Abstract
Background/Aims
Previous studies point to an association between childhood sexual abuse (CSA) and auditory hallucinations (AH). However, methodological issues limit the strength of these results. Here we compared childhood abuse between psychotic disorder patients and healthy control subjects using a reliable measure of abuse, and assessed the relationship between CSA and AH.
Methods
114 psychotic disorder patients and 81 healthy control subjects were administered the Structured Clinical Interview of the DSM-IV (SCID) and the Childhood Trauma Questionnaire (CTQ). We compared the severity of abuse between groups, and tested the relationship between different types of childhood abuse and specific psychotic symptoms.
Results
Psychotic patients reported more childhood abuse than controls (p<.001). Psychotic patients with a history of AH reported significantly more sexual, emotional, and physical abuse than patients without a history of AH (p<.05). Emotional and physical abuse, in the absence of sexual abuse, did not lead to a higher rate of AH. Finally, reports of childhood abuse did not increase the risk of any form of hallucination other than AH or of any form of delusion.
Conclusions
These results suggest that childhood abuse, especially childhood sexual abuse, shapes the phenotype of psychotic disorders by conferring a specific risk for AH.
Keywords: Childhood abuse, trauma, risk factors, auditory hallucinations, psychotic disorders, schizophrenia, psychosis
Introduction
It is well established that individuals with mental illness report a higher prevalence of childhood trauma than those without, suggesting that the experience of trauma during childhood can increase the risk of developing a psychiatric disorder (1). To understand the nature of this relationship, recent studies have examined the association between childhood trauma and specific symptoms of mental illness, such as psychosis, and many have reported a significant link (2–6). One of the most consistent findings across multiple studies is the greater risk for hallucinations after childhood abuse (7–9), with some studies pointing to childhood sexual abuse as a specific risk factor for the experience of auditory hallucinations (10–12).
However, two recent review articles have questioned the reliability and implications of these studies (13, 14). One limitation is the lack of a quantitative measure of childhood abuse which systematically assesses multiple domains of trauma (sexual, physical, emotional). For example, some studies have determined rates of abuse through review of the medical records of psychiatric patients (12, 15) while others have used surveys with a small array of general lifetime trauma questions (4, 5, 7, 9), leading to reports of childhood abuse that may not be assessed in a standardized way. On the other hand, many studies reporting a relationship between childhood sexual abuse and psychosis have focused solely on past sexual abuse, not assessing for any co-occurring physical or emotional abuse, leaving out possible confounding factors (3, 11, 16). A final problem has been the lack of a control group for comparison of baseline rates of abuse. In their review, Bendall and colleagues argue that establishing a higher prevalence of childhood trauma in psychotic patients, as compared to a healthy control group, is a critical first step in finding an association between trauma and psychosis (13). They state that using the same methods across subjects, researchers must first find higher rates of childhood trauma in individuals with psychosis than healthy controls, in order to make a reasonable argument that trauma is a risk factor for psychosis.
In the time since these reviews were published, more methodologically rigorous studies have worked to address these shortcomings and establish a stronger relationship between abuse and psychosis. Two studies found a dose-response relationship between the experience of trauma and risk for psychotic experiences (17, 18), comparing psychotic experiences prospectively (18) and comparing psychosis patients with siblings and healthy controls (17). In addition, a recent study found a specific relationship between childhood sexual abuse and transition to psychosis within an ultra-high risk group, with an estimated 2–4 times greater risk of transition to psychosis in individuals with high sexual abuse scores compared to those with low sexual abuse (19).
In the current study we add to this growing literature by addressing several of the previous limitations. Our experimental sample includes a large group of well-characterized patients with a psychotic disorder and demographically-similar control participants. In addition, all subjects received the CTQ, a valid and reliable measure of childhood abuse (20–22) that assesses five different kinds of abuse on a continuous scale, allowing us to test the relationship between each abuse type and different psychotic symptoms. Here we test the hypotheses that severity of childhood abuse is greater in psychotic disorder patients compared to healthy controls and that childhood sexual abuse increases the risk of experiencing auditory hallucinations in psychotic disorder patients.
Materials and Methods
Subjects
Participants included 114 psychotic disorder patients (53 with schizophrenia, 28 with schizoaffective disorder, and 33 with bipolar disorder, type 1, with psychotic features) and 81 healthy controls. All participants completed written informed consent after approval of the study protocol by the Vanderbilt University Institutional Review Board, Nashville, Tennessee. Psychotic patients were recruited from the inpatient unit and outpatient clinic of the Vanderbilt Psychiatric Hospital, and healthy controls were recruited via advertisements within the community. All participants were administered the Structured Clinical Interview for the DSM-IV-TR (SCID), which was later reviewed by an experienced psychiatrist and, if available, was supplemented with clinical information obtained from the treating physician. Participants were excluded if they had any significant medical or neurological disease, significant head injury or a history of drug dependence. Of the 114 psychotic disorder patients, 37 reported a co-morbid anxiety disorder (for breakdown by diagnosis, see Table 1). Control participants with a history of psychiatric illness or treatment with psychotropic medication were also excluded. The patient and control groups did not differ on gender, race or parental education (Table 2).
