti MC, Schingo PM, Marchetti P, Ferro F. Herlyn-Werner-Wunderlich syndrome: Uterus didelphys, blind hemivagina and ipsilateral renal agenesis. Sonographic and MR findings in 11 cases. Pediatr Radiol. 2007;37:657–65. doi: 10.1007/s00247-007-0497-y. [DOI] [PubMed] [Google Scholar]
- 4.Heinonen PK. Clinical implications of the didelphic uterus: Long-term follow-up of 49 cases. Eur J Obstet Gynecol Reprod Biol. 2000;91:183–90. doi: 10.1016/s0301-2115(99)00259-6. [DOI] [PubMed] [Google Scholar]
- 5.Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Devroey P. Clinical implications of uterine malformations and hysteroscopic treatment results. Hum Reprod Update. 2001;7:161–74. doi: 10.1093/humupd/7.2.161. [DOI] [PubMed] [Google Scholar]
- 6.Rana R, Pasrija S, Puri M. Herlyn-Werner-Wunderlich syndrome with pregnancy: A rare presentation. Congenit Anom (Kyoto) 2008;48:142–3. doi: 10.1111/j.1741-4520.2008.00195.x. [DOI] [PubMed] [Google Scholar]
- 7.Tanaka YO, Kurosaki Y, Kobayashi T, Equchi N, Mori K, Satah Y, et al. Uterus didelphys associated with obstructed hemivagina and ipsilateral renal agenesis: MR findings in seven cases. Abdom Imaging. 1998;23:437–41. doi: 10.1007/s002619900375. [DOI] [PubMed] [Google Scholar]
- 8.Kiechl-Kohlendorfer U, Geley TE, Unsinn KM, Gassner I. Diagnosing neonatal female genital anomalies using saline-enhanced sonography. AJR Am J Roentgenol. 2001;177:1041–4. doi: 10.2214/ajr.177.5.1771041. [DOI] [PubMed] [Google Scholar]


