Abstract
Background:
The pipeline embolization device (PED) provides effective, durable and safe endovascular reconstruction of large and giant intracranial aneurysms. However, 80% of all cerebral aneurysms found in the general population are less than 10 mm in size. Treatment of small aneurysms (<10 mm) with flow diverters may be advantageous over endosaccular modalities that carry risks of procedural rupture during aneurysm access or coil placement.
Methods:
We retrospectively reviewed a prospective, single-center aneurysm database to identify all patients with small (<10 mm) internal carotid artery (ICA) aneurysms who underwent endovascular treatment using the PED. Patient demographics, aneurysm characteristics, procedural details, complications, and technical and clinical outcomes were analyzed.
Results:
Forty-four cases were performed in 41 patients (age range 31-78 years). PED was successfully implanted in 42 cases. A single PED was used in 37/42 (88%) cases. Mean postprocedure hospital stay was 1.7 ± 0.3 days and 98% of patients were discharged home. Major complication occurred in one patient (2.3%), who died of early subarachnoid hemorrhage. Transient neurological deficit, delayed intracerebral hemorrhage (asymptomatic), and delayed groin infection occurred in one patient each. Follow-up rate was 91.8% (45 aneurysms in 35 patients) with a mean follow-up of 4.0 ± 1.9 months. By 6 months post-PED implantation, angiographic success (complete or near complete aneurysm occlusion) was observed in 80%. Mild (<50%), asymptomatic, nonflow limiting in-stent stenosis was observed in 5.4% (2/37 cases). All the 35 patients with follow-up remained at preprocedure neurological baseline.
Conclusion:
Small (<10 mm) ICA aneurysm treatment with PED implantation is safe and carries a high rate of early angiographic success.
Keywords: Cerebral aneurysms, flow diverter, pipeline embolization device
INTRODUCTION
Since its inception in 2007, flow-diverting technology has revolutionized the treatment approach of large and giant cerebral aneurysms from an endosaccular to an endoluminal focus. This innovative strategy has enabled successful endovascular treatment of intracranial aneurysms previously considered difficult to treat with the conventional modalities of clipping and coiling with or without adjunctive devices (i.e., large, giant, wide-necked, or with diffuse circumferential involvement of the parent artery).[6,11,18,19,21,30] The Pipeline embolization device (PED; Covidien Vascular Therapies, Mansfield, MA) is currently the only Food and Drug Administration (FDA)-approved flow diverter available in the United States. Its on-label usage as dictated by the FDA is limited to the treatment of large or giant (≥10 mm) wide-necked intracranial aneurysms from the petrous to the superior hypophyseal segments of the internal carotid artery (ICA).[32] Clinical experience worldwide with PED has demonstrated the effectiveness, durability, safety, and cost-effectiveness of endovascular reconstruction primarily in large and giant aneurysms[5,8,19,30] Rates of occlusion at 6 months following PED treatment of such aneurysms have been impressive, ranging from 81.8% to 94.4%.[18,21,30,33]
Nevertheless, large and giant intracranial aneurysms only encompass a small fraction of all intracranial aneurysms. In contrast, over 80% of all cerebral aneurysms found in the general population are less than 10 mm in size.[31,35] There is considerable documentation in the literature that the majority of ruptured aneurysms are smaller than 10 mm.[13,14,26,34] Treatment of small aneurysms (<10 mm) with flow diverters may be advantageous over endosaccular modalities, which inherently carry a risk of procedural rupture during access of the aneurysm sac or coil placement.[2,20,22,29] Specific data regarding the procedural, angiographic, and clinical outcomes of PED treatment in small aneurysms is limited in the literature and commonly reported in conjunction with series on large and giant aneurysms.[12,18,27,30]
In this report, we present periprocedural outcomes and 2- to 6-month angiographic follow-up results for a series of 44 cases with ICA aneurysms less than 10 mm in size that were treated with the PED at a single-center by a single-operator.
MATERIALS AND METHODS
Patient selection
We retrospectively reviewed a prospective, single-center aneurysm database to identify all patients with small (<10 mm) ICA aneurysms who underwent endovascular treatment using the PED. Data with respect to the following variables were prospectively collected: patient demographics, anatomic characteristics of the aneurysm, details of the interventional procedure, procedural and periprocedural complications, and technical and clinical outcomes. Patients presenting with severe headache and clinical suspicion for subarachnoid hemorrhage (SAH) were screened with a computed tomography (CT) scan of the head and, if necessary, lumbar puncture to rule out a hemorrhage event.
Endovascular procedure
Embolization procedures were performed as previously published.[6] In brief, all patients were treated preoperatively with a dual antiplatelet regimen consisting of aspirin 325 mg daily and clopidogrel 75 mg daily for 7 days prior to the intervention. The degree of P2Y12 receptor inhibition was not routinely tested. All procedures were performed with systemic anticoagulation using heparin with a 5000-unit bolus at the start of each case followed by an intraprocedure rebolus of 1000 units at each additional hour. The goal of each procedure was complete coverage of the aneurysm neck or fusiform/diseased vessel segment with the PED and maximum vessel wall apposition along the length of the PED. A triaxial system was used through femoral access. This consisted of a 6 French Flexor Shuttle sheath (Cook Medical, Bloomington, IN), a 5 French Navien distal intracranial catheter (formerly ReFlex Distal Intracranial Catheter) (Covidien Vascular Therapies, Mansfield, MA) serving as the guide catheter[7] and a Marksman microcatheter (Covidien Vascular Therapies, Mansfield, MA). The distal PED was opened in the ipsilateral supraclinoid ICA or, more commonly, in the ipsilateral M1 segment. Proper device expansion and deployment was assessed with native fluoroscopy. If a partially deployed PED did not open properly secondary to device failure or was malpositioned, the device was corked and removed.[5] Control digital subtraction angiography (DSA) was performed immediately after deployment and at 5 and/or 10 minutes after deployment to confirm patency of the parent vessels and to rule out intraluminal thrombus. At the end of the procedure, a Dyna CT scan without contrast was performed to assess PED morphology and to evaluate for intracranial hemorrhage. Groin closure and hemostasis was achieved with manual compression after allowing several hours for the PTT to normalize postprocedure.
