Abstract
Background
Patients with acute leukemia require immediate and aggressive in-patient treatment that results in many weeks to months of hospitalization. Thus, it is not surprising that distress has been found in as many as 45.5% of patients. While distress is a regularly reported outcome measure in clinical research, currently there is a lack of a clear consistent and universal definition of this concept.
Objective
The purpose of this article is to examine the current state of the science surrounding the concept of distress and propose a model of distress for patients with acute leukemia.
Interventions/Methods
The Walker and Avant framework was used to guide the analysis of the concept of distress in patients with AL. The findings from this analysis were then used to generate a model guided by the current science.
Results
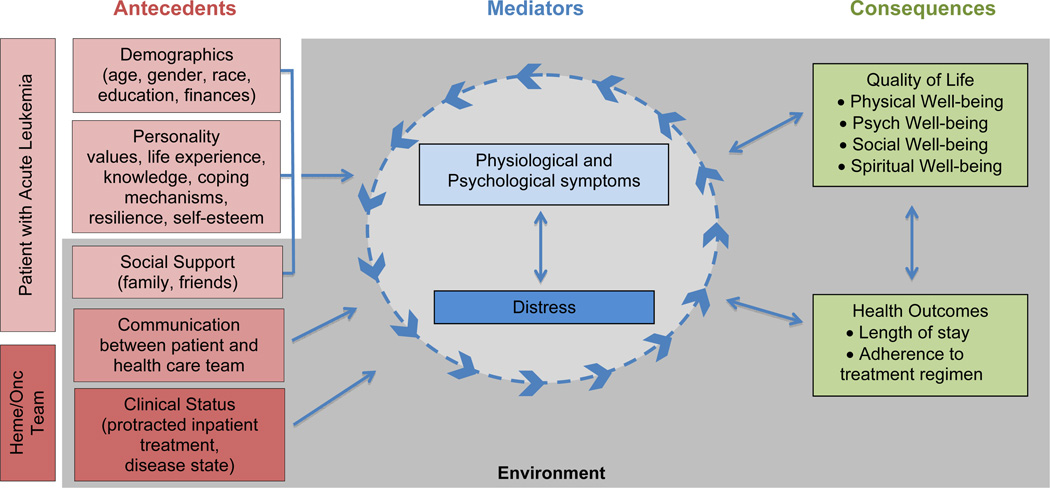
Distress in AL is generally accepted as multi-dimensional, quantifiable, subjective and temporal. Antecedents to distress include: demographics; intrinsic factors; social support; disease progression; treatment; and communication. Consequences to distress include: decreased quality of life; patient outcomes; as well as the severity of physical and psychological symptoms.
Conclusions
Distress is an outcome measure that is frequently assessed and reported within the literature. The operationalization of distress varies by investigator, limiting its generalizabiliy.
Implications for Practice
The proposed conceptual model may be used to guide further research on distress in patients with AL at high risk for negative outcomes. Improved understanding of patient distress may guide interventions aimed at managing the psychosocial needs for patients receiving treatment for AL.
Keywords: distress, acute leukemia, concept analysis, quality of life, symptoms
Model Case
K.B. is a 45 year old woman who presented to her primary care physician with complaints of flu-like symptoms. She also mentioned that she had increasing fatigue over the past few weeks and seemed to be bruising quite easily. Her doctor ordered lab work and K.B. received a call the next day from her doctor instructing her to go directly to hospital for further work-up. Further investigation confirmed that she had acute myelogenous leukemia. K.B. was immediately admitted to the hospital, underwent cardiac assessment with evaluation of left ventricular function and central-line catheter placement, and induction chemotherapy was initiated the next day and consisted of 24-hour high-dose chemotherapy every day for 7 days. Complications from the intense chemotherapy included mucositis and fungal pneumonia, which left her hospitalized for a total of 9 weeks. At a follow-up visit she was found to have relapsed disease and was subsequently readmitted for re-induction chemotherapy. K.B. remains hospitalized post re-induction secondary to neutropenic fever of unknown origin. Her family lives several hours away and her 3 children are unable to visit regularly due to transportation challenges, though her husband tries to bring at least one of them on most weekends. The nursing staff has noted that K.B. appears increasingly withdrawn, remains in her room and in bed most days and engages in less conversation than she did when she was first diagnosed. K.B. has expressed to her nurse Ruth that “she is just not sure she can do this over again”.
