Abstract
Background: Total or red meat intake has been shown to be associated with a higher risk of mortality in Western populations, but little is known of the risks in Asian populations.
Objective: We examined temporal trends in meat consumption and associations between meat intake and all-cause and cause-specific mortality in Asia.
Design: We used ecological data from the United Nations to compare country-specific meat consumption. Separately, 8 Asian prospective cohort studies in Bangladesh, China, Japan, Korea, and Taiwan consisting of 112,310 men and 184,411 women were followed for 6.6 to 15.6 y with 24,283 all-cause, 9558 cancer, and 6373 cardiovascular disease (CVD) deaths. We estimated the study-specific HRs and 95% CIs by using a Cox regression model and pooled them by using a random-effects model.
Results: Red meat consumption was substantially lower in the Asian countries than in the United States. Fish and seafood consumption was higher in Japan and Korea than in the United States. Our pooled analysis found no association between intake of total meat (red meat, poultry, and fish/seafood) and risks of all-cause, CVD, or cancer mortality among men and women; HRs (95% CIs) for all-cause mortality from a comparison of the highest with the lowest quartile were 1.02 (0.91, 1.15) in men and 0.93 (0.86, 1.01) in women.
Conclusions: Ecological data indicate an increase in meat intake in Asian countries; however, our pooled analysis did not provide evidence of a higher risk of mortality for total meat intake and provided evidence of an inverse association with red meat, poultry, and fish/seafood. Red meat intake was inversely associated with CVD mortality in men and with cancer mortality in women in Asian countries.
See corresponding editorial on page 865.
INTRODUCTION
Asia is experiencing marked changes in lifestyle and disease patterns, similar to those seen in Western countries (1, 2), with projected increases in the proportions of deaths from cancer, ischemic heart disease, and cardiovascular disease (CVD)4 (3). Therefore, it is important to identify modifiable risk factors, such as diet, which may be responsible for the rising rates of chronic disease in Asian populations.
Meat intake varies across regions and countries in Asia, with relatively low consumption in certain countries compared with others in the continent (4). Meat intake, specifically red meat, has been associated with an increased risk of mortality in Western populations (5, 6), although further studies are warranted in populations that consume different quantities and types of meat and have dissimilar confounding factors. Many mechanisms supporting a detrimental effect of meat have been proposed in relation to specific outcomes: an adverse lipid profile and free radical generation as a result of high intakes of SFA and iron, mutagens generated by high-temperature cooking (7, 8), and N-nitroso compounds formed in processed meat and endogenously from heme iron (9). The different rates of change and economic development in Asian countries provide a fertile environment for conducting etiologic research on chronic disease, because it provides a large range of exposures and a variety of endpoints. We initiated the Asia Cohort Consortium (ACC) to understand chronic disease etiology in Asia, where the association between dietary factors and chronic diseases has not been extensively studied. In the current study, we 1) compared ecological trends in meat intake over the past 37 y between Asia and the United States and 2) assessed whether meat intake was associated with all-cause, cancer and CVD mortality by using individual, prospective data from a pooled analysis of Asian cohort studies involving 296,721 men and women.
SUBJECTS AND METHODS
Meat consumption in Asia
We compared temporal trends in meat consumption in Bangladesh, China, Japan, South Korea, and the United States with the use of the FAO database (10). We compared meat consumption in Asia with that in the United States because of high meat consumption in the United States and supportive evidence for high mortality with high meat intake in a large US cohort study (5, 6). The FAO Statistical Database, the world's largest online agricultural database (available at http://faostat.fao.org/, accessed 13 June 2012), details historical and chronologic population-based production and disappearance data (referred to as food availability). For livestock production and product consumption, FAO has compiled relevant data—including agricultural production, fish production, trade, food supply, food balance sheets, supply utilization accounts, and population size—submitted by member countries in the form of replies to FAO questionnaires (11). The FAO Statistical Database provides data on per capita consumption of meat, beef, pork, poultry, and fish and seafood and defines total meat (excluding fish) as the sum of beef, poultry, pork, mutton, goat, and game. Per capita consumption (kcal/person per year) is the total amount of food in each commodity available for each individual in the total population during the period 1970–2007, representing the average amount available for the population as a whole.
Study population
The ACC was described elsewhere (12). For the meat and mortality analysis, a total of 8 prospective cohort studies from Bangladesh, mainland China, Japan, Korea, and Taiwan were included. We excluded participants who did not provide food-frequency questionnaires (FFQs) (n = 8177) and those for whom time under study was missing (n = 467). A total of 296,721 (112,310 men and 184,411 women) were included in this analysis. Each cohort collected cause-specific deaths through linkage to death registries or active follow-up. The study was reviewed and approved by the ethics committee for all participating cohort studies and by the institutional review board of Fred Hutchinson Cancer Research Center.
Assessment of dietary and nondietary factors
Each study assessed food intake with a validated FFQ consisting of the frequency of intake, further qualified as specified portions (weights, numbers, or servings) or serving sizes (eg, a half bowl, one bowl) (13–18). The number of items for red meat, poultry, and fish varied from 6 to 17 across studies (see Supplemental Table 1 under “Supplemental data” in the online issue). We quantified food-group intake in grams per day or servings per day using the reported frequency of intake of each relevant food item and study-specific portion sizes. Data on age, education, alcohol intake, tobacco smoking, and residence were collected through self-administered questionnaire or interview. Height and weight were self-reported or directly measured. BMI was calculated by dividing weight (in kg) by the square of height (in m).