Procedural assessment and follow-up
Procedural outcomes evaluated include the removal of incompletely deployed PED, the number of cases successfully completed, length of postprocedure hospital stay, number of patients discharged home, and immediate angiographic results. Immediate angiographic results were graded based on contrast stasis within the aneurysm using our previously described scale of mild, moderate or pronounced stasis and complete occlusion.[6] Procedural and periprocedural complications were also recorded and evaluated. These categories included mortality, transient neurological deficit, major and minor stroke, intracerebral hemorrhage (ICH), SAH, cranial nerve palsy, PED thrombosis, vessel dissection, and groin complications. Major stroke was defined as stroke present after 7 days that increased the NIH stroke scale by ≥4 points, and minor stroke was defined as a stroke that resolved completely within 7 days or increased the NIH stroke scale by ≤3 points. Groin complications included groin infection or significant groin hematoma, defined as a hematoma requiring prolonged hospital stay or preventing ambulation.
Follow-up angiographies were performed at 2-3 or 6-month post-PED implantation. Standard projections and the original working projections for PED deployment were used to assess any residual flow within the aneurysms. Aneurysm occlusion was classified as complete occlusion, near-complete occlusion (with trace residual aneurysm filling), or persistent filling. In-stent stenosis was calculated on the basis of the minimal lumen diameter, and was graded as none (0% to <25%), mild (25% to <50%), moderate (50% to <75%), or severe (75-100%). Dual antiplatelet therapy consisting of aspirin 325 mg daily and clopidogrel 75 mg daily was continued for 6 months postprocedure. After 6 months, patients were instructed to discontinue clopidogrel and continued daily aspirin 325mg until their 1-year follow-up angiography.
Data are presented as counts, percentages and means. When means are presented, the standard error of the mean (SEM) is used to assess sample distribution.
RESULTS
Patient and aneurysm characteristics
Between September 2011 and July 2012, 41 consecutive patients with a total of 53 unruptured small ICA aneurysms less than 10 mm were treated with the PED. The mean age of the patients was 54.9 years (range 31-78). Table 1 presents the patient demographics and aneurysm characteristics. Of the 41 patients, 38 (92.7%) were women and 3 (7.3%) were men. Twenty-eight (68.3%) of the patients were White, 11 (26.8%) were Black, 1 (2.4%) was Asian, and 1 (2.4%) was Hispanic.
Table 1.
Patient demographics and aneurysm characteristics
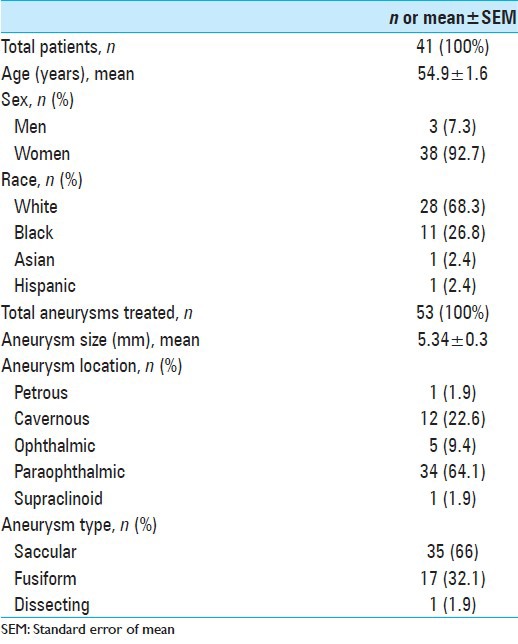
Of the 53 ICA aneurysms treated, the majority was paraophthalmic/clinoidal (34/53, 64.1%). Cavernous, ophthalmic, supraclinoid, and petrous locations accounted for 12 (22.6%), 5 (9.4%), 1 (1.9%), and 1 (1.9%), respectively. Seven of the cavernous aneurysms treated were in patients who had adjacent primary paraophthalmic aneurysm and the petrous aneurysm treated was a posttraumatic dissecting aneurysm. The mean size of the aneurysms treated was 5.34 ± 0.3 mm. Of the 53 treated aneurysms, 35 (66%) were saccular, 17 (32.1%) were fusiform and 1 (1.9%) was dissecting. Fusiform aneurysms were defined as involving >25% of the parent artery circumference. None of the patients treated presented with SAH and none had preexisting indwelling endoluminal devices.
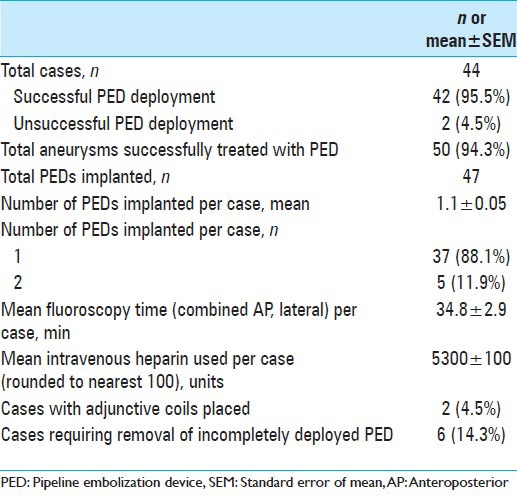
PED treatment characteristics
Altogether, 44 treatments were performed in 41 patients with a total of 53 aneurysms. The details from these procedures are shown in Table 2. Three patients had bilateral paraophthalmic ICA aneurysms and these were treated on separate dates. Six patients had multiple aneurysms that were treated during a single procedure. For each of these six patients, the additional aneurysms were ipsilateral and adjacent to the primary aneurysm. Of the 44 cases, 2 cases (with 3 aneurysms) were unsuccessful PED implantations secondary to significant tortuosity of the distal ICA. Of the 42 cases with successful PED implantation, a total of 50 aneurysms were treated. Thirty-seven of these cases (88.1%) required only a single PED while five cases (11.9%) required two PEDs. Removal of incompletely deployed PED (“corking”) occurred in 6 of the 42 cases (14.3%). A total of 54 PEDs were used and 47 (87%) were successfully implanted. PEDs were removed either secondary to technical failure of the device to open or secondary to device malposition. None of the cases required additional balloon angioplasty after PED implantation. This was a function of using the technique whereby the distal PED end was first properly positioned and well apposed to the parent vessel wall prior to completing final PED deployment. Adjunctive coils were placed immediately prior to device deployment in two cases (4.8%). The duration of fluoroscopy and amount of systemic heparin administered were used as an estimate of procedure length. The mean fluoroscopy time and mean intravenous heparin dose were 34.8 ± 2.9 minutes and 5,300 ± 100 units, respectively.