Introduction
The diagnosis of cancer for individuals and their families is inevitably a time filled with fear, uncertainty and questions. The person with cancer most often is required to make sudden modifications to their lifestyle which impacts every dimension of daily life;1 all while they are forced to face the possibility of their own mortality. Adding to the emotional toll of the cancer diagnosis, patients can experience intense treatment and disease related side-effects resulting in numerous symptoms that occur concurrently and are often disrupting, if not debilitating.2 Unfortunately when symptoms go unrecognized or undertreated by practitioners there is an increased risk that the patient may experience: additional/prolonged hospital stays, interruption in needed treatment, increased dependence and decreased functional status,2 all factors that may result in high levels of distress for patients and family members.
In patients diagnosed with acute leukemia (AL) adding to the natural complexities of a cancer diagnosis is the need for immediate and aggressive treatment, which is then often followed by additional weeks to months hospitalized. If left untreated AL can be fatal in as little as a few weeks,3 while even with treatment the relative 5-year survival rate is approximately 23.9% for patients with acute myeloid leukemia and 55.2% for patients with acute lymphoblastic leukemia.4 Treatment for AL requires patients to be hospitalized for the chemotherapy treatment, which takes place over a five-day to four-week period depending on disease type and phase of treatment.5,6 Patients typically spend many additional weeks hospitalized for supportive care needs depending on common disease and treatment-related complications including: neutropenic fever, mucositis, anemia, and thrombocytopenia.
Given that people diagnosed with AL often experience numerous physical and psychological symptoms it is not surprising that a high level of distress is generally found in this population.1,7,8 Specifically distress has been found to occur in over 45% of patients with leukemia.7,9 Yet, the physical and psychosocial issues faced by patients with AL are relatively understudied especially when compared to patients with many other solid tumors.10
The purpose of this article is to examine the current state of the science surrounding the concept of distress in patients diagnosed with acute leukemia. The findings from this examination will be used to propose a model of distress for patients with acute leukemia. Additionally, this paper will discuss the implications of distress on cancer nursing to enhance care and future research.
Methods
The Walker and Avant framework11 was used to guide the exploration and analysis of the concept of distress in patients with acute leukemia. This method involves examination of the defining attributes, as well as the antecedents and consequences found in the current literature around the concept under analysis. These findings are then used to generate a model guided by the current state of the science.
A review of literature published within the past 20 years was completed. The databases PubMed, Ovid, and PsychINFO were searched using the following combination of keywords: “distress”, “hematologic malignancy” and/or “acute leukemia”. This initial search combination resulted in 293 references in PubMed, 119 in Ovid/MEDLINE and 70 in PsychINFO. Literature included in the development of the concept was written in English and addressed distress (physical, psychological and/or psycho-social) through either review or clinical research in patients with either a hematologic malignancy or with acute leukemia specifically (excluding hematopoietic stem cell transplant). In each of the searches many of the references that surfaced were not related to distress in the hematology oncology population. Thus, the majority of the articles were excluded either because they discussed distress in bone marrow transplant patients or focused on symptom burden or respiratory distress. A total of 8 articles met the inclusion criteria.
The 8 articles were all descriptive studies investigating several different dimensions of distress including: symptom distress;12 quality of life and predictors of psychological distress;13 pain and emotional distress;14 psychological distress;15–17 symptom distress and link to distress and traumatic stress;18 and distress in incurable disease.19 Four of the articles included only patients with leukemia13,14,18,19 while the remaining 4 articles examined distress in patients with all hematologic malignancies15–17 or all cancers with a subset of patients with leukemia.12 The table details each of the studies reviewed and includes defining concept attributes, antecedents of distress, the empirical referents (operational definition of distress that was adopted for each study) as well as limitations of each study.
Concept Analysis
“Distress” is generally defined as “pain or suffering affecting the body, a bodily part, or the mind”.20 The National Comprehensive Cancer Network (NCCN) defines distress as “a multifactorial unpleasant emotional experience of a psychological (cognitive, behavioral, emotional), social and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms and its treatment…”21
The NCCN standard of care guidelines for the clinical setting state that “all patients should be screened for distress at their initial visit, at appropriate intervals, and as clinically indicated especially with changes in disease status.”21 The recommended assessment tool is the Distress Thermometer, which measures global distress via a numerical rating scale as well as five domains of distress including: practical problems, family problems, emotional problems, physical problems and spiritual/religious concerns.
