Abstract
In the bewildering array of scientific nomenclature in the medical field, it is important to use correct terminology, know their aberrations and the reason behind a specific terminology. This paper is an attempt towards compiling all the pseudo-nomenclatures coined in dermatology, in order to make it easier to retain and recollect these pseudo names, signs, morphology, diseases, and conditions. It is also imperative to know the true entities that these pseudo names masquerade as, so as to understand the explanation for assigning the term ‘pseudo’ to these conditions. A total of 52 pseudo-terms have been compiled here in reference to dermatology. Most of these pseudo-nomenclatures were coined due to some clinical or histopathological resemblance to the true conditions, while some were premature conclusions drawn from a flawed understanding of the basic nature of the condition. Clear understanding of each of these terms and the explanation behind them being pseudo will enable a dermatologist to avoid misdiagnosis and needless confusion.
Keywords: Pseudo epitheliomatous hyperplasia, pseudo scleroderma, pseudo-Nikolskiy's sign
Introduction
What was known?
There is a vast array of pseudo-names that has been in use in dermatology literature and it is important to know the correct etiology behind this specific nomenclature.
William Shakespeare famously said, “What's in a name? That which we call a rose, by any other name would smell as sweet?” However, this is certainly not the case in the clinical field, and it is important to know the correct terminology, their aberrations, and the etiology behind their specific nomenclature in dermatology. This page is an attempt towards compiling all the pseudo-nomenclatures coined in dermatology, in order to make it easier to retain and recollect these bewildering arrays of pseudo names, signs, morphology, diseases, and conditions. It is also imperative to know the true entities that these pseudo names masquerade as, so as to understand the explanation for assigning the term ‘pseudo’ to these conditions.
Pseudo-signs in Dermatology
Pseudo-Nikolskiy's sign: Seen in Steven Johnson syndrome, toxic epidermal necrolysis and in some cases of burns and bullous icthyosiform erythroderma. The underlying mechanism here is the necrosis of epidermal cells and not acantholysis, as seen in true Nikolskiy's sign. It is elicited the same way as the true sign. However, unlike Nikolskiy's sign, pseudo-Nikolskiy's sign is elicited only on clinically involved or erythematous areas[1] [1].
Pseudo-isomorphic phenomenon: Spread of cutaneous infection along the line of trauma. E.g. warts, molluscum contagiosum.[2] The true isomorphic phenomenon of Koebner is the development of isomorphic pathologic lesions along the line of trauma, seen in dermatological diseases like lichen planus, psoriasis [Figure 2].
Pseudo-Darier sign: Seen in smooth muscle hamartoma. Stroking induces transient induration with piloerection, which is called ‘pseudo-Darier sign.’[3] True Darier sign refers to the urtication and erythematous halo that are produced in response to rubbing and scratching of lesions of cutaneous mastocytosis [Figure 3].
Pseudo sign of Lesar Trelat: Inflammation of seborrheic keratosis caused by cytarabine: A pseudo sign of Leser-Trelat.[4] True Leser-Trelat sign refers to multiple eruptive seborrheic keratosis, in the context of an internal malignancy [Figure 4].
Pseudo stellate scar: Stellate pseudoscars are white, irregular, or star-shaped atrophic scars on light exposed skin, seen in elderly individuals. These pseudoscars are secondary to mild trauma and mostly proceeded by hemorrhage into the dermis. They are also seen after prolonged use of topical steroids.[5]
Pseudo rhagades: Seen in erythropoetic protoporphyria (EPP). These are shallow elliptical or linear peri-oral furrowing seen in children with EPP.[6] True rhagades are linear peri-oral scars seen in congenital syphilis [Figure 5].
Figure 1.
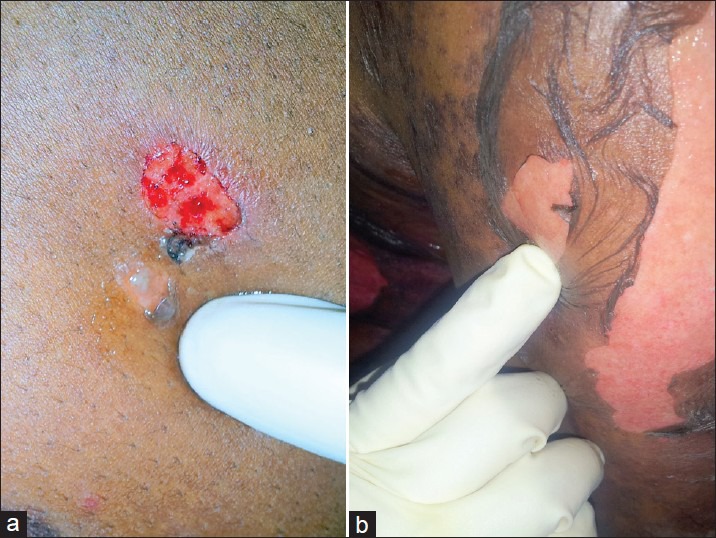
(a) Positive Nikolskiy's sign elicited in peri-lesional skin of pemphigus vulgaris. (b) Pseudo-Nikolskiy's sign seen in a patient of toxic epidermal necrolysis
Figure 2.

True isomorphic phenomenon of Koebner, seen in lichen planus
Figure 3.