Table 2.
PED treatment details
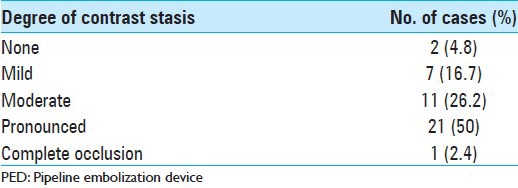
Immediate angiographic and clinical outcomes
Immediate angiographic results at the end of the procedure are presented in Table 3. Immediate complete angiographic occlusion was observed in one patient (2.4%) with a 6 mm fusiform cavernous aneurysm. Pronounced, moderate, and mild contrast stasis was observed in 21 (50%), 11 (26.2%), and 7 (16.7%) patients, respectively. Two patients (4.8%) had no contrast stasis within the aneurysm sac upon conclusion of the procedure. Both these patients had fusiform paraopthalmic artery aneurysms, 3 and 7 mm in size.
Table 3.
Immediate angiographic results following PED deployment
The mean postprocedure length of hospital stay for all patients was 1.7 ± 0.3 days. Two patients had total hospital stays of >5 days secondary to periprocedural complications compounded by baseline medical comorbidities as detailed below. In total, 40 of 41 patients (98%) were discharged home following treatment.
Periprocedural complications
Periprocedural complications are presented in Table 4. Of the 44 cases, major clinical periprocedural complication was encountered in one patient (2.3%), which has been described in detail in a prior publication.[6] In summary, the patient had emerged from anesthesia neurologically intact after successful PED implantation for a 3 mm wide-necked left-sided paraophthalmic artery aneurysm. Five hours after, she developed a change in mental status secondary to interval new acute SAH. Immediate post-SAH angiography demonstrated no change in the aneurysm morphology and no contrast extravasation. The timing of the hemorrhage is most consistent with a wire perforation during the initial procedure. Despite maximal medical and surgical interventions, the patient died from complications from the SAH.
Table 4.
Periprocedural complications
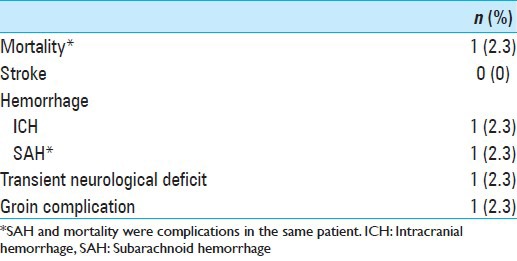
Transient neurological deficit occurred in one patient (2.3%). This patient with uncontrolled hypertension and a prior left-sided middle cerebral artery stroke had transient mild speech and vision changes in the setting of elevated systolic blood pressure following PED treatment of tandem left paraophthalmic and cavernous aneurysms. None of the patients treated had a major or a minor ischemic stroke. However, one patient (2.3%) had delayed ICH in the right occipital lobe 3 days after a technically uncomplicated PED treatment for a 4 mm right-sided paraopthalmic artery aneurysm. This patient was receiving systemic anticoagulation for a recent deep vein thrombosis, and the hemorrhage occurred during the heparin to warfarin transition. This patient was ultimately discharged to home in good condition on postprocedure day 11.
None of the patients treated experienced new or exacerbation of cranial nerve palsy, in situ PED thrombosis, iatrogenic vessel dissection, or significant groin hematoma. Delayed groin infection was observed in one patient (2.3%), which was treated with oral antibiotics without further complication.
Follow-up angiographic and clinical outcomes
Of the 38 surviving patients successfully treated with PED implantation there were a total of 49 aneurysms treated. Follow-up angiography has been done for 45/49 (91.8%) aneurysms, with a mean follow-up of 4.0 ± 1.9 months. Table 5 details the aneurysm characteristics and the angiographic outcomes of the aneurysms with follow-up. Of the 45 aneurysms with angiographic follow-up, 24 aneurysms had early follow-up at 2-3 months postprocedure, and 21 aneurysms at 6 months. Table 6 summarizes the observed angiographic occlusion rates at follow-up. Angiographic success, defined as having complete angiographic occlusion or near complete occlusion, was observed in 18/24 (75%) aneurysms at 2-3 month follow-up and 18/21 (85.7%) aneurysms at 6-month follow-up. Figures 1 and 2 show aneurysms with angiographic success at 2-3 months after PED treatment. Six aneurysms had persistent filling on 2-3 month follow-up angiography and have the following angioarchitecture: one fusiform, one medial cavernous, one medial paraophthalmic, one lateral paraophthalmic, and two ophthalmic. Of the 37 vessels with angiographic follow-up, 2 (5.4%) showed nonflow limiting mild (25% to <50%) in-stent stenosis. Both of these cases were asymptomatic and, thus, neither was treated. Additionally, there were no instances of PED migration on follow-up angiography. Of the 35 patients with follow-up, all remained at preprocedure neurological baseline.
Table 5.