Statistical analysis
Using individual-level data, we calculated study-specific HRs and 95% CIs using a Cox proportional hazards model; age was used as the time metric. Person-years of follow-up were estimated from the baseline entry date until the date of death, loss to follow-up (if applicable), or end of follow-up, whichever came first. Baseline age (<40, 40–49, 50–59, 60–69, 70–79, and ≥80 y), educational level (less than secondary, secondary, and more than secondary school graduate), alcohol intake (continuous), urban or rural residence, total energy intake (continuous), fruit and vegetable intake (continuous), BMI (in kg/m2; <18.5, 18.5–19.9, 20.0–24.9, 25.0–29.9, and ≥30.0), and tobacco smoking (never smoked, former smoker, current with <20 pack-years of smoking, and current with ≥20 pack-years of smoking) were adjusted for as potential confounding factors in the multivariate analyses. Outcomes of interest included all-cause mortality and cancer and CVD mortality. Because the number of food items varied across studies, in the main analysis, we obtained HRs and 95% CIs using study- and sex-specific quartiles of grams per day of each food group. For males and females separately, cohort-specific HRs were pooled to compute cross-cohort estimates by using a random-effects model. The random-effects model also produced a trend test for pooled HR estimates. Tertiles rather than quartiles of poultry intake were used to ensure an adequate number of cases in each category. In supplemental analyses, we computed pooled cohort HRs from cohort-specific estimates computed by using uniform cutoffs rather than cohort-specific cutoffs to construct intake quartiles and tertiles. In other supplemental analyses, we included 2 additional cohort studies that offered nonquantitative dietary intake data: 1) the Korean Multi-Center Cancer Cohort Study (19) and 2) the Radiation Effects Research Foundation in Hiroshima and Nagasaki, the Life Span Study cohort (20), which had assessed diet by using nonquantitative FFQs (data on frequency of intake only). We tested for heterogeneity across studies using a likelihood ratio test that compared random- and fixed-effect models for pooled cohort effect estimates. Because socioeconomic status may be related to meat intake and disease pattern in Asian populations and because meat intake varies over time, we also examined whether the associations varied by educational level. Also, we examined whether BMI, smoking status, or baseline period modified the associations. All statistical tests were 2-sided and P values <0.05 were considered to be statistically significant. We used SAS version 9.3 (SAS Institute) for the analyses.
RESULTS
Consumption trends using ecologic data
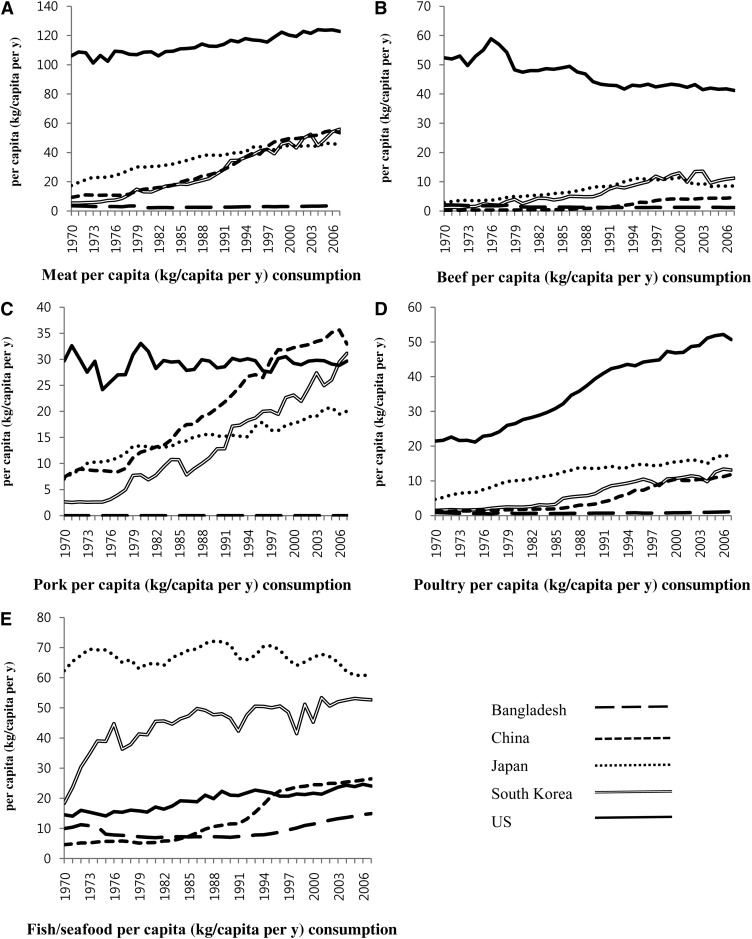
We examined temporal trends in per capita consumption of meat, beef, pork, poultry, and fish/seafood with the use of the international FAO database (Figure 1 and Figure 2). We compared meat-consumption patterns between the United States and Asian populations because there have been numerous meat- and chronic disease–related studies conducted in the United States (5, 6, 21–23). Ecological data indicate an increase in meat intake in Asian countries. Per capita consumption of meat (excluding fish) in the United States was >2 times that in China, Japan, and South Korea and >33 times that in Bangladesh in the 1990s and 2000s (Figure 1). In 2007, average meat consumption in the United States was 122.8 kg/y, whereas consumption in China, Japan, and South Korea ranged from 46.1 to 55.9 kg/y. Per capita beef consumption has decreased to some degree in the past decade in the United States but still remains substantially higher than that in Asian countries. Beef consumption increased in China, Japan, and Korea from 1970 to 2007. Although beef consumption in the United States remains higher, the gap with Japan or Korea has progressively decreased; in 1970, the difference was 18-fold; in 1980, it was 10-fold; in 1990, it was 5-fold; and in 2007, it was 4-fold. Per capita consumption of pork has continued to rise in China, Japan, and Korea; consumption in China and Korea has now surpassed consumption in the United States. Per capita consumption of poultry has been rising in China, Japan, South Korea, and the United States, but the difference between the United States and Asian countries remained substantial. Per capita consumption of fish and seafood in Japan and Korea has remained higher than that in the United States; consumption in China has risen to a level similar to that in the United States but that is still substantially lower than that in Japan and Korea.
FIGURE 1.
Meat (A–D) and seafood (E) consumption (FAO data) in Bangladesh, China, Japan, South Korea, and the United States. Meat (A) includes beef, poultry, pork, mutton, goat, and game.
