Abstract
The current standard for Bacillus anthracis vaccination is the Anthrax Vaccine Adsorbed (AVA, BioThrax). While effective, the licensed vaccine schedule requires five intramuscular injections in the priming series and yearly boosters to sustain protection. One potential approach to maintain or improve the protection afforded by an anthrax vaccine, but requiring fewer doses, is through the use of purified proteins to enhance an antibody response, which could be used on their own or in combination with the current vaccine. This study describes a novel, high-throughput system to amplify and clone every gene in the B. anthracis pXO1 and pXO2 virulence plasmids. We attempted to express each cloned gene in Escherichia coli, and obtained full-length expression of 57% of the proteins. Expressed proteins were then used to identify immunogens using serum from three different mammalian infection models: Dutch-belted rabbits, BALB/c mice, and rhesus macaque monkeys. Ten proteins were detected by antibodies in all of these models, eight of which have not been identified as immunoreactive in other studies to date. Serum was also collected from humans who had received the AVA vaccine, and similar screens showed that antigens that were detected in the infection models were not present in the serum of vaccinated humans, suggesting that antibodies elicited by the current AVA vaccine do not react with the immunoreactive proteins identified in this study. These results will contribute to the future selection of targets in antigenicity and protection studies as one or more of these proteins may prove to be worthy of inclusion in future vaccine preparations.
Keywords: Bacillus anthracis, recombinant vaccine, ligation-independent cloning, high-throughput expression, seroreactive
1. Introduction
Bacillus anthracis is a Gram-positive soil-borne bacteria and the causative agent of anthrax. Natural human anthrax infections are typically acquired by handling animal products contaminated with B. anthracis spores and normally present as a reasonably treatable cutaneous infection. Other forms of anthrax include gastrointestinal anthrax resulting from the ingestion of a contaminated animal product, and inhalational anthrax, which is the most deadly form of the disease and progresses very quickly [1,2]. The lethal potential of B. anthracis spores combined with their hardiness and ease of preparation has made them a central component to biological weapons research over the past 60 years in multiple countries, including Japan, the former Soviet Union, and Great Britain [3-5]. The anthrax letter attacks in the United States in 2001 resulted in 22 cases of inhalational anthrax, five of which were fatal even after intense antimicrobial therapy, demonstrating the potential use of this agent as an instrument in a future biological attack [6].
Two plasmids, pXO1 and pXO2, are maintained by virulent B. anthracis and impart much of this pathogen's virulence. The 184.5 kb pXO1 plasmid encodes the tripartite toxin complex [lethal factor (LF), protective antigen (PA) and edema factor (EF)], all of which are required for full virulence [7]. The 95.3 kb pXO2 plasmid is required for the synthesis of the capsule proteins responsible for inhibiting phagocytosis of B. anthracis spores [7,8].
In the United States, the only FDA-licensed vaccine against anthrax is the Anthrax Vaccine Adsorbed (AVA [BioThrax]; Emergent BioSolutions, Lansing, MI). This vaccine is composed of aluminum hydroxide-adsorbed culture supernatant, with the primary protective component being B. anthracis protein PA [9]. This vaccine is known to protect against inhalational anthrax in multiple animal models and in humans [10-12]. However, the regimen for this vaccine is somewhat cumbersome and expensive. It consists of a series of doses administered at 0 and 4 weeks, and at 6, 12, and 18 months, with yearly boosters [13]. Additionally, evaluation of the safety of the AVA vaccine is still ongoing. Multiple studies have shown that the protein composition of the vaccine varies from lot to lot, and other B. anthracis components, including the lethal factor toxin, are known to be present in ambiguous amounts [14,15]. It has also been demonstrated that the vaccine can cause some systemic and local reactions, including headache, fever, and injection site sensitivity [16]. As a result of these issues, there is a current effort to design a vaccine that displays increased safety and efficacy while sustaining or surpassing the protectiveness of the AVA vaccine.
Since PA is known to be the primary protective component of the AVA vaccine, efforts are underway to explore the use of recombinant PA as the active component of a new vaccine. Initial studies in rabbits [17] and nonhuman primates [18] showed a high level of PA-mediated protection against aerosol infection, and Phase I trials indicated that while recombinant PA is safe, important features such as optimal formulation and dosing schedule require further development [19,20]. Other studies have sought to combine the purified, recombinant PA with other B. anthracis proteins that elicit protective responses and could thus enhance the protection afforded by PA alone. Such “cocktail” style vaccines have seen a great deal of success against Bordetella pertussis infections. Pertussis vaccines licensed in the United States combine inactivated pertussis toxin with other bacterial components, including filamentous hemagglutinin, pertactin, and fimbrae proteins. One study demonstrated that acellular pertussis vaccines increased in efficacy as the number of recombinant protein components increased from one to three or more [21].
The success of the B. pertussis cocktail vaccine has contributed to the effort to identify antigenic B. anthracis proteins that may be used as components of a cocktail vaccine against anthrax infection [22-30]. One series of experiments combined PA with poly-γ-d-glutamic acid from the capsule to enhance protection against a spore challenge in mice and rabbits [31,32]. Other experiments have explored the use of spore-associated proteins in combination with PA. One such protein, BclA, was shown to afford a higher level of protection than PA alone in mice [27]. Additionally, the two spore proteins p5303 and BxpB were also shown to improve protection in mice after spore challenge when given in combination with PA [33].
Publication of the B. anthracis genome has paved the way for more focused efforts to identify and characterize potential candidates for vaccine studies. Computational analysis of the B. anthracis proteome has led to the identification of potentially immunogenic proteins that were assessed in a DNA vaccination study [34]. In addition, in vivo Induced Antigen Technology (IVIAT) strategies have identified seroreactive proteins that are expressed only under conditions similar to those seen during an infection [22].
Previous work has identified many seroreactive proteins within the B. anthracis proteome, and some of the genes encoding these proteins are found on the virulence plasmids (Table 1) [35]. Thus, we aimed to clone every virulence plasmid gene into an Escherichia coli expression vector and use a battery of sera from animal infection models to probe proteins expressed from this clone set for infection-specific seroreactive proteins. The novel vector created for use in this study combines the efficiency of Ligation-Independent Cloning (Stratagene) with the ColE1 promoter to attempt to clone and express the 226 B. anthracis virulence plasmid genes in E. coli. Expressed proteins were used in immunoblots using serum from mouse, rabbit, and macaque infection models to test for seroreactivity. These proteins were also used in immunoblots using serum from five human AVA recipients in an attempt to identify other immunoreactive components that may contribute to the protection provided by the AVA vaccine. The identification of unique seroreactive proteins in this study has added to the list of candidate proteins identified in other studies to be investigated further for their ability to stimulate a protective immune response against B. anthracis challenge. Inclusion of promising candidates in future vaccine preparations may improve vaccine protectiveness and could help minimize the cost, risk, and time involved to sustain immunity.
Table 1.
