Abstract
In January 2010, the American Joint Committee on Cancer (AJCC) updated its staging criteria for uveal melanoma. Here, we discuss the staging classifications and evaluate an interesting case to demonstrate. The development of a uniform means of staging cancer, such as defined by the AJCC, is critical for information sharing among the research community.
Keywords: American Joint Committee on Cancer, melanoma, prognosis, staging, uvea
Introduction
Uveal melanoma is the most common primary intraocular malignancy in adults, affecting an estimated six per million Caucasians annually in the United States.[1] Melanoma manifests as a unifocal, variably pigmented mass arising from melanocytes of the choroid, ciliary body, or iris. In advanced cases, melanoma can extend through the sclera and invade into the orbit.[1] Metastatic disease to the liver, lung, skin, and other organs remains a major threat associated with melanoma.[2]
Uveal melanoma is generally classified into size categories based on thickness of small (≤3 mm), medium (>3 –mm), or large (>8 mm) and prognosis is directly related to size.[3] In an analysis of 8033 eyes, Shields et al. studied Kaplan–Meier metastatic risk of uveal melanoma by tumor size categories small, medium, and large.[3] They found metastatic rates of 6%, 12%, and 20% for small tumors, 14%, 26%, and 37% for medium tumors, and 35%, 49%, and 67% for large tumors at 5, 10, and 20 years, respectively.[3]
The American Joint Committee on Cancer (AJCC) recently released the 7th edition of the AJCC cancer staging manual. This staging system has been designed for several cancers including cancer of the breast, colon, lung, head and neck, and both cutaneous and uveal melanoma. Herein, we present a case of posterior uveal melanoma and discuss the current AJCC staging criteria for posterior uveal melanoma.
Case Report
A 55-year-old White male noticed a pigmented spot on the iris left eye (OS). Examination revealed visual acuity of 20/20 in the right eye (OD) and 20/50 OS. Intraocular pressures were 18 mmHg OD and 15 mmHg OS. There was no ocular melanocytosis. The right eye was unremarkable.
The anterior segment OS revealed dilated episcleral sentinel vessels superotemporally leading to a brown iris tumor [Figure 1]. The tumor originated in the ciliary body with extension into the iris and with no extrascleral component. There was minor tumor seeding into the anterior chamber angle. The tumor measured 14 mm in diameter and 10.3 mm in thickness by ultrasonography. The final diagnosis was ciliochoroidal melanoma with secondary iris invasion and the tumor was classified according to the AJCC as a T3b N0 M0 with an anatomic stage IIIA and histologic grade GX. The patient was treated with an 18 mm custom-designed round I-125 radioactive plaque with an apex dose of 7000 cGy. Fine needle aspiration biopsy was performed at the time of plaque placement for cytogenetic testing.
Figure 1.
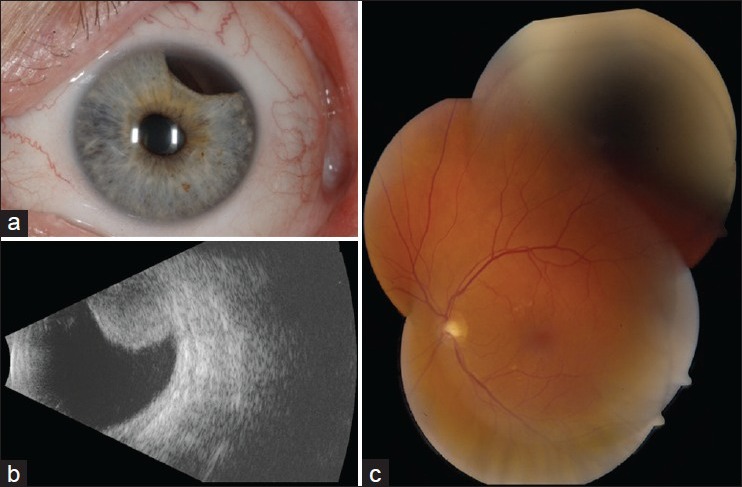
A 55-year-old White male with ciliary body melanoma with iris invasion classified as cTNM of stage T3b N0 M0 with an anatomic stage IIIA and histologic grade GX. (a) Ciliary body melanoma with iris extension. Sentinel vessels are noted superotemporally. (b) Ultrasonography depicting the intraocular melanoma measuring 10.3 mm in thickness and with moderate acoustic density. (c) Funduscopically, the ciliary body mass was located anterior to the equator and measure 14 mm basal dimension
Discussion
Prior to the AJCC classification, uveal melanoma prognosis was judged based on several factors including tumor basal dimension, thickness dimension, location within the uvea, extrascleral extension, and histopathologic factors of cell type, mitotic activity, nucleoli diameter, presence of necrosis, infiltrating lymphocytes, vascular loops, and others. More recently, genetic factors have been found to be highly predictive of uveal melanoma prognosis.[4] The AJCC is an attempt to unify these risk features into a single classification system. The large number of factors that contribute to ultimate prognosis of uveal melanoma underscores the importance of a standardized means for classification.