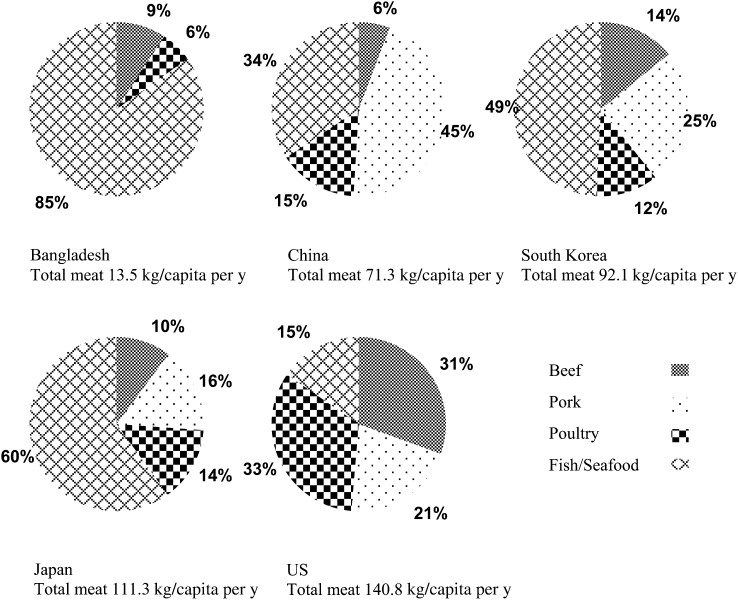
FIGURE 2.
Percentages of per capita consumption in 2000 in Bangladesh, China, Japan, South Korea, and the United States.
When we compared the proportions of per capita consumption of beef, pork, poultry, and fish/seafood in Bangladesh, China, Japan, and Korea with those in the United States, using the 2000 FAO database, the proportions of fish/seafood consumption in Asian countries were higher than those in the United States (34%–85% compared with 15%), whereas total meat consumption (largely beef and poultry, totaling 64%) in the United States was higher than that in Asian countries (Figure 2). China consumed the highest proportion of pork (45%) and Bangladesh and Japan consumed the highest proportion of fish/seafood (85% in Bangladesh and 60% in Japan).
Individual consumption and mortality
In our pooled analysis of the ACC data, the mean follow-up period ranged from 6.6 to 15.6 y. Most studies began enrollment in the early to mid 1990s (Table 1). Mean intakes of red meat and poultry in men were 14.2–92.3 and 4.6–22.3 g/d, respectively (Table 2). In women, mean intakes of red meat ranged from a low of 9.9 g/d in the Ohsaki National Health Insurance Cohort Study to 50.9 g/d in the Shanghai Women's Health Study. Poultry intake ranged from 2.8 to 15.4 g/d in women. Mean fish and seafood intake was >45 g/d in men and >36 g/d in women.
TABLE 1.
Baseline characteristics of the cohort studies included1
| Enrollment year, study, and sex | Follow-up period2 | Baseline cohort size | Age range at entry | Total energy intake3 | No. of all deaths | No. of cancer deaths | No. of CVD deaths |
| y | kcal/d | ||||||
| 1990–1992 | |||||||
| JPHC1 (males) | 14.2 ± 3.7 | 20,595 | 40–59 | 2124 (879) | 2300 | 953 | 600 |
| JPHC1 (females) | 14.7 ± 3.1 | 22,443 | 40–59 | 1398 (440) | 1128 | 541 | 284 |
| 1992–1995 | |||||||
| JPHC2 (males) | 11.2 ± 3.2 | 26,721 | 40–69 | 1675 (684) | 3662 | 1621 | 882 |
| JPHC2 (females) | 11.7 ± 2.6 | 29,690 | 40–69 | 1087 (330) | 1805 | 784 | 478 |
| 1990 | |||||||
| Miyagi (males) | 12.6 ± 2.7 | 21,536 | 40–64 | 1885 (886) | 2335 | 838 | 424 |
| Miyagi (females) | 12.9 ± 2.3 | 23,430 | 40–64 | 1307 (438) | 1152 | 421 | 202 |
| 1995 | |||||||
| Ohsaki (males) | 9.8 ± 3.8 | 23,462 | 40–80 | 1757 (829) | 4605 | 1649 | 1305 |
| Ohsaki (females) | 10.0 ± 3.8 | 25,443 | 40–80 | 1266 (461) | 2606 | 769 | 919 |
| 2000–2002 | |||||||
| HEALS (males) | 6.6 ± 1.1 | 4884 | 20–75 | 2806 (967) | 284 | 45 | 130 |
| HEALS (females) | 6.6 ± 0.8 | 6512 | 17–61 | 2431 (850) | 107 | 14 | 41 |
| 1992–1993 | |||||||
| Seoul (males) | 14.7 ± 1.7 | 13,600 | 25–82 | 2397 (497) | 808 | 424 | 145 |
| 1996–2000 | |||||||
| SWHS (females) | 8.6 ± 1.2 | 74,933 | 40–71 | 1634 (496) | 2908 | 1346 | 804 |
| 1990–1992 | |||||||
| CVDFACTS (males) | 14.9 ± 3.6 | 1512 | 18–92 | 2325 (943) | 332 | 80 | 93 |
| CVDFACTS (females) | 15.6 ± 2.7 | 1960 | 18–87 | 1716 (667) | 251 | 73 | 66 |
| Total | 24,283 | 9558 | 6373 |
CVD, cardiovascular disease; CVDFACTS, Cardiovascular Diseases Risk Factor Two-Township Study; HEALS, Health Effects of Arsenic Longitudinal Study; JPHC, Japan Public Health Center-Based Prospective Study; Miyagi, Miyagi Cohort Study; Ohsaki, Ohsaki National Health Insurance Cohort Study; Seoul, Seoul Male Cohort Study; SWHS, Shanghai Women's Health Study.
All values are means ± SDs.
All values are medians; IQRs in parentheses.
TABLE 2.
