Abstract
Background:
Inappropriate or excessive use of topical corticosteroids can lead to cutaneous and systemic adverse effects which occur more commonly with the use of very potent steroids. Monitoring and analysis of the prescription practices of topical steroids can help to achieve rational prescription of these drugs.
Aim:
The present study was carried out to study and analyze the pattern of prescribing topical corticosteroids among outpatients attending the dermatology clinic in a rural tertiary care and teaching hospital, Ambajogai, Maharashtra.
Materials and Methods:
A cross-sectional descriptive study was conducted for a duration of two months from August 2011 to September 2011, and 500 prescriptions were randomly collected from the dermatology pharmacy and analyzed.
Results:
About 66% of the prescriptions contained four to five drugs per prescription. Topical steroids were given in 28.4% of all the prescriptions. In almost all the prescriptions, strength, quantity of the steroid to be used, frequency, site, and duration of application was not mentioned. The chief complaints and diagnoses were not mentioned in about 85% of the prescriptions for topical corticosteroids. About 94.36% of the prescriptions contained very potent steroids.
Conclusion:
Inadequate prescribing information is a clear characteristic of the dermatological prescriptions containing topical corticosteroids. Doctors should be educated about the importance of giving patients sufficient information regarding the use of steroids. There is a need to revise hospital formulary where low-potency steroids can also be included along with potent ones so that the latter can be avoided in conditions where they are unnecessary.
Keywords: Prescribing practices, topical corticosteroids, very potent steroids
Introduction
What was known?
Topical corticosteroids, which were introduced in the late 1950s, have revolutionized the practice of dermatology and they still constitute one of the largest groups of drugs used in this discipline. They are widely used in dermatological practice and more trend is seen towards usage of potent and highly potent steroids. This may lead to various side effects, related directly to such factors as the application site, duration of application, potency, and occlusion of the medication. Hence a rational use of these medications is the need of the hour.
Most of the skin diseases are chronic and require treatment for a prolonged period which holds the risk of adverse effects. Among the drugs used in dermatology are antibiotics, antifungals, scabicides, vitamins, antiallergics, keratolytics, emollients, and topical corticosteroids. Of all these, topical corticosteroids constitute the mainstay of treatment for many skin conditions.
The various indications for which topical steroids are used include psoriasis, vitiligo, eczema, atopic dermatitis, phimosis, acute radiation dermatitis, and lichen sclerosus. Prolonged, inappropriate, or excessive use of topical steroids can lead to various cutaneous and systemic adverse effects. Local adverse effects of topical steroids include skin a trophy, contact dermatitis, tachyphylaxis, striae, telangiectasia, acneiform dermatitis, and so on, whereas systemic reactions may occur in the form of hypothalamic-pituitary-adrenal suppression, Cushing's disease, and femoral head osteonecrosis.[1]
The risk of systemic effects increases based on factors like potency of the corticosteroid, the amount applied, age of the patient, use of occlusive dressings, and duration of use.[2] The potential side effects usually occur with the excessive use of more potent agents, the risk being less when low-potency steroids are used.[3] So, physicians should use the weakest possible steroid that will effectively treat the dermatological condition.
Irrational prescription of drugs is a common occurrence in clinical practice which may even occur with the use of topical corticosteroids. Misuse of topical corticosteroids is very common in patients with facial dermatoses. Many patients prefer to use topical steroids as a fairness cream.[4] To minimize adverse cutaneous and systemic reactions, especially with prolonged use, the rational use of topical steroids should include careful consideration of the patient's age, total area of application, quantity to be applied, efficacy of the selected corticosteroid, and frequency of application.[5] Hence, one step to achieve rational prescribing is periodic auditing of prescriptions.
The purpose of this study is to monitor and analyze the pattern of prescribing topical corticosteroids among outpatients attending dermatology clinics in a rural tertiary care and teaching hospital, Ambajogai, Maharashtra, India. Being a tertiary care teaching hospital situated in a rural place, most of the patients attending the clinic belong to low socioeconomic strata with a number of dermatological conditions. The significance of the current study stems from the observation that there is lack of availability of specialists in dermatology in this hospital, and so, the erratic use of medicines has been noticed. Drug utilization studies not only improve standards of medical treatment at all levels in the health-care system, but also help in the identification of problems related to drug use such as polypharmacy, drug-drug interactions, and adverse drug reactions.[6]
Materials and Methods
Permission from the Institutional Ethics Committee was taken before initiation of the study. This cross-sectional descriptive study was conducted in S.R.T.R Medical College, Ambajogai, Maharashtra, India for a duration of two months from August 2011 to September 2011.