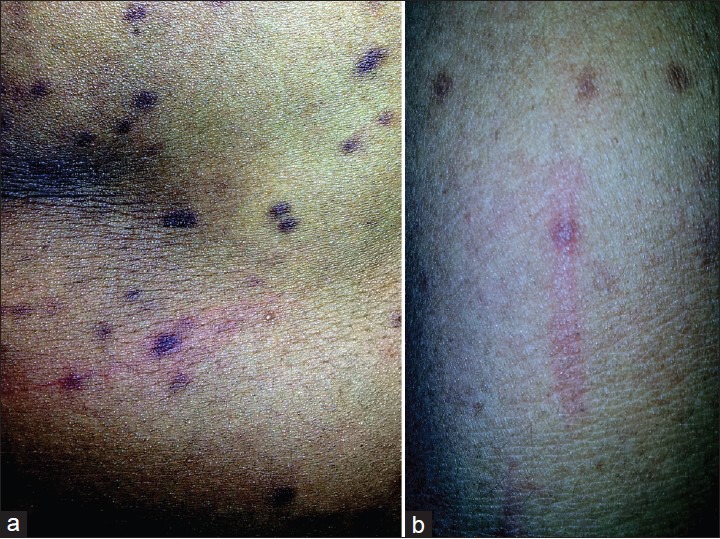
(a and b) Positive Darier sign in urticaria pigmentosa
Figure 4.

True lesar trelat sign seen in a patient of adenocarcinoma stomach
Figure 5.

Pseudo-rhagades seen in peri-oral skin in a patient of porphyria
Pseudo Terminology in Dermato–pharmacology
Pseudo-Thalidomide syndrome: Robert's syndrome, also known as pseudo-thalidomide syndrome, is characterized by cranio-facial abnormalities, tetra-phocomelia, growth retardation, sparse silvery blonde hair, and a mid-facial capillary vascular malformation extending from the forehead to the philtrum.[7] True thalidomide syndrome is a teratogenic outcome of thalidomide used during pregnancy, where the newborn has multiple birth defects, especially phocomelia.
Pseudo-catalase: Is an analog of normal human catalase. Catalase is an enzyme normally found in skin that decreases damage from free radicals. Pseudo-catalase is used in combination with narrow band UBV for the treatment of vitiligo.[8]
Pseudo-membranous colitis: Topical or systemic use of clindamycin in acne vulgaris can cause pseudo-membranous colitis as a serious adverse effect of the drug and is characterized clinically by abdominal cramp and diarrhea. Sigmoidoscopy shows pseudomembrane on the mucosa of the colon or rectum.[9]
Pseudotumor cerebri: Several medications used in dermatology, especially in acne vulgaris e.g. isotretinoin, minocycline, doxycycline, tetracycline, can cause pseudo-tumor cerebri. It is a syndrome of benign intra-cranial hypertension, characterized by headache and visual disturbances due to papilledema.[10]
Pseudo-morphological Appearances
Pseudo-vesiculations: Seen in cutaneous lesions of Sweet syndrome. They appear as single or multiple, tender, red, or purple-red papules or nodules. The pronounced edema in the upper dermis of the lesions results in their transparent, vesicle-like appearance, giving an illusion of vesiculation[11] [Figure 6].
Pseudo-tumors: Seen in classical type of Ehlers-Danlos syndrome. They are blue-grey, spongy, molluscoid pseudo-tumors, due to accumulation of connective tissue and are especially seen in scars or pressure points.[12]
Pseudo-verrucous papules/nodules: Pseudo-verrucous papules and nodules occur in the diaper and perineal areas in patients, of any age, with a predisposition to prolonged wetness. Children who wear diapers due to chronic urinary incontinence are prone to this type of dermatitis.[13]
Pseudocyst: Pseudocyst of the auricle is a non-inflammatory, fluid-filled cavity within the ear cartilage, due to habit twisting of the ear or rubbing in atopic eczema. It is called a pseudocyst because the walls of the cavity do not have a true epithelial lining but contains eosinophilic amorphous material.[14]
Pseudohyphae: Pseudohyphae are morphological forms of Candida albicans. C. albicans has the ability to grow in a variety of morphological forms ranging from unicellular budding yeast to true hyphae with parallel-sided walls. In between these two extremes, the fungus can exhibit a variety of growth forms that are collectively referred to as pseudohyphae. In this form, the daughter elongates and forms septum but remains attached to the mother cell and appears filamentous, resembling hyphae[15] [Figure 7].
Pseudo-epitheliomatous micaceous and keratotic balanitis: Pseudo-epitheliomatous micaceous and keratotic balanitis is a rare penile condition, which presents as thick, scaly, micaceous patches on the glans penis in older, uncircumscribed men. Histological examination shows hyperkeratosis, acanthosis, elongation of rete ridges and mild lower epidermal dysplasia and non-specific dermal inflammatory infiltrates. Some consider PEMKB, a locally invasive verrucous carcinoma[16] Figure 8.
Pseudo-membranous candidiasis: Is a type of oral candidiasis, characterized by curdy white patches covered by a pseudo-membrane over the gums, teeth, cheeks, and palate. The membrane consists of desquamated epithelial cells, fibrin, leukocytes, food debris, and fungal mycelia. On removal, the membrane reveals an erythematous base.[17]
Figure 6.

Pseudo-vesiculations seen in a patient of Sweet syndrome
Figure 7.