Immediate and follow-up anatomic outcome in 35 cases (33 patients) with 42 treated aneurysms
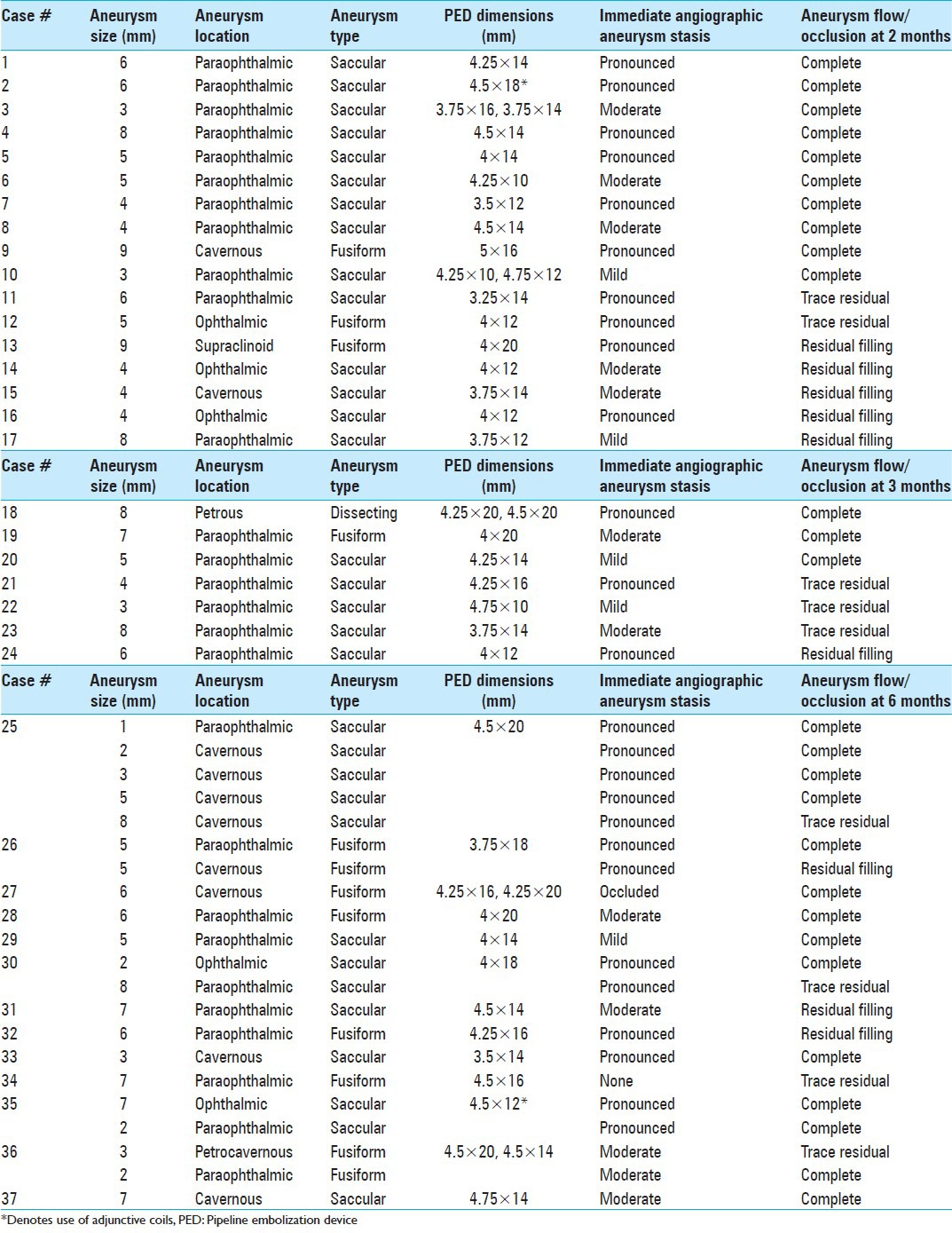
Table 6.
Follow-up angiographic occlusion rate
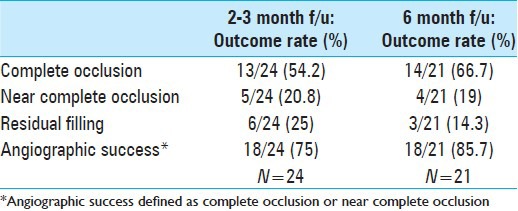
Figure 1.
PED treatment of a 6 mm paraophthalmic aneurysm with angiographic success at 2 months (Case 1). (a) Preembolization DSA. (b) Immediately after implantation there is pronounced contrast stagnation within the aneurysm persisting into the venous phase. (c) Two-month follow-up DSA demonstrates complete angiographic occlusion
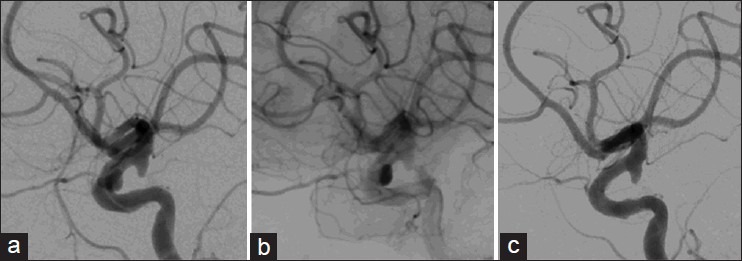
Figure 2.
PED treatment of a 6 mm paraophthalmic aneurysm with angiographic success at 2 months (Case 11). (a) Preembolization DSA. (b) Immediately after implantation there is pronounced contrast stagnation within the aneurysm persisting into the venous phase. (c) Two-month follow-up DSA demonstrates near complete angiographic occlusion with only trace filling of the aneurysm (arrow)
DISCUSSION
We present in this report a dedicated series investigating the safety and efficacy of the PED for treatment of small ICA aneurysms less than 10 mm in size. The PED was successfully implanted in 39 patients with 50 aneurysms. A single PED was used in 88.1% of the cases. Ninety-eight percent of patients were discharged home following the embolization procedure. Of the 44 cases in this series, a major periprocedural complication of death secondary to SAH occurred in 1 patient (2.3%). Transient neurological deficit, delayed ICH, and delayed groin infection occurred in one patient each (2.3% each). Of the 49 surviving aneurysms successfully treated, the follow-up rate was 91.8%. By 6 months following PED implantation, angiographic success was observed in 80%. Mild, nonflow limiting, in-stenosis was observed at a rate of 5.4% (2/37 cases). Of the 35 patients with follow-up, all remained at their neurological baseline.