Distress is also regularly a reported outcome measure in clinical research; however, most often there is not a clear, consistent definition of the concept. For example, quality of life and distress have been used interchangeably in the literature, and while these concepts do share similar domains, they are indeed unique and thus need to be distinguished.22 In contrast to distress as defined by NCCN, health-related quality of life (HQoL) focuses on outcomes related to disease and treatment, essentially eliciting those facets of life that are related to an individual’s health.23 There are four specific domains that are accepted as contributing to an individual’s overall HQoL state including: symptom status, functional status, general health perceptions, and overall quality of life.24
In addition, psychological and symptom distress are often not clearly distinguished in the literature. Psychological distress is defined as a “unique discomforting, emotional state… in response to a stressor”(pg. 539)25 While, Rhodes and Watson (1987), defined symptom distress as “degree or amount of physical or mental upset, anguish, or suffering experienced from a specific symptom.”(pg. 243)26 Symptom distress results from global distress in response to psychological and neurophysiological and immunological events.26 Though, there are similar themes among these varying distress terms, each is a unique manifestation for patients and families.
Dimensions and Attributes of Distress
All eight of the articles implied that distress for patients with acute leukemia is generally accepted to be multi-dimensional, quantifiable, subjective and temporal. And while none of the eight articles explicitly defined distress they did operationalize distress as a variety of dimensions including, psychological distress;12–19 physical distress;12,18,19 anticipatory distress related to sequelae of the disease-treatment;13 family distress;12,19 as well as social and decision-making distress.19
Distress is accepted as being a quantifiable, subjective concept most often assessed through the use of a patient-reported numerical rating scale. However, currently there is not a uniform approach to measuring the distress level of patients. From the literature the most commonly used approach for the assessment of distress is through the patient reported measures of anxiety and depression such as the Hospital Anxiety and Depression Scale,14–17 and/or through physical symptom inventories such as the Edmonton Symptom Assessment Scale,12,14 the Memorial Symptom Assessment Scale,18 the Brief Symptom Inventory,13 or the Functional Assessment of Chronic Illness Therapy.17,18
The defining attributes of the concept of distress in patients with AL include: (1) difficulty coping with disease or treatment process for AL, (2) presence of acute psychological and/or physiological discomfort, (3) acute change(s) to interpersonal communication and/or relationships, (4) difficulty enjoying life.
Example Cases
Walker and Avant (2011) recommend examining cases that illustrate both the purest case as well as additional cases that are similar but not exact to the proposed concept and model. The authors opted to present the model case at the beginning of this paper to set a clear scenario of the acute leukemia patient for the readers. Here additional cases will be presented to further demonstrate how the characteristics of the concept of distress in patients with acute leukemia are unique.
A borderline case contains most but not all the of the concepts’ attributes.11 The following is an example of such a borderline case. J.O. has been hospitalized for the past two weeks receiving induction chemotherapy for the treatment of his AL. The nurses note that he is anxious about how long he is going to spend in the hospital. He is complaining about difficulty sleeping yet he feels tired all the time. His family has been coming in to visit and when they are here he can be found laughing and enjoying his time with them. This case shows that J.O. does appear to have some trouble coping with the treatment and length of hospitalization and he also has physiological and psychological symptoms. However, he is still able to enjoy the visits with his family and interact normally.
A related case includes concepts that are related to the concept being examined, but are missing at least one attribute.11 L.M. is lying in bed extremely uncomfortable and exhausted. She can’t stop itching from a skin rash that developed after receiving a new antibiotic. She has expressed how uncomfortable and upset she is with her current state. This is an example of symptom distress as her frustration is directly related to her physical symptom and lacks additional necessary attributes associated with the concept of distress.
Contrary cases are examples that are clearly “not the concept”.11 C.R. most often has music playing in her room, with the blinds open to let the sunshine in. She has a bucket of candy for all her visitors on her bedside table and frequently has visitors. The nurses comment on how upbeat she has remained through her treatment. In this case none of the attributes of the concept are present.