Table 1.
Co-morbid anxiety disorder diagnoses for psychotic disorder patients broken down by primary diagnosis
| Diagnosis | Panic Disorder | Social Phobia | Specific Phobia | OCD | PTSD | GAD | Anxiety NOS | Total Patients with co-morbid Anxiety Disorder(s) |
|---|---|---|---|---|---|---|---|---|
| Schizophrenia (n=53) | 3 | 2 | 0 | 2 | 1 | 2 | 1 | 11 |
| Schizoaffective (n=28) | 3 | 0 | 0 | 3 | 10 | 0 | 0 | 16 |
| Bipolar w/ PF(n=33) | 5 | 1 | 1 | 2 | 5 | 1 | 0 | 10 |
Table 2.
Demographic and Clinical Characteristics of Participantsa
| Control n = 81 |
Psychotic Disorder n = 114 |
|
|---|---|---|
| Sex (male/female) | 41/40 | 58/56 |
| Race (White/Black/Other) | 53/25/3 | 69/38/7 |
| Age | 34.0 (11.81) | 37.3 (12.59) |
| Participant’s Education, Yearsb | 15.3 (2.46) | 12.9 (2.31) |
| Parental Education, Years | 13.3 (2.23) | 13.3 (3.35) |
| Pre-morbid IQ, WTARb | 108.6 (13.61) | 95.6 (17.41) |
| GAF | - | 42.4 (14.90) |
| HAM-D | - | 13.9 (10.70) |
| YMRS | - | 8.4 (8.21) |
| PANSS | - | 63.7 (20.02) |
| Duration of Illness, Years | - | 18.3 (13.60) |
GAF, Global Assessment of Functioning; HAM-D, Hamilton Depression Rating Scale; PANSS, Positive and Negative Syndrome Scale; WTAR, Wechsler Test of Adult Reading; YMRS, Young Mania Rating Scale
Mean (SD) unless indicated otherwise
Significantly different between Controls and Psychotic Disorder groups, p<.001
Measures
Trauma history was assessed with the short-version of the CTQ (23), a self-report questionnaire that measures the experience and severity of five different types of childhood trauma: physical abuse, sexual abuse, emotional abuse, emotional neglect, and physical neglect (24). Each category of abuse is assessed with five statements (e.g. someone tried to make me do sexual things or watch sexual things) for which participants select a level of frequency: never true, rarely true, sometimes true, often true, or very often true. These responses are then coded on a 5-point Likert scale. Total CTQ scores range from 25–125, with each individual abuse subscale ranging from 5–25 and higher scores indicating more severe abuse. The validity and reliability of the CTQ have been verified by independent studies (20–22). Additionally, the CTQ has been used in previous studies as an assessment of childhood trauma amongst psychotic disorder patients (6, 17, 19) and prior research has demonstrated the validity of self-report measures in individuals with serious mental illness (25–27) and of reports of abuse in patients with psychosis (28, 29).
To explore the relationship between childhood trauma and specific positive symptoms, patients were classified into groups of individuals who had or had never experienced a particular symptom during their lifetime, based on data from the SCID interview. Participants were assessed for 5 types of hallucinations (auditory, visual, tactile, gustatory, olfactory) and 8 types of delusions (reference, persecutory, grandiose, somatic, other, control, thought broadcasting, and bizarre). Demographic differences between patients who had and had never experienced auditory hallucinations can be found in Table 3.
Table 3.
Demographics and Clinical Characteristics of psychotic disorder patients split by those with and without auditory hallucinationsa
| Patients without Auditory Hallucinations n = 27 |
Patients with Auditory Hallucinations n = 87 |
|
|---|---|---|
| Sex (male/female) | (17/10) | (44/43) |
| Race (White/Black/Other) | (19/7/1) | (50/31/6) |
| Age | 35.5 (14.10) | 37.9 (12.10) |
| Participant’s Education, Years | 13.8 (2.58) | 12.7 (2.18) |
| Parental Education, Yearsb | 14.9 (3.80) | 12.7 (3.01) |
| Pre-morbid IQ, WTAR | 98.7 (16.83) | 94.6 (17.57) |
| GAF | 44.1 (17.89) | 42.3 (14.12) |
| HAM-Db | 8.7 (8.45) | 15.3 (10.51) |
| YMRS | 5.9 (7.61) | 9.1 (8.22) |
| PANSS | 61.1 (17.03) | 64.3 (20.45) |
| PTSD co-morbidity | n = 2 | n = 14 |
| Duration of Illness, Years | 15.7 (13.77) | 18.6 (13.42) |
GAF, Global Assessment of Functioning; HAM-D, Hamilton Depression Rating Scale; PANSS, Positive and Negative Syndrome Scale; PTSD, Post-traumatic Stress Disorder; WTAR, Wechsler Test of Adult Reading; YMRS, Young Mania Rating Scale
Mean (SD) unless indicated otherwise
Significantly different between patients with and without auditory hallucinations, p<.05
Analyses
To compare the severity of overall childhood abuse and the five different types of abuse between psychotic patients and control participants, we used a Multivariate Analysis of Variance (MANOVA). Next, we assessed the relationship between childhood abuse and auditory hallucinations in our patient group by comparing scores on the childhood abuse subscales between psychotic patients who had or had not experienced auditory hallucinations, using a MANOVA, controlling for scores on the Hamilton Depression Scale (HAM-D (30)). Based on our a priori hypothesis for a specific relationship between sexual abuse and auditory hallucinations, we used a one-way ANOVA to assess the relationship between childhood sexual abuse and auditory hallucinations, and an ANCOVA to confirm the pattern of results while controlling depressive symptoms. To test the specificity of the relationship between childhood abuse and experience of auditory hallucinations, we used MANOVAs to compare childhood abuse scores between psychotic patients who had or had not experienced 1) each of the 4 other types of hallucinations and 2) each of the 8 types of delusions. Post-hoc analyses were only performed for MANOVAs with an overall significant model. Finally, we performed a logistic regression and post-hoc sub-sample analysis to better understand the relationship between auditory hallucinations and different types of abuse.
