Abstract
A 4 year old boy presented with history of itchy raised lesions on body of 2 years duration. Though parental consanguinity was not present, his elder brother had similar complaints. Dermatological examination revealed multiple hyperpigmented papules with a central keratotic plug distributed mainly over face and extensors of upper and lower extremities. Koebnerisation was present. Skin biopsy revealed perforating collagen bundles in the upper dermis and epidermis which was confirmed by Van Gieson staining. Patient was being treated with topical retinoids and intralesional corticosteroids with minimal relief.
Keywords: Collagen, perforating disorders, reactive perforating collagenosis, retinoids
Introduction
What was known?
Reactive perforating collagenosis is a rare perforating disorder.
It is characterised by collagen bundles perforating the epidermis.
Reactive perforating collagenosis (RPC) is a rare form of transepidermal elimination (TEE) disorder in which there is extrusion of altered collagen from the epidermis. RPC can exist in two forms; the commoner acquired form and the rare familial form. In the familial form, the lesions manifest in early childhood is not associated with pruritus and usually spontaneously resolves. Very few cases of inherited RPC have been reported in literature. We herein report a rare case of RPC in a young child with similar complaints in sibling.
Case Report
A 4 year old boy presented with complaints of multiple, recurrent, dark coloured raised lesions on face, elbows and outer aspect of both legs of 2 years duration. The lesions would start as skin coloured papules which later developed dark central material. Some of the lesions would heal on its own in about a month leaving behind residual hyperpigmentation. Associated severe itching was present in all lesions. Patient's mother complained that she had noticed new lesions occurring at sites of trauma. There was history of similar complaints in his elder brother who was staying with his grandparents. There was no parental consanguinity.
Dermatological examination revealed multiple, discrete, symmetrical, hyperpigmented, hyperkeratotic papules distributed over face, both elbows and lateral aspect of both legs [Figure 1]. Most of the lesions showed a central keratotic plug. There was evidence of koebnerisation at multiple sites [Figure 2]. Systemic examination was essentially normal.
Figure 1.

Hyperkeratotic papules with central plugging over elbows and evidence of Koebnerisation
Figure 2.

Similar lesions on lower limbs
Routine lab investigations were normal. Skin biopsy from the lesion showed stratified squamous keratinised epidermis. Epidermis showed a hyperkeratotic crater filled with keratin, few polymorphonuclear leucocytes and occasional acellular basophilic fibrous strands. The shoulder of the crater shows marked acanthosis. The adjacent papillary dermis showed vertically oriented collagen bundles perforating the epidermis [Figure 3]. Moderate perivascular chronic mononuclear cell infiltrate was seen. The perforating collagen bundles were better delineated on Van Gieson stain [Figure 4]. Based on clinical and histopathological features, a diagnosis of reactive perforating collagenosis was made. The patient was started on topical tretinoin 0.05% cream and intralesional corticosteroids. The lesions showed some flattening with therapy but the patient continued to get new lesions at sites of minor trauma.
Figure 3.
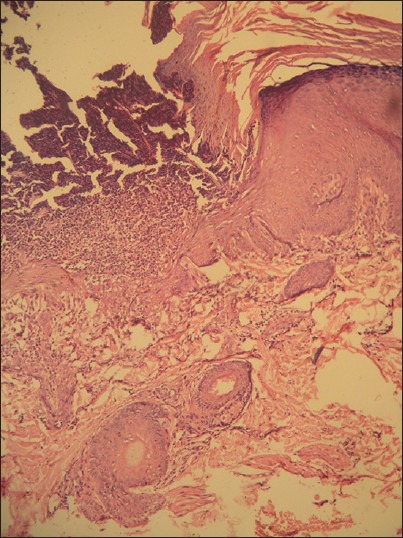
Histopathology of skin lesions revealing epidermal parakeratosis and perforating bundles of collagen (H and E, ×40)
Figure 4.

