Abstract
Chemical burns represent potentially blinding ocular injuries and constitute a true ocular emergency requiring immediate assessment and initiation of treatment. The majority of victims are young and exposure occurs at home, work place and in association with criminal assaults. Alkali injuries occur more frequently than acid injuries. Chemical injuries of the eye produce extensive damage to the ocular surface epithelium, cornea, anterior segment and limbal stem cells resulting in permanent unilateral or bilateral visual impairment. Emergency management if appropriate may be single most important factor in determining visual outcome. This article reviews the emergency management and newer techniques to improve the prognosis of patients with chemical injuries.
Keywords: Acid, alkali, chemical burns, eye, injury, ocular, treatment
Introduction
Ocular chemical injuries are a true ocular emergency and require immediate and intensive evaluation and treatment. The sequelae of an ocular burn can be severe and particularly challenging to manage. Improvements in the understanding of the pathophysiology of chemical injuries, as well as advancements in ocular surface reconstruction have provided hope for patients who would otherwise have a dismal visual prognosis. After chemical injury, the goal of therapy is to restore a normal ocular surface and corneal clarity. If extensive corneal scarring is present, limbal stem cell grafting, amniotic membrane transplantation and possibly keratoprosthesis can be employed to help restore vision. This article will review the literature available and discuss newer techniques available to improve the prognosis of patients with chemical injuries.
Epidemiology
Ocular chemical injuries can occur under diverse circumstances and in such varied locations as the home, the workplace, and school [Table 1]. These injuries are common in industrial chemical laboratories, in machine factories, in agriculture, and among laborers and construction workers. They also are frequently reported from fabric mills, automotive repair facilities, and cleaning and sanitizing crews. Chemical burns of the eyes occur most often among the age group from 20 to 40 years, with young men at greatest risk. In a retrospective study on the incidence and prevalence of ocular chemical burns, 171 consecutive patients were studied during an interval of 1 year. Industrial accidents caused 61% of these burns; 37% occurred in the home. The remainder were of unknown origin.[1] Automotive battery acid burns have become increasingly more common. During recharging of a lead acid storage battery, which contains up to 25% sulfuric acid, hydrogen and oxygen produced by electrolysis form a highly explosive gaseous mixture.[2]
Table 1.
Etiological factors commonly encountered in ocular chemical injuries
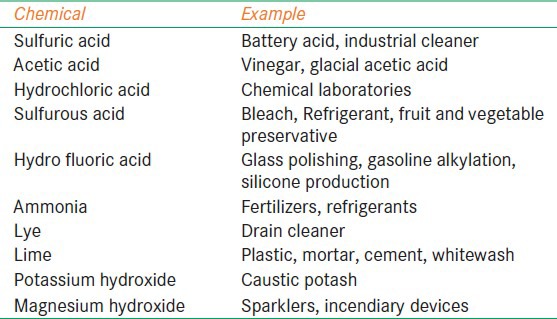
Etiological Factors (Commonly Encountered)
Recent studies put the incidence of ocular burns of the eye at 7.7-18% of all ocular traumas. The majorly of victims are young and exposure occurs at home, work and in association with criminal assaults. Alkali injuries occur more frequently than acidic injuries.
Pathogenesis
Acid burns
Acids have lower than normal pH values of the human eye (7.4) they precipitate tissue protein, creating a barrier to further ocular penetration. Due to this fact acid injuries tend to be less severe than alkali injuries. One exception to this is hydrofluoric acid, which may rapidly pass through cell membranes and enter anterior chamber of the eye.
It reacts with collagen resulting in shortening of collagen fibers which cause a rapid increase in intraocular pressure (IOP). After severe acid burns with ciliary body damage, decrease in levels of aqueous ascorbate has been demonstrated.
Alkali burns
Alkali burns cause corneal damage by pH change, ulceration, proteolyzes and collagen synthesis defects. Alkali substances are liphophilic and penetrate the eye more rapidly than acids. The basic substance can quickly deposit within the tissues of the ocular surface causing saponification reaction within those cells. The damaged tissue secrete proteolytic enzymes as part of an inflammatory response which leads to further damage. Alkali substances can penetrate into the anterior chamber causing cataract formation, damage to the ciliary body and damage to the trabecular meshwork.