Results
Consistent with previous studies, patients with a psychotic disorder reported significantly more overall childhood abuse than healthy control subjects (CTQ Total: F(1, 193) = 70.10, p < .001). A similar pattern was observed for each of the five sub-scales of childhood abuse (physical abuse: F(1, 193) = 30.13, p < .001; sexual abuse: F(1,193) = 39.34, p < .001; emotional abuse: F(1, 193) = 69.75, p < .001; emotional neglect: F(1, 193) = 44.08, p < .001; physical neglect: F(1, 193) = 34.09, p < .001) (for means, see Table 4).
Table 4.
Average Childhood Trauma Questionnaire Scores for Patients and Controlsa
| Healthy Controls n = 81 |
Psychosis Patients n = 114 |
Group Comparison df = 193 |
|
|---|---|---|---|
| CTQ Total | 33.0 (9.8) | 54.1 (21.1) | t = 8.4, p <.001 |
| Physical Abuse | 6.8 (2.5) | 10.3 (5.4) | t = 5.5, p <.001 |
| Sexual Abuse | 5.3 (1.8) | 9.8 (6.3) | t = 6.3, p <.001 |
| Emotional Abuse | 6.7 (2.8) | 12.4 (5.7) | t = 8.4, p <.001 |
| Emotional Neglect | 8.2 (3.7) | 12.7 (5.3) | t = 6.6, p <.001 |
| Physical Neglect | 6.1 (1.8) | 8.8 (3.9) | t = 5.8, p <.001 |
df, degrees of freedom; CTQ, Childhood Trauma Questionnaire
Mean (SD)
Because the psychotic disorders group included patients with different diagnoses (schizophrenia, schizoaffective disorder, and bipolar disorder with psychotic features), severity of each different subtype of abuse was compared between diagnostic groups. There was no main effect of diagnosis (F(10, 216) = 1.14, p = .33). Additionally, we did not find significant differences between the diagnostic groups on any sub-type of abuse, with the exception of emotional abuse (F(2,111) = 3.06, p=.051), which post-hoc analyses revealed to be driven by higher emotional abuse within the schizoaffective group (p = .016; means (standard deviation) for schizoaffective disorder: 14.57(5.4), schizophrenia: 11.38(5.2), bipolar disorder: 12.12(6.2)).
In order to test the hypothesis that childhood abuse is related to the experience of auditory hallucinations, we performed a MANOVA with all sub-types of abuse predicted by the presence or absence of auditory hallucinations, controlling for depression. This overall model was non-significant (F(5, 106) = 1.26, p = .29). Based on our a priori hypothesis of a specific relationship between childhood sexual abuse and the presence of auditory hallucinations, we compared scores on the CTQ sexual abuse subscale between patients with or without a history of auditory hallucinations. We found that patients with a psychotic disorder who had experienced auditory hallucinations reported significantly more childhood sexual abuse than patients who had never experienced auditory hallucinations (F(1, 112) = 6.2, p = .01). This relationship remained when controlling for symptoms of depression (F(1, 110) = 4.5, p = .04). A similar pattern of results was found when excluding patients with a co-morbid PTSD diagnosis (n = 16).