Perforating collagen bundles evident in Van Gieson stain (Van Gieson stain, ×40)
Discussion
Reactive perforating collagenosis is an uncommon type of perforating disorder. There are four different types of perforating disorders and all are characterized by transepidermal elimination of altered dermal substances. They are Kyrle's disease, perforating folliculitis, elastosis perforans serpiginosa and reactive perforating collagenosis. The elimination takes place by the upward movement of regenerating keratinocytes. In RPC there is transepidermal elimination of altered collagen. This entity was first described by Mehregan et al. in the year 1967.[1]
The inherited form of RPC is associated with a positive family history in about two thirds of patients.[2] Consanguinity in parents is present in some cases with an autosomal recessive mode of inheritance,[3] though dominant types have also been mentioned. There is a slight male preponderance with siblings being affected as in our case.
In the acquired variant, the lesions manifest after the age of eighteen years and are usually associated with itching. Acquired variant is mostly associated with diabetes and chronic renal failure. It is also associated with hypothyroidism, hyperparathyroidism, liver disorders, Hodgkin's disease, neurodermatitis, HIV and IgA nephropathy.[4]
The morphology of lesions is similar in both the entities and consists of umbilicated papules and nodules that can be skin coloured, erythematous or hyperpigmented and characteristically have a central keratotic plug. The distribution of lesions is generally over extensor aspect of extremities. Koebnerisation is commonly seen as in our patient.
In genetically predisposed individuals, trauma results in altered collagen and this predisposes to RPC.[5] Scratching induces lesions and common sites of involvement are the accessible and trauma prone sites, as seen in our patient also. Research has shown that in most cases no abnormality exists in the ultrastructure of the extruded collagen,[6] but histochemical changes may be present.[7]
Histologically, early lesions show variable acanthosis and accumulation of collagen, which is basophilic in dermal papillae. Mature lesions show characteristic features of RPC where there is plug of parakeratotic material, basophilic debris and degenerated collagen lying within cup-shaped depressions in epidermis. As the condition resolves, there is usually epidermal regeneration with minimal scarring. All these features were present in our patient.
Many treatment modalities have been tried with varying success rates. The important treatment options are topical retinoids, topical corticosteroids, intralesional steroids, Psoralen Ultra Violet-A, Narrow Band UV-B (PUVA, NBUVB) and allopurinol.[8,9,10]
Very few cases of inherited RPC are reported in literature.[11] There are only about 2 reports from India. The familial form can also be associated with pruritus and may not spontaneously resolve as in our patient, which is not reported before.
What is new?
Reactive perforating collagenosis can be rarely familial.
The familial form can also be associated with pruritus and may not spontaneously resolve as in our patient.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Mehregan AH, Schwartz OD, Livingood CS. Reactive perforating collagenosis. Arch Dermatol. 1967;96:277–82. [PubMed] [Google Scholar]
- 2.Kanan MW. Familial reactive perforating collagenosis and intolerance to cold. Br J Dermatol. 1974;91:405–14. doi: 10.1111/j.1365-2133.1974.tb13078.x. [DOI] [PubMed] [Google Scholar]
- 3.Woo TY, Rasmussen JE. Disorders of transepidermal elimination. Part I. Int J Dermatol. 1985;24:267–79. doi: 10.1111/j.1365-4362.1985.tb05781.x. [DOI] [PubMed] [Google Scholar]
- 4.Faver IR, Daoud MS, Su WP. Acquired reactive perforating collagenosis: Report of six cases and review of the literature. J Am Acad Dermatol. 1994;30:575–80. doi: 10.1016/s0190-9622(94)70065-6. [DOI] [PubMed] [Google Scholar]
- 5.Bovenmyer DA. Reactive perforating collagenosis. Experimental production of the lesion. Arch Dermatol. 1970;102:313–7. doi: 10.1001/archderm.102.3.313. [DOI] [PubMed] [Google Scholar]
- 6.Millard PR, Young E, Harrison DE, Wojnarowska F. Reactive perforating collagenosis: Light, ultrastructural and immunohistological studies. Histopathology. 1986;10:1047–56. doi: 10.1111/j.1365-2559.1986.tb02541.x. [DOI] [PubMed] [Google Scholar]
- 7.Herzinger T, Schirren CG, Sander CA, Jansen T, Kind P. Reactive perforating collagenosis – Transepidermal elimination of type IV collagen. Clin Exp Dermatol. 1996;21:279–82. doi: 10.1111/j.1365-2230.1996.tb00094.x. [DOI] [PubMed] [Google Scholar]
- 8.Cullen S. Successful treatment of reactive perforating collagenosis with tretinoin. Cutis. 1979;23:187–91. [PubMed] [Google Scholar]
- 9.Morton CA, Henderson IS, Jones MC, Lowe JG. Acquired perforating dermatosis in a British dialysis population. B J Dermatol. 1996;135:671–7. [PubMed] [Google Scholar]
- 10.Hoque SR, Ameen M, Holden CA. Acquired reactive perforating collagenosis: Four patients with a giant variant treated with allopurinol. Br J Dermatol. 2006;154:759–62. doi: 10.1111/j.1365-2133.2005.07111.x. [DOI] [PubMed] [Google Scholar]
- 11.Ramesh V, Sood N, Kubba A, Singh B, Makkar R. Familial reactive perforating collagenosis: A clinical, histopathological study of 10 cases. J Eur Acad Dermatol Venereol. 2007;21:766–70. doi: 10.1111/j.1468-3083.2006.02085.x. [DOI] [PubMed] [Google Scholar]