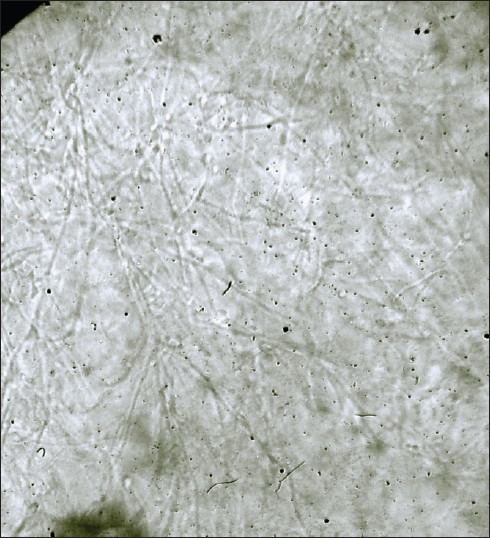
Light microscopic view (×10) showing branching pseudohyphae in a KOH mounted slide of vaginal discharge from a patient of vulvovaginal candidiasis
Figure 8.

Pseudo-epitheliomatous micaceous and keratotic balanitis
Pseudo-histopathological terms
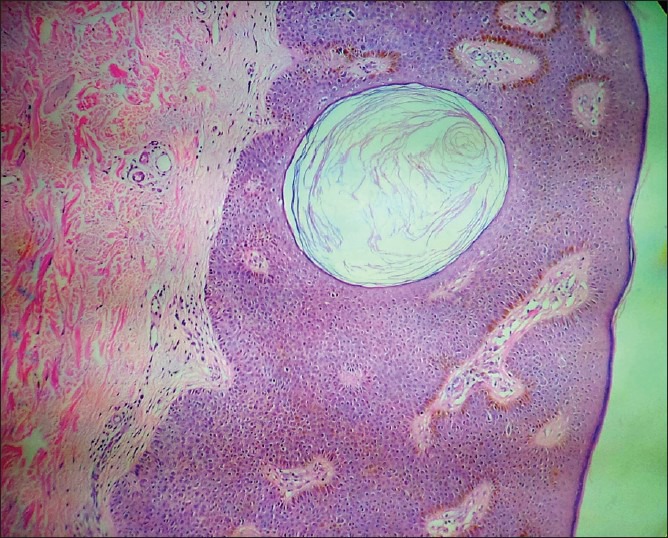
Pseudo-epitheliomatous hyperplasia: Also known as pseudo-carcinomatous hyperplasia, it refers to irregular and asymmetrical invasive epidermal proliferation as a response to a dermal disturbance, where the prickle cells grow down into the dermis. The columns may be penetrated by inflammatory cells, a feature not seen in malignant proliferation, and individual cells do not show atypical features suggestive of malignancy. This is seen at the margin of chronic ulcers, over chronic cutaneous granulomas like lupus vulgaris, tuberculosis verrucosa cutis, or hypertrophic lichen planus etc., ‘Pseudo’ tag is given to differentiate it from carcinomatous lesions[18] [Figure 9].
Pseudo-horn cyst: Pseudo-horn cyst is a hallmark histopathological finding seen in seborrheic keratosis. These are interwoven tracts of epithelial cells surrounding islands of connective tissue, in the greatly thickened epidermis. These horny invaginations on cross section appear as pseudo-horn cyst. In addition, there are also true horn cysts, which, like pseudo-horn cyst, show sudden and complete keratinization with a very thin granular layer[19] [Figure 10].
Pseudo-lyphoma: Cutaneous pseudo-lymphoma is a term used to describe inflammatory skin diseases that bear a clinical and histopathological resemblance to lymphomas but lack their malignant potential. The relevant entities that are included in this group are cutaneous lymphoid hyperplasia, Kimura disease, angiolymphoid hyperplasia with eosinophilia, Castleman disease, pseudo-mycosis fungoides, lymphomatoid contact dermatitis, Jessner's lymphocytic infiltration of skin.[20]
Pseudo-sarcoma: Atypical fibroxanthoma of skin is also known as pseudo-sarcoma of skin. The clinical course is benign, despite the highly anaplastic histological appearance. They arise as ulcerated or fleshy nodules on the sun-exposed skin of elderly people. Histopathologically, they are composed of large spindle-shaped, multinucleated pleomorphic cells, resembling a highly malignant soft tissue sarcoma.[21]
Pseudo-mycosis fungoides: This is a pseudo T-cell lymphoma, mimicking mycosis fungoides. Typical band-like or mycosis-fungoides like histopathological patterns arises spontaneously or as a T-cell infiltrate co-existing with B-cell chronic lymphocytic leukemia, or in association with drugs like anti-epileptics, imatinib mesylate, anti-histaminics etc.[22]
Pseudo-melanoma: Also known as traumatically activated naevus. Partial removal of melanocytic naevus results in proliferation of residual naevus cells, giving rise to a pathological picture like an early melanoma.[23]
Pseudo-pyogenic reaction: In histopathology of early idiopathic nodular panniculitis, the fat lobules in hypodermis are infiltrated with acute inflammatory cells, producing a pseudo-pyogenic reaction.[24]
Figure 9.