Virulence-plasmid associated seroreactive proteins that have been identified since 2002. Mammalian systems include mica [M], rabbits [R]. macaques [Q], guinea pigs, [G], and humans [H]. “*” denotes a protein identified in multiple studies
| Study | Locus Tag | Protein | Model |
|---|---|---|---|
| This study | pXOl-21 | Reductase | MRQ |
| pXOl-57 | Hypothetical protein | MRQ | |
| pXOl-52 | Hypothetical protein | MRQ | |
| pXOl-100 | Hypothetical protein | MRQ | |
| pXOl-110* | Protective antigen (PA) | MRQ | |
| pXOl-115 | Hypothetical protein | MRQ | |
| pX02-17 | Hypothetical protein | MRQ | |
| pX02-34 | Hypothetical protein | MRQ | |
| pX02-42* | S-layer amidase | MRQ | |
| pXO2-66 | ABC transporter | MRQ | |
| Ariel 2002 | pX01-54* | S-Layer protein | G |
| pXOl-90* | S-Layer, DNA interaction | GR | |
| pXOl-110* | Protective antigen (PA) | R | |
| pXOl-130 | SBP-ABC [Zn] (YodA) | R | |
| Gat 2006 | pXO-54* | S-Domain containing protein | G |
| pXO1-90* | S-Layer, DNA interaction | R | |
| pXOl-107* | Lethal factor (LF) | R | |
| pXOl-110* | Protective antigen (PA) | R | |
| pXOl-122* | Edema factor (EF) | R | |
| pXOl-130* | SBP-ABC [Zn] (YodA) | R | |
| pXO2-08* | NLP/P60 lipoprotein family | G | |
| pX02-42* | Amidase | R | |
| Chitlaru 2007 | pXOl-54* | S-Domain containing protein | R |
| pXOl-90* | S-Layer, DNA interaction | R | |
| pXOl-107* | Lethal factor (LF) | R | |
| pXOl-110* | Protective antigen (PA) | R | |
| pXOl-122* | Edema factor (EF) | R | |
| pXOl-130* | SBP-ABC [Zn] (YodA) | R | |
| Walz 2007 | pXOl-110* | Protective antigen (PA) | H |
| Rollins 2003 | pXOl-110* | Protective antigen (PA) | Q |
| pXO2-08* | NLP/P60 lipoprotein family | Q | |
| pX02-42* | Amidase | Q | |
| BXB0048* | Hypothetical protein | Q |
2. Materials and Methods
2.1 Ligation-independent cloning of B. anthracis genes
The genes from which the pXO1 clone set was derived were originally sequenced from a pXO2-deficient Sterne strain ([36], AF065404), and the genes from which the pXO2 clone set were derived was from a Pasteur strain sequenced in 1999 and directly submitted to NCBI by Okinaka et. al. (AF188935). The cea promoter was amplified from the plasmid pGE124 [37] by PCR using primers HG3 and HG4 (Table 2). The cea promoter fragment and the pTRC99A plasmid were digested with NdeI and EcoRI (New England Biolabs) and ligated. This new construct, pHG2, was electroporated into JM109 cells.
Table 2. Primers and Plasmids Table.
| HG1 | 5′-GGGGTTTTAATATTGAGAACGGTAATGTTTGTGCTGG-3′ |
| HG2 | 5′-GGGGTTTTGGATCCTATAAAATCCTCTTTGACTTTT-3′ |
| HG3 | 5′-GGGGTTTTCATATGGAGAACGGTAATGTTTGTGCTGG-3′ |
| HG4 | 5′-GGGGTTTTGAATTCTATAAAATCCTCTTTGACTTTT-3′ |
| HG50 | 5′-GGGGTTTTGAATTCTCTAGAGGATCCGTCGACCTGCAGATGAAATCTAACAATGCGCTCATCG-3′ |
| HG52 | 5′-GGGGTTTTAAGCTTTTATTAGTGATGGTGATGGTGATGGTGATGGTGATGCCCGGGGGTCGAGGTGGCCCGGCTCC ATGC-3′ |
| HG53 | 5′-GGGTTTGCATATGGAGAACGGTAATGTTTGTGC-3′ |
| HG54 | 5′-GGGTTTGGAAGCGGAAGAGCGGGTTATTGTCTCATGAGCGG-3′ |
| HG55 | 5′-GGGTTTTGAATTCATGGCTAGCATGACTGGTGGACAGCAAATGGGAGGAGCGGCCGCGAAATCTAACAATGCGCT CATCGTCATCC-3′ |
| HG56 | 5′ -GGGGTTTTAAGCTTTTATTAATGGTGATGGTGATGGTGATGGTGATGGTGGGCAGCGCGGCCGCCGGTCGAGGTGG CCCGGCTCCATGCACC-3′ |
| pHG2 | cea promoter amplified from pGE124 |
| pHG4 | tet gene cloned from pKRP12 and inserted into pHG2 |
| pHG5 | cea promoter, I0×His tagged tet gene, rmBTlT2 fragment of pHG4 cloned into Ndel and Sapl sites of pUCI8 |
| pHG6 | N-terminal T7 antigen tag and 5′ and 3′ LIC sites inserted into EcoRI-HindIII fragment of pHG5 |
| pHG7 | pHG4 promoter, T7, His, and LIC cloning site in pUCI8 created by NotI digest of pHG6 and recircularizing the larger fragment (i.e. without tet) |
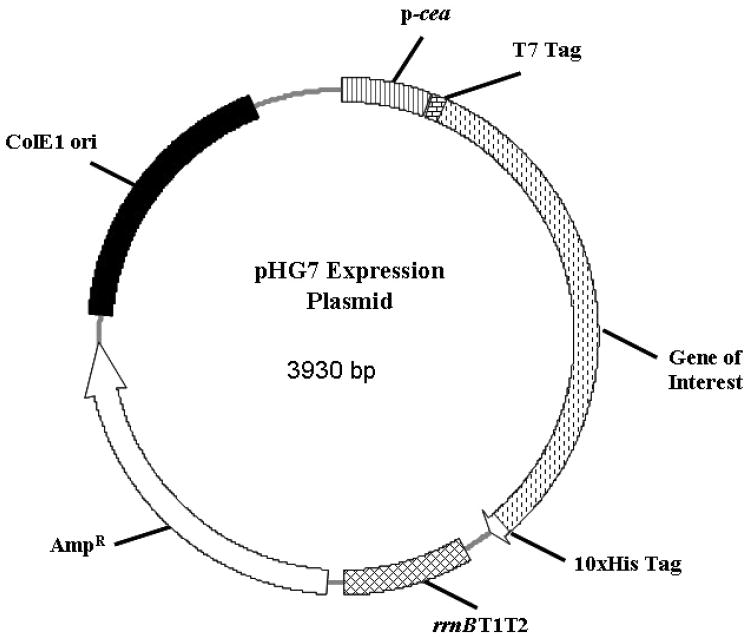
The tet gene was then amplified from pKRP12 [38] using primers HG50 and HG52 (Table 2), and the product was digested with EcoRI and HindIII and ligated into pHG2 to create pHG4. This step also added a 10x histidine tag to the C-terminus of the tet gene. The cea promoter, 10xHis-tagged tet gene, and rrnB T1T2 transcriptional terminator fragment of pHG4 were amplified using HG53 and HG54, digested with NdeI and SapI, and ligated into the same sites of the pUC18 plasmid to create pHG5. Addition of a T7 antigen tag upstream of the tet gene and ligation independent cloning (LIC) was achieved by amplifying the tet gene with HG55 and HG56 and replacing the pHG5 EcoRI-HindIII fragment with the HG55-HG66 PCR product. A NotI digest of pHG6 and recircularization of the plasmid backbone removed the tet gene from this construct, leaving the LIC cloning regions and flanking fusion tags. This final construct was named pHG7 (Figure 1).