Antecedents to Distress
There are several antecedent factors found to impact the distress that patients with leukemia experience. The patients are themselves, dynamic and multidimensional, and their perceptions are influenced by such factors as their education, age and gender.13 Specifically, those who are younger and female tend to be more prone to distress than older males. Additionally, personal intrinsic factors such as a person’s ability to adapt to treatment, having a fighting spirit,15 the presence of hopelessness/helpless, and degree of self-esteem15,18 have also been found to influence levels of distress in patients with acute leukemia. That is if an individual is considered to adapt well to treatment, possess a fighting spirit, not feel helpless or hopeless and or have a high degree of self-esteem, then their level of distress is hypothesized to be less than someone with the opposite intrinsic factors. The presence of strong social support networks has been found to be protective against the development of distress.13,15,18 The progression of time (i.e: time is moving slowly or time is moving quickly) was considered by Wittman and colleagues (2006) to also be an antecedent factor to distress.
The stage and the progression of the disease12,16 as well as the type of treatment12,14 and failure of treatment19 have also been found to contribute to the development of distress. Rodin and colleagues (2011) found that the patient’s ability to communicate with the health care team also influences the degree of distress experienced.
Consequences of Distress
The overall attributes and antecedent factors related to the concept of distress have the potential to influence the degree of distress experienced by the patient with leukemia and may ultimately impact both patient outcomes as well as the perceived quality of life. When distress is present and unrelieved there is the potential for it to negatively impact a patients overall quality of life,12,15,17 as well as increase the severity of physical12,14,15 and psychological symptoms.13,14,16–18
Additionally, patient outcomes12 were found to be effected by levels of distress. In this study, Delgado-Guay and colleagues (2009) found that the outcomes for patients admitted to the hospital who also received a palliative care referral were identified to have improved symptom management (pain, dyspnea, nausea, anxiety and delirium) which lead to decreased invasive measures for patients and was associated with survival to ICU discharge. Thus, by improving the levels of distress patients with acute leukemia experience there is the potential to positively impact not only a patient’s quality of life, but also patient related outcomes.
Through synthesis of the literature the proposed definition of distress experienced by acute leukemia patients is a multidimensional, subjective, quantifiable and temporal negative emotional response to their diagnosis, disease treatment, the environment they are in, as well as the psychological and physiologic symptoms they experience. As discussed previously, patients’ distress may be influenced by such factors, as demographics (e.g: age or gender),13 personality (e.g: spiritualness, coping style or optimistic/pessimistic),15,18 social support (e.g: interpersonal relationships, presence of family and friends),13,15,18 as well as their relationship and satisfaction with the health care team.18 Building from this definition, the included figure proposes a model of distress including the antecedents and consequences that have been found to influence the degree of distress experienced by patients with acute leukemia.
Figure.
Conceptual Model of Distress in Patients with Acute Leukemia
Implications for Clinical Practice and Research
Patients with acute leukemia often experience distress at varying degrees across their disease trajectory.9,27 Unrecognized and untreated distress is associated with increased symptoms and length of hospitalization, as well a reduced HQoL and may necessitate modifications in treatment regimens.28 Thus, nurses play a critical role in not only caring for patients who may be distressed, but also in the assessment and management of the distress that these patients may be experiencing.
Clinicians may find themselves wondering how the proposed model of distress in patients with acute leukemia can be of benefit to their practice. Revisiting the case study of K.B., the authors will now demonstrate how the proposed model can be used as a resource for clinicians to guide their nursing care for patients with acute leukemia.
After hearing K.B. confide that, “she is just not sure she can do this over again”, Ruth recognizes that K.B. has many of the antecedent’s shown in the model that increases her risk for experiencing distress. Specifically, K.B. is a mother who has expressed with both verbal and nonverbal queues that she is not adapting well to her treatment. Additionally, she is unable to see her spouse and children regularly, and may be struggling with guilt at not being able to be present for her husband and 3 children, and could internally fear that she may never, as her disease is not responding to treatment. Ruth also understands from the model that K.B. has had an extended hospitalization and as the model shows this environment, can negatively effect the patient, leaving them isolated from family and friends, void of personal space, privacy, and independence. This can then in turn exacerbate physiological and psychological symptoms which then can further increase feelings of distress and ultimately may mediate the development of many negative consequences (HQoL and Health Outcomes). Ruth, recognizing that K.B. is likely experiencing increased distress where patient care directed at managing this distress may improve both immediate and long-term outcomes for K.B., begins the first step in the nursing process: assessment.