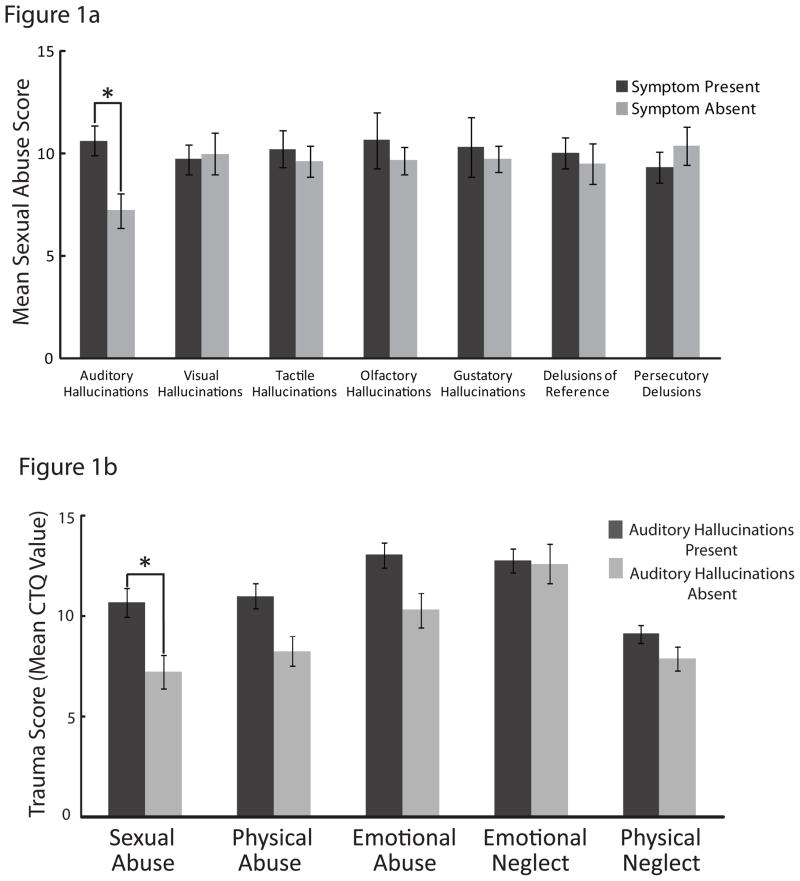
To determine whether there were differences in childhood abuse scores for the other types of psychotic symptoms, we performed a similar MANOVA for each type of hallucination and delusion, controlling for depression. None of these models were significant, so no post-hoc tests were performed. To further examine the specificity of the relationship between sexual abuse and auditory hallucinations, we performed one-way ANOVAs to compare severity of sexual abuse for each other positive symptom. We found no significant differences between sexual abuse scores for patients with and without the experience of other types of hallucinations (visual, tactile, olfactory, and gustatory; all F’s < .40, p’s > .53). Similarly, childhood sexual abuse scores did not differ between patients who did experience any of 8 types of delusions (reference, persecutory, grandiose, somatic, other, control, thought broadcasting, and bizarre) and those who did not (all F’s < .97, all p’s > .33) (Figure 1a).
Figure 1.
Figure 1a. Sexual Abuse Scores for Psychosis Patients With and Without Specific Positive Symptoms
Average scores on the CTQ sexual abuse subscale for individuals who have (symptom present) or have not (symptom absent) experienced each psychotic symptom. Psychotic disorder patients who have experienced auditory hallucinations report significantly more childhood sexual abuse than patients who have never experienced auditory hallucinations (p = .01). This difference in sexual abuse scores is not seen when patients are split by those who have or have not experienced any other type of hallucination or delusion. This figure presents average sexual abuse scores for all types of hallucinations and two of the most common forms of delusions (delusions of reference and persecutory delusions).
Figure 1b. Severity of Different Types of Abuse in Psychosis Patients With and Without Auditory Hallucinations
Average scores on all five CTQ abuse subscales for psychotic disorder patients split by those who have experienced auditory hallucinations (auditory hallucinations present) or have not experienced auditory hallucinations (auditory hallucinations absent). Psychotic disorder patients who have experienced auditory hallucinations report significantly more childhood sexual abuse (p = .01), physical abuse (p = .02), and emotional abuse (p = .03) than patients who have not experienced auditory hallucinations. However, when controlling for depression, this relationship only remains for sexual abuse (p = .04).
Due to the high correlation between sexual abuse, emotional abuse, and physical abuse in our sample (emotional and sexual abuse: r = .63, p<.001; physical and sexual abuse: r = .66, p<.001), we wanted to test whether the presence of sexual abuse confers risk for auditory hallucinations above and beyond physical and emotional abuse. This became particularly important after exploratory analyses revealed significantly greater emotional abuse (F(1, 112) = 4.93, p = .03) and physical abuse (F(1, 112) = 5.52, p = .02) in patients who had experienced auditory hallucinations compared to those who had not (Figure 1b). After controlling for depression these relationships failed to reach statistical significance after controlling for depression (emotional abuse: F(1, 110) = 1.93, p = .17; physical abuse: F(1, 110) = 3.6, p = .06), To further establish the specificity of sexual abuse as a risk factor for auditory hallucinations, we performed a binary logistic regression with sexual, physical, and emotional abuse as covariates and the experience of auditory hallucinations as the dependent variable. The model was significant (χ2 = 8.68, p = .03), but no single abuse type was a significant independent predictor for auditory hallucinations. However, sexual abuse had the lowest p-value relative to the other factors tested (sexual abuse χ2 = 1.62, p = .20, emotional abuse: χ2 = .17, p = .69; physical abuse: χ2 = .63, p = .43).