Figure 1.
Plasmid pHG7, engineered for expression of proteins under microaerobic conditions. Expression is driven by the SOS response, which induces the cea promoter. Expression produces a protein product with an N-terminal T7 tag and a C-terminal His tag.
For ligation independent cloning of pXOl and pX02 ORFs, the pHG7 plasmid was digested with NotI (Figure 2). Incubation with T4 DNA Polymerase and dTTP removed bases from the 3′overhangs to the first thymidine encountered. Primers designed to complement the gene of interest and the T4 DNA polymerase-generated overhang were used for PCR. The PCR product containing the gene of interest was subsequently exposed to T4 DNA polymerase and dATP, which removed bases on the 3′ end of the overhang until the first adenosine. The two complimentary overhangs created by these steps were used to anneal the gene of interest into the pHG7 expression plasmid (Figure 1). Ligation of the resulting nicked insert is accomplished by the host machinery after transformation into JM109 cells. Each clone was verified by restriction digest and DNA sequencing.
Figure 2.
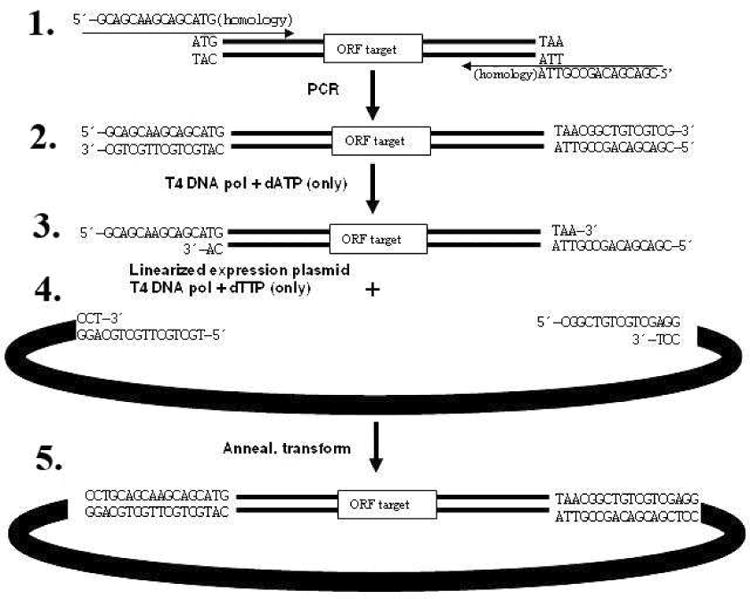
Ligation-independent cloning using pHG7: (1) An ORF target is amplified using primers with extensions homologous to the DNA ends generated by linearization of the expression vector. After amplification (2), the PCR product is treated with T4 DNA polymerase in the presence of one dNTP (dATP in this example). (3) 3′-5′ exonuclease activity results in a 5′ overhang and a terminal dATP on the opposite strand. This product can be annealed (4) to similarly treated plasmid DNA (with dTTP the only included dNTP) to generate a recombinant plasmid upon transformation (5).
2.2 Expression under low-oxygen conditions
Cultures of selected clones were grown overnight in 10 mL of Luria-Bertani broth supplemented with 0.15 mM KNO3 and 100 μg/mL ampicillin. High aeration samples were diluted 1:100 into 50 mL fresh media in a 250 mL baffled flask and allowed to grow to an OD600 of ∼0.5. Protein expression was induced with 1 μg/mL mitomycin C and grown overnight at 30°C shaking at 150 RPM. Low aeration samples were diluted 1:24 in 1 mL of fresh media contained in individual wells of a 96-well culture box (Axygen Scientfic), and grown to an OD600 of ∼0.5. Protein expression was induced with 1 μg/mL mitomycin C and grown overnight at 30°C shaking at 150 RPM on a microtiter plate shaker.
After 18 hours of induced growth, cultures were serially diluted and plated on LB plates supplemented with 100 μg/mL ampicillin. Plates were incubated overnight at 37°C, and colonies were counted to enable normalized loading and separation of cellular lysate using SDS-PAGE. Detection of expressed protein was done using the Penta-His HRP Conjugate Kit and following the manufacturer's provided protocol (Qiagen).
2.3 Expression and detection of clone set genes
E. coli containing expression plasmids for each gene of interest were grown overnight in 1 mL of LB broth in 96-well, round bottom deep-well culture boxes shaking at 900 RPM. Overnight cultures were diluted and induced as described above. The following day, cultures were centrifuged for 10 min at 1,278 × g and resuspended in 100 μL SDS gel loading buffer (50 mM Tris-Cl (pH 6.8), 100 mM DTT, 2% SDS, 0.1% bromophenol blue, 10% glycerol). The resulting lysate was separated by SDS-PAGE or 2 μL was spotted directly onto nitrocellulose transfer membrane and allowed to dry at 37°C for 30 m. Detection of expressed proteins was achieved using the Penta-His HRP Conjugate Kit and following the manufacturers provided protocol (Qiagen).
2.4 96-well Protein Purification
Proteins were expressed as described above. Three 1 mL cultures of each clone were grown and induced simultaneously. Purification was performed using TALON cobalt resin (Clontech) in a 96-well format for use with a titer-plate centrifuge (Sorvall). After overnight expression and centrifugation, cells were resuspended and lysed using 1 mL of TALON xTractor Buffer (Clontech) supplemented with 6 M urea. Lysates were left shaking at room temperature for 1 hr following addition of lysis buffer. A TALON HT 96-well plate was centrifuged at 700 × g for 30 s to remove storage ethanol. Beads were washed once in water and then twice in PBS (pH 7.4) supplemented with 6 M urea, and centrifuged after each resuspension at 700 × g for 30 s to remove supernatant. 3 mL of total lysate was used to resuspend the resin and allowed to incubate for 30 min at room temperature, either vortexing or pipetting every five minutes to ensure the resin would not settle out of solution. Flow through was collected by centrifuging at 700 × g for 30 s with a clean 96-well plate. The resin was washed five times with 200 μL PBS supplemented with 6M urea and 10 mM imidazole, and protein was eluted with two 200μL washes of PBS-urea containing 200 mM imidazole and stored at 4°C. Protein concentration was determined using a Bradford assay (BioRad), and the presence and relative purity of the target protein was determined using the previously described Penta-His HRP kit and a Coomassie stained SDS-PAGE gel, respectively.
