To the Editor:
The challenges posed by a modern multiethnic society have had a marked impact on current health provision. There are established inequalities in health care provision for ethnic minorities (1–3) with asthma prevalence, severity, and access to health care varying by ethnic group (4). Recently the Centers for Disease Control and Prevention recommended that improved asthma management and reduced asthma burden among children from ethnic minorities can be achieved through promoting interventions that take cultural differences and population specific characteristics into account (4). However, until recently appropriate lung function reference equations for groups other than white Europeans have been lacking, especially for younger children (5). In an attempt to address these issues, the Global Lung Function Initiative (GLI), which was established as a European Respiratory Society Taskforce, recently published the first global, all-age (3–95 yr), multiethnic reference equations for spirometry (6). Because the Quanjer GLI-2012 reference equations were derived from various studies around the world during the past 3 decades, it is important to establish the level of agreement between these equations and contemporary spirometry data. London, United Kingdom, is an ideal environment in which to validate these equations because ethnic minorities comprise 40% of the population.
The aims of this study were first, to investigate existing ethnic differences in lung function in a multiethnic population of children from London and second, to validate the GLI-2012 reference equations in this population.
As part of the Size and Lung Function in Children study (www.ucl.ac.uk/slic), anthropometry and spirometry were undertaken in primary school children within a mobile laboratory or in classrooms between December 2010 and July 2012. Children were classified into four main ethnic groups (white, black, South Asian, other/mixed) on the basis of information from parental questionnaires, child self-identification, and investigator observation. As there is currently no GLI ethnic-specific equation for South Asians (i.e., those from the Indian subcontinent), the “South East Asian equation” (derived from subjects from South China, Thailand, and Taiwan) was used for this population as it is closest geographically. Spirometry was performed using either the Jaeger Masterscreen (V5.01; Carefusion, Warzburg, Germany) or the Easy-on PC (ndd, Zurich, Switzerland) spirometer, which have been shown to produce very similar spirometry results (7). All subjects performed at least three maneuvers to standard protocol and American Thoracic Society/European Respiratory Society acceptability and repeatability criteria, adjusted for children, were applied (8, 9). Results were analyzed in two ways. First, to calculate the magnitude of ethnic differences in lung function, all spirometric data were expressed as percent predicted on the basis of the GLI-2012 equations for white subjects, which adjust for age, sex, and height (6). Second, to assess how valid the GLI-2012 equations were in this population, results from each child were expressed as ethnic-specific z-scores. If the GLI-2012 equations are appropriate for this contemporary multiethnic population, the mean (SD) z-score for each outcome in each group would be expected to approximate 0 (1) (10). Differences between groups were assessed using one way analysis of variance with Bonferroni correction for multiple comparisons. None of the data collected from the SLIC study were used in the development of the GLI-2012 equations. Some of these results have been reported in the form of an abstract (11).
Spirometry was attempted in 1,626 children aged 5–11 years from 14 London schools. Of these, 1,291 were asymptomatic and without any existing respiratory conditions or other chronic disease likely to affect lung function (335 were excluded for health reasons: airway obstruction on spirometry [14]; current asthma [172]; sickle cell disease [11]; preterm [70]; or symptomatic on the day of test [68]). Technically acceptable spirometry was obtained from 1,088/1,291 (84%) healthy children (Table 1). After adjustment for age and sex, black children were significantly taller (P < 0.001) and heavier (P < 0.001) and South Asian children were significantly lighter (P < 0.001) than white children. When compared with white children, FEV1 was significantly lower by a predicted mean (95% confidence interval) of 14% (12 to 17%) in black, 11% (9 to 14%) in South Asian, and 5% (2 to 8%) in other/mixed race children (Table 1).
TABLE 1.
