Abstract
The accuracy of 6 resting metabolic rate (RMR) prediction equations to indirect calorimetry was compared in 38 Hispanic women (age = 30 ± 7 years; body mass index = 28.9 ± 7.2 kg/m2; body fat = 42% ± 8%). Paired t tests examined differences between predicted and measured RMR; significance defined as P < 0.05. Bias and agreement were displayed using Bland-Altman plots. Accuracy was defined when the predicted RMR was ± 10% of the measured RMR. Data were analyzed with SPSS (version 19). Only the equation of Owen et al was not significantly different from the measured RMR (1336 ± 142 and 1322 ± 203 kcal/d, respectively). The equation of Owen et al was accurate for 84.2% of women; RMR prediction equations had limited applicability for young Hispanic women.
Keywords: Hispanic women, prediction equations, resting metabolic rate
ACCURATE RESTING METABOLIC RATE (RMR) measurements are imperative for assessing weight status, monitoring weight loss, planning effective treatment procedures, and optimizing treatment outcomes.1 The RMR is the energy necessary to support physiologic function and sustain body temperature while at rest.2 Several variables, including body composition,3 weight,4 heart rate,4 age,3,4 sex,3,5 menstrual cycle,6 smoking status,4 and caffeine intake,7 influence the RMR in healthy individuals. Given the high prevalence of obesity and associated chronic health conditions among Americans, accurate RMR determination is necessary.
Some controversy in the literature remains regarding the distinction between the RMR and the basal metabolic rate (BMR),8 and, in some cases, the terms are used interchangeably. Similar to the RMR, the BMR is typically the largest component of daily energy expenditure in healthy sedentary adults and represents the energy required to maintain body system function and temperature while at rest.9 Although both RMR and BMR represent the metabolic rate of participants in a rested and fasted state, BMR measurements are obtained shortly after participants wake, following an overnight stay in a metabolic chamber or research facility, thereby limiting ambulation prior to measurement.10 In contrast, the RMR is measured after participants arrive to the testing facility the morning of measurement10 and is slightly higher than the BMR.
Clinicians consider indirect calorimetry the “gold standard” for metabolic rate measurement; however, instrument costs frequently interfere with the use in the clinical setting.11 Prediction equations are commonly considered as a cost- and time-effective alternative method to estimate the BMR/RMR and determine energy requirements. Although, in theory, prediction equations offer clinicians a convenient method to estimate the BMR/RMR of patients, the identification of a single equation that yields consistent results among diverse populations remains elusive.1
In some cases, research describing the derivation of BMR/RMR prediction equations is unclear about whether the metabolic rate measurement protocols used established basal or resting conditions. While such studies refer to the equations as predictors of the BMR, review of the original research suggests that basal conditions may not have been achieved since the participants did not sleep at the laboratory prior to the measurement. Such methodological discrepancies have led researchers to make various suggestions regarding which metabolic rate prediction equations should be considered determinants of the BMR or RMR.4,8
Formulation of metabolic rate prediction equations has been an ongoing and controversial process for more than 1 century. While a multitude of equations are available for use (Table 1), research is currently being conducted to identify the best equation for use in clinical settings. Results from each prediction equation reflect the characteristics of the participants from which the equation was derived1; therefore, clinical application of the prediction equations to groups differing from the original participants may not be appropriate. For example, the Harris-Benedict equation,12 one of the earliest and most studied of the prediction equations,21 included predominantly normal weight participants who represented the American population of the early 1900s.12 Historically, the Harris-Benedict equation was used in clinical settings; however, several studies have reported that this equation overestimates metabolic rate1,18,19,22-24 and may not provide the most accurate predictions for the current general population. Approximately 60 years following the introduction of the Harris-Benedict equation, another prediction equation, the Cunningham equation,14 was developed from body mass, age, and height data, using select participants of the Harris-Benedict study. The Cunningham equation14 reflects the characteristics of the original Harris-Benedict participants; however, it uses lean body mass (LBM) as the primary predictor of metabolic rate. In contrast, the Robertson and Reid equation13 was developed to take into account age and estimated body surface area for metabolic rate prediction. The equation13 was derived using pooled data of British children, medical students, hospital staff members, and volunteers from the public and included individuals ranging in age from 3 to 80 years. Unfortunately, while the age distribution of the Robertson and Reid study participants was specified, the body weights and the racial/ethnic backgrounds were not reported.13 The database compiled by Schofield16,17 contributed to the prediction equations proposed by the Food and Agricultural Organization/World Health Organization/United Nations University (FAO/WHO/UNU)15 in 1985. This database16,17 reflected the results of an extensive review of study samples of previous metabolic rate research compiled over the course of 60 years and included studies from approximately 23 countries. However, the large proportion of Italian participants represented in the database,16,17 and subsequently used to derive the FAO/WHO/UNU equations,15 may restrict the applicability of these equations to certain races/ethnicities. Most recently, the Owen et al18 and Mifflin-St. Jeor19 equations were independently developed from a sample consisting of a broad spectrum of body weights (43-143 and 46-120 kg, respectively) and ages (18-65 and 20-76 years, respectively). However, the racial/ethnic background of the participants was not provided.18,19
Table 1.