2.5 Serum Dot Blots
We examined the seroreactivity of expressed proteins with sera from previous infection studies [39,40], thus eliminating the need for de novo infections. Mammalian serum from multiple species was obtained from several collaborators. Rabbit serum (Dr. Johnny Peterson, University of Texas-Galveston) was collected from Dutch-belted rabbits infected intranasally with 1 × 107 CFU of B. anthracis Ames spores. The rabbits were passively immunized 24 hours post-infection with a human monoclonal antibody (AVP-21D9) against PA and the serum collected 30 days post-infection and pooled [40]. Mouse serum (Dr. Henry Heine, USAMRIID) was collected from female BALB/c mice infected with 50 LD50s of B. anthracis Ames spores via aerosolization. At 60 hours post infection, after significant germination and bacteremia had occurred, the mice were treated with 100 mg/kg amoxicillin every 12 hours. Treatment lasted for 21 days, and surviving animals were bled and serum collected 60 days post-infection [39]. Convalescent serum from AVA-vaccinated rhesus macaques that had survived inhalational anthrax was provided by Dr. Conrad P. Quinn at the Centers for Disease Control in Atlanta, GA. Rhesus macaques were immunized with three intramuscular doses (weeks 0, 4, and 26) of AVA and survived aerosol challenge with 200-400 LD50 equivalents of B. anthracis Ames strain at week 52. Sera were harvested on days 14 and 30 post-challenge. Finally, human serum from AVA-vaccinated individuals was provided by Dr. Wendy Keitel (Baylor College of Medicine). These subjects were vaccinated using the original AVA schedule, which used 6 subcutaneous injections instead of 5 (0, 2, and 4 weeks, followed by injections at 6, 12, and 18 months, with yearly boosters thereafter.) Three samples were collected from five subjects and assayed individually. Samples were collected pre-injection, 1 month after the first injection, and 1 month after the second injection.
To screen for seroreactivity, 2 μL of expressed and purified proteins were spotted directly onto nitrocellulose transfer membrane and allowed to dry for 30 min at 37°C. Blots were then rinsed twice for 10 min with TBS and blocked overnight at 4°C with TBS containing 2% milk and 0.1% Tween-20, or PBS containing 2% milk for the human serum blots. Blots were rinsed twice with TBS with 0.1% Tween (TBST) and once with TBS before exposure to primary serum. The serum was diluted 1:20,000 in blocking buffer and allowed to incubate for 1 hr at room temperature. Blots were washed twice with TBST, once with TBS, and then exposed to secondary antibody. The secondary rabbit antibody was a goat anti-rabbit IgG, IgM, IgA conjugated to HRP (Open Biosystems). The secondary mouse antibody was a rabbit anti-mouse IgG, IgM antibody conjugated to HRP (Thermo Scientific). Secondary macaque antibody was a goat anti-monkey IgG, IgM, IgA antibody conjugated to HRP (Open Biosystems). Secondary human antibodies were goat anti-human IgG, IgM, IgA antibodies conjugated to HRP (Open Biosystems). Secondary antibodies were diluted 1:7,500 in blocking buffer and allowed to incubate on the membrane for 1 hr at room temperature. Membranes were washed twice with TBST and once with TBS and developed using SuperSignal West Pico Chemiluminescent Substrate (Pierce).
3. Results
3.1 Cloning of B. anthracis virulence plasmid clone set
Downstream genomics and proteomics projects often involve libraries with large numbers of clones, and high-throughput expression of these libraries can require hundreds of cultures and growth in relatively small volumes. Growing such cultures in 96-well boxes creates low-oxygen conditions that are generally regarded as sub-optimal for standard protein expression protocols. To address this, we adapted a system used by Eraso and Weinstock [37], which uses the cea-kil operon to drive protein expression under SOS-inducing, oxygen limiting conditions, and combined this promoter with a ligation-independent cloning system (Figure 1, 2). The SOS-inducible cea promoter was isolated from its original plasmid backbone, pGE124 [37]. The cloning plasmid, pHG7, was created as described in Materials and Methods and enabled the use of a consistent primer design to amplify and clone every pXO1 and pXO2 gene, each with a common complimentary region designed to anneal to the plasmid. The terminal expression vector added 10x-His and T7 epitope tags to each protein product (Figure 1).
3.2 Expression of pXO1/pXO2 clone set genes
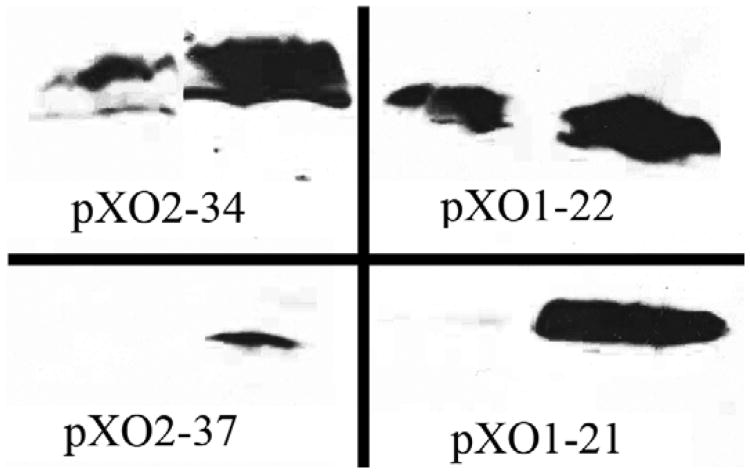
E. coli clones harboring individual B. anthracis virulence-plasmid genes under control of the cea promoter were first used to demonstrate that our high throughput system facilitated increased protein expression under the low-oxygen conditions typical of 96-well box cultures. Protein expression was induced under both high- and low-aeration conditions, and these samples were run on a Western blot and visualized using an anti-His antibody. Figure 3 illustrates four clones that showed increased expression under these low-aeration conditions. Of the subset of clones tested in this fashion (n=20), approximately 54% were characterized by improved protein expression under low-aeration conditions.
Figure 3.
Protein expression under high- and low-aeration conditions. Cultures of each clone were grown overnight and diluted into either a 250 mL flask (high aeration, left sample) or a single well in a 96-well box (low aeration, right sample). Both cultures were induced, grown overnight, and run on a Western Blot, where loading was normalized by serial dilutions and plating. All proteins were visualized at the expected size.
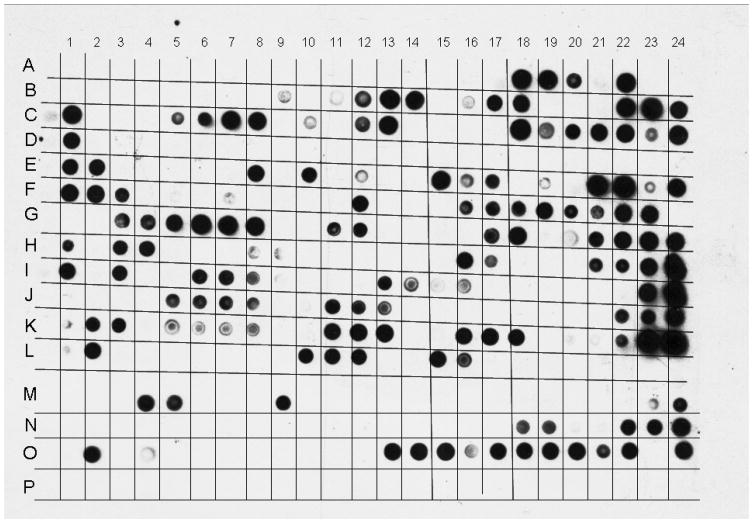
We then characterized protein expression of the full set of clones after induction with mitomycin C under low aeration conditions. Lysates were spotted directly onto nitrocellulose membranes and visualized by Western blot (Figure 4). Because a very large number of clones were being evaluated during each screen, sample loading was not normalized. Once protein expression was verified using this dot blot technique, size was verified using SDS-PAGE and Western blot. Of the 207 expression clones tested, 130 of them showed positive expression, and of those 130 proteins, 117 of them expressed at or near the predicted size (Table 3). The 13 proteins that expressed below their predicted size were nonetheless included in the serum screens described below, as these truncated products may still contain antibody-binding epitopes.