Parent vessel reconstruction with PED implantation is gradually becoming the endovascular modality of choice for large and giant, fusiform or wide-necked aneurysms. Several series have reproducibly demonstrated that the high technical success rate and durability of PED treatment in these aneurysms can be achieved with a low incidence of complications.[6,18,27] The safety profile of PED treatment has been partially attributed to avoidance of direct catheterization of the saccular component of aneurysms, a process that is associated with a risk of procedural rupture.[18] This risk is particularly high for endosaccular coiling of small aneurysms.[18,19,21] For this reason, an endoluminal approach may also be applicable in the treatment of small aneurysms. Few reports have been published thus far on PED use in small aneurysms.[18,21,27] The majority of these experiences are described in combination with those of the large and giant aneurysms, making it difficult to directly compare outcomes. In Lylyk's report on the initial Buenos Aires Experience with PED implantation in 63 intracranial aneurysms, 33 aneurysms were small (<10 mm), however, this was not further stratified into the number of these aneurysms located along the anterior versus posterior circulation.[18] Similarly, although Saatci et al. provided long-term outcomes on 239 aneurysms treated with the PED of which 136 aneurysms were less than 10 mm in size, detail on the distribution of these small aneurysms along the cerebrovasculature was lacking.[27] This heterogeneity in the literature on PED use complicates the direct comparison of results reported in these studies. Our current series fills this void in the literature by providing the outcomes and follow-up data specific for small ICA aneurysms treated with the PED.
A few publications on PED use do stratify results by anatomical size and location but are limited by a small sample size of aneurysms measuring less than 10 mm along the ICA.[3,10,17,30] In Szikora's initial Budapest experience with the PED, only 5 of the 19 aneurysms treated were along the ICA and less than 10 mm.[30] It is unclear from the report whether periprocedural complications were encountered in PED treatment of these 5 small ICA aneurysms. From the remaining publications, the periprocedural complication rate associated with PED treatment for small ICA aneurysms may be inferred from detailed analysis of the published results. In the Hong Kong PED experience, Chan et al., treated six patients with 10 small ICA aneurysms with 0% major morbidity and mortality rate.[3] In contrast, in Lubicz's PED experience in 20 patients with 27 aneurysms, 9 of these patients had 13 aneurysms less than 10 mm along the ICA.[17] Of these nine patients, one died (11%) as a result of probable PED thrombosis after discontinuation of dual antiplatelet therapy (only clopidogrel daily) in the setting of an ICH that developed 17 hours after PED implantation.[17] This patient had a 3 mm wide-necked ophthalmic artery aneurysm and a 3 mm wide-necked ICA bifurcation aneurysm treated with two PED in a single session. Recently Deutschmann et al. reported results of 12 patients with 12 wide-necked aneurysms treated with PED; 8 of these were ICA aneurysms less than 10 mm.[10] Of their 12 cases, transient mild aphasia was observed in 1 patient and amaurosis fugax was observed in another. Whether either of these two patients (16.6%) had small ICA aneurysms is unclear from the presented data.
Our experience with PED treatment for small ICA aneurysms is comparable to the few published reports on this experience. The 2.3% mortality in our series of 44 cases is closer to the bottom of the range of 0% observed by Chan et al., and 11% observed by Lubicz et al. Compared with the PED experience for large and giant aneurysms with reported mortality rates up to 5.5%,[17,18,21,27,30,32] we reported a mortality rate that is less than half. We did not observe any major morbidity in our series. In contrast, treatment of large and giant aneurysms with PED has been associated with a major morbidity of 1-5.5%.[27,30]
Three of our patients did experience minor complications as follows: transient neurological deficit (n = 1), delayed ICH (n = 1), and delayed groin infection (n = 1). The delayed ICH occurred 3 days after a technically uncomplicated PED treatment for a 4 mm right-sided paraopthalmic artery aneurysm. This patient was receiving systemic anticoagulation for a recent deep vein thrombosis, and the hemorrhage (right occipital ICH) occurred during the heparin to warfarin transition. The patient remained in good neurological condition and was discharged home on postprocedure day 11. The 6.9% rate of minor complications in this report is lower than the minor complication rate reported for PED treatment of large and giant aneurysms, which has been observed as high as 9.4%[18,21,23,30,31] and included occurrences of transient neurological deficits, delayed ICH, exacerbation of cranial neuropathies, delayed groin complications, carotid cavernous fistulas, and device migration.