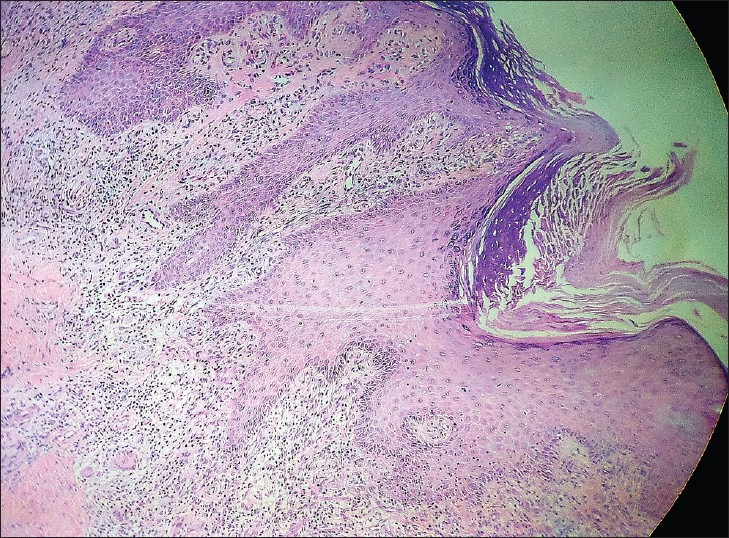
(H and E, ×10) view of tuberculosis verrucosa cutis showing pseudo-epitheliomatous hyperplasia i.e., irregular, asymmetrical invasive epidermal proliferation into dermis. (Courtesy: Dr. Asha Kubba, Delhi Dermapath Laboratory, New Delhi.)
Figure 10.
(H and E, ×10) view of seborrheic keratosis showing a distinct pseudohorncyst in the thickened epidermis. (Courtesy: Dr. Asha Kubba, Delhi Dermapath Laboratory, New Delhi.)
Pseudo-conditions/diseases
Pseudo folliculitis: Inflammatory papules resulting from re-entry of sharp tips of cut hair into the skin. Pseudo-folliculitis usually affects the beard area, when it is known as pseudo-folliculitis barbae. It is known as pseudo-folliculitis not only because it is clinically confused with folliculitis but also because a pseudo-follicle forms as the in-growing beveled hair tip proceeds into the dermis and epithelial cells downgrow in an attempt to ensheath it[25] [Figure 11].
Pseudo vasculitis: Necrotizing lesions from injected drug usually develop on the neck or extremity as a warm, firm, tender mass that can be misdiagnosed as abscess. In cocaine addicts, pseudo-vasculitis with extensive nasal destruction, as well as oropharyngeal and cutaneous ulcers, may be misdiagnosed as Wegener granulomatosis.[26]
Pseudo-xanthoma elasticum: Pseudo-xanthoma elasticum is an inherited disorder characterized by generalized fragmentation and progressive mineralization of the elastic fibers in various tissues, involving the dermis (in flexural sites), eye (angioid streak and retinal defects), and cardiovascular system (hypertension and vascular disease). Cutaneous lesions are small, yellowish papules occur in a linear or reticular pattern, commonly involving areas like the sides of neck, axillae, groins, and perineum[27] [Figure 12].
Pseudo-pseudoxanthoma elasticum: It is a penicillamine-induced degenerative dermatosis, histopathologically characterized by abnormal elastic fibers in the dermis. Clinically, the patient develops multiple small yellowish papules on both sides of neck mimicking pseudo-xanthoma elasticum, after long term therapy with D-penicillamine.[28]
Pseudo pelade of Brocq: Slowly progressive scarring alopecia of unknown cause clinically characterized by smooth, atrophic, small patches of scalp or beard alopecia, devoid of any signs of folliculitis or marked inflammation. Patches of alopecia may resemble ‘footprint in the snow’ on parting the scalp hair. Histopathologically marked by absence of inflammation except lymphocytic infiltrates and presence of prominent perifollicular fibrosis[29] [Figure 13].
Pseudo-acne : Acneiform red papules along transverse nasal crease in preadolescent individuals. They are basically keratin granulomas derived from ruptured and inflamed milia. Due to their clinical similarity to acne, they have been named pseudo-acne.[30]
Pseudo-cowpox: Milker's nodule is otherwise known as pseudo-cowpox. It is a paravaccinia (parapox) virus infection seen in individuals in close contact with cattle, like milkers, veterinarians, and workers in meat industry. Cutaneous lesions can be one or several papulovesicles to bluish nodules, which may rupture to form ulcers with eschar. Cowpox is caused by the cowpox virus (orthopox).[31]
Pseudo-eccrine chromhidrosis: This refers to the development of colored sweat when surface compounds or molecules mix with sweat to produce pigment e.g. the formation of blue sweat in copper workers. Extrinsic dyes, paints, fungi, and chromogenic bacteria are other causes of pseudo-eccrine chromhidrosis.[32]
Pseudo-ainhum: Ainhum is the autoamputation of a digit, due to development of constricting bands around bilateral fifth toes, seen in underdeveloped countries of Africa. In the remainder of the world, constricting bands that mimic ainhum are termed pseudo-ainhum. Causes of pseudo-ainhum are amniotic bands, constrictions associated with keratotic disorders, infections, and trauma.[33]
Pseudo-paralysis of Parrot: Originally described by Parrot, this pseudo-paralysis represents decreased movement of the extremity secondary to painful syphilitic periostitis.[34]
Pseudo-anaphylactic reaction: Pseudo-anaphylactic reaction or anaphylactoid reactions are a type of anaphylaxis that does not involve an allergic reaction. Non-immunologic mechanism causes de-granulation of mast cells and basophils. e.g., Hoigne's syndrome or pseudo-anaphylactic reaction to procaine penicillin G.[35]
Pseudo-syndactyly: Pseudo-syndactyly is seen in dystrophic epidermolysis bullosa, autosomal-recessive forms, where repeated blistering with progressive scarring causes fusion of adjacent fingers and toes, thus giving rise to pseudo-syndactyly. True syndactyly is a congenital malformation, where there is failure of differentiation, in which the fingers fail to separate into individual appendages.[36,37]
Pseudo-scleroderma: Pseudo-scleroderma refers to sclerosis of skin in conditions other than morphea or systemic sclerosis. This is seen in eosinophilic fasciitis, dermatomyositis, systemic lupus erythematosus, porphyria cutanea tarda, phenylketonuria, paraproteinemia etc.[38] [Figure 14].