Figure 4.
Anti-His dot blot showing expression of four individual 96-well boxes of expressed clones. The first two rows of a given 96-well box are spotted here in row “A,” the next two in row “B”, and so on through row “D,” where the last two rows of a given box are included. Cells were induced with mitomycin C, lysed, and 2 μL of lysate spotted for visualization. Array runs 16 rows by 24 columns. An example of positive expression is visible at CI3, which corresponds to the gene pX02-5 (GI: 6470156). An example of low but acceptable expression is seen in C19, which corresponds to gene pX02-15 (GI: 6470166.)
Table 3.
Data from expression studies of B. anthracis expression clone set.
| pXOl | |
|
| |
| Total genes on plasmid | 145 |
| Total genes tested | 129 |
| Expr. | 74 |
| %Expr. | 57.40% |
| Expr. + Size | 63 |
| % Expr. 4 Size | 48.80% |
|
| |
| pX02 | |
|
| |
| Total genes on plasmid | 84 |
| Total genes tested | 78 |
| Expr. | 56 |
| %Expr. | 71.80% |
| Expr. + Size | 54 |
| % Expr. + Size | 69.20% |
|
| |
| Totals | |
|
| |
| Total Genes Tested | 207 |
| Expr. | 130 |
| %Expr. | 62.80% |
| Expr. + Size | 117 |
| % Expr. + Size | 56.50% |
Analysis of the genes that expressed well in our system indicated that 57 of the 130 (44%) protein products were previously annotated as hypothetical proteins, and upon our evaluation, we found that they possess no significant homology to any characterized proteins. The remaining proteins possess a wide range of functions. 24 are associated with nucleic acid interaction, including DNA binding, transcriptional regulation, and recombination. Of these 24, 11 were specifically related to transposons and their associated integrases and transposases. Another ten proteins were associated with external structures in B. anthracis, including spore, capsule, and Slayer associated proteins and regulators (Supplementary Table 1).
We also examined the genes that expressed minimally, or not at all, in our system. Among those, almost 62% are predicted hypothetical proteins. Specifically, 15 of the 18 poorly expressed genes on the pXO2 plasmid are annotated as hypothetical. Among those that had been assigned a function, five were associated with transposons and four were associated with DNA binding (Supplementary Table 1).
3.3 High-throughput protein purification and mammalian serum screening
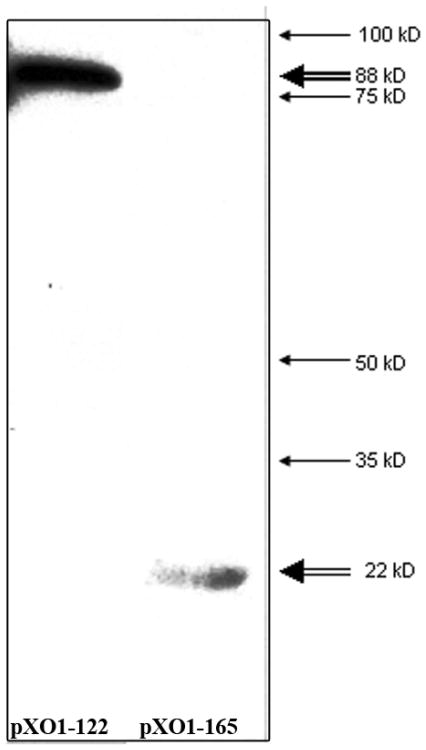
Our initial attempts to characterize seroreactivity in our library used crude bacterial lysate after mitomycin C induction. These studies were inconclusive, because a high level of background signal made the dot blots unreadable. To address this issue, we purified the expressed proteins using the TALON 96-well purification system (Clontech, Mountain View, CA), which binds histidine using a cobalt metal ion in a high-throughput format. Two examples of purified protein using this strategy, pXOl-122 and pXOl-65, are shown in Figure 5. After purification, all samples were subjected to Bradford assays, which indicated that each clone produced an average total yield between 20 and 50 μg of protein from 3 mL of culture.
Figure 5.
Western blots of two purified proteins using the 96-Well TALON method. The Western blot was performed with a Penta-HIS kit (Qiagen). The left sample is pXOl-122, which has a predicted size of approximately 88 kD, and the right sample is pXOl-65, which has a predicted size of 22 kD. These predicted sizes are indicated by the double arrow. The single arrows indicate the location of four molecular weight bands from the Precision Plus Protein Standards protein ladder (BioRad).
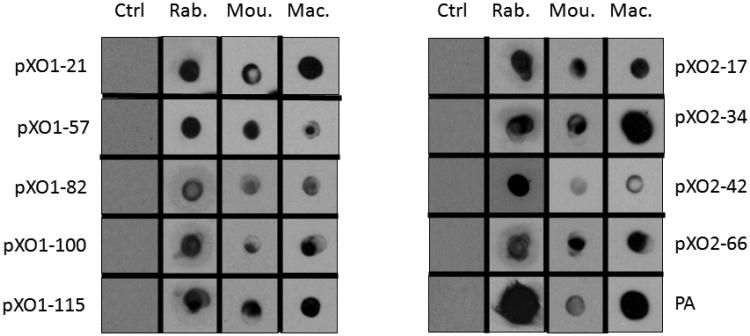
To identify which purified proteins were seroreactive, serum from three mammalian infection models (Rhesus macaque, Dutch-belted rabbits, and BALB/c mice) was used to probe the purified proteins. Upon visualization of the serum blots, signals significantly higher than background were selected as positive signals. Three screens using rabbit serum, two screens using mouse serum, and two screens using macaque serum were performed for each protein. Our screens identified a group of 17 proteins that reacted with sera from at least two of three infection models. Of these, 10 reacted with sera from all three infection models, including six hypothetical proteins, an S-layer amidase, and an ABC transporter. PA served as a positive control in these experiments. The dot blot results from these 10 proteins can be found in Figure 6, and a collective list of proteins identified in individual infection systems can be found in Table 4. Serum from uninfected, negative control rabbits showed no reactivity with any of the proteins that were screened, indicating that the proteins detected using the rabbit serum resulted from an antibody response during the initial B. anthracis infection.
Figure 6.
Serum blot results from pre-infected rabbits (left, “Ctrl”), infected rabbits (Rab.), infected mice (Mou.) and infected macaques (Mac.). In each case, primary antibody was visualized by using a species-specific, HRP-conjugated secondary antibody as described in Materials and Methods.