Meat intake and number of food items in the cohort studies included1
| Study and sex | Red meat2 | Number of food items | Poultry2 | No. of food items | Fish and seafood2 | No. of food items |
| g/d | g/d | g/d | ||||
| JPHC1 (males) | 33.8 ± 19.8 | 4 | 12.7 ± 9.0 | 1 | 52.8 ± 34.3 | 4 |
| JPHC1 (females) | 26.9 ± 17.0 | 11.3 ± 7.6 | 45.3 ± 29.7 | |||
| JPHC2 (males) | 17.8 ± 11.8 | 4 | 8.5 ± 8.1 | 1 | 58.1 ± 38.3 | 6 |
| JPHC2 (females) | 15.1 ± 10.2 | 7.1 ± 6.6 | 45.1 ± 28.8 | |||
| Miyagi (males) | 14.7 ± 12.0 | 4 | 7.9 ± 8.3 | 1 | 58.7 ± 35.3 | 3 |
| Miyagi (females) | 11.1 ± 9.1 | 6.5 ± 6.2 | 52.5 ± 30.1 | |||
| Ohsaki (males) | 14.2 ± 12.0 | 4 | 8.7 ± 8.4 | 1 | 62.8 ± 35.7 | 3 |
| Ohsaki (females) | 9.9 ± 8.7 | 6.9 ± 6.3 | 55.7 ± 30.6 | |||
| HEALS (males) | 19.1 ± 33.0 | 1 | 4.6 ± 14.0 | 1 | 60.3 ± 42.0 | 4 |
| HEALS (females) | 12.2 ± 19.8 | 2.8 ± 9.7 | 51.2 ± 38.1 | |||
| Seoul (males) | 92.3 ± 109.1 | 7 | 4.9 ± 9.0 | 1 | 50.6 ± 58.8 | 9 |
| SWHS (females) | 50.9 ± 36.7 | 9 | 15.3 ± 17.8 | 2 | 38.0 ± 36.8 | 5 |
| CVDFACTS (males) | 67.1 ± 67.0 | 8 | 22.3 ± 34.9 | 2 | 45.2 ± 53.7 | 3 |
| CVDFACTS (females) | 45.0 ± 39.7 | 15.4 ± 21.4 | 36.6 ± 37.2 | |||
| Total |
CVDFACTS, Cardiovascular Diseases Risk Factor Two-Township Study; HEALS, Health Effects of Arsenic Longitudinal Study; JPHC, Japan Public Health Center-Based Prospective Study; Miyagi, Miyagi Cohort Study; Ohsaki, Ohsaki National Health Insurance Cohort Study; Seoul, Seoul Male Cohort Study; SWHS, Shanghai Women's Health Study.
All values are means ± SDs.
Higher total meat intake was not associated with a higher risk of all-cause, cancer, or CVD mortality in either men or women (Table 3). In men, HRs (95% CIs) for the comparison of the highest with the lowest quartile were 1.02 (0.91, 1.15; P-trend = 0.82) for all mortality, 1.11 (0.94, 1.30; P-trend = 0.25) for cancer mortality, and 0.91 (0.78, 1.05; P-trend = 0.29) for CVD mortality. In women, HRs (95% CIs) for the comparison of the highest with the lowest quartile were 0.93 (0.86, 1.01; P-trend = 0.25) for all mortality, 0.90 (0.78, 1.04; P-trend = 0.27) for cancer mortality, and 1.02 (0.89, 1.18; P-trend = 0.80) for CVD mortality. Red meat intake appeared to be related to all-cause mortality in men and women with the lowest risk in the third quartile. A significant inverse trend with red meat intake was observed for CVD mortality in men (P-trend = 0.04) and cancer mortality in women (P-trend < 0.01). An inverse association with poultry intake was observed for risk of all-cause mortality in men (P-trend = 0.02) and women (P-trend = 0.03) and for risk of cancer mortality in women (P-trend < 0.01). Fish/seafood intake was inversely associated with risks of all-cause and CVD mortality in women (P-trend = 0.05 and 0.04, respectively).
TABLE 3.
HRs and 95% CIs for all-cause, cancer, and CVD mortality by meat intake1
| HR (95% CI) |
|||
| All-cause mortality | Cancer mortality | CVD mortality | |
| Men | |||
| No. of deaths | 14,326 | 5610 | 3579 |
| Total meat | |||
| Q1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Q2 | 0.95 (0.89, 1.01) | 0.99 (0.91, 1.08) | 0.87 (0.75, 1.00) |
| Q3 | 0.93 (0.85, 1.03)* | 1.01 (0.91, 1.13) | 0.91 (0.79, 1.04) |
| Q4 | 1.02 (0.91, 1.15)† | 1.11 (0.94, 1.30)† | 0.91 (0.78, 1.05) |
| P-trend | 0.82 | 0.25 | 0.29 |
| Red meat | |||
| Q1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Q2 | 0.94 (0.88, 1.00) | 0.95 (0.85, 1.05) | 0.89 (0.79, 0.99) |
| Q3 | 0.86 (0.80, 0.93) | 0.87 (0.78, 0.96) | 0.87 (0.79, 0.97) |
| Q4 | 0.93 (0.84, 1.02)† | 0.90 (0.77, 1.05)* | 0.87 (0.78, 0.98) |
| P-trend | 0.06 | 0.09 | 0.04 |
| Poultry | |||
| T1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| T2 | 0.88 (0.83, 0.93) | 0.93 (0.84, 1.02) | 0.82 (0.66, 1.02)* |
| T3 | 0.89 (0.81, 0.98) | 0.91 (0.80, 1.04) | 0.82 (0.64, 1.06)* |
| P-trend | 0.02 | 0.17 | 0.14 |
| Fish | |||
| Q1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Q2 | 0.98 (0.89, 1.08)* | 1.02 (0.90, 1.15) | 0.99 (0.82, 1.20)* |
| Q3 | 0.98 (0.89, 1.08)* | 1.04 (0.96, 1.13) | 0.96 (0.79, 1.15)* |
| Q4 | 1.05 (0.95, 1.16)† | 1.14 (1.04, 1.26) | 0.95 (0.80, 1.13) |
| P-trend | 0.43 | 0.02 | 0.50 |
| Women | |||
| No. of deaths | 9957 | 3948 | 2794 |