Formulas and Characteristics of 6 Commonly Used RMR Prediction Equations for Women
| Prediction Equation | Formula | Characteristics of Population Included in the Development of Equation |
|---|---|---|
| Harris-Benedict12 | kcal/d = 655.0955 + 9.5634 × weight (kg) + 1.8496 × height (cm) – 4.6756 × age (y) | n = 103 Predominantly normal weight women Weight (mean) = 56.4 kga Weight (range) = 35.6-94.1 kg Age range = 15-74 y No specific racial/ethnic information provided |
| Robertson and Reid13 | kcal/d = BSA (m2)b × 24 × (age-specific value) | n = 1323 Female nurses in training at Middlesex Hospital, England, medical students, and other hospital staff, children attending welfare clinics and on tonsillectomy waiting lists, and members of the public who responded to newspaper advertisements Age range = 3-74 y (included men aged up to 80 y) No specific weight information provided No specific racial/ethnic information provided |
| Cunningham14 | kcal/d = 500 + 22 × lean body massc | n = 223 Original participants of the Harris-Benedict study,12 excluding 16 male athletes Weight information was not published Weight (mean)d = 59.8 kg Weight (range)d = 33.2-94.1 kg Age ranged = 15-74 y No specific racial/ethnic information provided Not a gender-specific equation |
| FAO/WHO/UNU15 | 18-30 y: kcal/d = 13.3 × weight (kg) + 334 × height (m) + 35 30-60 y: kcal/d = 8.7 × weight (kg) – 25 × height (m) + 865 >60 y: kcal/d = 9.2 × weight (kg) + 637 × height (m) – 302 |
Developed using data from the Schofield study16,17 n = 11 000 (included men, women, and children) Included healthy adults of varying weights, heights, and ages Multiethnic cohort; included a large number of Italian participants |
| Owen et al18 7.18 × weight (kg) | Nonathletese: kcal/d = 795 + Athletes: kcal/d = 50.4 + 21.1 × weight (kg) | n = 44 (included 8 athletes) Participants represent a wide range of weight categories: underweight (n = 1), normal weight (n = 23), overweight (n = 4), obese (n = 10), and extremely obese (n = 6); excluding athletes: underweight (n = 1), normal weight (n = 15), overweight (n = 4), obese (n = 10), and extremely obese (n = 6) Weight (mean) = 74.9 and 79 kgf (excluding athletes) Weight (range) = 43-143 kg Age range = 18-65 y No specific racial/ethnic information provided |
| Mifflin-St. Jeor19 | kcal/d = 9.99 × weight (kg) + 6.25 × height (cm) – 4.92 × age (y) – 161 | n = 247 Healthy working-class women Participants represented normal weight (n = 135) and obese (n = 112) categories Weight (mean) = 78.9 ± 16.7 kg Weight (range) = 46-120 kg Age range = 20-76 y No specific racial/ethnic information provided |
Abbreviations: BSA, body surface area; FAO/WHO/UNU, Food and Agricultural Organization/World Health Organization/United Nations University; RMR, resting metabolic rate.
Calculated from the original Harris-Benedict study (Table D).12
BSA estimated from stature and body weight by the DuBois and DuBois formula20 : Area (cm2) = Weight (kg)0.425 × Height (cm)0.725 × 71.84.
In the present study, lean body mass was determined by dual-energy x-ray absorptiometric analysis.
Calculated from the original Harris-Benedict study tables (Tables C and D).12
In the present study, the Owen et al equation for nonathletes was used.
Calculated from the Owen et al clinical measurements and body composition table.18
Unfortunately, the aforementioned metabolic rate prediction equations may not be derived from participants with racially/ethnically varied backgrounds. This pattern potentially compromises prediction accuracy, as numerous studies25-29 have reported variability in RMR among different racial/ethnic groups. Early studies conducted by Benedict30 reported differences between the RMR in Asian girls, Mayan men, and South Indian women, in comparison with their non-Hispanic white counterparts. James31 and Schofield16 reported a possible 10% reduction in the RMR of South Asian Indians in comparison with Northern Europeans and Americans. Henry and Reese25 further investigated this observation and identified that the trend may be applicable to other tropical peoples. More recently, validation studies32-37 conducted with different races/ethnicities have indicated that several commonly used equations, such as Harris-Benedict,32-34,36,37 FAO/WHO/UNU,32,34,35 Mifflin-St. Jeor,32,33 and Owen et al,37 may not be appropriate for metabolic rate prediction in certain racial/ethnic groups. Frankenfield and colleagues1 identified that there are disparities in knowledge regarding the applicability of current metabolic rate prediction equations to diverse groups and urge researchers to conduct validation studies for these racial/ethnic populations.
The National Health and Nutrition Examination Survey 2007-200838 reported that a significant proportion of Hispanic men (79.3%) and women (76.1%) older than 20 years are overweight or obese (body mass index [BMI] ≥25 kg/m2), a factor that elevates the risk of developing several chronic diseases. To date, no recommendation has been made about the best metabolic rate prediction equation for Hispanic adults,1,36 and the only studies conducted36,37 suggest that currently available equations provide inaccurate metabolic rate predictions for this group. Further research is needed to assess the impact that race/ethnicity may have on the accuracy of metabolic rate prediction equations.39,40 Therefore, the primary objective of this study was to examine the accuracy of 6 commonly used prediction equations for metabolic rate (Harris-Benedict,12 Robertson and Reid,13 Cunningham,14 FAO/WHO/UNU,15 Owen et al,18 and Mifflin-St. Jeor19) with the measured RMR by indirect calorimetry among a sample of Hispanic women. To ensure consistency in the present analysis, all metabolic rate prediction equations discussed were considered predictors of the RMR.
METHODS
Study design and participant recruitment
This cross-sectional study compared the accuracy of 6 commonly used RMR prediction equations to the measured RMR in a convenience sample of Hispanic women. Procedures were approved by the University Institutional Review Board at Arizona State University and the University Committee on Activities Involving Human Subjects at New York University. All study participants signed an informed consent form.
Forty-four Hispanic women between the ages of 20 and 40 years were recruited from the Phoenix, Arizona, metropolitan area, with flyers posted at libraries, churches, college campuses, and community centers. The flyers, developed by the investigators, provided a brief description of the study and invited potential participants to call the study investigators for additional information. Potential participants were initially screened for eligibility over the telephone. Women were included in the study if they were of Hispanic ethnicity, aged 20 to 40 years, weight stable (defined by no weight fluctuation ≥10% in the past 6 months), less than 300 lb, and nonsmokers (defined by no use of cigars, cigarettes, or other tobacco products in the past 6 months). Hispanic ethnicity was defined for participants who identified themselves, one parent, and both corresponding grandparents as being of Hispanic origin. Participants reported regular menstruation (defined by at least 10 menstrual cycles over the past year) and no pregnancy or lactation in the prior year. In addition, participants were excluded if they reported having unresolved health issues, such as type 2 diabetes mellitus and thyroid disease.
Once eligibility was established over the telephone, participants were invited to the Arizona State University campus for 3 separate visits. During the first visit, participants learned about the study, signed an informed consent form, and completed a health history questionnaire. Participants were provided written and verbal instructions for the RMR measurement and fasting blood draw that were completed during the second visit. Body composition was determined by dual-energy x-ray absorptiometry (DXA) during the third visit. Study visits were scheduled at the convenience of each participant; however, all of the study visits were completed during the course of a year.
Anthropometry
Anthropometric assessments were conducted during the second study visit. Height was measured, without shoes, to the nearest 0.1 cm, using a stadiometer (Seca 214; Seca Corporation, Hanover, Maryland), and weight was measured to the nearest 0.1 kg, using a digital scale (Seca Corporation, Ontario, California). Body mass index (kg/m2) was calculated using the measured height (m) and weight (kg). At the third study visit, all participants completed a body composition assessment by DXA, using the LUNAR DPX-IQ bone densitometer (GE Healthcare, Madison, Wisconsin).