Ruth sits down with K.B. and asks her how she is feeling. Ruth actively listens as K.B. expresses her concerns, fears, and how badly she is feeling. Ruth then asks K.B. specifically about the level of distress that she is feeling. With the information that Ruth has assessed regarding the distress that K.B. is experiencing, she is able to go to the healthcare team and plan distress management care. This plan will allow for the continuous management and evaluation of distress levels and care needs as K.B.’s treatment evolves across her disease trajectory.
The model case study demonstrates how nurses knowledgeable about the attributes as well the antecedents and consequences of distress can use the model as a guide to increase the assessment and subsequent management of distress in patients with acute leukemia under their care. Accurately and adequately defining and subsequently assessing the degree and specific components of distress for patients with acute leukemia is crucial to providing holistic care.
Much work has been done in the investigation of distress, however there is still much more work that needs to be done. Advancing our understanding of the concept of distress through the development and future testing of models such as the one proposed has the potential to both improve the direct delivery of care to patients as well as contribute to future research guided by theory. This understanding may ultimately lead to improved patient outcomes and perceived quality of life for this unique population. It is only with a clear understanding of concepts and relevant issues that advancement in knowledge and patient care is possible.
Conclusions
Distress is an outcome measure that is frequently assessed and reported within the literature. Yet, the operationalization of distress as it applies to patients with acute leukemia varies by investigator. This fact may often limit the generalizability of findings and interventions directed at distress for patients including those with acute leukemia. Additionally, by limiting the assessment of distress to either symptom distress or through the assessment of such psychological symptoms as anxiety and depression, there is likelihood that the greater meaning and impact of distress on patient’s quality of life is being either missed, underscored, or misinterpreted. The goal of proposing this conceptual model is to begin to identify a clear definition of distress in the unique population of patients with acute leukemia. This model will be tested in future research and, if necessary, modified based on the research findings.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: The authors have no conflicts of interest to disclose.
References
- 1.Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psycho-Oncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 2.Cleeland CS, Reyes-Gibby CC. When is it justified to treat symptoms? Measuring symptom burden. Oncology. 2002;16(9) Suppl 10:64–70. [PubMed] [Google Scholar]
- 3.Kumar CC. Genetic abnormalities and challenges in the treatment of acute myeloid leukemia. Genes & Cancer. 2011;2(2):95–107. doi: 10.1177/1947601911408076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Howlander N, Noone AM, Neyman N, et al. SEER Cancer Statistics Review, 1975– 2009. Bethesda, MD: 2012. [Google Scholar]
- 5.Dohner H, Estey EH, Amadori S, et al. Diagnosis and management of acute myeloid leukemia in adults: Recommendations from an international expert panel, on behalf of the European Leukemia Net. Blood. 2010;115(3):453–474. doi: 10.1182/blood-2009-07-235358. [DOI] [PubMed] [Google Scholar]
- 6.Estey E, Dohner H. Acute myeloid leukaemia. Lancet. 2006;368(9550):1894–1907. doi: 10.1016/S0140-6736(06)69780-8. [DOI] [PubMed] [Google Scholar]
- 7.Carlson LE, Angen M, Cullum J, et al. High levels of untreated distress and fatigue in cancer patients. British Journal of Cancer. 2004;90(12):2297–2304. doi: 10.1038/sj.bjc.6601887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manitta V, Zordan R, Cole-Sinclair M, Nandurkar H, Philip J. The symptom burden of patients with hematological malignancy: A cross-sectional observational study. Journal of Pain and Symptom Management. 2011;42(3):432–442. doi: 10.1016/j.jpainsymman.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Albrecht T, Rosenzweig M. The symptom experience in patients hospitalized for the treatment of acute leukemia. Oncology Nursing Forum. 2012;39(6):E517. [Google Scholar]