| Total meat | |||
| Q1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Q2 | 0.88 (0.82, 0.94) | 0.92 (0.78, 1.08) | 0.88 (0.78, 0.99) |
| Q3 | 0.91 (0.82, 1.02) | 0.96 (0.79, 1.17)* | 0.88 (0.74, 1.04) |
| Q4 | 0.93 (0.86, 1.01) | 0.90 (0.78, 1.04) | 1.02 (0.89, 1.18) |
| P-trend | 0.25 | 0.27 | 0.80 |
| Red meat | |||
| Q1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Q2 | 0.93 (0.87, 0.98) | 0.92 (0.82, 1.04) | 0.93 (0.82, 1.06) |
| Q3 | 0.88 (0.81, 0.95) | 0.83 (0.74, 0.92) | 0.86 (0.75, 0.99) |
| Q4 | 0.93 (0.86, 1.00) | 0.85 (0.76, 0.94) | 1.03 (0.85, 1.25) |
| P-trend | 0.05 | <0.01 | 0.99 |
| Poultry | |||
| T1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| T2 | 0.91 (0.85, 0.97) | 0.91 (0.83, 1.01) | 0.97 (0.85, 1.09) |
| T3 | 0.93 (0.86, 0.99) | 0.88 (0.79, 0.97) | 1.05 (0.92, 1.18) |
| P-trend | 0.03 | <0.01 | 0.49 |
| Fish | |||
| Q1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Q2 | 0.86 (0.75, 0.98) | 0.97 (0.80, 1.17) | 0.84 (0.75, 0.94) |
| Q3 | 0.89 (0.83, 0.96) | 1.01 (0.81, 1.28)† | 0.79 (0.68, 0.91) |
| Q4 | 0.91 (0.85, 0.97) | 1.00 (0.83, 1.20) | 0.88 (0.77, 1.01) |
| P-trend | 0.05 | 0.92 | 0.04 |
Values were adjusted for age, BMI, education, smoking habit, rural/urban residence, alcohol intake, fruit and vegetable intake, and total energy intake. *P value for homogeneity across studies rejected at α < 0.05. †P value for homogeneity across studies rejected at α < 0.01. CVD, cardiovascular disease; Q, quartile; ref, reference; T, tertile.
In further analyses, we included 2 more cohort studies (Korean Multi-Center Cancer Cohort Study and Radiation Effects Research Foundation), which assessed diet using nonquantitative FFQs. We examined whether there were similar associations between frequencies of meat intake and all-cause, cancer, and CVD mortality. Similar to the results in the analysis of grams per day, we found no statistically significant associations for total meat intake with frequency of total meat consumption as the main exposure (data not shown). Furthermore, when we used common cutoffs rather than cohort-specific cutoffs to construct intake quartiles, the results were similar for total meat intake (data not shown). When we examined the associations for intakes of total meat, red meat, poultry, and fish in individual cohort studies, we found generally similar patterns with pooled results (see Supplemental Table 2 under “Supplemental data” in the online issue). Because socioeconomic status may have been linked to meat availability during the study period, we investigated whether associations varied by educational level (less than secondary, secondary, and more than secondary graduate) (Table 4). We found no statistically significant associations for all-cause mortality with total meat intake in any education stratum. For red meat intake, a lower risk of all-cause mortality was observed at the second and third quartiles in women with less than secondary school education. When we stratified BMI into 3 groups (BMI <20, 20 to <25, and ≥25), we found similar associations between total meat intake and all-cause mortality in both men and women. A comparison of the highest with the lowest quartile resulted in HRs (95% CIs) of 1.10 (0.94, 1.28) for men with a BMI <20, 1.01 (0.88, 1.16) for men with a BMI of 20 to <25, and 1.01 (0.82, 1.24) for men with a BMI ≥25; the respective values for women were 0.85 (0.70, 1.04) for women with a BMI <20, 1.00 (0.84, 1.18) for women with a BMI of 20 to <25, and 0.91 (0.77, 1.06) for women with a BMI ≥25. When we limited our analysis to never-smokers, HRs for total meat intake in relation to all-cause mortality in a comparison of the highest with the lowest quartile were 1.12 (0.97, 1.29) in men and 0.94 (0.87, 1.02) in women. We also found that baseline period (before or after 1995) did not modify any of the associations between total meat, red meat, poultry, or fish/seafood and risk of all-cause mortality (data not shown). When we excluded participants who died within the first 3 y of follow-up, we found that the results of total meat, red meat, poultry, or fish/seafood were similar for all-cause, cancer, and CVD mortality (data not shown).
TABLE 4.