Table 4. List of proteins detected in infection models. [A] indicates detection in mice, [B] rabbits, and [C] in macaques.
| Seroreactive Proteins | |
|---|---|
| pXOl-21ABC | Reductase |
| pXOl-57ABC | Hypothetical protein |
| pXOl-82ABC | Hypothetical protein |
| pXOl-l00ABC | Hypothetical protein |
| pXOl-110ABC | Protective antigen |
| pxol-115ABC | Hypothetical protein |
| pXO2-17ABC | Hypothetical protein |
| pX02-34ABC | Hypothetical protein |
| pX02-42ABC | S-layer amidase |
| pXO2-66ABC | ABC Transporter |
|
| |
| pX01-22AB | Hypothetical protein |
| pXOl-55BC | Hypothetical protein |
| pXO2-33AC | Hypothetical protein |
| pX02-37 AC | Hypothetical protein |
| pX02-52AC | Hypothetical protein |
| pX02-55AC | gamma-glutamyltranspeptidase |
| pX02-59AC | Signal peptidase |
|
| |
| pXOl-135B | Hypothetical protein |
| pX02-7C | Hypothetical protein |
| pX02-8B | Lysozyme-like protein |
| pX02-26B | Hypothetical protein |
| pX02-64A | Capsule synthesis regulator |
Finally, the purified proteins were used to determine whether any are detected by the humoral response following the AVA vaccination. It is generally accepted that PA is the primary immunogenic component of this vaccine, but it is possible other targets may contribute to the immune response. To test our purified proteins against the human antibody response, serum collected from individuals vaccinated with the AVA vaccine was used in a serum dot blot. Though we were able to see a clear, increasing response to PA throughout the vaccination schedule (Figure 7), there were no other signals common between the infection models and vaccination model.
Figure 7.
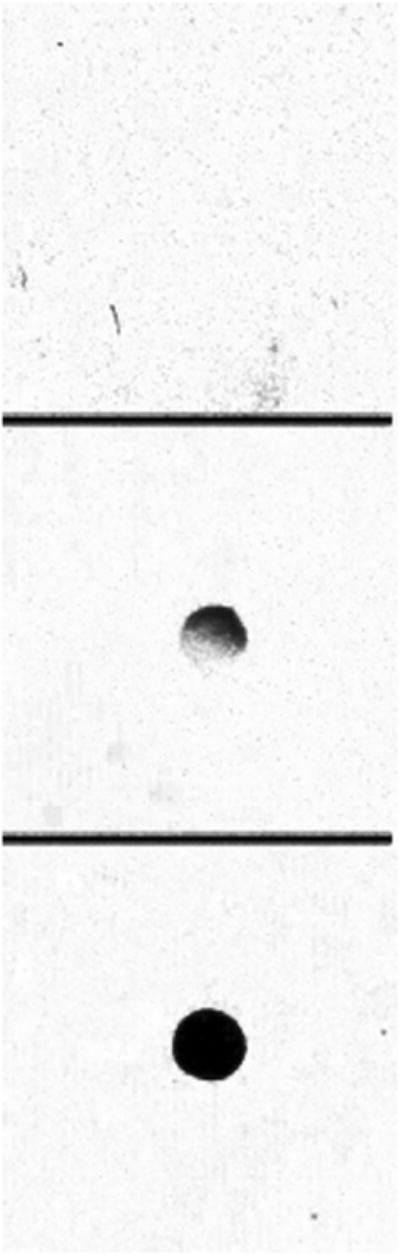
Recombinant PA visualized using serum from AVA-vaccinated human subjects. Top panel shows pre-vaccination control serum. Middle panel shows binding of serum after first AVA injection, and bottom panel shows binding of serum after final AVA injection.
4. Discussion
The current standard for anthrax vaccination, the AVA vaccine, has come under increasing scrutiny since the terrorist attacks in the United States in 2001. While effective, the licensed vaccine schedule is expensive and cumbersome. Furthermore, concerns regarding the safety and lot to lot variability of AVA have incited research into alternatives to and improvements of this standard.
Recombinant protein vaccines have the potential to be used to protect against anthrax, and considering that the AVA vaccine is composed primarily of PA, a recombinant vaccine combining PA with another protein (or collection of proteins) may increase protection and address concerns about safety and reproducibility in a more tightly controlled manner [27,42]. There has been increasing focus on accurate characterization of the antigen profile of B. anthracis, and the findings from some of these studies are summarized in Table 1 and in Chitlaru et al. [35]. However, a majority of the studies characterizing these proteins have largely focused on chromosomal proteins or a small subset of virulence plasmid proteins. Our novel approach was designed to target the entirety of the virulence plasmid-encoded proteins to determine whether the virulence plasmids contain multiple, previously uncharacterized immunoreactive targets. To carry out this investigation, we adapted a ligation-independent cloning technique using the ColE1 promoter to allow for use in low-aeration conditions and of the SOS response to mitomycin C to drive expression of recombinant proteins [37]. ColE1-driven expression of these proteins was improved under low aeration conditions, and approximately 57% of these clones expressed as full-length proteins detected by Western blot at the predicted size. This cloning technique was chosen because it enabled cloning of a large number of B. anthracis genes with a single primer design without the need for relatively expensive recombinanses and produced more efficient expression under the unique low-aeration conditions experienced during growth in 96-well boxes.
One strength of this system lies in its ability to be used in any project aiming to create and express a large clone set. With the exception of primer design, there should be little need to vary the protocol described here for future projects, and the SOS expression mechanism is optimized for oxygen conditions common in 96-well culture boxes. In addition, the ability to purify recombinant proteins from this high-throughput expression system contributes further to its strength. It is also noteworthy that these studies describe expression of Gram-positive B. anthracis genes in a Gram-negative E. coli strain, and as such these conditions are likely suboptimal for expression of B. anthracis genes. Attempts to express proteins from a Gram-negative system may result in greater success than was observed here.
To this point, some observations were made that could speak to general expression of heterologous proteins from B. anthracis in E. coli. While 44% of the proteins that expressed well have been annotated as hypothetical proteins, 18% of those that did have an annotated function were associated with DNA binding. Of the DNA binding proteins, 45% were associated with transposase biology. The high frequency of transposase-related proteins is not surprising. An increased understanding of transposes in general has allowed new genome sequencing projects to accurately identify these genes in their respective organisms. In addition, transposons are often associated with plasmids, providing their hosts with the ability to modify chromosomal genes and sustain a limited degree of variability that may ultimately benefit their overall fitness. An unexpected result was that we observed reasonable expression of proteins associated with external structures in B. anthracis, including components of the S-layer, spore, and capsule. Considering that these structures are unique to Gram-positive bacteria, faulty expression might have been expected in our Gram-negative system.
Screening expressed proteins with serum from multiple infection models identified 17 proteins that were immunogenic in at least two of our animal infection models. Importantly, 15 of these had not been previously identified in other studies, and eight of the 15 were immunoreactive in all three models. Further studies characterizing these candidates will reveal which, if any, may provide protection in a recombinant protein-based vaccine. Many of the immunoreactive proteins are annotated as hypothetical proteins. However, pXO2-42, found to be reactive in immunoreactivity screens here and elsewhere [22,23], is an S-layer amidase predicted to localize to the external cell surface. This suggests that pXO2-42 is readily accessible to the humoral immune response and therefore should be prioritized in future protection studies.
In addition, all previously reported immunogenic proteins that we expressed in the system described here were also found to be immunoreactive, suggesting that this reactivity is not due to any B. anthracis-specific post-translational modifications. This information may prove useful if the need arises to produce any of these proteins in heterologous systems for vaccine trials.