Biochemical analysis
Serum thyroid stimulating hormone (TSH) concentrations were assessed at the second study visit to confirm adequate thyroid function. Eight-hour fasting blood samples were taken by venipuncture, and concentrations were determined, in duplicate, by radioimmunoassay (MP Biomedicals Diagnostics Division, Orangeburg, New York). Participants were excluded from the study if their serum TSH concentration exceeded 6.75 μIU/mL.
Resting metabolic rate measurement and prediction
During the second study visit, the RMR was measured using the Delta Trac II metabolic monitor (Viasys Healthcare, Yorba Linda, California). Measurement procedures for the RMR were consistent with the best practice methods developed by the Academy of Nutrition and Dietetics Evidence Analysis Working Group.41 The metabolic cart was calibrated every morning, before the initial RMR measurement, using a gas mixture of oxygen (95%) and carbon dioxide (5%). Participants were instructed to fast for at least 8 hours and abstain from programmed physical activity42 and caffeine7,43 for 48 and 24 hours, respectively, prior to the RMR measurement. To minimize RMR fluctuations that naturally occur throughout the menstrual cycle,6 the RMR was measured within 1 week after the onset of menses. After resting for at least 20 minutes, each participant completed two 25-minute RMR measurements, which were then averaged. Data collected during the initial 5 minutes of the RMR measurement were discarded. The intra-assay variation for the RMR measurements was 2.9%. The RMR was also calculated with 6 commonly used prediction equations (Table 1): Harris-Benedict,12 Robertson and Reid,13 Cunningham,14 FAO/WHO/UNU,15 Owen et al,18 and Mifflin-St. Jeor.19 The equations were selected because of their use in practice and potential applicability to the study population.
Statistical analysis
Statistical analyses were performed using the Statistical Package for Social Sciences (SPSS), version 19.0 (SPSS Institute, Chicago, Illinois), and descriptive statistics (age, height, weight, BMI, % body fat, TSH, and measured RMR) were expressed as the mean ± standard deviation (SD). The paired t test examined differences between the measured RMR and the predicted RMR, for the 6 equations. Significance was defined as P < .05.
Bias and agreement between the results of each prediction equation and the measured RMR were assessed according to the limits identified by Bland and Altman.44 Bland-Altman plots displayed the calculated mean of the predicted and measured RMRs against the calculated difference between the predicted and measured RMRs for each study participant. The mean difference (predicted RMR – measured RMR) was defined by a solid horizontal line. On the y-axis, the distance of the mean difference line from the zero-difference point visually represented bias. Data points were plotted closest to the zero-difference point for participants whose RMR was most closely predicted to the measured RMR. Two dashed lines, located 2 SD above and below the mean difference line, corresponded to the limits of agreement defined by Bland and Altman.44 For each equation, prediction accuracy was defined as the percentage of participants whose predicted RMR was ± 10% of the measured RMR.
RESULTS
Of the 44 participants who initially signed the consent form, 6 participants did not complete the RMR measurements. A total of 38 Hispanic women finished the study and were included in the final analysis; descriptive characteristics are presented in Table 2. The mean age of participants was 30 ± 7 years (range, 20-40 years) and the mean BMI was 28.9 ± 7.2 kg/m2 (range, 19.7-46.1 kg/m2). Fifteen participants were of normal weight (BMI 18.5-24.9 kg/m2), 11 participants were over-weight (BMI = 25.0-29.9 kg/m2), 8 were obese (BMI = 30.0-39.9 kg/m2), and 4 were severely obese (BMI ≥40.0 kg/m2). Body composition was assessed by DXA; mean percent body fat was 42.0% ± 8.0% (range, 29.0%-55.0%). The mean measured TSH was 1.8 ± 1.0 μIU/mL (range, 0-4.5 μIU/mL) and was within the reference range for all participants. The education level of the participants indicated that, in general, this was a highly educated group; 29 (76.3%) women reported at least attending some college or technical school.
Table 2.
Characteristics of Hispanic Women (N = 38)
| Hispanic Women |
||
|---|---|---|
| Characteristics | Mean ± SD | Range (Minimum-Maximum) |
| Age, y | 30 ± 7 | 20-40 |
| Height, cm | 162 ± 7 | 149-178 |
| Weight, kg | 75 ± 20 | 43-125 |
| BMI, kg/m2 | 28.9 ± 7.2 | 19.7-46.1 |
| Body fat, % | 42 ± 8 | 29-55 |
| TSH, μIU/mL | 1.8 ± 1.0 | 0-4.5 |
| Measured RMR | 1322 ± 203 | 980-1815 |
| n (%) | ||
| Education | ||
| Less than high school | 2 (5.3) | . . . |
| High school graduate or equivalent | 2 (5.3) | . . . |
| Some college or technical school | 17 (44.7) | . . . |
| College graduate | 6 (15.8) | . . . |
| Postbaccalaureate (Master's, doctoral, or professional degree) | 6 (15.8) | . . . |
| Not reported | 5 (13.1) | |
Abbreviations: BMI, body mass index; RMR = resting metabolic rate; expressed in kcal; TSH, thyroid stimulating hormone.
Table 3 depicts the mean RMR calculated by each of the prediction equations and the differences from the RMR value measured by indirect calorimetry. The calculated difference (predicted RMR – measured RMR) assessed which equation predicted the RMR with the least bias. As indicated in Table 3, differences ranged from + 14 kcal (Owen et al) to + 216 kcal (Harris-Benedict); on average, all equations provided overpredictions when compared with the measured RMR. The percentage of difference (difference/measured RMR × 100) ranged from 5.5% (Owen et al) to 17.0% (Harris-Benedict). The paired t test indicated that 5 of the equations (Harris-Benedict, Robertson and Reid, Cunningham, FAO/WHO/UNU, and Mifflin-St. Jeor) significantly overpredicted the RMR (P < .05). The equation of Owen et al was the only equation that provided an RMR prediction that was not significantly different from the measured RMR.
Table 3.
