Abstract
A case of Papular acantholytic dermatosis restricted to the perianal area is being reported in a 26 year old male without involvement of the genitalia, groin and upper thighs for the first time in English literature. The patient presented with long standing grayish white confluent papules with eroded areas in the perianal region which were asymptomatic for a long time before the area got macerated. He did not respond to many weeks of topical steroids but is now showing improvement with topical tacrolimus ointment 0.1% applied twice daily. This entity appears to be very uncommon and also underreported. It is also suggested that this entity be included in the long list of non venereal anogenital lesions as it may mimic perianal warts or molluscum contagiosum.
Keywords: Focal acantholytic dyskeratosis, papular acantholytic dermatosis, perianal region
Introduction
What was known?
Papular acantholytic dermatosis of the anogenital/genitocrural area is a type of focal acantholytic dermatosis. As the name suggests, there is usually an asymptomatic papular eruption, which is localized to the genitalia, perineal region sometimes extending to the groin or the upper thighs. It is more common on and around vulva and there are very few case reports of men. Histologicaly, this can show signs of both Hailey Hailey disease as well as Darier's disease. It is chronic in nature and is known to run a protracted course.
Papular acantholytic dermatosis (PAD) of the anogenital area is an uncommon entity and is considered a variant of focal acantholytic dermatosis originally described by Ackerman in 1972. It can mimic Hailey Hailey disease, Darier's disease, and Grover's disease histologically, but it is differentiated from these entities clinicopathologically. Molecular genetic studies where feasible and possible have also demonstrated abnormal mutations in ATP2C1 gene in some cases. This entity because of its anogenital location should be considered as one of the non-venereal genital lesions due to its clinical resemblance to genital warts and molluscum contagiosum in the early stages. PAD may also be underreported and, therefore, more awareness regarding the entity is recommended among practicing dermatologists and pathologists.
Case Report
A 26-year-old man presented with discomfort in his perianal area for the past 6 months. He reported that he had first noticed an asymptomatic eruption that he could feel as rough skin and ignored it. He later showed it to his wife who described it as several small grayish bumps. Over the past 2 months, he started getting a burning and itching sensation in that area. On examination, he had grayish-white areas perianally with multiple firm, coalescent papules extending a little posterior toward the natal fold and anteriorly on the perineum [Figure 1]. There were some excoriations and maceration in some areas. There were no vesicles, oozing, or bleeding. Gram staining and 10% KOH mount did not show any organism. Proctoscopy performed by a surgeon showed normal anal mucosa. All other mucosae were normal. Penis, scotum, and groin were normal. No other area on his body was affected. He was a healthy man with a negative personal or family history of atopy or any other pre-existing dermatosis. He had no relevant sexual history. He had taken treatment from two dermatologists in the past 2 months who had given potent topical steroids and oral antihistamines, which did not benefit him. A 3-mm punch biopsy showed circumscribed foci of hyperkeratosis with acantholytic dyskeratosis and subrabasal cleft formation [Figure 2]. Within the foci, the epidermis showed scattered acantholytic dyskeratotic cells (corps ronds) [Figure 3]. The stratum corneum showed a column of parakeratotic dyskeratotic cells (grains). Underlying dermis showed sparse superficial perivascular lymphohistiocytic infiltrate. Mild papillomatosis was seen as well. Clinicopathological correlation ruled in favor of papular acantholytic dyskeratosis of the perianal area.
Figure 1.

Grayish-white confluent papules in the perianal and perianal area extending posteriorly toward natal cleft in the midline only
Figure 2.
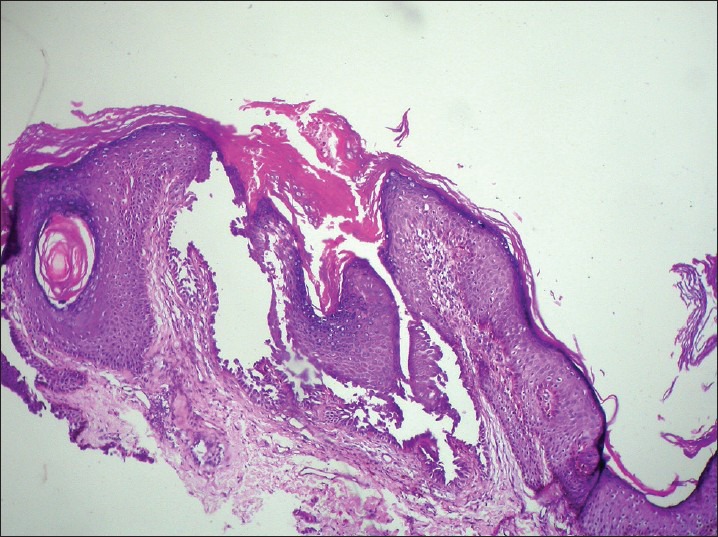
Low power view of papule showing suprabasal cleft, dyskeratosis, and acantholytic cells (H and E, ×10)
Figure 3.