While the AVA vaccine screen did not identify any targets other than the expected antibody interaction with PA, it provided further evidence that a multi-component subunit vaccine may be optimal to obtain maximum protection. If antibodies are raised against a greater number of targets during a natural infection, it would follow that there are a number of additional subunit candidates which may enhance protection compared to using PA only. Further studies will reveal which of the candidates described here may afford protection and could be combined with PA to create an improved protein-based recombinant vaccine against anthrax.
5. Conclusions
For cloning and expression of large numbers of genes, the ligation-independent cloning method described here was shown to be efficient and amenable for high-throughput DNA manipulations, protein expression and protein purification. Application of this technique to express the genes encoded on the B. anthracis pXO1 and pXO2 virulence plasmids led to the subsequent identification of 10 immunoreactive and/or antigenic proteins that could enhance the protective capacity of the current AVA vaccine or contribute to the design of a completely new anthrax vaccine
Supplementary Material
We created a high-throughput expression clone set for B. anthracis pXO1 and pXO2 plasmids. > We adapted ligation-independent cloning technique for expression in low-oxygen conditions. > Expression totals and quality was determined. > Animal serum was used to identify 8 previously unidentified immunogenic proteins.
Acknowledgments
The authors would like to thank Dr. Anthony Maresso, Dr. Daniel Catanese, and Embriette Alicki for the assistance and critical reading and editing of the manuscript; Dr. Johnny Peterson, Dr. Hank Heine, and Dr. Conrad P. Quinn for access to serum from infection studies; Dr. Wendy Keitel for critical insight and discussion regarding the study, and access to AVA human serum. This research was conducted with financial support from United States National Institutes of Health/National Institute of Allergy and Infectious Diseases SBIR 1R41 AI52522-01; Baylor College of Medicine.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Brian D. McWilliams, Email: bdmcwill@bcm.edu.
Timothy Palzkill, Email: timothyp@bcm.edu.
George M. Weinstock, Email: gweinsto@genome.wustl.edu.
References
- 1.Brachman P. Inhalation Anthrax. Ann NY Acad Sci. 1980;353(1):83–93. doi: 10.1111/j.1749-6632.1980.tb18910.x. [DOI] [PubMed] [Google Scholar]
- 2.LaForce F. Anthrax. Clin Infect Dis. 1994;19(6):1009–1013. doi: 10.1093/clinids/19.6.1009. [DOI] [PubMed] [Google Scholar]
- 3.Keim P, Smith KL, Keys C, Takahashi H, Kurata T, Kaufmann A. Molecular investigation of the Aum Shinrikyo anthrax release in Kameido, Japan. J Clin Microbiol. 2001;39(12):4566–4567. doi: 10.1128/JCM.39.12.4566-4567.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meselson M, Guilleman J, Huge-Jones M, Langmuir A, Shelokov A, Yampolskaya O. The Sverdlovsk anthrax outbreak of 1979. Science. 1994;266(5188):1202–1208. doi: 10.1126/science.7973702. [DOI] [PubMed] [Google Scholar]
- 5.Willis EA. Landscape with dead sheep: what they did to Gruinard Island. Med Confl Surviv. 2002;18(2):199–210. doi: 10.1080/13623690208409625. [DOI] [PubMed] [Google Scholar]
- 6.Jernigan DB, Raghunathan PL, Bell BP, Brechner R, Bresnitz EA, Butler JC, et al. Investigation of bioterrorism-related anthrax, United States, 2001: epidemiologic findings. Emerg Infect Dis. 2002;8(10):1019–1028. doi: 10.3201/eid0810.020353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Okinaka RT, Cloud K, Hampton O, Hoffmaster AR, Hill KK, Keim P, et al. Sequence and organization of pXO1, the large Bacillus anthracis plasmid harboring the anthrax toxin genes. J Bacteriol. 1999;181(20):6509–6515. doi: 10.1128/jb.181.20.6509-6515.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dixon TC. Anthrax. N Engl J Med. 2010;341(11):815–826. doi: 10.1056/NEJM199909093411107. [DOI] [PubMed] [Google Scholar]
- 9.Turnbull PC, Broster MG, Carman JA, Manchee RJ, Melling J. Development of antibodies to protective antigen and lethal factor components of anthrax toxin in humans and guinea pigs and their relevance to protective immunity. Infect Immun. 1986;52(2):356–363. doi: 10.1128/iai.52.2.356-363.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Friedlander AM, Pittman PR, Parker GW. Anthrax vaccine: evidence for safety and efficacy against inhalational anthrax. JAMA. 1999;282(22):2104–2106. doi: 10.1001/jama.282.22.2104. [DOI] [PubMed] [Google Scholar]
- 11.Fritz DL, Jaax NK, Lawrence WB, Davis KJ, Pitt ML, Ezzell JW, et al. Pathology of experimental inhalation anthrax in the rhesus monkey. Lab Invest. 1995;73(5):691–702. [PubMed] [Google Scholar]
- 12.Phipps AJ, Premanandan C, Barnewall RE, Lairmore MD. Rabbit and nonhuman primate models of toxin-targeting human anthrax vaccines. Microbiol Mol Biol Rev. 2004;68(4):617–629. doi: 10.1128/MMBR.68.4.617-629.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grabenstein JD. Vaccines: countering anthrax: vaccines and immunoglobulins. Clin Infect Dis. 2008;46(1):129–136. doi: 10.1086/523578. [DOI] [PubMed] [Google Scholar]
- 14.Turnbull PC. Anthrax vaccines: past, present and future. Vaccine. 1991;9(8):533–539. doi: 10.1016/0264-410x(91)90237-z. [DOI] [PubMed] [Google Scholar]
- 15.Whiting GC, Rijpkema S, Adams T, Corbel MJ. Characterisation of adsorbed anthrax vaccine by two-dimentional gel electrophoresis. Vaccine. 2004;22(31-32):4245–4251. doi: 10.1016/j.vaccine.2004.04.036. [DOI] [PubMed] [Google Scholar]
- 16.Pittman PR, Kim-Ahn G, Pifat DY, Coonan K, Gibbs P, Little S, Pace-Templeton JG, et al. Anthrax vaccine: immunogenicity and safety of a dose-reduction, route-change comparison study in humans. Vaccine. 2002;20(9-10):1412–1420. doi: 10.1016/s0264-410x(01)00462-5. [DOI] [PubMed] [Google Scholar]
- 17.Little SF, Ivins BE, Fellows PF, Pitt ML, Norris SL, Andrews GP. Defining a serological correlate of protection in rabbits for a recombinant anthrax vaccine. Vaccine. 2004;22(3-4):422–430. doi: 10.1016/j.vaccine.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 18.Ivins BE, Pitt ML, Fellows PF, Farchaus JW, Benner GE, Waag DM, et al. Comparative efficacy of experimental anthrax vaccine candidates against inhalation anthrax in rhesus macaques. Vaccine. 1998;16(11-12):1141–1148. doi: 10.1016/s0264-410x(98)80112-6. [DOI] [PubMed] [Google Scholar]
- 19.Friedlander AM, Little SF. Advances in the development of next-generation anthrax vaccines. Vaccine. 2009;27(4):D28–D32. doi: 10.1016/j.vaccine.2009.08.102. [DOI] [PubMed] [Google Scholar]