Pseudo-porphyria: The term pseudo-porphyria describes a bullous, photosensitive cutaneous condition that clinically mimics porphyria cutanea tarda in adults and erythropoietic protoporphyria in children, but lacks biochemical abnormalities pertaining to porphyrin metabolism. Pseudo-porphyria is frequently linked to ingestion of drugs like non-steroidal anti-inflammatory drugs, chloroquine, phenobarbital etc.[39]
Pseudo-bubo: Seen in Donovanosis. Sub-cutaneous swellings in inguinal areas, which may break down to form typical granulomas, are known as pseudo-bubos since there is no lymphadenitis on microscopic examination.[40] True bubo refers to the tender inguinal lymphadenopathy seen in chancroid and secondary stage of lymphogranuloma venereum.
Pseudo-granuloma inguinale: It is a clinical variant of chancroid resembling granuloma inguinale (Donovanosis). Selective culture media isolates Hemophilus ducreyi from the penile ulcer, which clinically looks like granuloma inguinale.[41]
Pseudo-acanthosis nigricans: Pseudo-acanthosis is a type of acanthosis nigricans that is seen in obese persons and is reversible on weight reduction[42] [Figure 15].
Pseudo-chancre redux: This term is used to describe a solitary gumma of the penis at the site of the original chancre.[43]
Pseudo-monilethrix: It is a hair shaft abnormality, where the hair shaft shows irregular, flattened, expanded areas that have an indented appearance, unlike monilethrix where the hair shafts have beaded appearance because of alternate zones of spindle-like thickening and thinning, placed at a regular intervals.[44]
Pseudo-Kaposi sarcoma: Acroangiodermatitis of Mali is also known as pseudo-Kaposi sarcoma. It is a pigmented, purpuric eruption that occurs around the malleolae and in the skin of dorsal forefoot (particularly the base of second toe). The lesions are brown to plum red plaques, resembling Kaposi's sarcoma clinically, hence the name.[45]
Pseudo-allergic reaction: The reaction is not substance-specific, and similar reactions may occur to unrelated compounds in the same individual, due to inhibition of cyclo-oxygenase pathway of arachidonic acid metabolism and reduction of PGE2, which is inhibitory for mast cell de-granulation. The severity of the reaction is related to the dose of the offending substance. These reactions are called pseudo-allergic because the inflammatory mediators are released by a non-immune mechanism.[46]
Pseudo-rheumatoid nodule: Sub-cutaneous granuloma annulare is otherwise known as pseudo-rheumatoid nodule, because of their clinical resemblance to rheumatoid nodule. Lesions are nodular and predominantly occur on the scalp and pretibial regions.[47]
Pseudo-ochronosis: Bluish-black macular pigmentation seen on the upper extremities of jewelry workers. Histopathologically, it is seen as localized argyria. The pigmentation simulates the typical pigmentation seen in endogenous ochronosis (alkaptonuria).[48]
Pseudo-pyogenic granuloma: Angiolymphoid hyperplasia with eosinophilia is also known as pseudo-pyogenic granuloma. It is a reactive proliferative disorder of blood vessels with a variable component of inflammatory cells. Histopathologically, there are circumscribed collection of vessels whose endothelial cells are epitheloid and have abundant eosinophilic cytoplasm and large nuclei.[49]
Pseudo-nits: Peipilar keratin casts or hair casts or pseudo-nits are thin, elongated, firm, cylindrical concretions that encircle the hair shafts and can be easily dislodged, unlike true nits, which are oval, glistening, translucent, whitish lidded capsule attached to the side of the hair shaft by a firm chitinous sheath.[50]
Pseudo-pemphigoid: Topical drug-induced cicatricial conuctivitis is known as pseudo-pemphigoid. Signs and symptoms are similar as with ocular cicatricial pemphigoid; therefore, immunohistologic evaluation of biopsied tissue is needed to confirm the diagnosis.[51]
Pseudo-mycosis: Botryomycosis is otherwise known as pseudo-mycosis. Cutaneous botryomycosis resembles a fungal infection but is actually a chronic, inflammatory response to bacterial infection. Staphylococcus aureus is the most commonly implicated bacteria, followed by Pseudomonas aeruginosa.[52]
Pseudo-elephantiasis: Pseudo-elephantiasis is a condition, caused due to inflammation, edema or obstruction of lymphatics, triggered by non-filarial infections like donovanosis, lymphogranuloma venereum, syphilis, tuberculosis.[53]
Figure 11.