Mean RMR Obtained by Prediction Equations Compared With Mean RMR Obtained by Indirect Calorimetry
| RMRa | Difference (Predicted RMR – Measured RMR), kcal | % Difference (Difference/Measured RMR × 100%) | P | |
|---|---|---|---|---|
| Measured RMR | 1322 ± 203 | . . . | . . . | . . . |
| Harris-Benedict | 1538 ± 190 | + 216 | 17.0 | <.001b |
| Robertson and Reid | 1446 ± 173 | + 124 | 10.5 | <.001b |
| Cunningham | 1444 ± 163 | + 122 | 10.8 | <.001b |
| FAO/WHO/UNU | 1530 ± 225 | + 208 | 16.2 | <.001b |
| Owen et al | 1336 ± 142 | + 14 | 5.5 | NS |
| Mifflin-St. Jeor | 1458 ± 210 | + 136 | 10.7 | <.001b |
Abbreviations: FAO/WHO/UNU, Food and Agricultural Organization/World Health Organization/United Nations University; NS, nonsignificant; RMR, resting metabolic rate; expressed in kcal.
Expressed as mean ± SD.
P < .05.
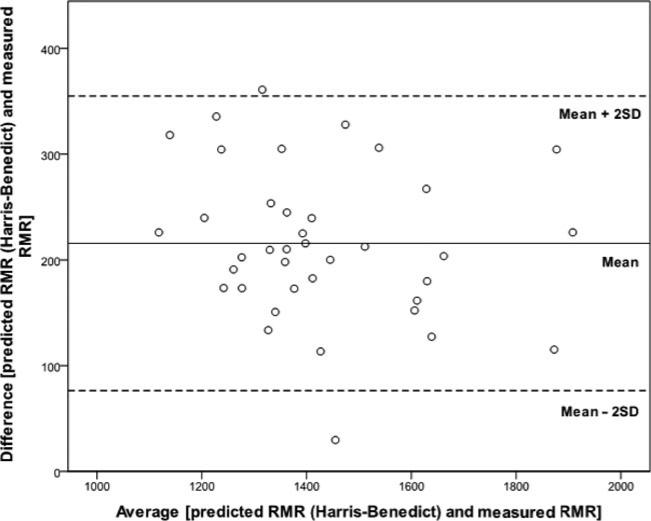
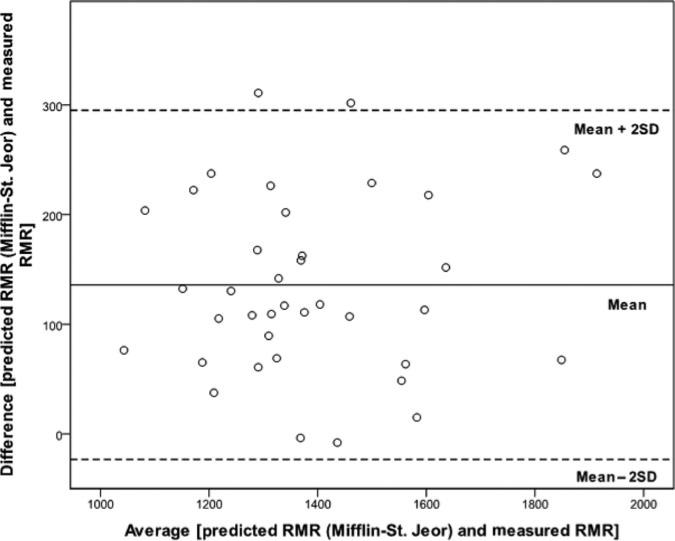
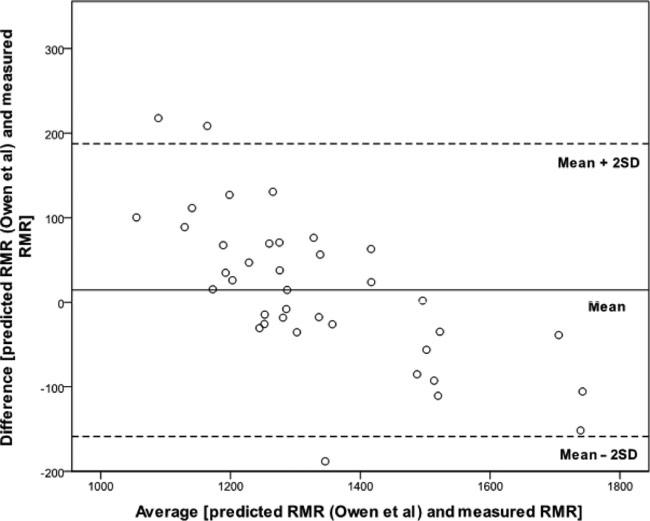
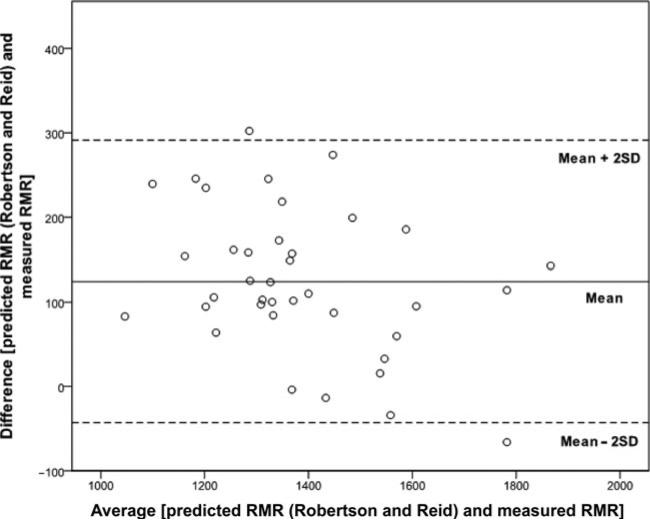
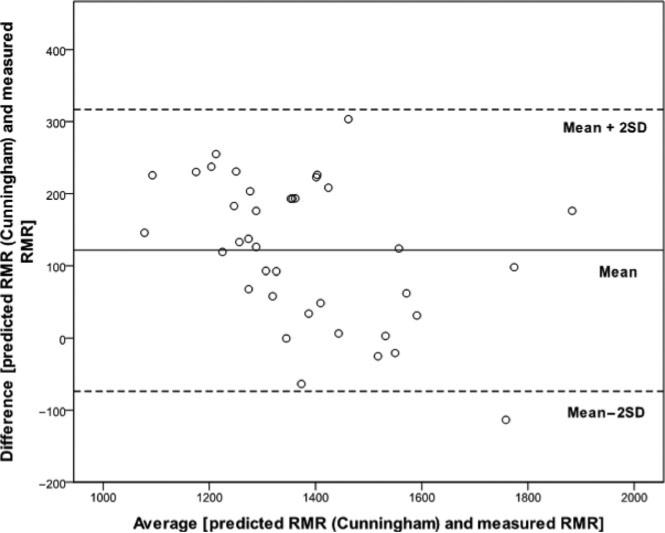
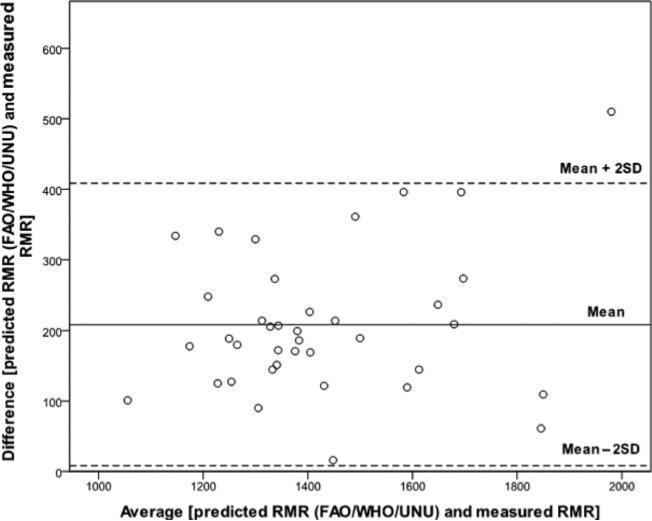
Bland-Altman plots visually supported these results (Figures 1-6). The Owen et al equation provided the least biased RMR prediction, indicated by the close proximity of the mean difference line to the zero-difference point (Figure 5). Data points plotted above the highest limit (mean + 2 SD) represented participants whose RMR was overpredicted. Data points plotted below the lowest limit (mean – 2 SD) represented participants whose RMR was underpredicted.