The damage to the corneal and conjunctival epithelium from an ocular burn may be so severe as to damage the pluripotent limbal stem cell causing a limbal stem cell deficiency. This may lead to opacification and neo-vascularization of the cornea. An acute IOP rise occurrence due to shrinkage and contraction of the cornea and sclera is possible.[3] Long-term IOP rises can occur from the accumulation of inflammatory debris within the trabecular meshwork, as well as due to damage to the trabecular meshwork itself. Damage to the conjunctiva can cause extensive scarring, perilimbal ischemia, and contracture of fornices. Loss of goblet cells and conjunctival inflammation can leave the ocular surface prone to dryness. Lid malposition may be present due to symblepharon formation leading to cicatricial entropion or ectropion.
Classification
Classification schemes regarding the extent of the initial injury were initially developed in the mid 1960's first by Ballen[4] and then modified by Roper-Hall.[5] The Roper-Hall classification system was largely based on the degree of corneal haze and the amount of perilimbal blanching/ischemia [Table 2].
Table 2.
Roper-Hall (Ballen) classification of ocular chemical injuries
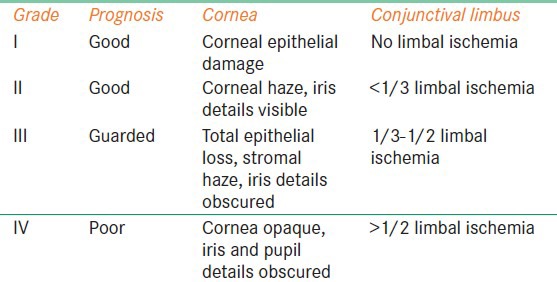
Pfister subsequently made a classification system varying from mild, mild-moderate, moderate severe, severe and very severe based upon pictures and photographs demonstrating corneal haze and perilimbal ischemia.[6]
Dua et al. proposed a classification scheme based upon clock hour limbal involvement as well as a percentage of bulbar conjunctival involvement [Table 3].[7]
Table 3.
New classification of ocular surface burn
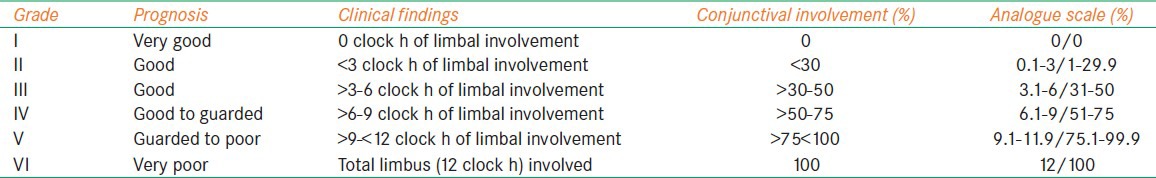
The important thing in the clinical setting is to note the amount of limbal, corneal and conjunctival involvement at the time of the initial injury and to document changes in the examination as the patient is followed. Grading of the severity may provide the patient with a general idea of the prognosis.
Clinical Course of Chemical Ocular Injury
According to McCulley the clinical course of ocular chemical injury can be divided into the following four phases: Immediate, acute, early reparative, and late reparative.[8]
Immediate phase
The immediate phase begins the moment a chemical agent comes in contact with the ocular surface. The key elements for determining the extent of chemical ocular injury and prognosis are:
The total area of the corneal epithelial defect
The area of the conjunctival epithelial defect
The number of clock hours or degrees of limbal blanching
The area and density of corneal opacification
Evidence of increase IOP on presentation
Loss of lens clarity.
Acute phase
The first 7 days after chemical eye injury constitute the acute phase of recovery. During this time, the tissues rid themselves of contaminants while re-establishing the superficial protective layer of corneal epithelium.