Because the independent effect of sexual abuse is difficult to disentangle from emotional and physical abuse, we performed a post-hoc analysis to test whether physical and/or emotional abuse—in the absence of sexual abuse—confers a risk for auditory hallucinations. For this analysis, we selected a sample (n=49) of individuals from the psychotic disorders group with no history of sexual abuse (scores 5–9 on sexual abuse subscale), but with similar emotional and physical abuse scores to the entire psychotic disorders group (t(162)=.76, p=.45; t(162)=1.11, p=.27, respectively). We split this sample into patients who had (n = 15) and had not (n = 34) experienced auditory hallucinations, and using a MANOVA found no significant difference in the severity of emotional abuse or physical abuse between groups (overall model (F(2, 46) = .22, p = .82; emotional abuse (F(1, 47) = .35, p = .56); physical abuse (F(1, 47) = .17, p = .68)). These results suggest that the pattern observed in the full dataset cannot be explained by physical or emotional abuse alone, and supports the notion that childhood sexual abuse is a specific risk factor for the experience of auditory hallucinations in psychotic disorder patients.
Discussion
We found that psychotic disorder patients experienced elevated rates of childhood trauma across all domains measured by the CTQ, relative to demographically-similar healthy control participants, which is consistent with previous research (3, 17, 32). This confirms that all types of childhood abuse put individuals at risk for the development of a serious psychiatric disorder (1, 15, 33, 34). We also found that psychotic disorder patients who experience auditory hallucinations report significantly more severe childhood sexual, physical and emotional abuse than patients who have never experienced auditory hallucinations. This finding is consistent with our a priori hypothesis of a relationship between childhood sexual abuse and auditory hallucinations, which has been suggested by earlier studies (8, 10, 12). We also found a similar relationship between auditory hallucinations and the experience of childhood physical and emotional abuse, two forms of abuse that were highly correlated with childhood sexual abuse. This high correlation between abuse types was reflected in our significant model of emotional, physical and sexual abuse predicting auditory hallucinations, in which none of the abuse types were significant independent predictors, suggesting that their inter-correlation limited our ability to detect independent effects. In the absence of childhood sexual abuse, however, childhood physical and emotional abuse showed no significant relationship with auditory hallucinations, suggesting that the experience of sexual abuse confers a greater risk for developing auditory hallucinations than emotional or physical abuse alone. In addition, childhood sexual abuse was the only type of abuse that continued to be associated with auditory hallucinations after controlling for symptoms of depression.
Interestingly, childhood sexual abuse was only related to auditory hallucinations but not other psychotic symptoms, indicating the auditory system may be especially vulnerable to the effects of childhood abuse. This pattern of results was not simply driven by co-morbid PTSD or depressive symptoms, and was observed in a sample that includes patients with schizophrenia, schizoaffective disorder, and bipolar disorder with psychotic features, suggesting also that childhood abuse, in particular childhood sexual abuse, may shape the phenotype of psychosis across diagnostic categories.
Notably, the current study addresses several limitations of earlier investigations by assessing childhood trauma with the CTQ, a reliable, valid and continuous measure of childhood trauma, in a large sample of well-characterized patients with a psychotic disorder compared with a group of healthy control participants. Although childhood abuse is not the only stressor linked to the development of psychosis, with some studies pointing to bullying (18) and daily life stress (35) as predictors, our study is, to our knowledge, among the first to equally assess and compare the impact of five major types of childhood abuse on a variety of psychotic symptoms. This systematic assessment provided a better window for looking at childhood abuse as a risk factor for psychosis, and allowed us to find specific relationships between childhood sexual, physical and emotional abuse and the experience of auditory hallucinations.
Previous Findings
A variety of studies have found a significant relationship between the experience of childhood abuse and an increased risk for adult psychopathology (1, 34, 36). In particular, evidence points to childhood abuse as an environmental stressor that increases one’s risk of developing psychosis. For example, Cutajar et al (3) reviewed state records to identify people with and without a history of childhood sexual abuse, and found that individuals who experienced childhood sexual abuse had significantly higher rates of psychotic disorders. Using interviews, Bebbington et al (16) found that the experience of sexual abuse conferred a higher odds ratio for experiencing psychosis, and that risk of psychosis increased with more exposure to sexual abuse. While these studies did not systematically assess the influence of multiple types of abuse, they provide strong evidence of a link between the experience of childhood sexual abuse and the development of psychotic symptoms later in life.