HRs and 95% CIs for all-cause mortality by meat intake, stratified by educational level1
| Education |
|||
| Low | Middle | High | |
| Men | |||
| No. of deaths | 5477 | 3102 | 1126 |
| Total meat | |||
| Q1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Q2 | 0.98 (0.84, 1.14) | 0.97 (0.86, 1.08) | 0.97 (0.81, 1.16) |
| Q3 | 1.07 (0.93, 1.22) | 0.83 (0.68, 1.00) | 1.10 (0.88, 1.37) |
| Q4 | 1.05 (0.86, 1.30)* | 1.07 (0.89, 1.28) | 1.10 (0.86, 1.40) |
| P-trend | 0.45 | 0.91 | 0.33 |
| Red meat | |||
| Q1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Q2 | 0.95 (0.86, 1.04) | 0.96 (0.87, 1.07) | 1.06 (0.90, 1.26) |
| Q3 | 0.91 (0.80, 1.04) | 0.83 (0.68, 1.03) | 0.87 (0.72, 1.05) |
| Q4 | 0.97 (0.85, 1.11) | 0.94 (0.78, 1.14)* | 0.93 (0.69, 1.26) |
| P-trend | 0.59 | 0.29 | 0.38 |
| Poultry | |||
| T1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| T2 | 0.88 (0.79, 0.99) | 0.89 (0.79, 1.00) | 0.77 (0.63, 0.94) |
| T3 | 0.94 (0.84, 1.04) | 0.97 (0.86, 1.10) | 0.89 (0.74, 1.08) |
| P-trend | 0.22 | 0.64 | 0.24 |
| Fish | |||
| Q1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Q2 | 0.99 (0.87, 1.13) | 0.98 (0.82, 1.17) | 1.14 (0.86, 1.50) |
| Q3 | 1.02 (0.89, 1.16) | 0.97 (0.82, 1.16) | 1.14 (0.82, 1.60)* |
| Q4 | 1.11 (0.97, 1.28) | 1.01 (0.81, 1.26) | 1.21 (0.89, 1.64) |
| P-trend | 0.19 | 0.95 | 0.17 |
| Women | |||
| No. of deaths | 4663 | 1928 | 985 |
| Total meat | |||
| Q1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Q2 | 0.89 (0.80, 0.98) | 0.84 (0.71, 1.00) | 1.03 (0.84, 1.26) |
| Q3 | 0.97 (0.85, 1.11) | 0.86 (0.71, 1.04) | 1.11 (0.90, 1.38) |
| Q4 | 0.98 (0.88, 1.10) | 0.88 (0.73, 1.06) | 1.09 (0.88, 1.37) |
| P-trend | 0.85 | 0.26 | 0.36 |
| Red meat | |||
| Q1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Q2 | 0.89 (0.81, 0.97) | 0.88 (0.76, 1.02) | 1.13 (0.92, 1.37) |
| Q3 | 0.84 (0.76, 0.93) | 0.87 (0.73, 1.03) | 1.07 (0.87, 1.31) |
| Q4 | 0.95 (0.84, 1.07) | 0.84 (0.69, 1.01) | 1.11 (0.90, 1.38) |
| P-trend | 0.29 | 0.09 | 0.44 |
| Poultry | |||
| T1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| T2 | 0.92 (0.84, 1.01) | 0.82 (0.70, 0.96) | 0.97 (0.79, 1.21) |
| T3 | 0.94 (0.86, 1.04) | 0.88 (0.73, 1.08) | 1.06 (0.87, 1.30) |
| P-trend | 0.26 | 0.22 | 0.55 |
| Fish | |||
| Q1 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| Q2 | 0.90 (0.82, 0.98) | 0.81 (0.65, 1.01) | 1.06 (0.87, 1.30) |
| Q3 | 0.89 (0.70, 1.12)* | 0.84 (0.71, 1.00) | 1.07 (0.88, 1.31) |
| Q4 | 0.98 (0.88, 1.08) | 0.89 (0.70, 1.12) | 0.96 (0.77, 1.19) |
| P-trend | 0.68 | 0.35 | 0.98 |
Values were adjusted for age, BMI, smoking habit, rural/urban residence, alcohol intake, fruit and vegetable intake, and total energy intake. Educational levels were categorized into: less than secondary; secondary; and more than secondary school. Japan Public Health Center-Based Prospective Study 2 and Health Effects of Arsenic Longitudinal Study were excluded from these analyses because educational level was not available. *P value for homogeneity across studies rejected at α < 0.05. Q, quartile; ref, reference; T, tertile.
DISCUSSION
Even with the marked increase in industrialization and urbanization in Asian countries, food-availability data from FAO indicated that meat consumption was still substantially higher in the United States than in any Asian country. The main differences between meat consumption in the United States and Asia were seen for beef and poultry. Even though meat consumption has continued to rise in China, Japan, and South Korea and even though the gap between the United States and Asian countries has narrowed, meat consumption in Asia has remained lower than that in the United States into the 21st century. In contrast, fish and seafood consumption in Japan and Korea is >2-fold that in the United States.
Our pooled analysis of 8 Asian prospective cohort studies did not provide evidence of a higher risk of mortality for total meat intake. For red meat and poultry, inverse associations were observed for mortality in both men and women. We found that fish intake was inversely associated with risk of mortality in women. No variation in the associations between mortality and total meat intake were observed by educational levels or study period.
Overall cancer and CVD mortality has increased in Asian countries (24–26), and mortality rates from some cancers are approaching those in Western countries (24, 27). Given the trend of increasing meat consumption over time in Asia, a westernized diet heavy in animal products has been invoked as a cause of this increasing incidence and mortality from cancer and CVD (28). However, Asian prospective cohort studies (29–33), most of which were included in our pooled analysis, have not supported the hypothesis that meat intake is involved in all-cause, cancer, or CVD mortality, unlike the pattern seen in Europe and North America (5, 6, 34, 35).
The absence of a positive association between meat intake and mortality in Asia may be related to several factors. First, Asia has been experiencing a dramatic change in many other chronic disease risk factors, including physical activity, adiposity, and access to medical care. At this stage, it is possible that meat consumption may not be as large a contributor to risk of death as socioeconomic status, a sedentary lifestyle (36, 37), or adiposity. Furthermore, other risk factors such as obesity (12), hypertension (38), and smoking (39) could largely explain the increasing risks of cancer or CVD in Asia to date. Second, the null, and even inverse, association between meat consumption and mortality observed in our data warrants further study because the dietary transition is still under way in many parts of Asia. Residual or unmeasured confounding factors, such as socioeconomic status related to meat availability, could be important because food accessibility and availability is related to income levels in the Asia-Pacific region (40); ie, even though we failed to detect differences by education, a higher intake of meat at this point in the epidemiologic transition may be a marker for other protective factors, including a sufficient intake of energy and access to medical care. Third, nondifferential measurement error in dietary assessments could have led to bias toward the null, although all the FFQs used in each study have been validated with modest to good correlation with a reference method (13–18). Although the absence of a positive association can be partly explained by aforementioned reasons, we still cannot rule out the hypothesis that total meat intake is not related to mortality in Asian populations, given the findings we observed in this pooled analysis.
A reduced risk of all-cause and cancer mortality with higher fish intakes in women could be explained as a result of delayed progression of disease through inhibition of eicosanoid biosynthesis, which leads to a reduction in prostaglandin conversion from arachidonic acid (41, 42). We found an inverse association in women only, perhaps because social and cultural differences between men and women determine health behaviors such as alcohol intake and tobacco smoking in Asia; therefore, these risk factors could play a role to a lesser extent in women than in men.