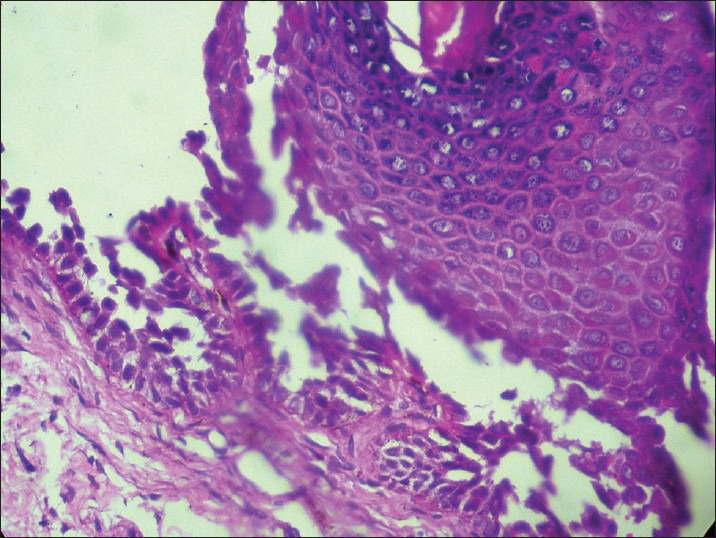
High power view of dyskeratotic acantholytic cells (Corps ronds) (H and E, ×40)
Discussion
Papular acantholytic dyskeratosis (PAD) is a clinical form of a rare and distinct entity first described by Bernard Ackerman in 1972 as focal acantholytic dyskeratosis.[1] He observed that the features that we commonly find in Darier's disease were not confined to just that entity, but were also found in other conditions where lesions were either single or multiple, evanescent or long-standing papules or nodules or, at times, even clinically unapparent, i.e., the “incidental” variant. The distinctive histological features in all these lesions were suprabasal clefts around intact papillae (villi) and dyskeratotic acantholytic cells at various levels in the epidermis-like corps ronds and grains, hyperkeratosis, and parakeratosis. He unified these entities as focal acantholytic dyskeratosis.[1] Over a period of time, several sporadic cases of papular lesions located in the anogenital region such as labia, perineum, groin, perianal area, anal canal, penis, scrotum, and lips have been described, where the lesions have been long-standing and their histology consistently shows features of acantholytic dyskeratosis with a histological diagnosis of Darier's disease or HHD.[2,3,4,5,6,7,8,9,10] Some authors have labeled these cases “PAD” as well as “acantholytic dermatoses of the genitocrural/perineal region.” In the limited number of reports available, this entity seems more common in women with only few cases reported in males.[3] Many of them have been asymptomatic, except for some presenting with itching and burning, and all have been persistent.[4,5] The moist and warm milieu of the genitoperineal area could be the reason for the localization of this entity to that particular area.[3,4,6] One of the authors has also suggested the possible role of ovarian hormones based on the premenstrual itching and burning that his patients described.[4,6] The burning and itching in a moist environment could be the reason why some lesions present with maceration. All three cases of PAD of anal canal had a history of hemorroidectomy, which may have acted as a precipitating agent.[7] Whitish-gray papules, confluent papules, deep-seated vesicle like lesions, erosions, crusting, and macerated patches have all been described by various authors.[2,3,4,5,6,7,8,9,10] Many cases have involvement of multiple locations like genitalia and upper thighs, genitalia and perianal area, anal canal and lips, and so on.[3,4,6,7,8] Absence of involvement of areas like axillary folds, inframammary folds, neck, and seborrheic areas help rule out HHD and Darier's disease. Absence of family history goes against the diagnosis of HHD and Darier's disease, which are both autosomal dominant disorders. HHD localized to the genital areas in both the sexes has been reported, but these cases invariably have a family history of similar or more widespread involvement.[3] Localized or segmental variant of Darier's disease showing acantholytic dyskeratosis has also been reported on the trunk and extremities, but never over the genitalia.[3] The coexisting histological features of HHD and Darier's disease rules against the diagnosis of either of them in a localized form.[1,3,4] Grover's disease is ruled out due to absence of lesions anywhere else on the body and the long-standing nature of the lesions. ATP2C1 mutations have been demonstrated by workers, and it has been suggested that PAD may be a variant of HHD.[8,9] Pernet et al.,[9] described two patients with vulvar and perianal dyskeratotic acantholytic dermatosis with ATP2C1 mutations. Therefore, they have suggested that this mutation may lead to a distinct phenotype, which is variably described as “PAD of the vulva” or “PAD of the vulvocrural and/or the anogenital area.” They also suggested that these different clinical entities should be considered as being allelic to HHD.[9]