- 20.Gorse GJ, Keitel W, Keyserling H, Taylor DN, Lock M, Alves K, et al. Immunogenicity and tolerance of ascending doses of a recombinant protective antigen (rPA102) anthrax vaccine: A randomized, double-blinded, controlled, multicenter trial. Vaccine. 2006;24(33-34):5950–5959. doi: 10.1016/j.vaccine.2006.05.044. [DOI] [PubMed] [Google Scholar]
- 21.Jefferson T, Rudin M, DiPietrantonj C. Systematic review of the effects of pertussis vaccines in children. Vaccine. 2003;21(17-18):2003–2014. doi: 10.1016/s0264-410x(02)00770-3. [DOI] [PubMed] [Google Scholar]
- 22.Rollins SM, Peppercorn A, Young JS, Drysdale M, Baresch A, Bilkowski MV, et al. Application of in vivo induced antigen technology (IVIAT) to Bacillus anthracis. PLoS One. 2008;3(3):e1824. doi: 10.1371/journal.pone.0001824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gat O, Horsey A, Ariel N, Inbar I, Zaide G, Broder Y, et al. Search for Bacillus anthracis potential vaccine candidates by a functional genomic-serologic screen. Infect Immun. 2006;74(7):3987–4001. doi: 10.1128/IAI.00174-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ariel N, Zvi A, Makarova KS, Chitlaru T, Elhanany E, Velan B, et al. Genome-based bioinformatic selection of chromosomal Bacillus anthracis putative vaccine candidates coupled with proteomic identification of surface-associated antigens. Infect Immun. 2003;71(8):4563–4579. doi: 10.1128/IAI.71.8.4563-4579.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu YT, Lin SB, Huang CP, Huang CM. A novel immunogenic spore coat-associated protein in Bacillus anthracis: characterization via proteomics approaches and a vector-based vaccine system. Protein Expr Purif. 2008;57(1):72–80. doi: 10.1016/j.pep.2007.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ariel N, Zvi A, Grosfeld H, Gat O, Inbar Y, Velan B, et al. Search for potential vaccine candidate open reading frames in the Bacillus anthracis virulence plasmid pXO1: in silico and in vitro screening. Infect Immun. 2002;70(12):6817–6827. doi: 10.1128/IAI.70.12.6817-6827.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brahmbhatt TN, Darnell SC, Carvalho HM, Sanz P, Kang TJ, Bull RL, et al. Recombinant exosporium protein BclA of Bacillus anthracis is effective as a booster for mice primed with suboptimal amounts of protective antigen. Infect Immun. 2007;75(11):5240–5247. doi: 10.1128/IAI.00884-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walz A, Mujer CV, Connolly JP, Alefantis T, Chafin R, Dake C, et al. Bacillus anthracis secretome time course under host-stimulated conditions and identification of immunogenic proteins. Proteome Sci. 2007;5(11) doi: 10.1186/1477-5956-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chitlaru T, Ariel N, Zvi A, Lion M, Velan B, Shafferman A, et al. Identification of chromosomally encoded membranal polypeptides of Bacillus anthracis by a proteomic analysis: prevalence of proteins containing S-layer homology domains. Proteomics. 2004;4(3):677–691. doi: 10.1002/pmic.200300575. [DOI] [PubMed] [Google Scholar]
- 30.Delvicchio VG, Connolly JP, Alefantis TG, Walz A, Quan MA, Patra G, et al. Proteomic profiling and identification of immunodominant spore antigens of Bacillus anthracis, Bacillus cereus, and Bacillus thuringiensis. Appl Environ Microbiol. 2006;72(9):6355–6363. doi: 10.1128/AEM.00455-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chabot DJ, Scorpio A, Toberey SA, Little SF, Norris SL, Friedlander AM. Anthrax capsule vaccine protects against experimental infection. Vaccine. 2004;23(1):43–47. doi: 10.1016/j.vaccine.2004.05.029. [DOI] [PubMed] [Google Scholar]
- 32.Wimer-Macken S, Hinchcliffe M, Petrie CR, Warwood SJ, Tino WT, Williams MS, et al. An intranasal vaccine targeting both the Bacillus anthracis toxin and bacterium provides protection against aerosol spore challenge in rabbits. Vaccine. 2006;24(18):3953–3963. doi: 10.1016/j.vaccine.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 33.Cybulski RJ, Sanz P, McDaniel D, Darnell S, Bull RL, O'Brien A. Recombinant Bacillus anthracis spore proteins enhance protection of mice primed with suboptimal amounts of protective antigen. Vaccine. 2008;26(38):4927–4939. doi: 10.1016/j.vaccine.2008.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gat O, Horsey A, Ariel N, Inbar I, Zaide G, Broder Y, et al. Search for Bacillus anthracis potential vaccine candidates by a functional genomic-serologic screen. Infect Immun. 2006;74(7):3987–4001. doi: 10.1128/IAI.00174-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chitlaru T, Altboum Z, Reuveny S, Shafferman A. Progress and novel strategies in vaccine development and treatment of anthrax. Immunological Reviews. 2011;239:221–236. doi: 10.1111/j.1600-065X.2010.00969.x. [DOI] [PubMed] [Google Scholar]
- 36.Okinaka RT, Cloud K, Hampton O, Hoffmaster AR, Hill KK, Keim P, et al. Sequence and organization of pXO1, the large Bacillus anthracis plasmid harboring the anthrax toxin genes. J Bacteriol. 1999;181(20):6509–6515. doi: 10.1128/jb.181.20.6509-6515.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eraso J, Chidambaram M, Weinstock G. Increased production of Colicin E1 in stationary phase. J Bacteriol. 1996;178(7):1928–1935. doi: 10.1128/jb.178.7.1928-1935.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reece KS, Phillips GJ. New plamids carrying antibiotic-resistance cassettes. Gene. 1995;165(1):141–142. doi: 10.1016/0378-1119(95)00529-f. [DOI] [PubMed] [Google Scholar]
- 39.Heine HS, Bassett J, Miller L, Hastings JM, Ivins BE, Pitt ML, et al. Determination of antibiotic efficacy against Bacillus anthracis in a mouse aerosol challenge model. Antimicrob Agents Chemother. 2007;51(4):1373–1379. doi: 10.1128/AAC.01050-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peterson JW, Corner JE, Noffsinger DM, Wenglikowski A, Walberg KG, Chatuev BM, et al. Human monoclonal anti-protective antigen antibody completely protects rabbits and is synergistic with ciprofloxacin in protecting mice and guinea pigs against inhalation anthrax. Infect Immun. 2006;74(2):1016–1024. doi: 10.1128/IAI.74.2.1016-1024.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Salles B, Weisemann JM, Weinstock GM. Temporal control of colicin E1 induction. J Bacteriol. 1987;169(11):5028–5034. doi: 10.1128/jb.169.11.5028-5034.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chichester JA, Musiychuk K, de la Rosa P, Horsey A, Stevenson N, Ugulava N, et al. Immunogenicity of a subunit vaccine against Bacillus anthracis. Vaccine. 2007;25(16):3111–3114. doi: 10.1016/j.vaccine.2007.01.068. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.