Our results in this series were achieved without significant ischemic complications. We attribute this to our technique of PED deployment. Prior to fully deploying a PED, we ensured that the distal PED end was fully open and well apposed to the parent vessel wall. In this series, 6 of the 42 cases (14.3%) required removal of an incompletely deployed PED. With this method, none of the cases in this series required additional balloon angioplasty after PED implantation or any other postprocessing maneuvers that would subsequently increase the risk profile of the procedure. Our experience with this technique supports the belief that the primary concern with PED implantation is not ischemic complications but rather hemorrhagic.[15,36] Periprocedural ischemic complications can be managed with intraarterial thrombolytics, whereas hemorrhagic complications are typically associated with major morbidity and mortality in the setting of dual antiplatelet therapy.[28,15,36] As such, we do not routinely test for P2Y12 receptor inhibition. Additionally, the VerifyNow (Accumetrics, San Diego, CA) assay used to measure the degree of P2Y12 receptor inhibition has been demonstrated unreliable with fluctuations observed in serial testing of the same patient.[9] The results also vary from institution to institution and are not associated with a standardized threshold of desired P2Y12 receptor inhibition. Several centers have demonstrated acute titration of clopidogrel dose or replacement with prasugrel (Effient) for “hyporesponders” was associated with increased hemorrhagic complications in PED procedures.[1,9] For these reasons, the utility of P2Y12 testing in PED procedures remains to be validated. Until then, we maintain the safety profile of our PED procedures by following the protocol set by the Pipeline for Uncoilable or Failed Aneurysms (PUFS) trial where P2Y12 testing was not performed and dual antiplatelet regimen consisted of oral aspirin 325 mg and clopidogrel 75 mg daily for 6 months.[32]
Mild in-stent stenosis (25% to <50%) was observed in 2 of the 37 cases (5.4%) with follow-up angiography. Both cases were asymptomatic and required no additional intervention. This rate is less than half the rate (1/7) reported by Chan et al.,[3] and falls within the 3.5-10% range observed in large and giant aneurysms treated by the PED.[18,19,21,30]
Follow-up data in this series demonstrates that complete aneurysm occlusion can be achieved as early as 2 months following PED treatment for small ICA aneurysms. Of the 17 treated aneurysms that had angiographic follow-up at 2 months, almost 60% were completely occluded. At 2-3 months after PED implantation, angiographic success was achieved in 75% demonstrating either complete or near complete occlusion. By 6 months follow-up, this rate increased to 80%. All ICA aneurysms (100%) located along the posterior/ventral surface of the vessel wall achieved angiographic success at all follow-up time points [Figures 1 and 2]. Our results are approximately in line with the obliteration rates observed in other experiences on PED use in small ICA aneurysms. Of the five small ICA aneurysms treated with PED in the report by Szikora et al., all five were completely occluded at 6-month follow-up,[30] while Chan et al., reported an occlusion rate of 70% (7/10) at 2-6 months,[30] and Deutschmann et al., reported a 50% rate at 5-6 months.[10] Lastly, 11 of the 12 small ICA aneurysms treated with PED by Lubicz et al., achieved angiographic success at 3-6 months.[17]
Our occlusion rates are also comparable to those observed for PED treatment of large and giant aneurysms. Complete occlusion rates for large and giant aneurysms are over 80%, however, the majority of follow-up in these studies were performed at 6- or 12-month intervals and also confounded by adjunctive coil use as well as a higher number of PEDs implanted.[18,19,21,27,31] In contrast, Lylyk and colleagues found only a 47% 3-month obliteration rate for large and giant aneurysms. As such, results from our series demonstrating a 75% angiographic success for PED treatment of small ICA aneurysms at 2-3 months follow-up support the hypothesis proposed by several groups that small aneurysms may achieve occlusion faster than large and giant aneurysms.[8,18,27] In addition, our high angiographic success rate is achieved with an average of 1.1 ± 0.05 PEDs implanted per case. This is in contrast to the average of 3.1 PEDs used per case in the PUFS trial demonstrating over 80% occlusion at 6 months.[32] The ability to achieve early angiographic success with only a single PED for the majority (>80%) of the cases in this report illustrates the elegance and good economy of the endoluminal approach via flow diversion with PED for the treatment of small ICA aneurysms.
In this series, we have demonstrated the safety and efficacy of PED implantation for the treatment of small ICA aneurysms. Compared with the literature on PED treatment of large and giant aneurysms,[8,18,21,23,30,31] we report a lower complication rate and demonstrate high early angiographic success in the PED treatment of small ICA aneurysms. Additionally, compared with traditional endovascular modalities of coiling with or without adjunctive devices, PED use for small ICA aneurysms has several potential advantages. Unlike coiling, aneurysm occlusion with PED is a progressive biologic process. As such, a PED treated aneurysm with a small residual on initial follow-up imaging will typically progress to complete angiographic occlusion over time. In contrast, a small neck remnant of a coiled aneurysm either persists or enlarges and subsequently requires additional treatment. A significant advantage of the endoluminal approach is avoidance of the most feared risk of intraprocedural aneurysm rupture during access or coil placement inherent to endosaccular techniques.[2,20,22,29] For unruptured aneurysms, this intraprocedural rupture risk ranges from 1.2% to 4%[16,24,29] and is associated with high rates of morbidity and mortality. The combined risk of permanent neurologic disability and death associated with intraprocedural rupture is as high as 29% for unruptured aneurysms.[4] Small aneurysm size is a known risk factor for intraprocedural rupture and well documented in the literature.[2,20,22,24] For aneurysms 6 mm or smaller, this risk approaches 5%[2,20,22,24] with an estimated mortality ranging from 1% to 16.7%[20,24,29] and major morbidity of 27.8%.[24] Considering this risk profile for treating small aneurysms with endosaccular techniques, the 2.3% major morbidity and mortality reported in this series of PED treatment for small ICA aneurysms supports an endoluminal approach as a valid alternative. The durability of PED treatment is another advantage of using this modality for small ICA aneurysms. The recurrence rate of aneurysms less than 10 mm treated with coiling has been reported as high as 21% with approximately half requiring retreatment.[25]
At present in the United States, the FDA has limited the on-label indication of PED use to large and giant ICA aneurysms. Large and giant intracranial aneurysms only encompass a small fraction of the cerebral aneurysms observed in population studies.[31,33,35] The International Study of Unruptured Intracranial Aneurysms (ISUIA) reported that 73.9% of the observed 1449 cerebral aneurysms were characterized as small, less than 10 mm.[31] In a meta-analysis of the literature on the prevalence of unruptured intracranial aneurysms, Vlak et al. found that 83% of the aneurysms were small.[33] Most recently, the Japanese have published the largest prospective cohort on the natural history of unruptured cerebral aneurysms. Of the 6679 aneurysms observed, aneurysms less than 10 mm accounted for 89.6%.[33] What's more, several reports indicate that the majority of ruptured aneurysms are smaller than 10 mm.[13,14,26,34] Given these findings, PED implantation has the potential to further revolutionize the endovascular approach for intracranial aneurysm treatment. Internationally, several series on PED experience include data on treatment of small aneurysms.[3,17,30] We present the largest series to date on PED treatment of small ICA aneurysms. Our results show that these aneurysm types can be safely treated with PED implantation. Furthermore, high angiographic success in these aneurysms can be reached as early as 2 months posttreatment. Early angiographic success represents the potential for complete parent vessel reconstruction sooner than 6 months as previously suggested and as such, a decrease in the rupture risk of an aneurysm with a shorter waiting period. Such information can be reassuring for patients by decreasing the stress and anxiety associated with waiting for aneurysm occlusion.