Papular acantholytic dyskeratosis is a chronic disease. Experience with topical steroids has been uniformly disappointing. Tretinoin has been reported to be temporarily effective in one case.[4] Recently, topical tacrolimus ointment (0.1%) was reported to be effective in a patient. Electrocauterisation, cryosurgery, and CO2 laser with an emphasis on reaching more depth of the lesions have been tried with variable success outcomes.[4,6,10]
This appears to be the first case confined to the perianal and perineal region in a male without simultaneous involvement of the penis, scrotum, anal canal, or lips. A closed, warm, and moist milieu may be one of the triggering factors for developing secondary maceration, burning, and itching in our patient. He did not benefit from topical steroids and was prescribed 0.1% tacrolimus ointment, which he has been applying for the past 3 weeks with marked reduction in burning and itching. Acantholytic dermatosis of the genitalia/perineal/genitocrural/perianal region may be underreported; therefore, it is important to sensitize dermatologists as well as pathologists about this entity. It should also be included in the list of non-venereal genital disorders as it can mimic condylomata or molluscum contagiosum.
What is new?
This is, to the best of my knowledge, the first case report of PAD restricted to the perianal and perineal region in a male without involvement of the penis, groin scrotum, or upper thighs.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Ackerman AB. Focal acantholytic dyskeratosis. Arch Dermatol. 1972;106:702–6. [PubMed] [Google Scholar]
- 2.Chorzelski TP, Kudejko J, Jablonska S. Is papular acantholytic dyskeratosis of the vulva a new entity? Am J Dermatopathol. 1984;6:557–60. doi: 10.1097/00000372-198412000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Wong TY, Mihm MC., Jr Acantholytic dermatosis localized to genitalia and crural areas of male patients: A report of three cases. J Cutan Pathol. 1994;21:27–32. doi: 10.1111/j.1600-0560.1994.tb00687.x. [DOI] [PubMed] [Google Scholar]
- 4.Krishnan RS, Ledbetter LS, Reed JA, Hsu S. Acantholytic dermatosis of the vulvocrural area. Cutis. 2001;67:217–9. 220. [PubMed] [Google Scholar]
- 5.Wang L, Yang XC, Hao F, Mei Y, Ye QY. Papular acantholytic dyskeratosis of the vulva. Eur J Dermatol. 2009;19:402–3. doi: 10.1684/ejd.2009.0697. [DOI] [PubMed] [Google Scholar]
- 6.Coppola G, Muscardin LM, Piazza P. Papular acantholytic dyskeratosis. Am J Dermatopathol. 1986;8:364–5. doi: 10.1097/00000372-198608000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Lee JH, Kim YC, Lew W. A case of focal acantholytic dyskeratosis occurring on both the lip and the anal canal. Yonsei Med J. 2003;44:166–8. doi: 10.3349/ymj.2003.44.1.166. [DOI] [PubMed] [Google Scholar]
- 8.Lipoff JB, Mudgil AV, Young S, Chu P, Cohen SR. Acantholytic dermatosis of the crural folds with ATP2C1 mutation is a possible variant of Hailey-Hailey Disease. J Cutan Med Surg. 2009;13:151–4. doi: 10.2310/7750.2008.08005. [DOI] [PubMed] [Google Scholar]
- 9.Pernet C, Bessis D, Savignac M, Tron E, Guillot B, Hovnanian A. Genitoperineal papular acantholytic dyskeratosis is allelic to Hailey-Hailey Disease. Br J Dermatol. 2012;167:210–2. doi: 10.1111/j.1365-2133.2012.10810.x. [DOI] [PubMed] [Google Scholar]
- 10.Dittmer CJ, Hornemann A, Rose C, Diedrich K, Thill M. Successful laser therapy of a papular acantholytic dyskeratosis of the vulva: Case report and review of literature. Arch Gynecol Obstet. 2010;281:723–5. doi: 10.1007/s00404-009-1313-8. [DOI] [PubMed] [Google Scholar]