Pseudo-folliculitis seen in beard area (also known as pseudo folliculitis barbae)
Figure 12.

Small yellowish papules in linear pattern seen in neck folds of a patient of pseudo-xanthoma elasticum
Figure 13.
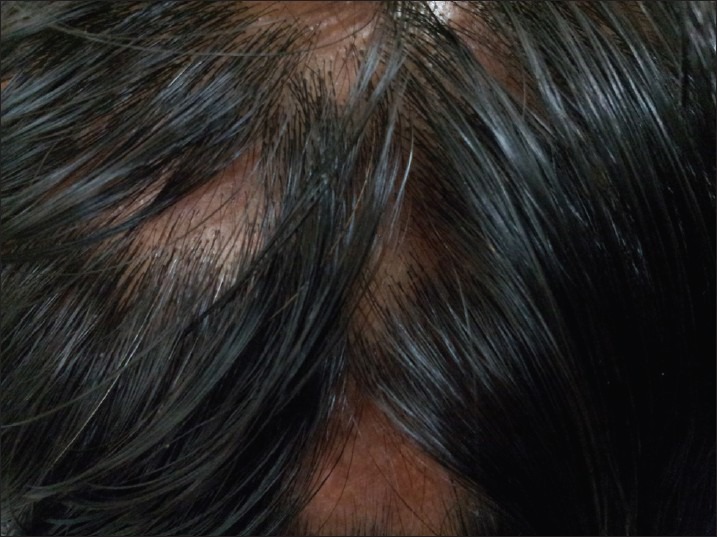
“Footprints in the snow” appearance, seen in pseudopelade of Brocq
Figure 14.

(a) Scleroderma seen in a patient of systemic sclerosis with ‘salt and pepper’ pigmentation. (b) Pseudo-scleroderma seen in a patient of eosinophilic fasciitis
Figure 15.

Pseudo-acanthosis seen in posterior nuchal fold in an obese female
Conclusion
This is a comprehensive compilation of the pseudo-terminologies that one frequently and infrequently comes across during the learning years, as well as practice of dermatology. Most of these pseudo-nomenclatures were coined due to some clinical or histopathological resemblance to the true conditions that they are named after, while some were premature conclusions drawn from a flawed understanding of the basic nature of the condition. Clear understanding of each of these terms, and the explanation behind them being pseudo, will enable a dermatologist to avoid misdiagnosing these pseudo conditions to avoid needless confusion.
What is new?
An exhaustive compilation of all pseudo terminologies in dermatology, categorized under pseudo-signs, pseudo terms in dermato-pharmacology, pseudo-morphology, pseudo-histopathology and pseudo-diseases.
Acknowledgment
I would like to acknowledge Dr. Asha Kubba's (Consultant Dermatopathologist, Delhi Dermatopath laboratory, New Delhi) contribution for providing the histopathological images for Figures 9 and 10.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Valia AR, Ramesh V, Jerajani HR, Fernandez RJ. Blistering Disorders. In: Valia RG, Valia AR, editors. IADVL Textbook of dermatology. 3rd ed. Mumbai: Bhalani Publishing House; 2001. pp. 1087–152. [Google Scholar]
- 2.Boyd AS, Nelder KH. The isomorphic response of Koebner. Int J Dermatol. 1990;29:401–10. doi: 10.1111/j.1365-4362.1990.tb03821.x. [DOI] [PubMed] [Google Scholar]
- 3.Stokes JH. Nevus pilaris with hyperplasia of non striated muscle. Arch Dermatol Syphil. 1923;7:479. [Google Scholar]
- 4.Patton T, Zirwas M, Nieland-Fisher N, Jukic D. Inflammation of seborrheic keratoses caused by cytarabine: A pseudo sign of Leser-Trelat. J Drugs Dermatol. 2004;3:565–6. [PubMed] [Google Scholar]
- 5.Colomb D. Stellate spontaneous pseudoscars. Senile and presenile forms: Especially those forms caused by prolonged corticoid therapy. Arch Dermatol. 1972;105:551–4. doi: 10.1001/archderm.105.4.551. [DOI] [PubMed] [Google Scholar]
- 6.Lim HW, Murphy GM. The porphyrias. Clin Dermatol. 1996;14:375–87. doi: 10.1016/0738-081x(96)00067-3. [DOI] [PubMed] [Google Scholar]
- 7.Romke C, Froster-Iskenius U, Heyne K, Hohn W, Hof M, Grzejszczk G, et al. Roberts syndrome and SC phocomelia. A single genetic study. Clin Genet. 1987;31:170–7. doi: 10.1111/j.1399-0004.1987.tb02790.x. [DOI] [PubMed] [Google Scholar]
- 8.Taïeb A, Picardo M. Clinical practice. Vitiligo. N Engl J Med. 2009;8:160–9. doi: 10.1056/NEJMcp0804388. [DOI] [PubMed] [Google Scholar]
- 9.Milstone EB, McDonald AJ, Scholhamer CF., Jr Pseudomembranous colitis after topical application of clindamycin. Arch Dermatol. 1981;117:154–5. [PubMed] [Google Scholar]
- 10.Friedman DI. Medication–induced intracranial hypertension in dermatology. Am J Clin Dermatol. 2005;6:29–37. doi: 10.2165/00128071-200506010-00004. [DOI] [PubMed] [Google Scholar]
- 11.Sweet RD. An acute febrile neutrophilic dermatosis. Br J Dermatol. 1964;76:349. doi: 10.1111/j.1365-2133.1964.tb14541.x. [DOI] [PubMed] [Google Scholar]
- 12.Burrows NP, Lovel CR. Disorders of Connective Tissue. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. Sussex: Wiley-Blackwell; 2010. p. 4532. [Google Scholar]