CONCLUSION
Parent vessel reconstruction via flow diversion with the PED is a valid and safe treatment alternative for small ICA aneurysms. This endoluminal approach avoids endosaccular access and as such, theoretically reduces the intraprocedural aneurysm rupture risk associated with coiling. Compared with PED implantation for large and giant aneurysms, use in small ICA aneurysms may be achieved with a lower complication rate and earlier angiographic success. As our series continues to grow and additional follow-up data is available, we continue to provide further insight on PED applications for such aneurysms. Furthermore, earlier angiographic occlusion may allow for shortened duration of dual-antiplatelet regimens, although this would require further study.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2013/4/1/114/117711
Disclaimer: The authors of this article has no conflict of interest to disclose, and has adhered to SNI's policies regarding human/animal rights, and informed consent. Advertisers in SNI did not ask for, nor did they receive access to this article prior to publication
Contributor Information
Li-Mei Lin, Email: li.mei@jhmi.edu.
Geoffrey P. Colby, Email: gcolby1@jhmi.edu.
Jennifer E. Kim, Email: jenikim256@gmail.com.
Judy Huang, Email: Jhuang24@jhmi.edu.
Rafael J. Tamargo, Email: Rtamarg@jhmi.edu.
Alexander L. Coon, Email: acoon2@jhmi.edu.
REFERENCES
- 1.Akbari SH, Reynolds MR, Kadkhodayan Y, Cross DT, 3rd, Moran CJ. Hemorrhagic complications after prasugrel (Effient) therapy for vascular neurointerventional procedures. J Neurointerv Surg. 2013;5:337–43. doi: 10.1136/neurintsurg-2012-010334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brinjikji W, Lanzino G, Cloft HJ, Rabinstein A, Kallmes DF. Endovascular treatment of very small (3 mm or smaller) intracranial aneurysms: Report of a consecutive series and a meta-analysis. Stroke. 2010;41:116–21. doi: 10.1161/STROKEAHA.109.566356. [DOI] [PubMed] [Google Scholar]
- 3.Chan TT, Chan KY, Pang PK, Kwok JC. Pipeline embolisation device for wide-necked internal carotid artery aneurysms in a hospital in Hong Kong: Preliminary experience. Hong Kong Med J. 2011;17:398–404. [PubMed] [Google Scholar]
- 4.Cloft HJ, Kallmes DF. Cerebral aneurysm perforations complicating therapy with Guglielmi detachable coils: A meta-analysis. AJNR Am J Neuroradiol. 2002;23:1706–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Colby GP, Gomez JF, Lin LM, Paul AR, Coon AL. In situ removal of the pipeline embolization device: The ‘corking’ and ‘pseudo-corking’ techniques. J Neurointerv Surg. 2013;5:e6. doi: 10.1136/neurintsurg-2011-010234. [DOI] [PubMed] [Google Scholar]
- 6.Colby GP, Lin LM, Gomez JF, Paul AR, Huang J, Tamargo RJ, et al. Immediate procedural outcomes in 35 consecutive pipeline embolization cases: A single-center, single-user experience. J Neurointerv Surg. 2013;5:237–46. doi: 10.1136/neurintsurg-2012-010299. [DOI] [PubMed] [Google Scholar]
- 7.Colby GP, Lin LM, Huang J, Tamargo RJ, Coon AL. Utilization of the Navien distal intracranial catheter during 78 cases of anterior circulation aneurysm treatment with the pipeline embolization device. J Neurointerv Surg. 2013 doi: 10.1136/neurintsurg-2013-010692. [DOI] [PubMed] [Google Scholar]
- 8.De Barros Faria M, Castro RN, Lundquist J, Scrivano E, Ceratto R, Ferrario A, et al. The role of the pipeline embolization device for the treatment of dissecting intracranial aneurysms. AJNR Am J Neuroradiol. 2011;32:2192–5. doi: 10.3174/ajnr.A2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delgado Almandoz JE, Crandall BM, Scholz JM, Fease JL, Anderson RE, Kadkhodayan Y, et al. Pre-procedure P2Y12 reaction units value predicts perioperative thromboembolic and hemorrhagic complications in patients with cerebral aneurysms treated with the Pipeline Embolization Device. J Neurointerv Surg. 2013 doi: 10.1136/neurintsurg-2012-010582. [DOI] [PubMed] [Google Scholar]
- 10.Deutschmann HA, Wehrschuetz M, Augustin M, Niederkorn K, Klein GE. Long-term follow-up after treatment of intracranial aneurysms with the pipeline embolization device: Results from a single center. AJNR Am J Neuroradiol. 2012;33:481–6. doi: 10.3174/ajnr.A2790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fiorella D, Albuquerque F, Gonzalez F, McDougall CG, Nelson PK. Reconstruction of the right anterior circulation with the pipeline embolization device to achieve treatment of a progressively symptomatic, large carotid aneurysm. J Neurointerv Surg. 2010;2:31–7. doi: 10.1136/jnis.2009.000554. [DOI] [PubMed] [Google Scholar]
- 12.Fischer S, Vajda Z, Aguilar Perez M, Schmid E, Hopf N, Bäzner H, et al. Pipeline embolization device (PED) for neurovascular reconstruction: Initial experience in the treatment of 101 intracranial aneurysms and dissections. Neuroradiology. 2012;54:369–82. doi: 10.1007/s00234-011-0948-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joo SW, Lee SI, Noh SJ, Jeong YG, Kim MS, Jeong YT. What is the significance of a large number of ruptured aneurysms smaller than 7 mm in diameter? J Korean Neurosurg Soc. 2009;45:85–9. doi: 10.3340/jkns.2009.45.2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kassell NF, Torner JC. Size of intracranial aneurysms. Neurosurgery. 1983;12:291–7. doi: 10.1227/00006123-198303000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Leung GK, Tsang AC, Lui WM. Pipeline embolization device for intracranial aneurysm: A systematic review. Clin Neuroradiol. 2012;22:295–303. doi: 10.1007/s00062-012-0178-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Levy E, Koebbe CJ, Horowitz MB, Jungreis CA, Pride GL, Dutton K, et al. Rupture of intracranial aneurysms during endovascular coiling: Management and outcomes. Neurosurgery. 2001;49:807–11. doi: 10.1097/00006123-200110000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Lubicz B, Collignon L, Raphaeli G, De Witte O. Pipeline flow-diverter stent for endovascular treatment of intracranial aneurysms: Preliminary experience in 20 patients with 27 aneurysms. World Neurosurg. 2011;76:114–9. doi: 10.1016/j.wneu.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 18.Lylyk P, Miranda C, Ceratto R, Ferrario A, Scrivano E, Luna HR, et al. Curative endovascular reconstruction of cerebral aneurysms with the pipeline embolization device: The buenos aires experience. Neurosurgery. 2009;64:632. doi: 10.1227/01.NEU.0000339109.98070.65. [DOI] [PubMed] [Google Scholar]