- 10.Paul CL, Sanson-Fisher R, Douglas HE, Clinton-McHarg T, Williamson A, Barker D. Cutting the research pie: A value-weighting approach to explore perceptions about psychosocial research priorities for adults with haematological cancers. European Journal of Cancer Care. 2011;20(3):345–353. doi: 10.1111/j.1365-2354.2010.01188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walker L, Avant K. Strategies for theory construction in nursing. 4th ed. Upper Saddle River, NJ: Pearson/Prentice Hall; 2005. [Google Scholar]
- 12.Delgado-Guay MO, Parsons HA, Li Z, Palmer LJ, Bruera E. Symptom distress, interventions, and outcomes of intensive care unit cancer patients referred to a palliative care consult team. Cancer. 2009;115(2):437–445. doi: 10.1002/cncr.24017. [DOI] [PubMed] [Google Scholar]
- 13.Greenberg DB, Kornblith AB, Herndon JE, et al. Quality of life for adult leukemia survivors treated on clinical trials of cancer and leukemia Group B during the period 1971– 1988: Predictors for later psychologic distress. Cancer. 1997;80(10):1936–1944. doi: 10.1002/(sici)1097-0142(19971115)80:10<1936::aid-cncr10>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 14.Morselli M, Bandieri E, Zanin R, et al. Pain and emotional distress in leukemia patients at diagnosis. Leukemia Research. 2010;34(2):e67–e68. doi: 10.1016/j.leukres.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 15.Montgomery C, Pocock M, Titley K, Lloyd K. Predicting psychological distress in patients with leukaemia and lymphoma. Journal of Psychosomatic Research. 2003;54(4):289–292. doi: 10.1016/s0022-3999(02)00396-3. [DOI] [PubMed] [Google Scholar]
- 16.Vollmer TC, Wittmann M, Schweiger C, Hiddemann W. Preoccupation with death as predictor of psychological distress in patients with haematologic malignancies. European Journal of Cancer Care. 2011;20(3):403–411. doi: 10.1111/j.1365-2354.2010.01203.x. [DOI] [PubMed] [Google Scholar]
- 17.Wittmann M, Vollmer T, Schweiger C, Hiddemann W. The relation between the experience of time and psychological distress in patients with hematological malignancies. Palliative & Supportive Care. 2006;4(4):357–363. doi: 10.1017/s1478951506060469. [DOI] [PubMed] [Google Scholar]
- 18.Rodin G, Yuen D, Mischitelle A, et al. Traumatic stress in acute leukemia. PsychoOncology. 2011 doi: 10.1002/pon.2092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shirai Y, Kawa M, Miyashita M, Kazuma K. Nurses’ perception of adequacy of care for leukemia patients with distress during the incurable phase and related factors. Leukemia Research. 2005;29(3):293–300. doi: 10.1016/j.leukres.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 20.Anon. Merriam-Webster On-line Dictionary. 2012 Jan 20; Available at: http://www.merriam-webster.com.
- 21.Holland J, Anderson B, Beriebart W, et al. NCCN Clinical Practice Guidelines in Oncology: Distress; v3. 2012 [Google Scholar]
- 22.Carlson LE, Bultz BD. Cancer distress screening: Needs, models, and methods. Journal of Psychosomatic Research. 2003;55(5):403–409. doi: 10.1016/s0022-3999(03)00514-2. [DOI] [PubMed] [Google Scholar]
- 23.Ferrans CE, Zerwic JJ, Wilbur JE, Larson JL. Conceptual model of health-related quality of life. Journal of Nursing Scholarship. 2005;37(4):336–342. doi: 10.1111/j.1547-5069.2005.00058.x. [DOI] [PubMed] [Google Scholar]
- 24.Ferrans CE. Advances in measuring quality-of-life outcomes in cancer care. Seminars in Oncology Nursing. 2010;26(1):2–11. doi: 10.1016/j.soncn.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Ridner S. Psychological distress: Concept analysis. Journal of Advanced Nursing. 2004;45(5):536–545. doi: 10.1046/j.1365-2648.2003.02938.x. [DOI] [PubMed] [Google Scholar]
- 26.Rhodes V, Watson P. Symptom distress–the concept: Past and present. Seminars in Oncology Nursing. 1987;3(4):242–247. doi: 10.1016/s0749-2081(87)80014-1. [DOI] [PubMed] [Google Scholar]
- 27.Albrecht TA, Rosenzweig M. Management of cancer-related distress in patients with a hematologic malignancy. Journal of Hospice & Palliative Nursing. 2012;14(7):462–468. doi: 10.1097/NJH.0b013e318268d04e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pirl WF, Muriel A, Hwang V, et al. Screening for psychosocial distress: A national survey of oncologists. The Journal of Supportive Oncology. 2007;5(10):499–504. [PubMed] [Google Scholar]