Five hundred prescriptions were randomly collected from the drug-dispensing counter and analyzed. The prescriptions were written by dermatologists. The data collected included age, sex, symptoms, diagnosis, number of drugs, and potency of the steroid, and whether dose, duration, strength, quantity to be applied, and frequency of administration was mentioned.[7]
Results
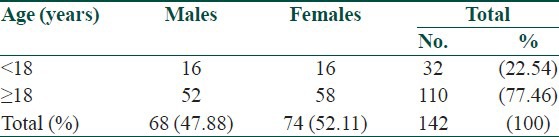
The total number of drugs prescribed in the 500 prescriptions was 2,050 with the average number of drugs per prescription being 4.1. The maximum number of drugs on a single prescription was seven and the minimum was one. For 366 patients (73.2%), ≥4 drugs were prescribed on a single prescription [Figure 1]. Injections were rarely prescribed to the patients. Majority (52.11%) of the prescriptions for topical steroids were for females. Most (77.46%) of the patients receiving them were males and females above 18 years of age [Table 1].
Figure 1.
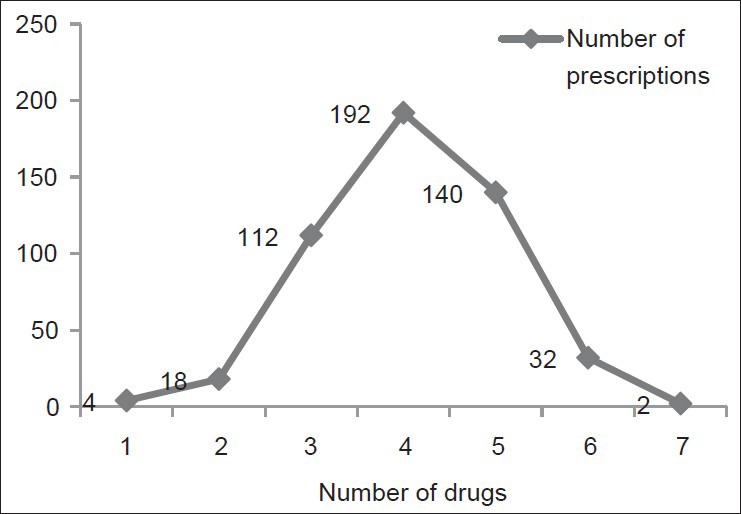
Number of drugs per prescription
Table 1.
Age and sexwise distribution of patients prescribed topical steroids (n=142)
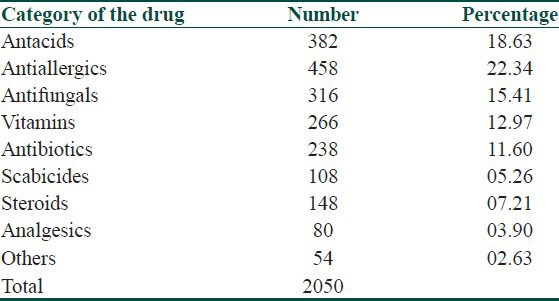
Of the 2,050 drugs, the most commonly prescribed class of drugs was antiallergics (22.34%) followed by antacids (18.63%) [Table 2]. An analysis of prescriptions showed that topical steroids were prescribed in 142 (28.4%) of all prescriptions. None of the prescriptions contained more than one topical steroid. Oral corticosteroids were prescribed to only six patients. About 132 (94.36%) of the prescriptions contained very potent steroids; fluocinolone acetonide was the most commonly used drug followed by clobetasol propionate. The chief complaints as well as diagnoses were not mentioned in about 85% of the prescriptions containing steroids. In the remaining prescriptions, steroids were prescribed for conditions like allergic/contact dermatitis and dermatophytosis.
Table 2.
Main therapeutic categories of drugs
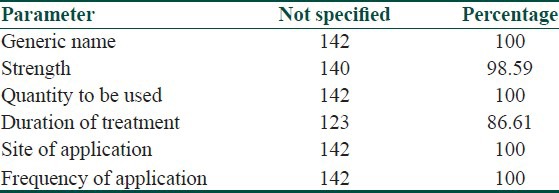
All the steroids were prescribed by brand names. In almost all the prescriptions, strength, quantity of the steroid to be used, frequency, and site of application were not mentioned. In majority (86.61%) of the prescriptions, duration of application was not mentioned [Table 3].