The strengths of our study include the size of the total ACC cohort and a prospective study design with assessment of long-term usual dietary intake. In the ACC study, we were able to include unpublished individual data from some Asian studies, which provides greater accuracy than meta-analyses. We had extensive information on potential confounders. Furthermore, we analyzed the data and adjusted for confounding factors in a standardized, uniform way by using the original data from each cohort, which is not allowed in a meta-analysis.
Our study had several limitations. Unmeasured or residual confounding may still exist, although we adjusted for potential confounding factors, including alcohol intake, fruit and vegetable intake, education, and smoking status. We did not analyze processed meat intake because a limited number of processed meats were included in the FFQs. We could not evaluate whether meat preparation or cooking procedures were associated with risk of mortality because most of the cohorts did not include such detailed information in their questionnaires. We were not able to examine changes in meat intake or timing of meat intake in relation to mortality because dietary information was not assessed at multiple times during the study period of each cohort. Heterogeneity in intake was observed across studies; however, we found that study-specific results in general did not show an increased risk of mortality with higher total meat intake. We could not investigate the role of meat intake with specific types of CVD and cancer outcomes because we did not have the relevant information from the different cohorts. However, our finding warrants subsequent studies to explore the role of diet in the development of specific CVD or cancer outcomes in this ACC study.
In conclusion, our pooled analysis of prospective cohort studies showed that higher total and red meat consumption was not associated with an increased risk of cancer or CVD mortality. Fish and seafood intake was inversely associated with mortality in women. Additional dietary studies among Asian populations are needed to elucidate outstanding questions: 1) Is meat intake associated with an increased risk of cancer and CVD mortality beyond changes in lifestyle and environmental factors?; 2) Do some, as yet undefined, characteristics of Asian populations explain the association that we observed with meat intake?; and 3) Is the cumulative exposure to a high intake of meat crucial to disease etiology?
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—K-YY, PB, WZ, DK, JP, and RS: conceived the study; JEL, DFM, and RS: designed the research; JEL and RS: drafted the manuscript; DFM: analyzed the data; and all authors: revised the manuscript and approved the final manuscript. None of the authors declared a conflict of interest. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Abbreviations used: ACC, Asia Cohort Consortium; CVD, cardiovascular disease; FFQ, food-frequency questionnaire.
REFERENCES
- 1.Popkin BM. The nutrition transition and obesity in the developing world. J Nutr 2001;131:871S–3S [DOI] [PubMed] [Google Scholar]
- 2.Gill T. Epidemiology and health impact of obesity: an Asia Pacific perspective. Asia Pac J Clin Nutr 2006;15(suppl):3–14 [PubMed] [Google Scholar]
- 3.World Health Organization The global burden of disease: 2004 update. Geneva, Switzerland: World Health Organization, 2008 [Google Scholar]
- 4.Food and Agriculture Organization of the United Nations The state of food and agriculture. Rome, Italy: Food and Agriculture Organization of the United Nations, 2009 [Google Scholar]
- 5.Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Stampfer MJ, Willett WC, Hu FB. Red meat consumption and mortality: results from 2 prospective cohort studies. Arch Intern Med 2012;172:555–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sinha R, Cross AJ, Graubard BI, Leitzmann MF, Schatzkin A. Meat intake and mortality: a prospective study of over half a million people. Arch Intern Med 2009;169:562–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cross AJ, Sinha R. Meat-related mutagens/carcinogens in the etiology of colorectal cancer. Environ Mol Mutagen 2004;44:44–55 [DOI] [PubMed] [Google Scholar]
- 8.Sinha R, Knize MG, Salmon CP, Brown ED, Rhodes D, Felton JS, Levander OA, Rothman N. Heterocyclic amine content of pork products cooked by different methods and to varying degrees of doneness. Food Chem Toxicol 1998;36:289–97 [DOI] [PubMed] [Google Scholar]
- 9.Hughes R, Cross AJ, Pollock JR, Bingham S. Dose-dependent effect of dietary meat on endogenous colonic N-nitrosation. Carcinogenesis 2001;22:199–202 [DOI] [PubMed] [Google Scholar]
- 10. Food and Agriculture Organization of the United Nations. FAO statistical databases (FAOSTAT). Food consumption data. Rome, Italy: FAO, 2012.
- 11.Speedy AW. Global production and consumption of animal source foods. J Nutr 2003;133:4048S–53S [DOI] [PubMed] [Google Scholar]
- 12.Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K, He J, Gupta PC, Ramadas K, Tsugane S, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med 2011;364:719–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shu XO, Yang G, Jin F, Liu D, Kushi L, Wen W, Gao YT, Zheng W. Validity and reproducibility of the food frequency questionnaire used in the Shanghai Women's Health Study. Eur J Clin Nutr 2004;58:17–23 [DOI] [PubMed] [Google Scholar]
- 14.Kim MK, Lee SS, Ahn YO. Reproducibility and validity of a self-administered semiquantitative food frequency questionnaire. Korean J Commun Nutr. 1996;1:376–94 [Google Scholar]
