Sir,
The association between systemic sclerosis and malignancy is not very strong, although not rare. In this article, we describe an unusual co-existence of Anti Scl-70 positive systemic sclerosis with non small cell carcinoma of lung.
A 54 years old male patient presented to Dermatology Out-Patient Department (OPD) with vesicular eruption on left shoulder which was diagnosed as Herpes zoster. Incidentally, we discovered tightening of the skin of his face, upper chest, back and both hands [Figure 1a]. He said he had been experiencing this stiffening of skin for 6 months. There was no history of Raynaud's phenomenon. He had been diagnosed with metastatic squamous cell carcinoma of lung 3 months back and was being treated with palliative chemotherapy like Doxorubicin and Paclitaxel and radiation.
Figure 1a.

Sclerodermatous face showing constricted mouth, hyperpigmented, stiff skin of face and upper trunk which also shows lesions of herpes zoster
On cutaneous examination, the skin over the extremities, face and trunk were hard, shiny and could not be pinched up. There were few mat-like telangiectasias on face. The oral aperture was constricted with radial furrows. The fingers were edematous, with mild flexion contracture and a smooth, shiny, tight skin without any digital pitted scarring [Figure 1b].
Figure 1b.

Sclerodactyly with flexion contracture
A skin biopsy revealed mild thinning of the epidermis, hyalinization of the dermal collagen, sparse lymphocytic infiltrate [Figure 2]. Mucin staining was negative which ruled out scleromyxedema. There was high titer of Anti-Nuclear Antibody (ANA) (1:640) and strongly positive Anti Scl-70 antibody. His contrast CT scan of thorax showed a large mass in right lung which on CT guided Fine Needle Aspiration Cytology (FNAC) revealed squamous cell carcinoma. CT scan of abdomen showed multiple metastatic deposits in liver.
Figure 2.
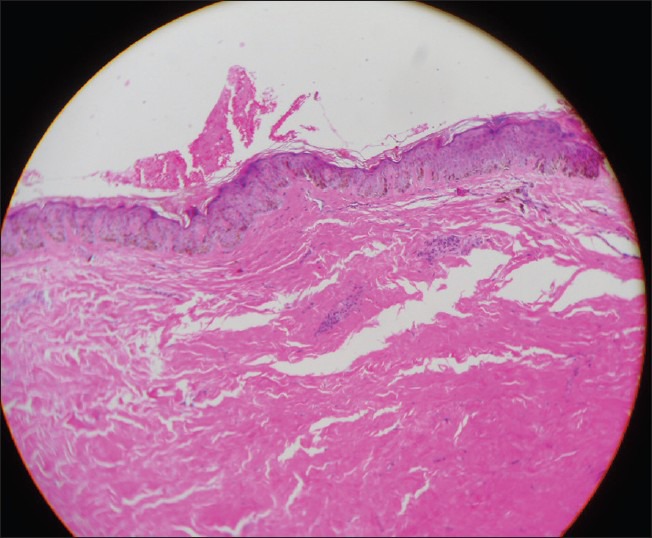
Photomicrograph of hematoxylin-eosin stained section of skin showing mild thinning of the epidermis, hyalinization of the dermal collagen, sparse lymphocytic infiltrate
Systemic sclerosis has been linked with occurrence of internal malignancy and a possible role of tumor derived connective tissue growth factors has been implicated.[1] Systemic sclerosis with history of Raynaud's phenomenon and nail fold bleeding with underlying uterine carcinoma has been reported. It was found to improve with resection of the tumor.[2] A case of melanoma developing anti Jo-1 positive paraneoplastic scleroderma has also been published.[3] There is one reported case of autoantibody positive paraneoplastic SSc in Hairy cell leukemia.[4] Association of scleroderma and malignancy has been found to occur in 3 situations-chemotherapy (like bleomycin or taxanes) or radiation induced scleroderma, lung cancer developing over preexisting interstitial fibrotic lung disease in a scleroderma patient and paraneoplastic scleroderma. Isolated cases of carcinoma of the thyroid, ovary, cervix, brain, esophagus, stomach, breast, lymphoma and leukemia with systemic sclerosis have been reported which may be coincidental.[5] The atypical presentations of paraneoplastic SSc that differentiate it from idiopathic variety are: Age at onset over 50 years, male gender (majority of SSc develop in females), sclerodactyly, progressive skin sclerosis extending to the neck and trunk, and acute onset of Raynaud's phenomenon. On the contrary, the absence of Raynaud's phenomenon with a normal capillaroscopy pattern can be another distinguishing feature of cancer induced systemic sclerosis.[6] The reported cases of malignancy superimposed on lung disease have a prolonged history of the patient suffering from systemic sclerosis.[7] In our case, the sclerodermatous changes of skin had started 3 months before the diagnosis of his lung cancer and was progressing rapidly. As the malignancy had already metastasized, we may presume that the cancer preceded the onset of dcSSc. Hence, there was a strong suspicion of paraneoplastic etiology of this connective tissue disease. Although most of the reported cases of scleroderma occurring in the context of malignancy have negative serum autoantibodies, our case had laboratory parameters indistinguishable from idiopathic dcSSc type.
An elderly male patient developing systemic sclerosis in a short span of time should warn us against a possible underlying malignancy. Paraneoplastic systemic sclerosis with anti SCL 70 positivity and underlying lung malignancy is a rare case and hence has been reported here.
References
- 1.Gruber BL, Miller F, Kaufman LD. Simultaneous onset of systemic sclerosis (scleroderma) and lung cancer: A case report and histologic analysis of fibrogenic peptides. Am J Med. 1992;92:705–8. doi: 10.1016/0002-9343(92)90795-d. [DOI] [PubMed] [Google Scholar]
- 2.Yamamoto M, Suzuki C, Naishiro Y, Tsukuda H, Murakami R, Yamamoto H, et al. [A case of pseudoscleroderma as paraneoplastic syndrome due to carcinoma of cervical uteri] Nihon Rinsho Meneki Gakkai Kaishi. 2003;26:293–8. doi: 10.2177/jsci.26.293. [DOI] [PubMed] [Google Scholar]
- 3.Thoelke A, Schmid HP, Figl R, Schadendorf D, Ugurel S. Jo-1 positive paraneoplastic systemic sclerosis in a patient with metastatic melanoma. Eur J Dermatol. 2006;16:428–30. [PubMed] [Google Scholar]
- 4.Juarez M, Marshall R, Denton C, Evely R. Paraneoplastic scleroderma secondary to hairy cell leukaemia successfully treated with cladribine. Rheumatology (Oxford) 2008;47:1734–5. doi: 10.1093/rheumatology/ken367. [DOI] [PubMed] [Google Scholar]
- 5.Talbott JH, Barrocas M. Progressive systemic sclerosis (PSS) and malignancy, pulmonary and non-pulmonary. Medicine (Baltimore) 1979;58:182–207. doi: 10.1097/00005792-197903000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Racanelli V, Prete M, Minoia C, Favoino E, Perosa F. Rheumatic disorders as paraneoplastic syndromes. Autoimmun Rev. 2008;7:352–8. doi: 10.1016/j.autrev.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 7.M’Raihi ML, Haltiti R, Zegaya M. [Combination of scleroderma and non bronchiolo-alveolar bronchial carcinoma. Report of a case and short review of the literature] Rev Pneumol Clin. 1988;44:198–201. [PubMed] [Google Scholar]