Figure 1.
Bland-Altman plot displaying the agreement and bias between the RMR predicted with the Harris-Benedict equation and the measured RMR. RMR indicates resting metabolic rate.
Figure 6.
Bland-Altman plot displaying the agreement and bias between the RMR predicted with the Mifflin-St. Jeor equation and the measured RMR. RMR indicates resting metabolic rate.
Figure 5.
Bland-Altman plot displaying the agreement and bias between the RMR predicted with the Owen et al equation and the measured RMR. RMR indicates resting metabolic rate.
For each equation, prediction accuracy was assessed according to a commonly accepted error limit used in prior studies.1,45,46 Table 4 shows the prediction accuracy of each equation in comparison with the measured RMR. Owen et al predicted the RMR within ± 10% of the measured RMR for the greatest proportion of participants (84.2%), whereas Harris-Benedict provided the least accurate RMR predictions (13.2%). For all equations, overpredictions were more common than underpredictions.
Table 4.
Assessment of Accuracy for Each Prediction Equation in Comparison With RMR Obtained by Indirect Calorimetry Using Commonly Accepted Error Limit of ± 10% of Measured RMR (N = 38)
| Predication Accuracy |
|||
|---|---|---|---|
| Prediction Equation | Within Range of Agreement, n (%) | Below Range of Agreement, n (%) | Above Range of Agreement, n (%) |
| Harris-Benedict | 5 (13.2) | 0 (0) | 33 (86.8%) |
| Robertson and Reid | 22 (57.9) | 0 (0.0) | 16 (42.1) |
| Cunningham | 18 (47.4) | 0 (0) | 20 (52.6) |
| FAO/WHO/UNU | 7 (18.4) | 0 (0) | 31 (82.6) |
| Owen et al | 32 (84.2) | 1 (2.6) | 5 (13.2) |
| Mifflin-St. Jeor | 21 (55.3) | 0 (0) | 17 (44.7) |
Abbreviations: FAO/WHO/UNU, Food and Agricultural Organization/World Health Organization/United Nations University; RMR, resting metabolic rate.
DISCUSSION
We found that, for the present sample of Hispanic women aged 20 to 40 years, the Owen et al equation predicted the RMR with the least bias and greatest accuracy. The remaining 5 prediction equations significantly overestimated the RMR in comparison with the measured RMR for this group, with mean differences ranging from 136 to 216 kcal; the Harris Benedict ( + 216 kcal) and FAO/WHO/UNU ( + 208 kcal) equations provided the most biased RMR prediction.
Successful weight loss interventions and treatment plans require accurate prediction of energy requirements. Given the alarming prevalence of overweight and obesity among Hispanic women in the United States,38 such results are of concern due to the likelihood that RMR predictions calculated in clinical settings exceed actual requirements. The demographics of the participants in our study were different from the demographics of many participants who were included in the development of each prediction equation. Since none of the studied prediction equations were derived using a large group of Hispanic women, these equations may have limited applicability to this racial/ethnic group. The female participants included in the development of the Harris-Benedict equation were predominantly of normal weight, and information describing their racial/ethnic background was not included.12 In addition, because of the dramatic decline in activity levels with modern-day transportation and conveniences, the body composition of the original Harris-Benedict sample may differ from that of normal weight individuals included in the present study. Since fat-free mass3,9 and LBM31 greatly influence the RMR, these body composition differences may have also contributed to the decreased accuracy of the Harris-Benedict equation.
Although the Cunningham equation is based on data from the original Harris-Benedict sample,14 the equation may have predicted the RMR more closely to the measured RMR for our sample than did the Harris-Benedict equation, due to its reliance on LBM rather than age and other anthropometric values. Sixteen athletes included in the original Harris-Benedict sample were excluded for the derivation of the Cunningham equation.14 Therefore, the average LBM of participants in the Cunningham sample may be more comparable with that of the present sample. The FAO/WHO/UNU equations were developed from a pooled database of previously conducted studies where many ethnic/racial groups were not strongly represented.15,17 According to an annotated bibliography compiled by Schofield,17 only 3 small studies included Hispanic participants. Unfortunately, Hispanic women were included only in one of these studies,17 suggesting that the demographics of this group did not strongly influence the development of the overall FAO/WHO/UNU equations. Although it is unclear whether the small study sample that was used in the derivation of the Owen et al equation18 included Hispanic women, the Owen et al equation most closely predicted the RMR for the present study participants.