Studies have also examined the relationship between childhood abuse and the experience of specific positive symptoms, many of which point to an association between sexual abuse and hallucinations (for review see McCarthy-Jones, 2011 (37)). Shevlin et al (7) found that neglect, rape, and molestation all significantly increased an individuals’ risk for visual hallucinations, while childhood rape and molestation increased the risk of experiencing auditory hallucinations. In a sample of bipolar disorder patients, Hammersley et al (11) found that individuals who had experienced childhood sexual abuse were significantly more likely to report auditory hallucinations than those who had not. Finally, in a group of non-psychotic disordered individuals who experienced auditory-visual hallucinations, psychotic disorder patients who experienced auditory-visual hallucinations, and healthy control subjects, Daahlman et al (10) found higher rates of childhood sexual and emotional abuse in both cohorts of individuals who hallucinated, regardless of disease status. This provided evidence for childhood trauma as a specific risk factor for the development of auditory-visual hallucinations. Our current findings add to this literature and support previous proposals of a specific link between childhood abuse and auditory hallucinations, with evidence for childhood sexual abuse as a particular risk factor.
Why might an association between childhood sexual abuse and auditory hallucinations exist?
While there is no clear answer to this question, one possible theoretical framework for understanding this relationship is the diathesis-stress model of schizophrenia, envisioned by Bleuler and further developed by Rosenthal (38), Mirsky (39), Ciompi (40) and others. This model suggests that for individuals with an underlying biological vulnerability for mental illness, environmental stressors can exacerbate this vulnerability and result in the manifestation of a psychiatric disorder. Previous research has shown that childhood trauma is a stressor with particular effects on brain regions involved in the hypothalamic-pituitary-adrenal (HPA) axis, a system which is activated as part of the stress response in humans (41), and is thought to be abnormal in patients with schizophrenia (for review, see Walker et al, 2008 (42)). In fact, it has been shown that a history of childhood trauma is associated with increased emotional and psychotic reactions to small daily stressors in patients with psychotic disorders. This suggests that the experience of childhood trauma can lead to abnormalities in the stress response in adulthood, which the authors speculate may be due to an abnormal HPA axis response following exposure to trauma that relates to psychotic experiences (43). Therefore, the HPA axis provides a possible route through which childhood trauma could aggravate the underlying biological risk factors implicit in schizophrenia, putting individuals at greater risk for experiencing symptoms of psychosis. Although the neural underpinnings of auditory hallucinations are still largely unclear, we speculate that the networks involved in auditory hallucinations are particularly affected by the stress of childhood trauma, resulting in an even greater risk for the experience of auditory hallucinations.
Limitations
While our study addresses methodological issues found in previous papers, there are still limitations. Because of the high prevalence of auditory hallucinations in our psychotic disorder group, our cohort of individuals who had not experienced auditory hallucinations (n=27) was small compared with those who did (n = 87). Additional studies with a larger sample of patients without auditory hallucinations would be helpful to test the generalizability of our findings. Also, although self-report questionnaires are often used in psychiatric populations, many patients in the current study were assessed following a psychiatric hospitalization, and were experiencing psychotic symptoms at the time of study. While patients completed the questionnaires when both the treating physician and research team felt they were stable enough to participate in a research study, in some cases the self-reported values may be imprecise. Finally, the CTQ is a measurement of abuse experienced before the age of 18, and the average age of our participants was over 30 years old, indicating a significant period of time between the abuse and self-report. In some cases this delay may have resulted in a recall bias of inexact or incomplete data.
Clinical Implications