- 19.McAuliffe W, Wycoco V, Rice H, Phatouros C, Singh TJ, Wenderoth J. Immediate and midterm results following treatment of unruptured intracranial aneurysms with the pipeline embolization device. AJNR Am J Neuroradiol. 2012;33:164–70. doi: 10.3174/ajnr.A2727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mitchell PJ, Muthusamy S, Dowling R, Yan B. Does small aneurysm size predict intraoperative rupture during coiling in ruptured and unruptured aneurysms? J Stroke Cerebrovasc Dis. 2012 doi: 10.1016/j.jstrokecerebrovasdis.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 21.Nelson PK, Lylyk P, Szikora I, Wetzel SG, Wanke I, Fiorella D. The pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol. 2011;32:34–40. doi: 10.3174/ajnr.A2421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nguyen TN, Raymond J, Guilbert F, Roy D, Berube MD, Mahmoud M, et al. Association of endovascular therapy of very small ruptured aneurysms with higher rates of procedure-related rupture. J Neurosurg. 2008;108:1088–92. doi: 10.3171/JNS/2008/108/6/1088. [DOI] [PubMed] [Google Scholar]
- 23.Phillips TJ, Wenderoth JD, Phatouros CC, Rice H, Singh TP, Devilliers L, et al. Safety of the pipeline embolization device in treatment of posterior circulation aneurysms. AJNR Am J Neuroradiol. 2012;33:1225–31. doi: 10.3174/ajnr.A3166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pierot L, Spelle L, Vitry F. Immediate clinical outcome of patients harboring unruptured intracranial aneurysms treated by endovascular approach: Results of the ATENA study. Stroke. 2008;39:2497–504. doi: 10.1161/STROKEAHA.107.512756. [DOI] [PubMed] [Google Scholar]
- 25.Raymond J, Guilbert F, Weill A, Georganos SA, Juravsky L, Lambert A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003;34:1398–403. doi: 10.1161/01.STR.0000073841.88563.E9. [DOI] [PubMed] [Google Scholar]
- 26.Roessler K, Cejna M, Zachenhofer I. Aneurysmatic subarachnoidal haemorrhage: Incidence and location of small ruptured cerebral aneurysms-A retrospective population-based study. Wien Klin Wochenschr. 2011;123:444–9. doi: 10.1007/s00508-011-1598-z. [DOI] [PubMed] [Google Scholar]
- 27.Saatci I, Yavuz K, Ozer C, Geyik S, Cekirge HS. Treatment of intracranial aneurysms using the pipeline flow-diverter embolization device: A single-center experience with long-term follow-up results. AJNR Am J Neuroradiol. 2012;33:1436–46. doi: 10.3174/ajnr.A3246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Serebruany VL, Malinin AI, Ferguson JJ, Vahabi J, Atar D, Hennekens CH. Bleeding risks of combination vs. single antiplatelet therapy: A meta-analysis of 18 randomized trials comprising 129,314 patients. Fundam Clin Pharmacol. 2008;22:315–21. doi: 10.1111/j.1472-8206.2008.00582.x. [DOI] [PubMed] [Google Scholar]
- 29.Sluzewski M, Bosch JA, van Rooij WJ, Nijssen PC, Wijnalda D. Rupture of intracranial aneurysms during treatment with Guglielmi detachable coils: Incidence, outcome, and risk factors. J Neurosurg. 2001;94:238–40. doi: 10.3171/jns.2001.94.2.0238. [DOI] [PubMed] [Google Scholar]
- 30.Szikora I, Berentei Z, Kulcsar Z, Marosfoi M, Vajda ZS, Lee W, et al. Treatment of intracranial aneurysms by functional reconstruction of the parent artery: The budapest experience with the pipeline embolization device. AJNR Am J Neuroradiol. 2010;31:1139–47. doi: 10.3174/ajnr.A2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.UCAS Japan Investigators. Morita A, Kirino T, Hashi K, Aoki N, Fukuhara S, et al. The natural course of unruptured cerebral aneurysms in a Japanese cohort. N Engl J Med. 2012;366:2474–82. doi: 10.1056/NEJMoa1113260. [DOI] [PubMed] [Google Scholar]
- 32.US Food and Drug Administration. Pipeline embolization device PMA P100018. Summary of safety and effectiveness data. 2011 [Google Scholar]
- 33.Vlak MH, Algra A, Brandenburg R, Rinkel GJ. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: A systematic review and meta-analysis. Lancet Neurol. 2011;10:626–36. doi: 10.1016/S1474-4422(11)70109-0. [DOI] [PubMed] [Google Scholar]
- 34.Weir B, Disney L, Karrison T. Sizes of ruptured and unruptured aneurysms in relation to their sites and the ages of patients. J Neurosurg. 2002;96:64–70. doi: 10.3171/jns.2002.96.1.0064. [DOI] [PubMed] [Google Scholar]
- 35.Wiebers DO, Whisnant JP, Huston J, 3rd, Meissner I, Brown RD, Jr, Piepgras DG, et al. Unruptured intracranial aneurysms: Natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003;362:103–10. doi: 10.1016/s0140-6736(03)13860-3. [DOI] [PubMed] [Google Scholar]
- 36.Yu SC, Kwok CK, Cheng PW, Chan KY, Lau SS, Lui WM, et al. Intracranial aneurysms: Midterm outcome of pipeline embolization device: A prospective study in 143 patients with 178 aneurysms. Radiology. 2012;265:893–901. doi: 10.1148/radiol.12120422. [DOI] [PubMed] [Google Scholar]