GROUP CHARACTERISTICS AND LUNG FUNCTION RESULTS
| White | Black | South Asian | Other/mixed | |
|---|---|---|---|---|
| N |
359 |
340 |
226 |
163 |
| Boys, % |
47.1 |
41.2 |
48.7 |
45.4 |
| Age, yr |
8.19 (1.6) |
8.40 (1.59) |
8.13 (1.66) |
8.23 (1.62) |
| Weight z* |
0.39 (1.00) |
0.91 (0.99) |
−0.06 (1.25) |
0.36 (1.15) |
| Height z* |
0.30 (0.94) |
0.83 (0.91) |
0.12 (1.10) |
0.33 (1.01) |
| BMI z* |
0.34 (1.01) |
0.69 (1.05) |
−0.18 (1.32) |
0.26 (1.19) |
| FEV1 (z-score)† |
0.03 (0.87) |
−0.00 (0.93) |
−0.08 (0.96) |
0.19 (0.88) |
| FVC (z-score)† |
0.17 (0.85) |
0.22 (0.93) |
0.24 (0.97) |
0.42 (1.00) |
| FEV1/FVC (z-score)† |
−0.29 (0.84) |
−0.46 (0.96) |
−0.66 (0.95) |
−0.43 (0.82) |
| FEV1/FVC (z-score)‡ | −0.29 (0.84) | −0.35 (0.95) | −0.15 (0.92) | −0.23 (0.79) |
Data presented as mean (SD) unless otherwise indicated. A z-score of 0 equates to the 50th centile or 100% predicted.
According to CDC 2000 (14).
According to the Quanjer GLI-2012 ethnic specific equations (6).
According to the Quanjer GLI-2012 ethnic specific equations for white children (6). Data from South Asian children were expressed according to the “South East Asian equation.”
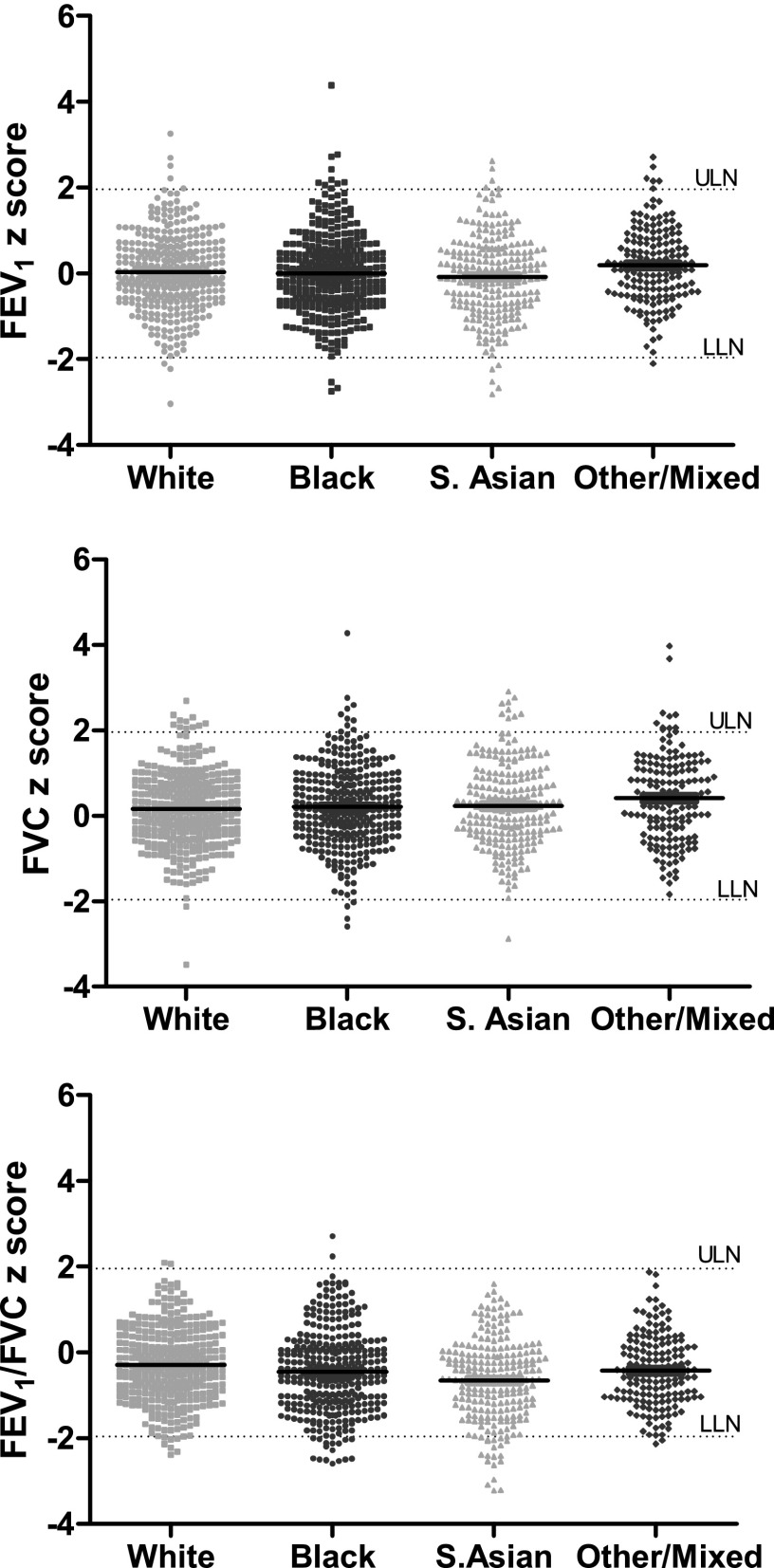
When data were expressed according to the GLI-2012 ethnic-specific reference equations, the mean (SD) FVC and FEV1 z-scores approximated 0 (1) across all groups, albeit being slightly elevated among those allocated to the “other” group in whom numbers were more limited (Figure 1, Table 1). Similarly, with the exception of the South Asian children, in whom predicted values were slightly under-estimated when applying the South East Asian equation, FEV1/FVC z-score was close to that expected from a healthy population in all groups. 95% of children in each group fell within the 95th limits of normality for FEV1 and FVC, suggesting that these outcomes can be reliably used to identify presence of lung disease irrespective of ethnic origin. Although similar results were observed for FEV1/FVC in the white or “other” groups (5.6 and 6.7% respectively falling below the 5th centile), 9.1% of black children and 13.8% South Asian healthy children fell below this lower limit of normal, when applying the ethnic-specific equations. However, if all FEV1/FVC data were expressed in relation to the white equation, close agreement was seen across all groups (Table 1, bottom row).