- 13.Chang MW, Orlow SJ. Neonatal, Pediatric, and Adolescent Dermatology. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's Dermatology in general medicine. 7th ed. New York: McGraw-Hill; 2008. p. 943. [Google Scholar]
- 14.Grabski WJ, Salasche SJ, McCollough ML, Angeloni VL. Pseudocyst of the auricle associated with trauma. Arch Dermatol. 1989;125:528–30. [PubMed] [Google Scholar]
- 15.Berman J, Sudbery PE. Candida albicans: A molecular revolution built on lessons from budding yeast. Nat Rev Genet. 2002;3:918–30. doi: 10.1038/nrg948. [DOI] [PubMed] [Google Scholar]
- 16.Ganem JP, Steele BW, Creager AJ, Carson CC. Pseudo-epitheliomatous keratotic and micaceous balanitis. J Urol. 1999;161:217–8. [PubMed] [Google Scholar]
- 17.Hay RJ, Roberts SO, Mackenzie DW. Mycology. In: Champion RH, Burton JL, Ebling FJ, editors. Textbook of dermatology. Oxford: Blackwell Scientific Publications; 1992. p. 1128. [Google Scholar]
- 18.Winer LH. Pseudoepitheliomatous hyperplasia. Arch Dermatol Syphilol. 1940;42:856–7. [Google Scholar]
- 19.Sanderson KF. The structure of seborrheic keratoses. Br J Dermatol. 1986;80:588. doi: 10.1111/j.1365-2133.1968.tb12357.x. [DOI] [PubMed] [Google Scholar]
- 20.Wood GS. Inflammatory diseases that simulate Lymphomas: Cutaneous pseudolymphomas. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's Dermatology in general medicine. 7th ed. New York: McGraw-Hill; 2008. p. 943. [Google Scholar]
- 21.Dahl I. Atypical fibroxanthoma of the skin: A clinico-pathological study of 57 cases. Acta Pathol Microbiol Scand. 976;84:183–97. [PubMed] [Google Scholar]
- 22.Ploysangam T, Breneman DL, Mutasim DF. Cutaneous pseudolymphomas. J Am Acad Dermatol. 1998;38:877. doi: 10.1016/s0190-9622(98)70154-9. [DOI] [PubMed] [Google Scholar]
- 23.Bishop JA. Lentigos, Melanocytic Naevi and Melanoma. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. Sussex: Wiley-Blackwell; 2010. p. 5419. [Google Scholar]
- 24.Eng AM, Aronson IK. Dermatopathology of panniculitis. Semin Dermatol. 1984;3:1–13. [Google Scholar]
- 25.Strauss JS, Kligman AM. Pseudofolliculitis of the beard. Arch Dermatol. 1956;74:533–42. doi: 10.1001/archderm.1956.01550110077016. [DOI] [PubMed] [Google Scholar]
- 26.Feeney CM, Briggs S. Crack hands: A dermatologic effect of smoking crack cocaine. Cutis. 1992;50:193–4. [PubMed] [Google Scholar]
- 27.Altman LK, Shenhav R, Schaudinischky L. Pseudoxanthoma elasticum. An underdiagnosed genetically heterogeneous disorder with protean manifestations. Arch Intern Med. 1974;134:1048–54. doi: 10.1001/archinte.134.6.1048. [DOI] [PubMed] [Google Scholar]
- 28.Bécuwe C, Dalle S, Ronger-Savlé S, Skowron F, Balme B, Kanitakis J, et al. Elastosis perforans serpiginosa associated with pseudo-pseudoxanthoma elasticum during treatment of Wilson's disease with penicillamine. Dermatology. 2005;210:60–3. doi: 10.1159/000081487. [DOI] [PubMed] [Google Scholar]
- 29.Braun-Falco, Imei S, Schmoeckel C. Pseudopelade of Brocq. Dermatologica. 1986;172:18–26. doi: 10.1159/000249287. [DOI] [PubMed] [Google Scholar]
- 30.Hongcharu W, Taylor CR, Chang Y, Aghassi D, Suthamjariya K, Anderson RR. Topical ALA-photodynamic therapy for the treatment of acne vulgaris. J Invest Dermatol. 2000;115:183–92. doi: 10.1046/j.1523-1747.2000.00046.x. [DOI] [PubMed] [Google Scholar]
- 31.Barrabiera SR. Diseases caused by poxvirus- orf and milker's nodules: A review. J Venom Anim Toxins Incl Trop Dis. 2005;11:102–8. [Google Scholar]
- 32.Yokozeki H, Hibino T, Takemura T, Sato K. Cysteine proteinase inhibitor in eccrine sweat is derived from sweat gland. Am J Physiol. 1991;260:14–20. doi: 10.1152/ajpregu.1991.260.2.R314. [DOI] [PubMed] [Google Scholar]
- 33.Pickus EJ, Lionelli GT, McKinley ET, Lawrence WT, Witt PD. Digital constriction bands in pseudoainhum: Morphological, radiographic, and histological analysis. Ann Plast Surg. 2001;47:194. doi: 10.1097/00000637-200108000-00016. [DOI] [PubMed] [Google Scholar]