Table 3.
Details of information not included on prescriptions for topical corticosteroids (n=142)
Less than one-third of the steroids were given as combination products containing antimicrobials, whereas majority (88.74%) were given alone.
Discussion
Many studies have observed excessive and inappropriate use of potent topical corticosteroids. In a study carried out in India, the prescription of topical corticosteroids was studied in 200 patients attending a dermatology outpatient clinic. Potent topical corticosteroids were commonly used in 86 (43%) patients. The quantity of topical steroid was mentioned in only 4%, frequency of administration was mentioned in 77%, the site of administration in 69%, and duration of treatment in 55% of the total prescriptions.[8]
Another study conducted on the prescription of topical steroids in north Palestine showed that topical corticosteroids are commonly prescribed for outpatients attending dermatology clinics there (51.6%). The quantity of the corticosteroid to be applied was not mentioned in 87.7% of the prescriptions and duration of use not mentioned in 71.6%.[5]
In a study carried out in the United States from 1989 to 1991, it was found that dermatologists were 3.9 times more likely to prescribe very-high-potency steroids than were other physicians.[9]
The present study showed that the 500 prescriptions contained 2,050 drugs with the average number of drugs per prescription being 4.1. About 66% of the prescriptions contained four to five drugs. This reflects a trend toward polypharmacy. The complications of polypharmacy are multiple such as increased problems with side effects of medications, adverse drug reactions, drug-drug interactions, noncompliance with the medical regimen, and direct cost of drugs as well as indirect costs resulting from hospitalization for iatrogenic illnesses.[10]
Topical corticosteroids were prescribed in 28.4% of all the prescriptions. Analysis of the prescriptions showed that prescribing information about topical steroids was inadequate in majority of the prescriptions. The diagnosis and chief complaints were not mentioned in about 85% of the prescriptions in which steroids were prescribed. In these 85% prescriptions, the basis of prescribing topical steroids could not be established. There may be a possibility of prescribing these drugs for the conditions where they are not indicated which suggests irrational use. The practice of inadequate prescription writing may mislead the patient about usage of medications which may be responsible for overutilization or underutilization of steroids resulting in potential side effects or subtherapeutic response to a drug, respectively. Antiallergics were the most commonly prescribed drug class followed by antacids and antifungals. Whether very high use of these drugs was rational could not be explained because of the 500 prescriptions, complaints and diagnoses were not mentioned in about 75%. Antacids were prescribed in 76% of all prescriptions. The use of such medicines, when they are not indicated, can lead to an unnecessary burden on the health-care system.
Among the topical steroids prescribed, 94.36% belonged to very potent groups (fluocinolone, clobetasol)[11] which shows a trend toward prescribing potent steroids. The prescription of very potent steroids should be limited when possible. Long and excessive use may carry the risk of suppression of the hypothalamic-pituitary-adrenal axis as well as local adverse effects.[12] This pattern of prescription may be influenced by the availability of the preparation in the hospital pharmacy and the choice of the dermatologist. The hospital authorities should make provisions for making low-potency steroids available in the hospital pharmacy taking into consideration the adverse effects of potent steroids. In this study, none of the topical steroids was prescribed by their generic names. Using brand names for prescribing may sometimes create dispensing errors. Drugs with similar brand names but different ingredients might mistakenly be switched.[5] Moreover, prescribing drugs by their generic names could reduce the cost and thus increase prescription compliance.
Incomplete prescription of topical steroids will either limit their clinical benefit or may predispose the patient to potential side effects. To achieve maximum effectiveness, patients must be encouraged to apply these agents appropriately. Physicians and dermatologists must be aware of giving proper advice to the patients about the amount of topical steroid to be applied on different parts of the body. Use of the fingertip unit (FTU) method can be a simple tool to help doctors and patients obtain a better understanding of the amount of topical steroid to be used.[13]
In this study, some irrational combinations of topical corticosteroids were also observed. Prescribing steroids along with antifungal drugs in fungal infections can decrease the effectiveness of antifungal agents. The grave consequences of excessive and irrelevant use of topical corticosteroids were explained to the dermatologists. The same study can be repeated to evaluate any improvement after creating awareness about the rational prescription of topical corticosteroids. There is a need to revise hospital formulary where low-potency steroids can also be included along with potent ones so that the latter can be avoided in conditions where they are unnecessary. There is a need to put more emphasis on rational and complete prescription of topical steroids. The medical community should prescribe with a social perspective in mind and should stay away from practices which will be detrimental to the society at large. Continuing medical education for residents in the dermatology department is also greatly needed. The FTU method provides guidelines as to the amount of ointment needed in adults and children based on specific anatomic areas. The use of FTU should be promoted worldwide to reduce the variations in the use of topical corticosteroids and to encourage adherence to therapy.[14] Periodic evaluation of drug utilization pattern needs to be done to enable suitable modification in the prescription of drugs to increase the therapeutic benefit and decrease the adverse effects.