Cancer staging is a means of classification of the extent of disease using clinical, pathologic, and genetic criteria. The creation of a universal standard by the AJCC was initially published as the 1st edition in 1977, and, since then, the AJCC has been revised on a 6-8 year basis. In January 2010, the 7th edition of the AJCC Cancer Staging Manual was published. The AJCC Staging is especially helpful for assessment of rare cancers, like uveal melanoma, allowing collaboration of centers of excellence to be performed using a single classification.[5,6] Furthermore, staging allows evaluation of outcomes following various protocol therapies.[4]
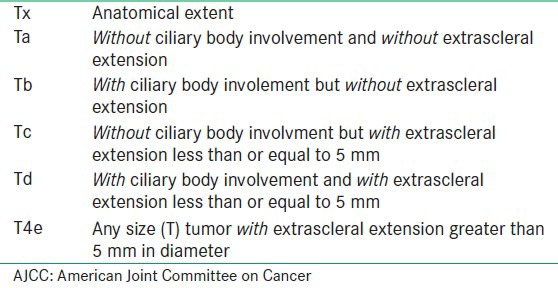
The most recent edition of the AJCC staging manual uses the tumor, node, and metastasis (TNM) model for anatomical staging. In this system, the extent of the primary tumor (T), presence or absence of lymph node involvement (N), and presence or absence of distant metastasis (M) provides information on disease spread. For posterior uveal melanoma, T is categorized based on tumor basal dimension and thickness into four increasing size classes, including T1, T2, T3, T4 [Table 1]. Secondarily, T is classified according to specific anatomic extent regarding ciliary body involvement and extrascleral extension using categories a through e[5] [Table 2]. The regional lymph nodes are assessed by NX (cannot be assessed), N0 (lymph node metastasis absent), and N1 (lymph node metastasis present). Similarly, distant metastases are assessed according to MX (cannot be assessed), M0 (distant metastasis absent), and M1 (distant metastasis present). When present, M1 is further divided into M1a for metastasis ≤3 cm, M1b for those 3.1-8.0 cm, and M1c for those ≥8 cm.
Table 1.
AJCC tumor (T) classification of uveal melanoma (primary choroidal and ciliary body melanoma) defined by basal diameter and tumor thickness[5]
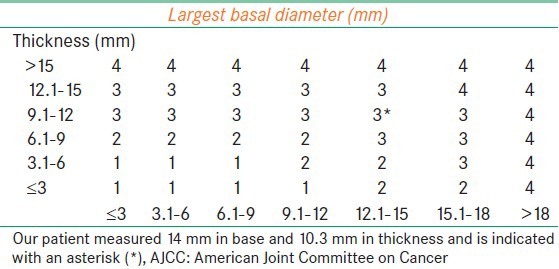
Table 2.
AJCC tumor (T) sub-classifications defined by anatomical extent of the tumor based on ciliary body and/or extrascleral involvement
A further refinement in the AJCC classification of uveal melanoma is the grouping of the individual T, N, and M into Anatomic Staging (Stage I-IV) [Table 3]. The stages are considered increasingly higher risk for metastasis from Group I to IIA, IIB, IIIA, IIIB, IIIC, and to IV. This staging has yet to be tested with long-term prognostic results. In addition to the above clinical information, identified as cTNM, the AJCC accounts for pathologic information, pTNM, in a similar fashion. The histologic grade is recorded as GX (cannot be assessed), G1 (spindle cell), G2 (mixed cell), and G3 (epithelioid cell).[5]
Table 3.
AJCC anatomic stage of uveal melanoma defined by tumor, node, and metastasis values[5]
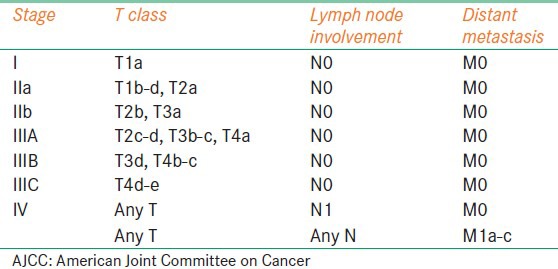
Our patient with tumor dimensions of 14 mm diameter and 10.3 mm base was found to have a cTNM of stage T3b N0 M0 with an anatomic stage IIIA and histologic grade GX. Plaque radiotherapy was the chosen method of treatment over enucleation, as even tumors >8 mm thickness, as in this case, most plaque-irradiated eyes are retained and 43% have visual acuity better than 20/100.[7] Fine needle aspiration biopsy was performed at the time of plaque placement and sent for cytogenetic analysis. We perform cytogenetic analysis of all uveal melanomas to better understand patient prognosis. Eyes with monosomy 3 or abnormalities of chromosome 8 within the melanoma demonstrate poorer prognosis and necessitate more intense systemic follow-up.[8] In this case, results revealed monosomy 3 and amplification of 8q, conferring a negative prognosis.[8] All patients, especially those with high risk for systemic metastasis, are encouraged to have evaluation by a medical oncologist and proceed with liver function tests every 3-6 months, magnetic resonance imaging (MRI) of the abdomen every 3-6 months, and chest radiograph every 6 months. Our patient is being followed conservatively and currently has no signs of systemic metastases.