Approximately 60% of participants in the present study were overweight or obese. We expected that equations previously identified as accurate RMR predictors among over-weight and obese groups would provide the closest RMR prediction. Heshka et al23 identified the Robertson and Reid equation as one of the best prediction equations for obese men and women (mean age = 38.6 ± 10.6 and 38.5 ± 11.4 years, respectively). Siervo et al47 reported that the Owen et al equation was the best RMR predictor for normal weight women (range, 18-35 years; mean age = 23.8 ± 3.8 years) and the Robertson and Reid equation was the best RMR predictor for obese women (range, 18-35 years; mean age = 23.8 ± 5.5 years). Alternatively, Frankenfield et al,21 concluded that the Mifflin-St. Jeor equation was the most accurate RMR prediction equation for nonobese (range, 20-78 years; mean age = 41 ± 3 years) and obese men (range, 18-62 years; mean age = 40 ± 2 years) and nonobese (range, 22-74 years; mean age = 38 ± 2 years) and obese women (range, 25-69 years; mean age = 40 ± 2 years), in comparison with the Harris-Benedict and Owen et al equations. A more recent validation study48 also did not support the use of the Owen et al equation in overweight and obese women (range, 20-71 years; mean age = 50.7 ± 11.7 years); however, results indicated that the Harris-Benedict and Mifflin-St. Jeor equations may be appropriate for women with class I obesity (BMI = 30.0-34.9 kg/m2). In addition, for class I and II obese (BMI = 35.0-39.9 kg/m2) women who were older than 60 years, the FAO/WHO/UNU equation provided acceptable RMR predictions.48 Researchers have made varying recommendations for the best prediction equations to use among men and women of different weight categories. Such suggestions may have differed because of the inconsistencies between the participant age ranges in the studies,23,47,48 the inclusion of both genders in analysis,21 and incompatible definitions of prediction accuracy between studies.21,23,47,48
Prior studies have also provided evidence, suggesting the limited generalizability of many commonly used prediction equations for racial/ethnic minorities. Studies26-29 report a lower RMR among African American participants than among their non-Hispanic white counterparts. While the cause of this trend is unclear, validation studies32,33 indicate that commonly used equations, such as those of Harris-Benedict,32,33 FAO/WHO/UNU,32 and Mifflin-St. Jeor,32,33 may not be appropriate for RMR prediction in African Americans. However, Vander Weg et al33 reported that the Owen et al equation predicted the RMR with appropriate accuracy for African American women; the same result was not observed for European participants. Such reports further support the possibility of an ethnic/racial component that influences the RMR. Two studies conducted with Asian participants34,35 indicated that the Harris-Benedict34 and FAO/WHO/UNU34,35 equations overestimated the RMR in Asian women. Case et al34 suggested that the Liu et al equation,49 developed from data of Chinese participants, is most appropriate for the RMR prediction of Asian groups.
Few studies have directly evaluated the generalizability of commonly used prediction equations for Hispanic adults. Wahrlich et al36 conducted a similar assessment on a small cohort of Brazilian men and women residing in the Sonoran desert of the southwestern United States. For women in this study,36 the Harris-Benedict and Schofield equations (similar to the FAO/WHO/UNU equation) overestimated RMR by 15% and 13.8%, respectively, in comparison with indirect calorimetry. Although, on average, the women36 were of normal weight and had a body fat percentage of 33.3%, our results provided similar overestimations of the RMR (Table 3; percent difference of the Harris-Benedict and FAO/WHO/UNU equations was 16.3% and 15.7%, respectively). de Luis et al37 reported that many commonly used prediction equations either overpredicted or underpredicted the RMR in obese Spanish men and women. In contrast with our results, the Harris-Benedict and Owen et al equations significantly underpredicted RMR values whereas the FAO/WHO/UNU equation provided the closest RMR prediction.37 Although de Luis et al37 included a relatively large cohort of Spanish women, the results have limited applicability to the participants of this study. On average, the Spanish women37 were older and had a larger BMI than the women in the present study. Neither study conducted with Hispanic participants36,37 identified the best equation to use with this racial/ethnic group.
This study is the first to provide a comprehensive evaluation of 6 commonly used RMR prediction equations with a population of exclusively Hispanic women. Participants included in the study represented a broad spectrum of body weights, increasing the applicability of results to other weight categories. The strong methodology of this study included body composition measurements by DXA and RMR measurements by indirect calorimetry. This investigation is limited by the relatively small cohort and narrow age range, which may have interfered with the detection of possible trends between participant characteristics and RMR prediction accuracy. Since this study strictly examined data from Hispanic women, results are not generalizable to men or other racial/ethnic groups. In addition, the education level of the study participants suggested that this was a highly acculturated sample50; therefore, results may not be applicable to all Hispanic women in the United States.
CONCLUSION
Results of previous studies including racial/ethnic groups indicate that commonly used prediction equations may be limited in their generalizability32-37 and indirect calorimetry remains the gold standard method to determine the RMR in clinical practice.11 Unfortunately, elevated costs often associated with indirect calorimetry11 may be prohibitive and clinicians may need to rely on prediction equations to estimate the RMR. The present study evaluated the accuracy of 6 RMR prediction equations in comparison with the measured RMR for a small cohort of Hispanic women. The Owen et al equation provided the least biased and most accurate RMR prediction, whereas the remaining equations overpredicted the RMR. Furthermore, the equation of Owen et al was the only equation that predicted RMR values that were not significantly different from the measured RMR. Because of the high prevalence of overweight and obesity among the greater Hispanic population in the United States,38 and the importance of accurate RMR predictions in health care settings, such results have clinical significance. Inaccurate RMR predictions may result in ineffective weight assessments and weight loss regimens for Hispanic women. Future studies should include larger samples of Hispanic women, stratified for normal weight, overweight, and obese weight classifications. Additional research should be directed toward further evaluating the appropriateness of commonly used RMR prediction equations for other racial/ethnic groups in order for the best equation to be identified or developed.
APPLICATIONS
Although many RMR prediction equations are available, clinicians and registered dietitians must be mindful of the distinct limitations that exist for each equation when treating individuals of certain racial/ethnic groups. Specifically for Hispanic individuals, limitations in RMR prediction accuracy may surface due to underrepresentation of this racial/ethnic group during the development of the prediction equation. Validation studies are being conducted to identify and/or develop the best prediction equation for racial/ethnic groups. However, until such a finding is determined, indirect calorimetry remains the most accurate practice for RMR assessments.
Figure 2.
Bland-Altman plot displaying the agreement and bias between the RMR predicted with the Robertson and Reid equation and the measured RMR. RMR indicates resting metabolic rate.
Figure 3.