Figure 1.
Spirometric lung function results according to the GLI-2012 ethnic specific reference equations (6). Data from South Asian children were expressed according the “South East Asian equation.” For the purposes of this analysis the 95% limits of normality are shown.
These results demonstrate that although there are significant ethnic differences in FEV1 and FVC in primary school children, the magnitude of which is similar to that reported in older subjects (6), these differences can be minimized by using the GLI-2012 ethnic-specific reference equations. Furthermore, as reported previously (6), FEV1/FVC remained relatively constant across all ethnic groups. The results also indicate that these equations are valid for use in a multiethnic population of contemporary school children, as previously demonstrated in healthy Australasian subjects aged 4–80 years (12). The slightly lower z-score for FEV1/FVC in South Asian children despite similar absolute values, emphasizes the urgent need to develop ethnic-specific equations for this group (6). When compared with the other ethnic-specific coefficients, the South East Asian GLI equation provided the best precision when interpreting FEV1 and FVC results in children from the Indian sub-continent living in London (data not shown). However, predicted FEV1/FVC in these children is better reflected by that derived from white subjects until appropriate ethnic-specific equations can be developed for South Asian subjects. Results from children of other/mixed ethnic backgrounds must be interpreted with caution due to the limited numbers (13). Nevertheless, with the exception of FEV1/FVC in South Asian subjects when using the South East Asian equation, mean results for all outcomes in all groups were within ±0.5 z-scores; representing differences that are unlikely to be of clinical significance (6, 12). In conclusion, although further work is required to develop suitable reference equations for South Asians, and to validate equations for those of other/mixed race, use of the Quanjer GLI-2012 ethnic-specific reference equations appear to be valid in a multiethnic population of contemporary school children. This will facilitate diagnosis of respiratory conditions in children, irrespective of ethnic origin, by improved differentiation between health and disease.