The epithelium serves as a protective barrier against the enzymes in tears that lead to corneal thinning and progression to perforation. It also modulates stromal regeneration and repair. Significant inflammatory mechanisms begin to evolve on the ocular surface and inside the eye. In this stage, there is the rise in IOP in a bimodal manner.[3]
Early reparative phase (8-20 days)
This is the transition period of ocular healing, in which the immediate regeneration of ocular surface epithelium and acute inflammatory events give way to chronic inflammation, stromal repair and scarring. It is during this stage, corneal ulceration tends to occur. Stromal ulceration thus resulting has been attributed to action of digestive enzymes such as collagenase, metalloproteinase and other proteases released from regenerating corneal epithelium and polymorphonuclear leukocytes.
Late reparative phase and sequelae
Three weeks after a chemical injury occurs the healing process begins late reparative phase. This stage is characterized by completion of healing with good visual prognosis (Grade I and II) and complications in those with guarded visual prognosis (Grade III and IV). The late complications of chemical burns include poor vision, corneal scarring, xerophthalmia, dry eyes, symblepharon, ankyloblepharon glaucoma, uveitis, cataract, adenexal abnormalities such as lagophthalmos, entropion, ectropion and trichiasis.
Management of Chemical Burns
Immediate initiation of treatment influences the final outcome favorably and one should not wait for careful assessment of the injury.
Initial evaluation and immediate treatment
Patients suffering from a chemical injury often present to the emergency. Once history of chemical exposure is obtained chemical should be identified if possible, but this should but delay treatment. Immediate treatment should include copious irrigation prior to ophthalmic evaluation irrigation with isotonic saline or lactate ringer solution should be performed and sometimes irrigating volumes up to 20 L or more is required to change pH to physiological levels (pH testing should be done). Once copious irrigation is achieved and pH is neutralized, the ocular examination should proceed with attention is being paid to fornices, visual acuity, IOP, perilimbal blanching. In pediatric cases, if the examination is not possible under topical anesthesia it should be done under general anesthesia.
Acute phase treatment
Once the emergency treatment and evaluation are completed, the challenging task of healing the chemically injured eye begins. The major treatment goals that are important throughout the healing phases are: (a) reestablishment and maintenance of an intact and healthy corneal epithelium (b) control of the balance between collagen synthesis and collagenolysis and (c) minimizing the adverse sequelae that often follow a chemical injury. Acute phase treatment includes a broad spectrum topical antibiotic, cycloplegic and antiglaucoma therapy. Apart from above mentioned medications various therapies to promote reepithelization, support repair and control inflammation are used.
Modalities to promote reepithelization are:
Tear substitutes: Preservative free tear substitutes can ameliorate persistent epitheliopathy, reduce the risk of recurrent erosions and accelerate visual rehabilitation
Bandage soft contact lens: Hydrophilic high oxygen permeability lenses should be preferred. They promote epithelial migration, helps in the basement membrane regeneration and enhances epithelial stromal adhesion
-
Investigational drugs:
- Retinoic acid - Has shown promise in treatment of ocular surface disorders associated with goblet cell dysfunction
- Epidermal growth factor and fibronectin - Has a favorable effect on promoting epitheliazation.
Drugs that support repair and minimizing ulceration
Ascorbate: Ascorbate is an essential water soluble vitamin that is a cofactor in rate limiting step of collagen formation. Supplementation of ascorbate by restoring depleted aqueous ascorbate levels reduces the incidence of corneal thinning and ulceration. Oral ascorbate (2 g/day) and topical 10% solution formulated in artificial tears are effective
Collagenase inhibitors: Collagenase inhibitors promote wound healing by inhibiting collagenolytic activity and thus preventing stromal ulceration. Several collagenase inhibitors including cysteine, acetylcysteine, sodium ethylenediamine tetra acetic acid (EDTA), calcium EDTA, penicillamine and citrate have been reported to be efficacious. Only 10-20% acetylcysteine (mucomist) is available commercially. It is an unstable solution and has to be refrigerated and used within 1 week of its preparation.