Bland-Altman plot displaying the agreement and bias between the RMR predicted with the Cunningham equation and the measured RMR. RMR indicates resting metabolic rate.
Figure 4.
Bland-Altman plot displaying the agreement and bias between the RMR predicted with the FAO/WHO/UNU equation and the measured RMR. RMR indicates resting metabolic rate; FAO/WHO/UNU, Food and Agricultural Organization/World Health Organization/United Nations University.
Acknowledgments
Dr Milliron is supported by the National Cancer Institute of the National Institutes of Health under award number R25CA122061.
Footnotes
For the remaining authors, no conflicts of interest and source of funding were declared.
REFERENCES
- 1.Frankenfield D, Roth-Yousey L, Compher C. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: a systematic review. J Am Diet Assoc. 2005;105(5):775–789. doi: 10.1016/j.jada.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 2.Hill JO, Catenacci VA, Wyatt HR. Obesity: etiology. In: Shils ME, Shike M, Ross AC, Caballero B, Cousins RJ, editors. Modern Nutrition in Health and Disease. 10th ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2006. pp. 1013–1028. [Google Scholar]
- 3.Bogardus C, Lillioja S, Ravussin E, et al. Familial dependence of the resting metabolic rate. N Engl J Med. 1986;315(2):96–100. doi: 10.1056/NEJM198607103150205. [DOI] [PubMed] [Google Scholar]
- 4.Freni SC, Lewis SM, Mayhugh MA, et al. Improved equations for estimating the resting metabolic rate. Hum Ecol Risk Assess. 2000;6(6):1039–1054. [Google Scholar]
- 5.Harris JA, Benedict FG. A biometric study of human basal metabolism. Proc Natl Acad Sci USA. 1918;4(12):370–373. doi: 10.1073/pnas.4.12.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bisdee JT, James WP, Shaw MA. Changes in energy expenditure during the menstrual cycle. Br J Nutr. 1989;61:187–199. doi: 10.1079/bjn19890108. [DOI] [PubMed] [Google Scholar]
- 7.Koot P, Deurenberg P. Comparison of changes in energy expenditure and body temperatures after caffeine consumption. Ann Nutr Metab. 1995;39:135–142. doi: 10.1159/000177854. [DOI] [PubMed] [Google Scholar]
- 8.da Rocha EEM, Alves VGF, Silva MHN, Chiesa CA, da Fonseca RBV. Can measured resting energy expenditure be estimated by formulae in daily clinical nutrition practice? Curr Opin Clin Nutr Metab Care. 2005;8:319–328. doi: 10.1097/01.mco.0000165012.77567.1e. [DOI] [PubMed] [Google Scholar]
- 9.Ravussin E, Swinburn BA. Pathophysiology of obesity. Lancet. 1992;340(8816):404–408. doi: 10.1016/0140-6736(92)91480-v. [DOI] [PubMed] [Google Scholar]
- 10.Turley KR, McBride PJ, Wilmore JH. Resting metabolic rate measured after subjects spent the night at home vs at a clinic. Am J Clin Nutr. 1993;58:141–144. doi: 10.1093/ajcn/58.2.141. [DOI] [PubMed] [Google Scholar]
- 11.Frankenfield D, Hise M, Malone A, Russell M, Gradwell E, Compher C. Prediction of resting metabolic rate in critically ill adult patients: results of a systematic review of the evidence. J Am Diet Assoc. 2007;107(9):1552–1561. doi: 10.1016/j.jada.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 12.Harris JA, Benedict FG. A Biometric Study of Basal Metabolism in Man. Carnegie Institute of Washington; Washington, DC: 1919. Publication No. 279. [Google Scholar]
- 13.Robertson JD, Reid DD. Standards for the basal metabolism of normal people in Britain. Lancet. 1952;1:940–943. doi: 10.1016/s0140-6736(52)90543-6. [DOI] [PubMed] [Google Scholar]
- 14.Cunningham JJ. A reanalysis of the factors influencing basal metabolic rate in normal adults. Am J Clin Nutr. 1980;33:2372–2374. doi: 10.1093/ajcn/33.11.2372. [DOI] [PubMed] [Google Scholar]
- 15.Food and Agricultural Organization/World Health Organization/United Nations University . Energy and Protein Requirements. World Health Organization; Geneva, Switzerland: 1985. Report of a Joint FAO/WHO/UNU Expert Consultation. World Health Organization Technical Report Series 724.
- 16.Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr. 1985;39C(suppl 1):5–41. [PubMed] [Google Scholar]
- 17.Schofield C. An annotated bibliography of source material for basal metabolic rate data. Hum Nutr Clin Nutr. 1985;39C(suppl 1):42–91. [PubMed] [Google Scholar]
- 18.Owen OE, Kavle E, Owen RS, et al. A reappraisal of caloric requirements in healthy women. Am J Clin Nutr. 1986;44:1–19. doi: 10.1093/ajcn/44.1.1. [DOI] [PubMed] [Google Scholar]
- 19.Mifflin MD, St. Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51:241–247. doi: 10.1093/ajcn/51.2.241. [DOI] [PubMed] [Google Scholar]
- 20.Dubois D, DuBois EF. A formula to estimate the approximate surface area if height and weight be known. Arch Int Med. 1916;17:863–871. [Google Scholar]
- 21.Frankenfield DC, Rowe WA, Smith JS, Cooney RN. Validation of several established equations for resting metabolic rate in obese and nonobese people. J Am Diet Assoc. 2003;103:1152–1159. doi: 10.1016/s0002-8223(03)00982-9. [DOI] [PubMed] [Google Scholar]
- 22.Daly JM, Heymsfield SB, Head CA, et al. Human energy requirements: overestimation by widely used prediction equation. Am J Clin Nutr. 1985;42:1170–1174. doi: 10.1093/ajcn/42.6.1170. [DOI] [PubMed] [Google Scholar]
- 23.Heshka S, Feld K, Yang MU, Allison DB, Heymsfield SB. Resting energy expenditure in the obese: a cross-validation and comparison of prediction equations. J Am Diet Assoc. 1993;93:1031–1036. doi: 10.1016/0002-8223(93)92043-w. [DOI] [PubMed] [Google Scholar]
- 24.Owen OE, Holup JL, D'Akessui DA, et al. A reappraisal of the caloric requirements of men. Am J Clin Nutr. 1987;46:875–885. doi: 10.1093/ajcn/46.6.875. [DOI] [PubMed] [Google Scholar]