The relationship between childhood abuse and auditory hallucinations has clinical implications. Clinicians should obtain an abuse history from patients who experience auditory hallucinations, since the patient might not reveal such a history and miss appropriate treatment. Also, clinicians should be aware of the high correlation between childhood sexual, physical and emotional abuse, and consider all of these abuse types as potential risk factors for experiencing auditory hallucinations. Any person with a known history of sexual, physical or emotional trauma should be evaluated for auditory hallucinations. Finally, these results were found in a cohort of individuals with schizophrenia, schizoaffective disorder, and bipolar disorder, suggesting that childhood trauma is a risk factor for auditory hallucinations across multiple psychotic disorders. Prevention, early intervention and treatment models should be considered for this cohort of individuals who are at a greater risk for developing a serious psychiatric disorder.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP. Childhood sexual abuse and mental health in adult life. Br J Psychiatry. 1993;163:721–32. doi: 10.1192/bjp.163.6.721. [DOI] [PubMed] [Google Scholar]
- 2.Janssen I, Krabbendam L, Bak M, Hanssen M, Vollebergh W, de Graaf R, et al. Childhood abuse as a risk factor for psychotic experiences. Acta Psychiatr Scand. 2004;109:38–45. doi: 10.1046/j.0001-690x.2003.00217.x. [DOI] [PubMed] [Google Scholar]
- 3.Cutajar MC, Mullen PE, Ogloff JR, Thomas SD, Wells DL, Spataro J. Schizophrenia and other psychotic disorders in a cohort of sexually abused children. Arch Gen Psychiatry. 2010;67:1114–9. doi: 10.1001/archgenpsychiatry.2010.147. [DOI] [PubMed] [Google Scholar]
- 4.Spauwen J, Krabbendam L, Lieb R, Wittchen HU, van Os J. Impact of psychological trauma on the development of psychotic symptoms: relationship with psychosis proneness. Br J Psychiatry. 2006;188:527–33. doi: 10.1192/bjp.bp.105.011346. [DOI] [PubMed] [Google Scholar]
- 5.Scott J, Chant D, Andrews G, Martin G, McGrath J. Association between trauma exposure and delusional experiences in a large community-based sample. Br J Psychiatry. 2007;190:339–43. doi: 10.1192/bjp.bp.106.026708. [DOI] [PubMed] [Google Scholar]
- 6.Holowka DW, King S, Saheb D, Pukall M, Brunet A. Childhood abuse and dissociative symptoms in adult schizophrenia. Schizophr Res. 2003;60:87–90. doi: 10.1016/s0920-9964(02)00296-7. [DOI] [PubMed] [Google Scholar]
- 7.Shevlin M, Dorahy M, Adamson G. Childhood traumas and hallucinations: an analysis of the National Comorbidity Survey. J Psychiatr Res. 2007;41:222–8. doi: 10.1016/j.jpsychires.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Hardy A, Fowler D, Freeman D, Smith B, Steel C, Evans J, et al. Trauma and hallucinatory experience in psychosis. J Nerv Ment Dis. 2005;193:501–7. doi: 10.1097/01.nmd.0000172480.56308.21. [DOI] [PubMed] [Google Scholar]
- 9.Whitfield CL, Dube SR, Felitti VJ, Anda RF. Adverse childhood experiences and hallucinations. Child Abuse Negl. 2005;29:797–810. doi: 10.1016/j.chiabu.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Daahlman KM, Diederen KMJ, Derks EM, van Lutterveld R, Kahn RS, Sommer IEC. Childhood trauma and auditory verbal hallucinations. Psychological Medicine. 2012;42:2475–2484. doi: 10.1017/S0033291712000761. [DOI] [PubMed] [Google Scholar]
- 11.Hammersley P, Dias A, Todd G, Bowen-Jones K, Reilly B, Bentall RP. Childhood trauma and hallucinations in bipolar affective disorder: preliminary investigation. Br J Psychiatry. 2003;182:543–7. doi: 10.1192/bjp.182.6.543. [DOI] [PubMed] [Google Scholar]
- 12.Read J, Agar K, Argyle N, Aderhold V. Sexual and physical abuse during childhood and adulthood as predictors of hallucinations, delusions and thought disorder. Psychol Psychother. 2003;76:1–22. doi: 10.1348/14760830260569210. [DOI] [PubMed] [Google Scholar]
- 13.Bendall S, Jackson HJ, Hulbert CA, McGorry PD. Childhood trauma and psychotic disorders: a systematic, critical review of the evidence. Schizophr Bull. 2008;34:568–79. doi: 10.1093/schbul/sbm121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morgan C, Fisher H. Environment and schizophrenia: environmental factors in schizophrenia: childhood trauma--a critical review. Schizophr Bull. 2007;33:3–10. doi: 10.1093/schbul/sbl053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spataro J, Mullen PE, Burgess PM, Wells DL, Moss SA. Impact of child sexual abuse on mental health: prospective study in males and females. Br J Psychiatry. 2004;184:416–21. doi: 10.1192/bjp.184.5.416. [DOI] [PubMed] [Google Scholar]
- 16.Bebbington P, Jonas S, Kuipers E, King M, Cooper C, Brugha T, et al. Childhood sexual abuse and psychosis: data from a cross-sectional national psychiatric survey in England. Br J Psychiatry. 2011;199:29–37. doi: 10.1192/bjp.bp.110.083642. [DOI] [PubMed] [Google Scholar]
- 17.Heins M, Simons C, Lataster T, Pfeifer S, Versmissed D, Lardinois M, et al. Childhood trauma and psychosis: a case-control and case-sibling comparison across different levels of genetic liability, psychopathology and type of trauma. Am J Psychiatry. 2011;168:1286–1294. doi: 10.1176/appi.ajp.2011.10101531. [DOI] [PubMed] [Google Scholar]
- 18.Kellehan I, Keeley H, Corcoran P, Ramsay H, Wasserman C, Carli V, et al. Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. Am J Psychiatry. 2013;AiA:1–8. doi: 10.1176/appi.ajp.2012.12091169. [DOI] [PubMed] [Google Scholar]