Drugs to control inflammation
Corticosteroids reduce inflammatory cell infiltration and stabilize neutrophilic cytoplasmic and lysosomal membranes. Use of topical steroids alone can potentially lead to a further increase in corneoscleral melt.[9] Davis et al. evaluated patients with topical prednisolone 0.5% in conjunction with topical ascorbate 10% and concluded that there was not an associated increase in corneoscleral melt if topical steroids were used until reepithelization.[10]
Early reparative phase treatment
An intact epithelium should have already been achieved by this time. If it has not been, then aggressive therapy is instituted by use of lubricants, punctual plugs, punctual occlusion with cautery, bandage contact lens, tarsorrhaphy. If epithelium is not intact, corticosteroids dosage is tapered and discontinued by 14th day after injury. Ascorbate and citrate are continued, antiglaucoma therapy is continued as required. Antibiotics are maintained and examination for the formation of symblepharon continued.
Late reparative phase treatment
The patient whose injured eye has not achieved an intact epithelium by the 21st day is at significant risk of permanent vision loss. Along with continued medical treatment, surgical modalities are the mainstay of treatment in this state of ocular burn. The various strategies include conjunctival/tenons advancement, tissue adhesives, therapeutic penetrating keratoplasty, amniotic membrane transplantation.
Rehabilitative phase
After the eye has stabilized, limbal stem cell transplantation has shown remarkable promise in rehabilitating ocular chemical injuries that have resisted treatment. Limbal stem cell can be donated from the patient uninjured fellow eye, a blood relative or a post mortem globe. All have shown promise in reestablishing a healthy ocular surface prior to further reconstructive surgery. Once a healthy surface is achieved, penetrating keratoplasty or keratoprosthesis may be considered.[11]
Conclusion
Patient coming with chemical ocular injury need a through and immediate evaluation and intensive treatment. Advances in understanding of the pathophysiology of the injury have led to improvement in treatment such as use of topical ascorbate and citrate, as well as surgical treatment such as Amniotic membrane transplantation, stem cell transplantation, penetrating keratoplasty and ultimately keratoprosthesis placement if necessary. The goal of treatment is restoration of the normal ocular surface anatomy and lid position, control of glaucoma and restoration of corneal clarity.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kuckelkorn R, Makropoulos W, Kottek A, Reim M. Retrospective study of severe alkali burns of the eyes. Klin Monbl Augenheilkd. 1993;203:397–402. doi: 10.1055/s-2008-1045695. [DOI] [PubMed] [Google Scholar]
- 2.Holekamp TL. Ocular injuries from automobile batteries. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1977;83:805–10. [PubMed] [Google Scholar]
- 3.Paterson CA, Pfister RR. Intraocular pressure changes after alkali burns. Arch Ophthalmol. 1974;91:211–8. doi: 10.1001/archopht.1974.03900060219014. [DOI] [PubMed] [Google Scholar]
- 4.Ballen PH. Treatment of chemical burns of the eye. Eye Ear Nose Throat Mon. 1964;43:57–61. [PubMed] [Google Scholar]
- 5.Roper-Hall MJ. Thermal and chemical burns. Trans Ophthalmol Soc U K. 1965;85:631–53. [PubMed] [Google Scholar]
- 6.Pfister RR. Chemical injuries of the eye. Ophthalmology. 1983;90:1246–53. [PubMed] [Google Scholar]
- 7.Dua HS, King AJ, Joseph A. A new classification of ocular surface burns. Br J Ophthalmol. 2001;85:1379–83. doi: 10.1136/bjo.85.11.1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCulley JP. Chemical injuries. In: Smolin G, Thoft RA, editors. The Cornea: Scientific Foundation and Clinical Practice. Boston Mass: Little Brown and Co; 1987. pp. 527–42. [Google Scholar]
- 9.Donshik PC, Berman MB, Dohlman CH, Gage J, Rose J. Effect of topical corticosteroids on ulceration in alkali-burned corneas. Arch Ophthalmol. 1978;96:2117–20. doi: 10.1001/archopht.1978.03910060497024. [DOI] [PubMed] [Google Scholar]
- 10.Davis AR, Ali QK, Aclimandos WA, Hunter PA. Topical steroid use in the treatment of ocular alkali burns. Br J Ophthalmol. 1997;81:732–4. doi: 10.1136/bjo.81.9.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dohlman CH, Schneider HA, Doane MG. Prosthokeratoplasty. Am J Ophthalmol. 1974;77:694–70. doi: 10.1016/0002-9394(74)90534-0. [DOI] [PubMed] [Google Scholar]