- 25.Henry CJK, Rees DG. New predictive equations for the estimation of basal metabolic rate in tropical peoples. Eur J Clin Nutr. 1991;45(4):177–185. [PubMed] [Google Scholar]
- 26.Foster GD, Wadden TA, Vogt RA. Resting energy expenditure in obese African American and Caucasian women. Obes Res. 1997;5(1):1–8. doi: 10.1002/j.1550-8528.1997.tb00276.x. [DOI] [PubMed] [Google Scholar]
- 27.Jakicic JM, Wing RR. Differences in resting energy expenditure in African-American vs Caucasian overweight females. Int J Obes Relat Metab Disord. 1998;22(3):236–242. doi: 10.1038/sj.ijo.0800575. [DOI] [PubMed] [Google Scholar]
- 28.Gannon B, DiPietro L, Poehlman ET. Do African Americans have lower energy expenditure than Caucasians? Int J Obes Relat Metab Disord. 2000;24(1):4–13. doi: 10.1038/sj.ijo.0801115. [DOI] [PubMed] [Google Scholar]
- 29.Sharp TA, Bell ML, Grunwald GK, et al. Differences in resting metabolic rate between white and African-American young adults. Obes Res. 2002;10(8):726–732. doi: 10.1038/oby.2002.99. [DOI] [PubMed] [Google Scholar]
- 30.Benedict FG. The racial element in human metabolism. Am J Phys Anthropol. 1932;16(4):463–473. [Google Scholar]
- 31.James WP. Dietary aspects of obesity. Postgrad Med J. 1984;60(suppl 3):50–55. [PubMed] [Google Scholar]
- 32.Valliant MW, Tidwell DK, Hallam JS, Wadsworth DD, Owens S, Chitwood LF. A resting metabolic rate equation including bioelectrical impedance-derived lean body mass provides a better prediction in premenopausal African American women across a spectrum on body mass indices. Top Clin Nutr. 2009;24(2):145–151. [Google Scholar]
- 33.Vander Weg MW, Watson JM, Klesges RC, Eck Clemens LH, Slawson DL, McClanahan BS. Development and cross-validation of a prediction equation for estimating resting energy expenditure in healthy African-American and European-American women. Eur J Clin Nutr. 2004;58:474–480. doi: 10.1038/sj.ejcn.1601833. [DOI] [PubMed] [Google Scholar]
- 34.Case KO, Brahler CJ, Heiss C. Resting energy expenditures in Asian women measured by indirect calorimetry are lower than expenditures calculated from prediction equations. J Am Diet Assoc. 1997;97:1288–1292. doi: 10.1016/S0002-8223(97)00308-8. [DOI] [PubMed] [Google Scholar]
- 35.Nhung BT, Khan NC, Hop LT, et al. FAO/WHO/UNU equations overestimate resting metabolic rate in Vietnamese adults. Eur J Clin Nutr. 2005;59(10):1099–1104. doi: 10.1038/sj.ejcn.1602199. [DOI] [PubMed] [Google Scholar]
- 36.Wahrlich V, Anjos LA, Going SB, Lohman TG. Basal metabolic rate of Brazilians living in the southwestern United States. Eur J Clin Nutr. 2007;61(2):289–293. doi: 10.1038/sj.ejcn.1602498. [DOI] [PubMed] [Google Scholar]
- 37.de Luis DA, Aller R, Izaola O, Romero E. Prediction equation of resting energy expenditure in an adult Spanish population of obese adult population. Ann Nutr Metab. 2006;50(3):193–196. doi: 10.1159/000090740. [DOI] [PubMed] [Google Scholar]
- 38.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults 1999-2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 39.Hasson RE, Howe CA, Jones BL, Freedson PS. Accuracy of four resting metabolic rate prediction equations: effects of sex, body mass index, age, and race/ethnicity. J Sci Med Sport. 2011;14(4):344–351. doi: 10.1016/j.jsams.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 40.Deemer SE, King GA, Dorgo S, Vella CA, Tomaka JW, Thompson DL. Relationship of leptin, resting metabolic rate, and body composition in premenopausal Hispanic and non-Hispanic white women. Endocr Res. 2010;35(3):95–105. doi: 10.3109/07435800.2010.496088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Compher C, Frankenfield D, Keim N, Roth-Yousey L. Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Am Diet Assoc. 2006;106(6):881–903. doi: 10.1016/j.jada.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 42.Chad KE, Wenger HA. The effect of exercise duration on the exercise and post-exercise oxygen consumption. Can J Sport Sci. 1988;13:204–207. [PubMed] [Google Scholar]
- 43.Collins LC, Cornelius MF, Vogel RL, Walker JF, Stamford BA. Effect of caffeine and/or cigarette smoking on resting energy expenditure. Int J Obes Relat Metab Disord. 1994;18:551–556. [PubMed] [Google Scholar]
- 44.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- 45.Frankenfield DC, Coleman A, Alam S, Cooney RN. Analysis of estimation methods for resting metabolic rate in critically ill adults. JPEN J Parenter Enteral Nutr. 2009;33(1):27–36. doi: 10.1177/0148607108322399. [DOI] [PubMed] [Google Scholar]
- 46.Li AC, Tereszkowski CM, Edwards AM, Randall Simpson JA, Buchholz AC. Published predictive equations overestimate measured resting metabolic rate in young, healthy females. J Am Coll Nutr. 2010;29(3):222–227. doi: 10.1080/07315724.2010.10719837. [DOI] [PubMed] [Google Scholar]
- 47.Siervo M, Boschi V, Falconi C. Which REE prediction equation should we use in normal-weight, overweight and obese women? Clin Nutr. 2003;22(2):193–204. doi: 10.1054/clnu.2002.0625. [DOI] [PubMed] [Google Scholar]
- 48.Ziegler J, Rothpletz-Puglia P, Touger-Decker R, Byham-Gray L, O'Sullivan Maillet J, Denmark R. Resting energy expenditure in overweight and obese adults: agreement between indirect calorimetry and predictive formulas. Top Clin Nutr. 2010;25(2):180–187. [Google Scholar]
- 49.Liu HY, Lu YF, Chen WJ. Predictive equations for basal metabolic rate in Chinese adults: a cross-validation study. J Am Diet Assoc. 1995;95(12):1403–1408. doi: 10.1016/S0002-8223(95)00369-X. [DOI] [PubMed] [Google Scholar]
- 50.Padilla AM. Acculturation: Theory, Models and Some New Findings. Westview Press; Boulder, CO: 1980. [Google Scholar]