What is new?
In this study, the prescribing trend is more towards the potent and highly potent steroids. This could be attributed towards the availability of only these medications in the hospital pharmacy. But the prescription practices of the dermatologist cannot be overlooked. Hence this study was conducted to study the prescription and drug utilization practices in the dermatology outpatient department at our hospital, which is a rural tertiary care teaching hospital.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Fisher DA. Adverse effects of topical corticosteroid use. West J Med. 1995;162:123–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Hengge UR, Ruzicka T, Schwartz RA, Cork MJ. Adverse effects of topical glucocorticosteroids. J Am Acad Dermatol. 2006;54:1–15. doi: 10.1016/j.jaad.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 3.Topical corticosteroids. London: BMJ Publishing Group RPS Publishing; 2006. British Medical Association and Royal Pharmaceutical Society of Great Britain. British National Formulary 52. Section 13.4. [Google Scholar]
- 4.Saraswat A, Lahiri K, Chatterjee M, Barua S, Coondoo A, Mittal A, et al. Topical corticosteroid abuse on the face: A prospective, multicenter study of dermatology outpatients. Indian J Dermatol Venereol Leprol. 2011;77:160–6. doi: 10.4103/0378-6323.77455. [DOI] [PubMed] [Google Scholar]
- 5.Sweileh WM. Audit of prescribing practices of topical corticosteroids in outpatient dermatology clinics in north Palestine. East Mediterr Health J. 2006;12:161–9. [PubMed] [Google Scholar]
- 6.Cork MJ, Timmins J, Holden C, Carr J, Berry V, Tazi Ahnini R, et al. An audit of adverse drug reactions to aqueous cream in children with atopic aczema. The Pharmaceutical Journal. 2003;271:747–8. [Google Scholar]
- 7.Thawani VR, Motghare VM, Dani AD, Shelgaonkar SD. Therapeutic audit of dermatological prescriptions. Indian J Dermatol. 1995;40:13–8. [Google Scholar]
- 8.Uppal R, Sharma SC, Bhowmik SR, Sharma PL, Kaur S. Topical corticosteroids usage in dermatology. Int J Clin Pharmacol Toxicol. 1991;29:48–50. [PubMed] [Google Scholar]
- 9.Stern RS. The pattern of topical corticosteroid prescribing in the United States, 1989-1991. J Am Acad Dermatol. 1996;35(2 Pt 1):183–6. doi: 10.1016/s0190-9622(96)90319-9. [DOI] [PubMed] [Google Scholar]
- 10.Colley CA, Lucas LM. Polypharmacy: The cure becomes the disease. J Gen Intern Med. 1993;8:278–83. doi: 10.1007/BF02600099. [DOI] [PubMed] [Google Scholar]
- 11.Motghare V, Thawani V, Parate SM. Topical use of corticosteroids in dermatology. Indian J Dermatol. 1995;40:159–62. [Google Scholar]
- 12.Walsh P, Aeling JL, Huff L, Weston WL. Hypothalamus-pituitary-adrenal axis suppression by superpotent topical steroids. J Am Acad Dermatol. 1993;29:501–3. doi: 10.1016/s0190-9622(08)82011-7. [DOI] [PubMed] [Google Scholar]
- 13.Long CC, Finley AY. The finger-tip unit: A new practical measure. Clin Exp Dermatol. 1991;16:444–7. doi: 10.1111/j.1365-2230.1991.tb01232.x. [DOI] [PubMed] [Google Scholar]
- 14.Rathi SK, DSouza P. Rational and ethical use of topical corticosteroids based on safety and efficacy. Indian J Dermatol. 2012;57:251–9. doi: 10.4103/0019-5154.97655. [DOI] [PMC free article] [PubMed] [Google Scholar]