- 34.Kochar MS, Caniza M. Parrot pseudoparalysis of the upper extremities. A case report. J Bone Joint Surg Am. 1996;78:284–7. doi: 10.2106/00004623-199602000-00018. [DOI] [PubMed] [Google Scholar]
- 35.Schmied C, Schmied E, Vogel J, Saurat JH. Hoigné's syndrome or pseudo-anaphylactic reaction to procaine penicillin G: A still current classic. Schweiz Med Wochenschr. 1990;120:1045–9. [PubMed] [Google Scholar]
- 36.Fine JD, Johnson LB, Weiner M, Stein A, Cash S, Deleoz J, et al. Pseudosyndactyly and musculoskeletal deformities in inherited epidermolysis bullosa (EB): Experience of the National EB Registry, 1986-2002. J Hand Surg. 2005;30:14–22. doi: 10.1016/j.jhsb.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 37.Eaton CJ, Lister GD. Syndactyly. Hand Clin. 1990;6:555–75. [PubMed] [Google Scholar]
- 38.Haustein U. Scleroderma and pseudoscleroderma: Uncommon presentations. Clin Dermatol. 2005;23:480–90. doi: 10.1016/j.clindermatol.2005.01.019. [DOI] [PubMed] [Google Scholar]
- 39.Tremblay JF, Veilleux CM. Pseudoporphyria associated with hemodialysis treated with N-acetylcysteine. J Am Acad Dermatol. 2003;49:1189–90. doi: 10.1016/s0190-9622(03)00893-4. [DOI] [PubMed] [Google Scholar]
- 40.Donovanosis. In: O’Farrell N, editor; Holmes KK, Sparling PF, Mardh PA, Lemon SM, Stamm WE, Piot P, et al., editors. Sexually transmitted diseases. 3rd ed. New York: McGraw-Hill; 1999. pp. 525–31. [Google Scholar]
- 41.Werman BS, Herskowitz LJ, Olansky S, Kleris G, Sottnek FO. Clinical variant of chancroid resembling granuloma inguinale. Arch Dermatol. 1983;119:890–4. [PubMed] [Google Scholar]
- 42.Pavithran K, Karunakaran M, Palit A, Ragunatha S. Disorders of keratinization. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3rd ed. Mumbai: Bhalani Publishing House; 2008. pp. 995–1069. [Google Scholar]
- 43.Sanchez M, Luger AF. Syphilis. In: Fitzpatrick TB, Eisen AZ, Wolff K, Freedberg IM, Austen FK, editors. Dermatology in general medicine. 4th ed. New York: McGraw-Hill; 1993. pp. 2703–43. [Google Scholar]
- 44.Gummer CL, Dawber RP, Swift JA. Monilethrix: An electron microscopic and electron histochemical study. Br J Dermatol. 1981;105:529–41. doi: 10.1111/j.1365-2133.1981.tb00796.x. [DOI] [PubMed] [Google Scholar]
- 45.Mortimer PS, Burnand KG, Neumann HA. Diseases of the Veins and Arteries: Leg Ulcers. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. Sussex: Wiley-Blackwell; 2010. p. 47. 22. [Google Scholar]
- 46.Grattan C. Aspirin-sensitive urticaria. Clin Exp Dermatol. 2003;28:123–7. doi: 10.1046/j.1365-2230.2003.01228.x. [DOI] [PubMed] [Google Scholar]
- 47.Burrington JD. ‘Pseudorheumatoid’ nodules in children: Report of 10 cases. Pediatrics. 1970;45:473–8. [PubMed] [Google Scholar]
- 48.Robinson-Bostom L, Pomerantz D, Wilkel C, Mader R, Lerner L, Dufresne R, et al. Localized argyria with pseudo-ochronosis. J Am Acad Dermatol. 2002;46:222–7. doi: 10.1067/mjd.2002.116227. [DOI] [PubMed] [Google Scholar]
- 49.Kandil E. Dermal angiolymphoid hyperplasia with eosinophilia versus pseudopyogenic granuloma. Br J Dermatol. 1970;83:405–8. doi: 10.1111/j.1365-2133.1970.tb15726.x. [DOI] [PubMed] [Google Scholar]
- 50.Rasmussen JE. Pediculosis and the pediatrician. Pediatr Dermatol. 1984;2:74–9. doi: 10.1111/j.1525-1470.1984.tb00447.x. [DOI] [PubMed] [Google Scholar]
- 51.Anders N, Wollensak J. Ocular pseudopemphigoid after topical drug administration. Klin Monbl Augenheilkd. 1994;205:61–4. doi: 10.1055/s-2008-1045493. [DOI] [PubMed] [Google Scholar]
- 52.Fernandes NC, Maceira JP, Knackfuss IG, Fernandes N. Botriomicose cutânea. An Bras Dermatol. 2002;77:65–70. [Google Scholar]
- 53.Shah BH, Shah DM. Pseudo-elephantiais of Vulva of Tubercular aetiology. Ind J Dermatol Venereol. 1968;34:245–7. [Google Scholar]