- 19.Thompson AD, Nelson B, Yuen HP, Lin A, Amminger GP, McGorry PD, et al. Sexual trauma increases the risk of developing psychosis in an ultra high-risk “prodromal” population. Schizophr Bull. 2013 doi: 10.1093/schbul/sbt032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paivio SC, Cramer KM. Factor structure and reliability of the Childhood Trauma Questionnaire in a Canadian undergraduate student sample. Child Abuse Negl. 2004;28:889–904. doi: 10.1016/j.chiabu.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 21.Scher CD, Stein MB, Asmundson GJ, McCreary DR, Forde DR. The childhood trauma questionnaire in a community sample: psychometric properties and normative data. J Trauma Stress. 2001;14:843–57. doi: 10.1023/A:1013058625719. [DOI] [PubMed] [Google Scholar]
- 22.Wright KD, Asmundson GJ, McCreary DR, Scher C, Hami S, Stein MB. Factorial validity of the Childhood Trauma Questionnaire in men and women. Depress Anxiety. 2001;13:179–83. [PubMed] [Google Scholar]
- 23.Bernstein DP, Fink L. Pearson Education. 1997. Childhood Trauma Questionniare: A Retrospective Self-Report (CTQ) [Google Scholar]
- 24.Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–90. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 25.Meyer IH, Muenzenmaier K, Cancienne J, Struening E. Reliability and validity of a measure of sexual and physical abuse histories among women with serious mental illness. Child Abuse Negl. 1996;20:213–9. doi: 10.1016/s0145-2134(95)00137-9. [DOI] [PubMed] [Google Scholar]
- 26.Niv N, Cohen AN, Mintz J, Ventura J, Young AS. The validity of using patient self-report to assess psychotic symptoms in schizophrenia. Schizophr Res. 2007;90:245–50. doi: 10.1016/j.schres.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 27.Goldberg RW, Seybolt DC, Lehman A. Reliable self-report of health service use by individuals with serious mental illness. Psychiatr Serv. 2002;53:879–81. doi: 10.1176/appi.ps.53.7.879. [DOI] [PubMed] [Google Scholar]
- 28.Fisher HL, Craig TK, Fearon P, Morgan K, Dazzan P, Lappin J, et al. Reliability and comparability of psychosis patients’ retrospective reports of childhood abuse. Schizophr Bull. 2011;37:546–53. doi: 10.1093/schbul/sbp103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dill DL, Chu JA, Grob MC, Eisen SV. The reliability of abuse history reports: a comparison of two inquiry formats. Compr Psychiatry. 1991;32:166–9. doi: 10.1016/0010-440x(91)90009-2. [DOI] [PubMed] [Google Scholar]
- 30.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Friedman S, Harrison G. Sexual histories, attitudes, and behavior of schizophrenic and “normal” women. Arch Sex Behav. 1984;13:555–67. doi: 10.1007/BF01542090. [DOI] [PubMed] [Google Scholar]
- 32.Nettelbladt P, Svensson C, Serin U. Background factors in patients with schizoaffective disorder as compared with patients with diabetes and healthy individuals. Eur Arch Psychiatry Clin Neurosci. 1996;246:213–8. doi: 10.1007/BF02188956. [DOI] [PubMed] [Google Scholar]
- 33.Rosenberg SD, Lu W, Mueser KT, Jankowski MK, Cournos F. Correlates of adverse childhood events among adults with schizophrenia spectrum disorders. Psychiatr Serv. 2007;58:245–53. doi: 10.1176/ps.2007.58.2.245. [DOI] [PubMed] [Google Scholar]
- 34.Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Arch Gen Psychiatry. 2007;64:49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]
- 35.Van Winkel R, Stefanis NC, Mylin-Germeys I. Psychosocial stress and psychosis. A review of the neurobiological mechanisms and the evidence for gene-stress interaction. Schizophr Bull. 2008;34:1095–1105. doi: 10.1093/schbul/sbn101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 37.McCarthy-Jones S. Voices from the storm: a critical review of quantitative studies of auditory verbal hallucinations and childhood sexual abuse. Clin Psychol Rev. 2011;31:983–92. doi: 10.1016/j.cpr.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 38.Rosenthal D. Genetic theory and abnormal behavior. New York: McGraw-Hill; 1970. [Google Scholar]
- 39.Mirsky AF, Duncan CC. Etiology and expression of schizophrenia: neurobiological and psychosocial factors. Annu Rev Psychol. 1986;37:291–319. doi: 10.1146/annurev.ps.37.020186.001451. [DOI] [PubMed] [Google Scholar]
- 40.Ciompi L. The psyche and schizophrenia: the bond between affect and logic. Cambridge, Mass: Harvard University Press; 1988. [Google Scholar]
- 41.Charmandari E, Kino T, Souvatzoglou E, Chrousos GP. Pediatric stress: hormonal mediators and human development. Horm Res. 2003;59:161–79. doi: 10.1159/000069325. [DOI] [PubMed] [Google Scholar]
- 42.Walker E, Mittal V, Tessner K. Stress and the hypothalamic pituitary adrenal axis in the developmental course of schizophrenia. Annu Rev Clin Psycho. 2008;4:189–216. doi: 10.1146/annurev.clinpsy.4.022007.141248. [DOI] [PubMed] [Google Scholar]
- 43.Lardinois M, Lataster T, Mengelers R, van Os J, Myin-Germeys I. Acta Psychiatr Scand. 2011;123:28–35. doi: 10.1111/j.1600-0447.2010.01594.x. [DOI] [PubMed] [Google Scholar]