There have been few publications on uveal melanoma employing the AJCC classification. Khan et al. evaluated 131 patients with iris melanoma using the AJCC classification of iris melanoma to pool international data from eight cancer centers in six countries for clinical and pathological characteristics of iris melanoma at each stage.[9] The study revealed the prevalence of T1, T2, T3, and T4 iris tumors to be 56%, 34%, 2%, and 1%, respectively.[9] Clinically they found that most tumors presented with brown pigmentation and in the inferior quadrants of the iris.[9] Similarly, Shields et al. used the AJCC tumor classification for prognostication of 343 patients with conjunctival melanoma.[10] For T1, T2, and T3 class tumors, they found recurrence or new tumor rates of 44%, 78%, and 76%, lymph node metastasis rates of 17%, 52%, and 49%, and distant metastasis rates of 11%, 35%, and 42%. They commented that patients with T1 conjunctival melanoma showed substantially better prognosis than those with T2 or T3.[10] A similar study of the clinical features and prognosis of uveal melanoma by AJCC classification has yet to be completed, but could offer patients and physicians valuable insight into the prognosis of the various degrees of uveal melanoma.
In summary, the AJCC classification and staging of uveal melanoma is somewhat complex but could provide improved understanding of this highly fatal malignancy. We encourage all ocular oncologists to collaborate with this classification to provide a more unified method of predicting outcomes.
Footnotes
Source of Support: Support provided in part by the Lift for a Cure, Morrisdale, PA (CLS) and the Eye Tumor Research Foundation, Philadelphia, PA (CLS).
Conflict of Interest: None declared.
References
- 1.Shields JA, Shields CL. Philadelphia: Lippincott Williams Wilkins; 2008. Atlas of Intraocular Tumors; pp. 85–176. [Google Scholar]
- 2.Edge SB, Byrd DR, Comptom CC, editors. 7th ed. New York, NY: Springer; 2010. AJCC Cancer Staging Manual. [Google Scholar]
- 3.Shields CL, Furuta M, Thangappan A, Nagori S, Mashayekhi A, Lally DR, et al. Metastasis of uveal melanoma millimeter-by millimeter in 8033 consecutive eyes. Arch Opthalmol. 2009;127:989–98. doi: 10.1001/archophthalmol.2009.208. [DOI] [PubMed] [Google Scholar]
- 4.Shields CL, Ganguly A, O’Brien J, Sato T, Shields JA. Uveal melanoma trapped in the Temple of Doom. Editorial Am J Ophthalmol. 2012;154:219–21. doi: 10.1016/j.ajo.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 5.Edge SB, Byrd DR, Compton CC, editors. AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer; 2010. Purposes and Principles of Cancer Staging; pp. 3–14. [Google Scholar]
- 6.Edge SB, Byrd DR, Compton CC, editors. AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer; 2010. Malignant Melanoma of the Uvea; pp. 547–60. [Google Scholar]
- 7.Shields CL, Naseripour M, Cater J, Shields JA, Demirci H, Youseff A, et al. Plaque radiotherapy for large Posterior Uveal Melanomas (>8mm-Thick) in 354 Consecutive Patients. Ophthalmology. 2002;109:1838–49. doi: 10.1016/s0161-6420(02)01181-8. [DOI] [PubMed] [Google Scholar]
- 8.Damato B, Duke C, Coupland SE, Hiscott P, Smith PA, Campbell I, et al. Cytogenetics of Uveal Melanoma: A 7-year clinical experience. Ophthalmology. 2007;114:1925–31. doi: 10.1016/j.ophtha.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 9.Khan S, Finger PT, Yu GP, Razzaq L, Jager MJ, de Keizer RJ, et al. Clinical and pathological characteristics of biopsy-proven Iris Melanoma. Arch Opthalmol. 2012;130:57–67. doi: 10.1001/archophthalmol.2011.286. [DOI] [PubMed] [Google Scholar]
- 10.Shields CL, Kaliki S, Al-Dahmesh SA, Lally SE, Shields JA. American Joint Committee on Cancer (AJCC) clinical classification predicts conjunctival melanoma outcomes. Ophthal Plast Reconstr Surg. 2012;28:313–23. doi: 10.1097/IOP.0b013e3182611670. [DOI] [PubMed] [Google Scholar]