- 15.Tsubono Y, Kobayashi M, Sasaki S, Tsugane S. Validity and reproducibility of a self-administered food frequency questionnaire used in the baseline survey of the JPHC Study Cohort I. J Epidemiol 2003;13:S125–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ogawa K, Tsubono Y, Nishino Y, Watanabe Y, Ohkubo T, Watanabe T, Nakatsuka H, Takahashi N, Kawamura M, Tsuji I, et al. Validation of a food-frequency questionnaire for cohort studies in rural Japan. Public Health Nutr 2003;6:147–57 [DOI] [PubMed] [Google Scholar]
- 17.Chen Y, Ahsan H, Parvez F, Howe GR. Validity of a food-frequency questionnaire for a large prospective cohort study in Bangladesh. Br J Nutr 2004;92:851–9 [DOI] [PubMed] [Google Scholar]
- 18.Lee MS, Pan WH, Liu KL, Yu MS. Reproducibility and validity of a Chinese food frequency questionnaire used in Taiwan. Asia Pac J Clin Nutr 2006;15:161–9 [PubMed] [Google Scholar]
- 19.Yoo KY, Shin HR, Chang SH, Lee KS, Park SK, Kang D, Lee DH. Korean Multi-center Cancer Cohort Study including a Biological Materials Bank (KMCC-I). Asian Pac J Cancer Prev 2002;3:85–92 [PubMed] [Google Scholar]
- 20.Preston DL, Pierce DA, Shimizu Y, Cullings HM, Fujita S, Funamoto S, Kodama K. Effect of recent changes in atomic bomb survivor dosimetry on cancer mortality risk estimates. Radiat Res 2004;162:377–89 [DOI] [PubMed] [Google Scholar]
- 21.Chao A, Thun MJ, Connell CJ, McCullough ML, Jacobs EJ, Flanders WD, Rodriguez C, Sinha R, Calle EE. Meat consumption and risk of colorectal cancer. JAMA 2005;293:172–82 [DOI] [PubMed] [Google Scholar]
- 22.Cross AJ, Leitzmann MF, Gail MH, Hollenbeck AR, Schatzkin A, Sinha R. A prospective study of red and processed meat intake in relation to cancer risk. PLoS Med 2007;4:e325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Willett WC, Hu FB. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr 2011;94:1088–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008 v1.2, cancer incidence and mortality worldwide: IARC CancerBase no. 10. Lyon, France: International Agency for Research on Cancer, 2010 [Google Scholar]
- 25.Ramahi TM. Cardiovascular disease in the Asia Middle East region: global trends and local implications. Asia Pac J Public Health 2010;22:83S–9S [DOI] [PubMed] [Google Scholar]
- 26.Sasayama S. Heart disease in Asia. Circulation 2008;118:2669–71 [DOI] [PubMed] [Google Scholar]
- 27.American Cancer Society Global cancer facts & figures. 2nd ed. Atlanta, GA: ACS, 2011 [Google Scholar]
- 28.Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nutr Rev 1997;55:31–43 [DOI] [PubMed] [Google Scholar]
- 29.Kojima M, Wakai K, Tamakoshi K, Tokudome S, Toyoshima H, Watanabe Y, Hayakawa N, Suzuki K, Hashimoto S, Ito Y, et al. Diet and colorectal cancer mortality: results from the Japan Collaborative Cohort Study. Nutr Cancer 2004;50:23–32 [DOI] [PubMed] [Google Scholar]
- 30.Lee SA, Shu XO, Yang G, Li H, Gao YT, Zheng W. Animal origin foods and colorectal cancer risk: a report from the Shanghai Women's Health Study. Nutr Cancer 2009;61:194–205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khan MM, Goto R, Kobayashi K, Suzumura S, Nagata Y, Sonoda T, Sakauchi F, Washio M, Mori M. Dietary habits and cancer mortality among middle aged and older Japanese living in hokkaido, Japan by cancer site and sex. Asian Pac J Cancer Prev 2004;5:58–65 [PubMed] [Google Scholar]
- 32.Sato Y, Nakaya N, Kuriyama S, Nishino Y, Tsubono Y, Tsuji I. Meat consumption and risk of colorectal cancer in Japan: the Miyagi Cohort Study. Eur J Cancer Prev 2006;15:211–8 [DOI] [PubMed] [Google Scholar]
- 33.Nagao M, Iso H, Yamagishi K, Date C, Tamakoshi A. Meat consumption in relation to mortality from cardiovascular disease among Japanese men and women. Eur J Clin Nutr 2012;66:687–93 [DOI] [PubMed] [Google Scholar]
- 34.Kelemen LE, Kushi LH, Jacobs DR, Jr, Cerhan JR. Associations of dietary protein with disease and mortality in a prospective study of postmenopausal women. Am J Epidemiol 2005;161:239–49 [DOI] [PubMed] [Google Scholar]
- 35.Couto E, Boffetta P, Lagiou P, Ferrari P, Buckland G, Overvad K, Dahm CC, Tjonneland A, Olsen A, Clavel-Chapelon F, et al. Mediterranean dietary pattern and cancer risk in the EPIC cohort. Br J Cancer 2011;104:1493–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pham NM, Mizoue T, Tanaka K, Tsuji I, Tamakoshi A, Matsuo K, Ito H, Wakai K, Nagata C, Sasazuki S, et al. Physical activity and colorectal cancer risk: an evaluation based on a systematic review of epidemiologic evidence among the Japanese population. Jpn J Clin Oncol 2012;42:2–13 [DOI] [PubMed] [Google Scholar]
- 37.Noda H, Iso H, Toyoshima H, Date C, Yamamoto A, Kikuchi S, Koizumi A, Kondo T, Watanabe Y, Wada Y, et al. Walking and sports participation and mortality from coronary heart disease and stroke. J Am Coll Cardiol 2005;46:1761–7 [DOI] [PubMed] [Google Scholar]
- 38.Murakami Y, Hozawa A, Okamura T, Ueshima H. Evidence for Cardiovascular Prevention From Observational Cohorts in Japan Research Group. Relation of blood pressure and all-cause mortality in 180,000 Japanese participants: pooled analysis of 13 cohort studies. Hypertension 2008;51:1483–91 [DOI] [PubMed] [Google Scholar]
- 39.Nakamura K, Huxley R, Ansary-Moghaddam A, Woodward M. The hazards and benefits associated with smoking and smoking cessation in Asia: a meta-analysis of prospective studies. Tob Control 2009;18:345–53 [DOI] [PubMed] [Google Scholar]
- 40.Yang RY, Hanson PM. Improved food availability for food security in Asia-Pacific region. Asia Pac J Clin Nutr 2009;18:633–7 [PubMed] [Google Scholar]
- 41.Rose DP, Connolly JM. Omega-3 fatty acids as cancer chemopreventive agents. Pharmacol Ther 1999;83:217–44 [DOI] [PubMed] [Google Scholar]
- 42.Tapiero H, Ba GN, Couvreur P, Tew KD. Polyunsaturated fatty acids (PUFA) and eicosanoids in human health and pathologies. Biomed Pharmacother 2002;56:215–22 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.