Footnotes
Author Contributions: S.L., J.S., and S.S. designed the study; R.B. and J.K. performed data collection and analysis; A.W. performed the statistical analysis; all authors contributed to the manuscript and approved the final draft.
This research was funded by the Wellcome Trust and Asthma UK.
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Smith GD, Chaturvedi N, Harding S, Nazroo J, Williams R. Ethnic inequalities in health: a review of UK epidemiological evidence. Crit Public Health. 2000;10:375–408. [Google Scholar]
- 2.Burchard EG, Ziv E, Coyle N, Gomez SL, Tang H, Karter AJ, Mountain JL, Perez-Stable EJ, Sheppard D, Risch N. The importance of race and ethnic background in biomedical research and clinical practice. N Engl J Med. 2003;348:1170–1175. doi: 10.1056/NEJMsb025007. [DOI] [PubMed] [Google Scholar]
- 3.Phimister EG. Medicine and the racial divide. N Engl J Med. 2003;348:1081–1082. doi: 10.1056/NEJMp030028. [DOI] [PubMed] [Google Scholar]
- 4.Moorman J E, Zahran H, Truman BI, Molla MT. Current Asthma Prevalence: United States, 2006–2008. U.S. Department of Health and Human Services, Atlanta, GA 30333, Epidemiology and Analysis Program Office; Surveillance, Epidemiology, and Laboratory Services; Centers for Disease Control and Prevention. CDC Health Disparities and Inequalities Report - United States, 2011.Supplement/Vol.60, 84–86. 14–1-2011.
- 5.Stanojevic S, Wade A, Lum S, Stocks J. Reference equations for pulmonary function tests in preschool children: a review. Pediatr Pulmonol. 2007;42:962–972. doi: 10.1002/ppul.20691. [DOI] [PubMed] [Google Scholar]
- 6.Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver B, Enright PL, Hankinson JL, Ip MS, Zheng J, et al. Multi-ethnic reference values for spirometry for the 3–95 year age range: the global lung function 2012 equations. Eur Respir J. 2012;40:1324–1343. doi: 10.1183/09031936.00080312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonner R, Kirkby J, Lum S, Stocks J. A guide to choosing the appropriate spirometer. Inspire. 2011;11:2. [Google Scholar]
- 8.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 9.Kirkby J, Welsh L, Lum S, Fawke J, Rowell V, Thomas S, Marlow N, Stocks J. The EPICure study: comparison of pediatric spirometry in community and laboratory settings. Pediatr Pulmonol. 2008;43:1233–1241. doi: 10.1002/ppul.20950. [DOI] [PubMed] [Google Scholar]
- 10.Stanojevic S, Wade A, Stocks J. Reference values for lung function: past, present and future. Eur Respir J. 2010;36:12–19. doi: 10.1183/09031936.00143209. [DOI] [PubMed] [Google Scholar]
- 11.Lum S, Bonner R, Kirkby J, Sonnappa S, Stocks J. Validation of the GLI-2012 mulit-ethnic spirometry reference equations in London school children. Thorax. 2012;67:A18–A19. [Google Scholar]
- 12.Hall GL, Thompson BR, Stanojevic S, Abramson MJ, Beasley R, Coates A, Dent A, Eckert B, James A, Filsell S, et al. The Global Lung Initiative 2012 reference values reflect contemporary Australasian spirometry. Respirology. 2012;17:1150–1151. doi: 10.1111/j.1440-1843.2012.02232.x. [DOI] [PubMed] [Google Scholar]
- 13.Quanjer PH, Stocks J, Cole TJ, Hall GL, Stanojevic S. Influence of secular trends and sample size on reference equations for lung function tests. Eur Respir J. 2011;37:658–664. doi: 10.1183/09031936.00110010. [DOI] [PubMed] [Google Scholar]
- 14.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL. CDC growth charts: United States. Adv Data. 2000;314:1–27. [PubMed] [Google Scholar]